Implementing 'Preventing ill health by risky behaviours'
This commissioning for quality and innovation (CQUIN) allows South London and Maudsley NHS Foundation Trust to refocus on alcohol screening and interventions.
Summary
While South London and Maudsley NHS Foundation Trust (SLaM) has made some progress in providing more robust assessment and interventions for people with alcohol problems, the challenges of inpatient care have made continued development of good practice difficult. The ‘Preventing ill health’ commissioning for quality and innovation (CQUIN) provides SLaM new impetus to refocus on alcohol screening and interventions and steps have been taken to modify its systems and protocols to achieve this.
Background
Alcohol is the substance most commonly used by people with mental health problems. Evidence suggests that the prevalence of alcohol use disorders in the psychiatric inpatient population may be as high as 50%. Mental and behavioural disorder due to alcohol use was the second most common cause of alcohol hospital related admissions in 2014 to 2015.
Alcohol contributes to over 60 physical health conditions and is likely to be a factor in the premature mortality of people with mental health problems. The average age of death of people with a diagnosis of mental and behavioural disorder due to alcohol is 57.5 years.
Alcohol is also strongly associated with a range of mental disorders, including depression, anxiety and bipolar disorder, as well as a range of risks, including suicide and violence/homicide.
While SLaM has made some progress in providing more robust assessment and interventions for people with alcohol problems, the challenges of inpatient care (like staff turnover, high use of bank and agency staff) have made continued development of good practice difficult.
As part of the local 2016 to 2017 dual diagnosis CQUIN, work was undertaken by SLaM to develop more robust pathways to substance misuse treatment. This work continues and the Preventing ill health CQUIN will provide further leverage for this given the requirement to offer referral and not solely signposting.
What was involved?
A Trust standard, in line with NICE guidance on alcohol screening, had already been developed to screen all service users aged 16 plus using AUDIT (Alcohol Use Disorders Identification Test). The 10 item version of AUDIT is the ‘gold standard’ tool and the version used in SLaM.
Following discussions with commissioners, agreements were made to ensure that work on the CQUIN could proceed in a way that was clinically meaningful in the context of mental health services.
Training on how to use AUDIT and deliver the interventions indicated by the score obtained is integrated into the Trust’s level 2 dual diagnosis training. This is a 5 day course, delivered 1 day each week, followed by a recall day about 6 weeks later. It is open to all staff.
As well as practising using AUDIT and delivering brief advice within the training, participants are required to practice these skills in their clinical areas as part of the ‘homework’.
For people that have not completed the dual diagnosis course the Alcohol Screening and Interventions for Inpatient Staff, a new half day course, has been developed. Rather than focus solely on brief advice (as suggested by the CQUIN), it is a broader alcohol screening and interventions training package.
The course aims to ensure that staff have the knowledge and skills to conduct alcohol screening, deliver brief advice, and know about, and can offer, referral to specialist substance misuse services.
It is anticipated that trained nurses and team dual diagnosis leads will take a lead on conducting the screening and providing the interventions so they are the target group for the training, however all inpatient staff are welcome to attend.
Other disciplines may be able to integrate delivering brief advice into their role. For example, on one ward an occupational therapist has included a session on alcohol in her healthy living group programme.
Given that nurses are the main target group the Alcohol Screening and Interventions training is now being embedded within the preceptorship programme for new nurses.
The consultant nurse for dual diagnosis is leading on implementation of the CQUIN. Each Clinical Academic Group (CAG) has identified a senior member of staff to take strategic responsibility for the CQUIN. New band 7 dual diagnosis practitioners in each acute inpatient unit have a key role supporting delivery of the CQUIN (like providing teaching, role-modelling, supervision, prompting staff). Each team is expected to have a team dual diagnosis lead and people in these roles are providing a ‘bottom up’ approach to supporting the work.
The Electronic Patient Journey (EPJ) - the Trust’s electronic patient record - was modified to ensure that data on alcohol screening and the delivery of the interventions could be extracted, so that an audit of information systems can be conducted. When AUDIT is completed the score is automatically calculated.
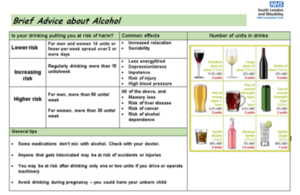
The drinking risk category that the person’s drinking falls into is displayed (lower, increasing or higher risk and possibly dependent), and a prompt to the type of intervention that is appropriate to that risk category is provided (like brief advice). Hyperlinks to further resources that can be printed out to support delivering of the interventions are in the system.
For the reporting process data were extracted from EPJs and dashboards created to audit progress. Overall alcohol screening was attempted on 43% of service users (362/840). A breakdown of the 362 screened showed:
- 83% were lower risk drinkers, so no specific intervention was required
- 10% were drinking at increasing or higher risk levels so were eligible for brief advice
- 8% were possibly dependent and therefore an offer of referral to a specialist alcohol service should have been made; this figure is higher than the 2014 Adult Psychiatric Morbidity Survey which reported that 1.9% were harmful or mildly dependent drinkers (AUDIT scores of 16 to 19) and 1.2% were probably dependent drinkers (AUDIT scores of 20 or more)
- In 14% of cases it was not possible to obtain the information required.; the most likely reason for this is that the person was too psychiatrically unwell
Because it was not possible to easily extract data from our electronic patient record on the number of interventions provided, changes were made to facilitate this. These require staff to record interventions in a different location and in a different way in the patient record. We think it is because of this change that the number of recorded interventions was very low - there were no reports of the people eligible for brief advice having received this intervention and only 4% of those eligible for referral to specialist alcohol services had been offered this.
Steps have been taken to remind people of this change: emailing information (with screenshots) to all the consultant psychiatrists, clinical service leads, ward managers and team dual diagnosis leads; including information on how/where to record interventions in the Alcohol Screening and Interventions for Inpatient Staff and dual diagnosis courses; and providing demonstrations of this during the training and at development days held for the team dual diagnosis leads.
What works well?
The use of AUDIT within the EPJ ensures that the alcohol risk score is automatically calculated and, based on this score, the system prompts the health professional to undertake the appropriate type of intervention.
Data on alcohol screening and the delivery of the interventions can be extracted, so that an audit can be conducted.
Ward managers can easily monitor the extent to which AUDIT has been completed by staff through its inclusion within the ‘My ward report’ system.
Information about the CQUIN was circulated in a variety of ways including:
- presentation at Q4 workshop for 2016 to 2017 dual diagnosis CQUIN
- presentations at dual diagnosis leads’ development days
- agenda items at various CAG meetings
- emails to key personnel
A summary sheet to outline the CQUIN requirements and how to record interventions on EPJ was also circulated widely.
What could be better?
Historically details of interventions have been recorded as free text in the ‘events’ section of the ‘ward progress note’. Recording interventions in this new way will require a change to reporting practice, and numbers have been low whilst this has become more embedded. Ensuring that staff know how to record interventions is part of the training.
Next steps
The milestones for Q1 have been met. A meeting with commissioners is now required to set Trust wide improvement targets across the indicators for subsequent quarters.
We have discussed with commissioners the possibility of conducting an audit on the people that took up the offer of referral to specialist services, to see if they engaged.
Further information
Contact Cheryl Kipping, Consultant nurse – dual diagnosis, South London and Maudsley NHS Foundation Trust <Cheryl.Kipping@slam.nhs.uk]>.