VDEC Pre-clinical team helps to develop organ-on-a-chip to protect human health
Scientists at VDEC use ‘organ-on-a-chip’ models to study infections and immune responses, aiming to improve vaccine testing and reduce reliance on animal research.
Executive summary
Scientists are constantly trying to improve the use and efficiency of models in research. As such, they are exploring a move away from traditional tissue or whole-body models. This move is proving to be a successful route to protecting human health against a variety of pathogens.
Target
The Pre-clinical team at UKHSA’s Vaccine Development and Evaluation Centre (VDEC) has developed an expanding capability in the use of microphysiological systems (MPS), an example of this are the ‘organ-on-a-chip’ models.
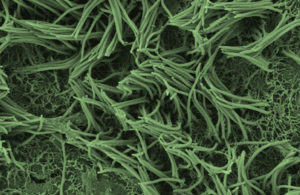
Essentially, we can grow a range of different cell types in 3D structures that represent tissues and mimic human organs in miniature chambers supplied with very small volumes of growth medium (a substitute for human blood). Although we started out simply by infecting these systems with various strains of pathogens, we are now developing the ability to introduce parts of the human immune system as well so that we can model and understand how our bodies fight infectious disease and how we can enhance or supplement that protection.
Aims
Understanding the correlates of protection for new and emerging coronaviruses is at the forefront of science strategy around the world. The pandemic potential of coronaviruses such as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Middle Eastern Respiratory Syndrome (MERS-CoV) has been proven in recent years. Understanding how they evolve, and impact humans is of utmost importance. Once we can understand how this works, we are then able to (or we then have another method to) test the efficacy of vaccines against evolving variants.
One model that highlights the importance of developing such systems is the adaptation of human alveolus MPS. The SARS-CoV-2 infection model described here (1) replicates the breathing-like stretch observed in lung epithelial cells and other biochemical characteristics of SARS-CoV-2 infection, allowing this to be used as a successful model of infection in live human tissue.
Options
An additional future benefit of this cutting-edge research is that it should help to reduce our reliance on animal research. Although that is a long-term view, it may also be possible that by increasing the complexity of the MPS models and analytical tools we use to interrogate them, we may one day be able to replace some aspects of animal research in medical research.
Outcome
Working alongside the teams that are developing and testing the MPS technology are teams using established challenge models, allowing direct comparison of human tissue replicating a whole organ system. The team at VDEC currently have 2 human lung-on-chip models. The first, a human bronchial airway and the second, human alveolus. Both models have been infected with SARS-CoV-2 in order to investigate the effect of this virus against various lung tissue types. A ‘non-breathing’ lung-on-chip alveolus model has also successfully been infected with SARS-CoV-2 and SARS-CoV, allowing characterisation of the differences between severe coronavirus infections.
Future work
Leading on from the success of the SARS-CoV-2 MPS, further work to develop a MPS model that can rival the current ‘gold standard’ MERS model is currently being carried out by the team at VDEC. This could provide clear evidence that MPS models are equally as effective as current models, refining the process of challenge studies across the board. We are working to extend the range of tissue types available for testing, for example working with brain and gut (2), as well as lung tissue to investigate movement of virus from organ to organ or to study difficult-to-study syndromes like long COVID or premature ageing.
The team is also pivoting transcriptomics, whole genome sequencing as well as sophisticated histopathological techniques to analyse these tiny samples. This means we will be able to detect small changes in the biochemistry, microbiology, and immunology of infected human cells very early on in the infection process to help us test new ways to protect humans. We have begun countermeasure testing antiviral drugs but intend to include vaccines testing as well using MPS technology, with a view to provide an alternate approach to certain aspects of human clinical trials. MPS-based technologies could allow detection of uniquely human issues with vaccine or therapeutic candidates ahead of human clinical trials, which could add an early ‘go’ or ‘no-go’ step as well as saving money downstream.
The use of MPS technology also allows our scientists to study infections from a new standpoint, as various environmental or immunological elements can be added or removed to investigate their impact. An example of this is that lung tissue can be infected with SARS-CoV-2 in the presence of individual immune cell populations to help us reveal and understand the significance of their roles in disease and recovery.
VDEC is at the forefront of this exciting technology, pushing its potential to the limits of human disease research and therapeutics for the benefit of public health.
Microphysiological systems: how ‘organ on a chip’ technology is changing science
References
-
Šuligoj, Tanja and Coombes, Naomi S and Booth, Catherine and Savva, George M and Bewley, Kevin R and Funnell, Simon GP and Juge, Nathalie. ‘Modelling SARS-CoV-2 infection in a human alveolus microphysiological system’. Access Microbiology (2024). 6:9.
-
Jones EJ, Skinner BM, Parker A, Baldwin LR, Greenman J, Carding SR and Funnell SGP. ‘An in vitro multi-organ microphysiological system (MPS) to investigate the gut-to-brain translocation of neurotoxins’. Biomicrofluidics (2024). Sep 13;18(5):054105. doi: 10.1063/5.0200459. PMID: 39280192; PMCID: PMC11401645.
Updates to this page
-
Added a video documentary of the organ-on-a-chip research.
-
First published.