Advancing our health: prevention in the 2020s – consultation document
Published 22 July 2019
Presented to Parliament by the Parliamentary Under Secretary of State for Public Health and Primary Care.
July 2019
CP 110
ISBN: 978-1-5286-1545-7
Executive summary
1. Opportunities
The 2020s will be the decade of proactive, predictive, and personalised prevention. This means:
- targeted support
- tailored lifestyle advice
- personalised care
- greater protection against future threats
New technologies such as genomics and artificial intelligence will help us create a new prevention model that means the NHS will be there for people even before they are born. For example, if a child had inherited a rare disease we might be able to diagnose and start treatment while they are still in the womb, so they are born healthy.
Using data held by the NHS, and generated by smart devices worn by individuals, we will be able to usher in a new wave of intelligent public health where everyone has access to their health information and many more health interventions are personalised.
In the 2020s, people will not be passive recipients of care. They will be co-creators of their own health. The challenge is to equip them with the skills, knowledge and confidence they need to help themselves.
We are:
-
embedding genomics in routine healthcare and making the UK the home of the genomic revolution
-
reviewing the NHS Health Check and setting out a bold future vision for NHS screening
-
launching phase 1 of a Predictive Prevention work programme from Public Health England (PHE)
2. Challenges
Over the decades, traditional public health interventions have led to significant improvements in the nation’s health.
Thanks to our concerted efforts on smoking, we now have one of the lowest smoking rates in Europe with fewer than 1 in 6 adults smoking. Yet, for the 14% of adults who still smoke, it’s the main risk to health. Smokers are disproportionately located in areas of high deprivation. In Blackpool, 1 in 4 pregnant women smoke. In Westminster, it’s 1 in 50.
Obesity is a major health challenge that we’ve been less successful in tackling. And clean air will continue to be challenging for the next decade. On mental health, we’ve improved access to services. In the 2020s, we need to work towards ‘parity of esteem’ not just for how conditions are treated, but also for how they are prevented. On dementia, we know ‘what’s good for your heart is also good for your head’. A timely diagnosis also enables people with dementia to access the advice, information, care and support that can help them to live well with the condition, and to remain independent for as long as possible.
The new personalised prevention model offers the opportunity to build on the success of traditional public health interventions and rise to these new challenges.
The NHS is also doing more on prevention. The Long Term Plan contained a whole chapter on prevention, and set out a package of new measures, including:
- all smokers who are admitted to hospital being offered support to stop smoking
- doubling the Diabetes Prevention Programme
- establishing alcohol care teams in more areas
- almost 1 million people benefiting from social prescribing by 2023 to 2024
These measures will help to shift the health system away from just treating illness, and towards preventing problems in the first place.
We are:
-
announcing a smoke-free 2030 ambition, including options for revenue raising to support action on smoking cessation
-
publishing Chapter 3 of the Childhood Obesity Strategy, including bold action on: infant feeding, clear labelling, food reformulation improving the nutritional content of foods, and support for individuals to achieve and maintain a healthier weight. In addition, driving forward policies in Chapter 2, including ending the sale of energy drinks to children
-
launching a mental health prevention package, including the national launch of Every Mind Matters
3. Strong foundations
When our health is good, we take it for granted. When it’s bad, we expect the NHS to do their best to fix it. We need to view health as an asset to invest in throughout our lives, and not just a problem to fix when it goes wrong. Everybody in this country should have a solid foundation on which to build their health.
This is particularly important in the early years of life. Most children are born into safe and loving homes that help them develop and thrive. But this is not always the case. We must help all children get a good start in life.
This ‘asset-based approach’ should then follow through to other stages of life, including adulthood and later life. It’s difficult to live a fulfilling life if you’re worried about money, live in cold or damp conditions, or feel cut-off from those around you.
At national level, we will lay the foundations for good health by pushing for a stronger focus on prevention across all areas of government policy. At local level, we expect different organisations to be working together on prevention. This means moving from dealing with the consequences of poor health to promoting the conditions for good health and designing services around user need, not just the way we’ve done things in the past.
We will:
-
launch a new health index to help us track the health of the nation, alongside other top-level indicators like GDP
-
modernise the Healthy Child Programme
-
consult on a new school toothbrushing scheme, and support water fluoridation
Conclusion
The commitments outlined in this green paper signal a new approach for the health and care system. It will mean the government, both local and national, working with the health and care system, to put prevention at the centre of all our decision-making. But for it to succeed, and for us to transform the NHS and improve the nation’s health over the next decade, individuals and communities must play their part too. Health is a shared responsibility and only by working together can we achieve our vision of healthier and happier lives for everyone.
Introduction
From life span to health span
Thanks to developments in public health and healthcare, we’ve made great progress in helping people to live longer lives. For example, life expectancy has increased by almost 30 years over the past century.[footnote 1] Cancer survival rates are up [footnote 2] and mortality rates from heart disease and stroke are down.[footnote 3]
However, these improvements in life expectancy are beginning to slow,[footnote 4] and over 20% of years lived are expected to be spent in poor health. On average, men born today can expect to live 16 years in poor health. For women, it’s 19 years.[footnote 5]
There is also a clear social gradient to healthy life expectancy. That is, people in deprived areas tend not only to live shorter lives, but they also spend more of those years in poor health. For example, women living in the 10% most deprived areas can expect to live 18 fewer years in good health than those in the 10% least deprived areas.
Figure 1: Female healthy life expectancy at birth and years lived in poorer states of health by national deprivation deciles, England, 2015 to 2017[footnote 6]
Deprivation deciles: 1 = most deprived, 10 = least deprived
| Deprivation decile | Healthy life expectancy | Years lived in poorer states of health | Life expectancy |
|---|---|---|---|
| 1 | 52.0 | 26.7 | 78.7 |
| 2 | 56.9 | 23.5 | 80.3 |
| 3 | 59.2 | 22.4 | 81.6 |
| 4 | 61.9 | 20.6 | 82.5 |
| 5 | 64.1 | 19.0 | 83.1 |
| 6 | 65.8 | 17.9 | 83.7 |
| 7 | 66.9 | 17.3 | 84.2 |
| 8 | 68.2 | 16.4 | 84.6 |
| 9 | 68.7 | 16.5 | 85.1 |
| 10 | 70.4 | 15.9 | 86.2 |
Inequalities also exist across a range of other dimensions, including ethnicity, gender, sexuality and having a disability. The underlying causes of these inequalities often cluster together, with people experiencing ‘multiple disadvantage’. There are also certain groups who experience poorer health outcomes than the wider population, such as people sleeping rough, leaving care, and offenders in prison or in the community.
For learning disabilities, autism and other neurodevelopmental or behavioural conditions such as attention deficit hyperactivity disorder (ADHD), an early diagnosis can help a child’s development. Specifically, it can help them get the help they need at school, and ensure families and carers can support them better. This in turn helps to improve wider outcomes and prevent needs escalating. But this early diagnosis doesn’t always happen. We also know that adults living with these conditions often have worse mental and physical health than the wider population, and can struggle to access the help they need.[footnote 7]
Risk factors like obesity, smoking and physical inactivity place us at higher risk of both early death and ill-health/disability.[footnote 8] Yet, we know the things that kill us (such as cancer, heart disease and stroke) are not always the same as the things that make us unwell. Some of the most common causes of ill-health are: joint, bone and muscle problems, depression and anxiety, long-term conditions like asthma and diabetes.[footnote 9]
Figure 2: Leading causes of years lived with disability, England, 2017[footnote 10]
| Cause | Percentage of total years lived with disability |
|---|---|
| Musculoskeletal disorders | 22.7% |
| Mental disorders | 14.0% |
| Neurological disorders | 9.0% |
| Unintentional injuries | 6.4% |
| Chronic respiratory diseases | 6.3% |
| Sense organ diseases | 6.0% |
| Other non-communicable diseases | 5.8% |
| Skin and subcutaneous diseases | 5.6% |
| Diabetes and kidney diseases | 4.9% |
| Cardiovascular diseases | 4.4% |
Problems with joints, bones and muscles
For the last 30 years, problems with joints, bones and muscles have been the most common cause of years lived with disability in England.[footnote 11] They affect around 15 million people (1 in 3 adults in England).[footnote 12] They are sometimes called musculoskeletal (or ‘MSK’) conditions. The most common are conditions of musculoskeletal pain, such as osteoarthritis or back and neck pain. Women are more likely to be affected than men.[footnote 13] The risk of having back pain also increases with rising body mass index.[footnote 14] For this reason, the policy priority is helping people to achieve a healthier weight, eat well and stay active.
Osteoarthritis: Nora’s story
Nora used to struggle to cope with the pain of osteoarthritis. Her muscles and joints had become stiffer and more painful, making it harder to enjoy interests like jam-making, gardening and art classes. Nora decided it was time to make some changes to push back against the negative impact arthritis was having on her life.
After taking advice from healthcare professionals and doing online research, Nora started an exercise routine that worked for her, incorporating Pilates, low-impact exercise on a cross-trainer or a bike and swimming.
“My advice to anyone with arthritis is to keep moving. I know everyone says that but take it from me I’ve seen such positive changes in my life since I’ve been exercising. It’s the small things you notice that make the biggest difference to how you feel. For the first time in years I’m able to make jam from the fruit I grow in my garden without taking medication. That means the world to me.”
Depression, anxiety and other mental health problems
Poor mental health is the second most common cause of years lived with disability in England.[footnote 16] The most common conditions are depression and anxiety, which make up the majority of mental health cases.[footnote 17] Approximately 1 in 4 people report living with a mental health issue.[footnote 18] Incidence is highest in the working-age population, and higher in women than men.[footnote 19] Other groups at greater risk include: those living on low incomes, people with problem debt, and those identifying as lesbian, gay, bisexual or transgender (LGBT).[footnote 20]
Anxiety and depression at work: Helen’s story
Helen was first diagnosed with a mental health condition 15 years ago. After speaking to colleagues at work, Helen now receives the help and support she needs to continue in her role.
“It was around 3 years ago when I suffered panic attacks. I was feeling sick, not wanting to go into work. I had depression as well; you don’t even want to get out of bed, you just want to hide.”
Other long-term health conditions
Together, musculoskeletal problems and mental health conditions account for almost 40% of the total years lived with disability in England. The remaining 60% is split among a number of mainly long-term conditions, such as diabetes, lung conditions like asthma and chronic obstructive pulmonary disease (COPD), sight loss, hearing loss and dementia.[footnote 22]
In many cases, long-term conditions cluster together. This is sometimes called multimorbidity. There are no official measures, but between 15 and 30% of the adult population are thought to be living with multiple conditions.[footnote 23] Problems are more common in later life, in deprived communities, and among people who are overweight or who smoke.[footnote 24]
Living with multiple conditions: Susan’s story
Susan used to work as a catering manager at a university. She had to stop work in 2008 when she got fibroids, and was bedridden for 2 weeks at a time. Since stopping work, Susan has been diagnosed with osteoarthritis, COPD, hypothyroidism, angina, high blood pressure and high cholesterol, depression and diabetes. She takes 14 different medications every day and her illnesses can feel as though they consume her life.
“I just have to take each day as it comes. Planning doesn’t work.”
The drivers of good health
The good news is that much premature ill-health and disability can be prevented, and there are actions we can take to increase our chances of living longer, healthier lives. Some health conditions we are born with and cannot avoid. Where this is the case, the priority is supporting people to enjoy a good quality of life and to live well.
The mission
Last year, the government set a mission as part of the Ageing Society Grand Challenge[footnote 26] to “ensure that people can enjoy at least 5 extra healthy, independent years of life by 2035, while narrowing the gap between the experience of the richest and poorest”.
The green paper proposals will not deliver the whole ‘5 years’. But they will help us towards achieving this mission. Further details on this will be provided later in the year, through a government response to the green paper.
The mission is based on the technical term ‘disability-free life expectancy at birth’. That is, the time a child born today can expect to live without a limiting health condition: a mental or physical condition that’s long-term and affects day-to-day activities.[footnote 27]
The latest figures for disability-free life expectancy are 62 years for women and 63 for men.[footnote 28] To achieve our mission in England, we will need to increase this to at least 67 for women and 68 for men by 2035. That’s almost 4 months per year. Given that disability-free life expectancy has remained stable in recent years,[footnote 29] this is likely to be extremely difficult, and will require bold action.
Much has been written on the factors that shape our health. As set out in the Prevention Vision, evidence suggests there are 4:
- the services we receive (Chapter 1)
- the choices we make (Chapter 2)
- the conditions in which we live (Chapter 3)
- our genes, which we inherit from our parents
Figure 3: Determinants of premature mortality and their contribution (McGinnis and others, 2002)[footnote 30]
Genetic predisposition, 30%; social circumstances, 15%; health care 10%; environmental exposure 5%; behavioural patterns, 40%
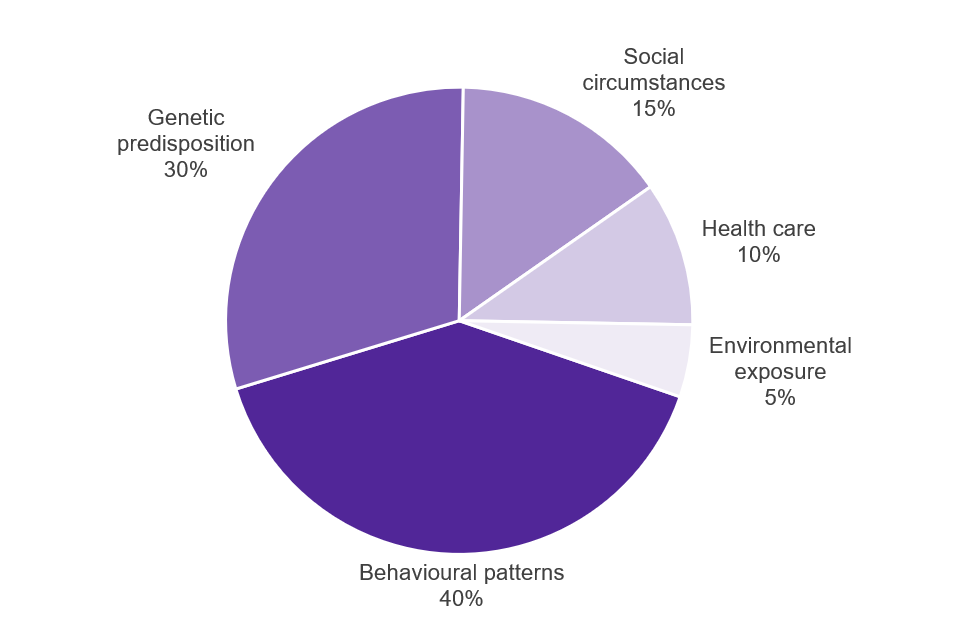
Figure 4: Estimated impact of determinants on health status (Canadian Institute of Advanced Research, 2002)[footnote 31]
Health care system 25%; biology/genetic endowment 15%; physical environment 10%; social and economic environment 50%
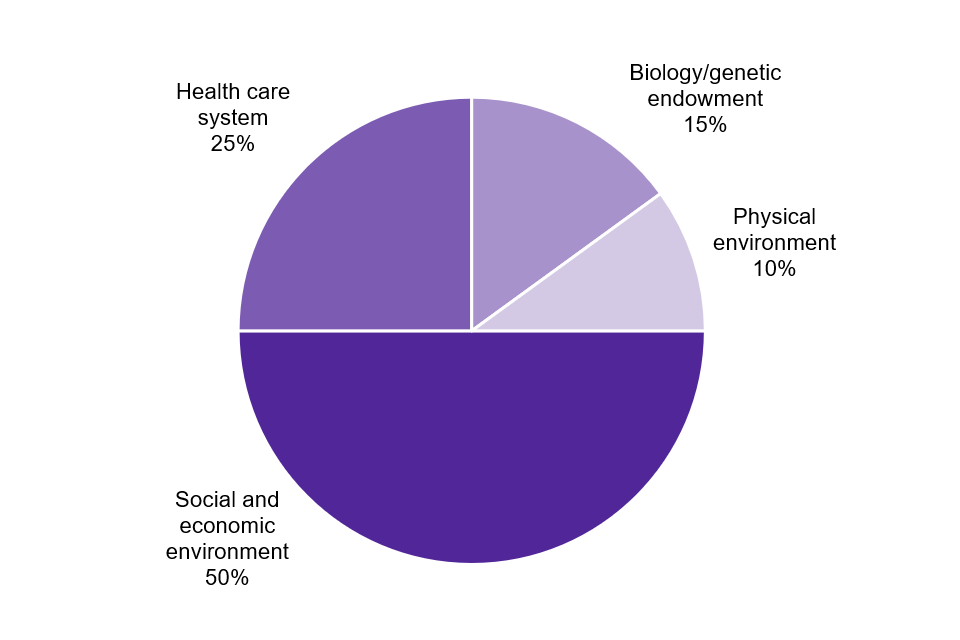
There are different views about the contribution made by each, which is likely to vary from person to person and from disease to disease. Nevertheless, most people agree that the choices we make, shaped by the conditions in which we live, have the biggest impact. The focus of this green paper is on services, choices and conditions.
If we are to achieve our mission, we need to take bold action in all areas: making the most of the opportunities in front of us and being open to innovations ahead. This includes:
- bringing in a new wave of intelligent public health, which is more proactive, predictive and personalised, while also taking tough action on our biggest challenges: smoking, obesity and mental ill-health[footnote 32]
- taking a behavioural science approach to some of our biggest challenges on prevention. This means making healthy choices as easy as possible for people, and, in some cases, making all options healthier
- viewing health as our most precious asset, and not just a problem to fix when it goes wrong. Good health is the foundation of happy families, thriving communities, and a strong economy. When our health is good, we take it for granted. When our health is bad, we expect the NHS to do their best to fix it. We need to lay the foundations for good health so everyone has a chance to live a healthy and happy life
Chapter 1: Opportunities
Intelligent public health
In today’s increasingly digital world, technology and data have a clear role to play in helping us to deliver more proactive, predictive and personalised services to people. We’ve already taken the first steps in doing this.
PHE’s social marketing campaigns already personalise lifestyle advice to different audiences, with 90% of their social media messaging on smoking being seen by people who smoke. That’s modern, efficient and focused prevention in action.
The future is even greater personalisation and a closer fit with individual needs. There will always be a place for interventions that improve everyone’s health. But it can be less intrusive and better value for money to offer people more personalised and tailored support. Many are already opting in to this kind of approach. In the next decade, intelligent public health will mean:
- focused support and advice to those who need it and choose to participate
- precision medicine
- tackling current and future threats
Predictive prevention
Starting this year, PHE will work together with NHSX and other partners across the public health system, academia, industry and the voluntary sector to build a portfolio of new innovative projects that will help us evaluate and model Predictive Prevention at scale.
Phase one of the programme includes:
-
getting the foundations right by building trust with the public about how data can be used to improve their experience, and the benefits of participating
-
refining our overall approach to analysis and insight generation to help us understand and support the most at-risk and vulnerable groups
-
developing exemplar projects to prove the concept of personalised prevention and establish the evidence base
-
designing the future shape of the programme, with a view to increasing the scale and ambition
Use of data: a citizen’s view
The data we generate about our health, our activities, our genomes and our environment can empower us in unimaginable ways. We can tailor our diet to meet our metabolism, we can account for air pollution in our exercise plans, and we can take action to prevent painful diseases decades before they would begin. And we know this is only the beginning.
Finding insights in this data is an ongoing challenge, one that can be met on our phones and tablets, in the GP surgery or nationally, at a population level. We are entering a new era of evidence-based self-care, driven by us as patients in partnership with the NHS.
PHE and the NHS use data and insights to create these algorithms and models, and the public can have a role in this if we choose to help by either allowing our phones and devices to send data, or by allowing PHE and the NHS to access our anonymised clinical data. There is some indication from PHE’s targeted marketing campaigns that citizens are willing to share their contact details to receive information, and to have an ongoing dialogue around health issues relevant to them. To date, there have been over 7.1 million responses to this type of offer from PHE. The UK Biobank has also been able to build a record of the data of over half a million volunteers.
To make this work, PHE and NHS organisations will ensure that they respect and protect our data. They will focus on the requirements of the General Data Protection Regulation and Data Protection Act 2012, adhere to the Caldicott principles and implement Department of Health and Social Care (DHSC) policy on patient preferences. At all stages, they will work closely with the Information Commissioner’s Office, the National Data Guardian, the new Centre for Data Ethics and Innovation, and academics and other experts in information governance.
They will work closely with the public, privacy organisations and other relevant bodies including the Information Commissioner’s Office and the Centre for Data Ethics and Innovation, to understand what we consider to be acceptable use of our data. They will also explore developing models of dynamic, informed consent, so we can choose how and when we want to share our personal data for this purpose.
The impact achieved will be constantly evaluated in the open, with regular and transparent engagement with the health sector and the public – ensuring that individual interventions are having a positive impact overall, and that we are narrowing the gap between richest and poorest.
Some of the most exciting opportunities for intelligent prevention are those that can be developed locally, including as part of devolution areas that have a broad focus on economic development alongside a commitment to improve health. The learning from these experiences can be shared more widely to enable other areas to benefit.
In support of this ambition, the government is exploring ways to support a West Midlands Combined Authority Radical Prevention Fund. This will involve a programme of work to explore, test and learn from new opportunities to prevent ill-health using the latest technology – stimulating innovation in ways that can support both health and wealth.
Case study: Digital Diabetes Prevention programme
From August 2019, there will be a digital way to take part in the Healthier You: NHS Diabetes Prevention Programme. The digital version gives the same advice on healthy eating, exercise and weight management as the face-to-face programme, but through wearable technologies, apps and websites. It is designed for those at risk of type 2 diabetes who find it difficult to attend sessions because of work or family commitments. Early analysis from pilots involving over 4,000 people shows the digital programme is reaching more people of working age.
Andrew, a 51-year-old farmer from North Yorkshire, took part in the pilot. This helped him lose weight and reduce his blood sugar levels out of the pre-diabetic range. He said:
“It’s given me a helping hand in the right direction. I get a video message from my personal health coach a couple of times a week with diet recommendations and fitness techniques personalised to me and my lifestyle plan. I send a text back and we keep up the conversation digitally. I also like reading the comments and conversations on the online community.”
The NHS is also working to give more people access to digital ways to manage their diabetes, including through an online ‘healthy living for people with type 2 diabetes’ support tool, and by investing £2 million into a new NHS Test Bed programme. Last year (2018), NHS England also launched a guide on NHS UK for managing type 1 diabetes.
Focused support and advice
In the future, the support and advice we provide to people will become much more focused and tailored. We will start this transformation with 2 of our largest existing programmes – screening and NHS Health Checks.
Intelligent screening
Screening programmes have long been used to identify those at risk of or already living with health problems. By preventing conditions – or detecting them at more treatable stages – it’s possible to save lives and improve outcomes.
Our vision for future screening in the NHS is for:
- uptake to be maximised, including by making screening easier for people to access, and tackling unjustified variations in take-up
- existing national screening programmes to become more personalised and stratified by risk, so we focus interventions where they are most needed. For example, reviewing the case for increasing cervical screening intervals for lower-risk groups, such as women vaccinated against human papillomavirus. We also know that the predictive power of a screening test is increased if you identify high-risk groups, rather than screening everybody
- focused screening within high-risk populations to be offered for a greater range of conditions. For example, considering introducing lung cancer screening to high-risk individuals, such as smokers, together with more personalised ongoing support
- better use of technology, including an expansion of our offer on genomics, better use of data and embedding the use of artificial intelligence. This includes incorporating genetic testing into screening and diagnostics. For example, using next generation sequencing to confirm cases of cystic fibrosis in children (currently being tested in the newborn bloodspot programme), or screening for genes associated with Lynch syndrome, which leads to an increased risk of bowel cancer
- recommendations to be developed in a co-ordinated way across different kinds of screening opportunity, while continuing to be based on the best evidence and advice. For example, by reviewing how the different sources of expert advice on screening, in particular the National Institute for Health and Care Excellence (NICE) and the UK National Screening Committee (UK NSC), relate to one another
- faster implementation of recommended interventions and programmes, with clear accountability for delivery and investment in supporting IT
Professor Sir Mike Richards is currently carrying out a review of cancer screening. The report is due to be published in September 2019. This provides a good opportunity to update and modernise our approach to screening.
We recognise that there are challenges in the existing screening arrangements, and that reform is needed to achieve our vision for the future. Recommendations from the review will help shape our plans for change, supported by a strategic review of IT required to enable our vision for future screening. NHSX will lead on this element of the screening strategy.
We also recognise that there remains variation in screening outcomes across the country, and by deprivation and ethnicity. As part of our response to Public Accounts Committee (PAC) recommendations, we will set out our understanding of the variation in performance and a plan for reducing these inequalities. We are due to respond to these recommendations in July.
Intelligent health checks
NHS Health Checks is a national programme commissioned by councils. Health Checks offer people aged 40 to 74 a free check-up of their overall health, every 5 years. The results can tell people whether they are at higher risk of developing certain health problems, such as heart disease, diabetes, stroke and dementia. They help underpin the NHS Long Term Plan commitments to prevent 150,000 heart attacks, strokes and cases of dementia, and to double the NHS Diabetes Prevention Programme.
Case study: Southwark Digital Health Check tool
Southwark Council developed an online digital health check tool to help more people benefit from the NHS Health Check programme. People who had already been offered an NHS Health Check, but had not responded, were sent a text message inviting them to access the digital check.
A third of the people accessed the digital check. Half of these completed it to find out their chance of having a heart attack or stroke in the next 10 years. More than 1 in 10 of those using the digital check were found to be at high risk of having a heart attack or stroke and so went on to complete a face-to-face NHS Health Check. These important checks focus on the leading causes of premature death and ill-health such as obesity, smoking, high blood pressure and type 2 diabetes, therefore offering people the chance to lower or manage their risk.
The NHS Health Check programme has achieved a lot. But uptake varies across the country,[footnote 33] the risks identified in a check could be followed up more consistently by the NHS, and evidence is emerging that people could benefit from a more tailored service.[footnote 34] There may also be a case for a particular focus on supporting people through key changes in their life, in particular thinking about future care needs and how they can remain healthy and active in older age.
Building on the gains made over the last 10 years, we believe the time is right to take a step back and consider whether changes to the programme could help it deliver even greater benefits. The government will commission an evidence-based review of the NHS Health Checks programme to maximise the benefits it delivers in the next decade.
Details will be confirmed later this year, but the scope is likely to include:
- ways of increasing uptake, particularly among high-risk groups
- options for making it more focused, for example identifying people on the basis of information about their likely risks, rather than making the same offer to everyone. This could mean more support to those who need it most
- considering how it’s delivered, for example using developing digital service offers to intervene in a more efficient and tailored way
- reviewing what’s covered in an NHS Health Check, for example increasing the range of health and care advice that checks can offer
- reviewing the evidence for a specific ‘MOT’ when approaching retirement age to help prevent or delay future care and support needs
Precision medicine
Genomics is changing the future of health and medicine. From providing more tailored cancer treatments to helping diagnose unknown conditions, it will underpin a new era of precision medicine. Over the next decade, we want to build on our position as a world leader in genomics and make the UK the number one destination to research and develop the latest scientific advances in genomic healthcare.
How genomics works
The human genome is made of DNA and is the ‘instruction manual’ for how our bodies come into existence, maintain our cells, and ultimately die. It is the unique blueprint that makes every person different from every other, and tiny variations in the genome can have significant impacts on our life and health. Sequencing these variations can help doctors identify people at risk of developing treatable diseases, speed up diagnoses and find effective personalised treatments that deliver better results with fewer side effects.
For the last 70 years, the UK has been at the forefront of the use of genetics to improve healthcare. However, it’s only in the last 10 years, with advances in science and technology, that we have begun to unlock the wider potential. We have led the way globally with initiatives like the 100,000 Genomes Project, which was led by Genomics England and is the largest national sequencing project anywhere in the world. This project is already making a real difference for patients. Early results show 1 in 4 rare disease patients previously without a diagnosis now receive one, and up to half of cancer patients could be provided with findings that put them and family members on a better care pathway.
Later this year, Genomics England and the NHS will start returning results of additional findings related to preventable conditions to participants who have chosen to receive them. These may be available based upon follow-up analysis of their samples.
The Genomic Medicine Service in the NHS is the first of its kind in the world to integrate whole genome sequencing into the healthcare system. It aims to deliver equitable access to genomic testing to help more accurately diagnose disease and personalise treatments and interventions. Our partnerships with researchers, industry and governments, domestically and internationally, all contribute to advancing this area.
Genomic approaches will be transformative for early detection of many of the common diseases and cancers. Opportunities to understand how best to realise these benefits will be explored as part of plans to sequence 5 million genomes by 2023 to 2024, through a unique collaboration between the NHS, UK scientists and industry.
Genetic risk in healthy populations
We know genetic factors play a role in human health and disease, including most major chronic diseases. For some diseases, many thousands of genetic variations across our genomes each have a small impact on the chance that we will develop some common diseases. It is now possible to combine this genetic information from many people into polygenic risk scores (PRS), which identify those at highest risk of particular diseases. This could allow individuals to make lifestyle changes that will help prevent disease or reduce its impact, lead to more effective prescription medicines and improve other public health interventions.
PRS could also help to define new, currently invisible, patient populations. This could, for example, include people at risk of heart disease who would benefit from receiving statin therapy but who are currently not receiving preventative treatment because their blood pressure and cholesterol levels are normal. As the evidence develops, complementing existing risk scores (such as the QRisk Score for cardiovascular disease) with this kind of genetic information will be a priority for the UK healthcare system.
Building on recent advances realised through UK BioBank, the clinical implementation of this approach will be pioneered at scale in the new Accelerating Detection of Disease (ADD) challenge, which aims to recruit up to 5 million healthy participants into a world-leading research cohort in order to shed new light on the detection and treatment of common diseases. A key part of the ADD challenge will be to offer as many participants as possible their PRS. Individuals will volunteer their genetic information, which will be used in accordance with relevant legislation, regulation and good practice guidance on use of data, in order to develop and improve the evidence base for the use of PRS.
The goal of the ADD challenge will be to support research, prevention and treatment across major chronic diseases, including cancer, dementia, heart disease and mental health conditions. The project will seek to enrol under-represented groups, such as ethnic minorities, to enable a better understanding of disease and preventative measures for every individual in society and reduce existing health inequalities. The project brings together the NHS, industry and leading charities including Cancer Research UK, the British Heart Foundation and Alzheimer’s Research UK. It will be the largest ever study of its kind, collecting a broad range of data from healthy volunteers over many years.
We will be publishing a National Genomics Healthcare Strategy in autumn 2019. This will set out how the genomics community can work together to make the UK the global leader in genomic healthcare.
We have an ambition to embed genomics in routine healthcare and make the UK home to the genomic revolution that’s on the horizon.
By 2023 to 2024, the UK will aim to carry out 5 million genomic analyses, including sequencing at least one million whole genomes from patients in the NHS and participants in the UK Biobank.
Some of these genomic analyses will be provided by the ADD challenge, which will now incorporate the government’s commitment to develop a genomic volunteer service and will be free to participants.
This year, seriously ill children who are likely to have a rare genetic disorder, children with cancer, and adults suffering from certain rare conditions or specific cancers will be offered whole genome sequencing as part of their routine care. This will put the UK at the cutting edge of genomic technologies to predict and diagnose inherited and acquired disease, and to personalise treatments and interventions.
Case study: Whole genome sequencing
Genome sequencing has the potential to dramatically improve the speed of diagnosis and influence the treatment plans for children with rare childhood conditions. The Next Generation Children Project led by clinical researchers in Cambridge used whole genome sequencing to help doctors identify genetic diseases in 350 babies receiving intensive care at Addenbrooke’s Hospital.
The study showed that the diagnosis and treatment of some of the most critically ill babies can be improved by sequencing their whole genome. A diagnosis was provided in 2 to 3 weeks instead of around 3 to 6 months and identified a quarter of the babies as having an underlying genetic condition. The diagnosis also changed the treatment plans for three-quarters of the babies which often saved the need for further tests.
Tackling current and future threats
Antimicrobial resistance
Antimicrobial resistance (AMR) is one of the most pressing global challenges we face this century. If no action is taken, up to 10 million people per year could die worldwide. This would make drug-resistant infections a bigger killer than cancer currently is now over the next 30 years.[footnote 35] AMR is already estimated to contribute on average to over 2,000 deaths annually and cost the NHS approximately £95 million each year in the UK.[footnote 36]
In recognition that there are no ‘quick fixes’, the UK government set out its longer-term vision of a world in which AMR is contained and controlled by 2040, supported by a 5-year action plan. This covers actions across human and animal health, addressing infection prevention, use of antimicrobials, increasing the availability of clean water, and minimising spread through the environment and food.
Tackling sepsis
Our recent focus on sepsis has meant better awareness and improved recognition of symptoms among clinicians, with more people being correctly diagnosed. At the same time, as we face the possibility of a world without effective antibiotics, it’s critical that we conserve our antibiotics so that they remain effective when they are really needed.
The UK’s 5-year national action plan for AMR includes the commitment to develop a real-time patient-level data source of patients’ infection, treatment and resistance history that will be used to inform their treatment and the development of interventions to tackle severe infection, sepsis and AMR.
But the UK cannot tackle AMR alone. Global problems require global solutions. That’s why One Health co-ordinates action in all sectors, across the world. In the UK, we continue to play our part globally by modelling best practice, sharing this good practice with other countries, and supporting international efforts.
To maintain the UK’s position as world leaders on AMR and to deliver international action, we have appointed Professor Dame Sally Davies as the UK Special Envoy on AMR.
As an international expert, Dame Sally will support the UK government on the delivery of their 5-year AMR action plan while working with the World Health Organization, World Organisation for Animal Health, Food and Agriculture Organization and the United Nations to maintain momentum on the global stage. Dame Sally will work across all sectors and advise on the delivery of a ‘One Health’ response to AMR including health, agriculture and the environment.
A new model for the evaluation and purchasing of antimicrobials in the UK
The national action plan includes a commitment to testing solutions that address the failure of companies to develop new antimicrobials. We’re the first country in the world to announce that we’ll test new, innovative models to pay companies for antibiotics based on their value to the NHS, not volumes used. We hope this will send a strong signal to the rest of the world that testing models to incentivise the development of new, vital medicines is of great importance.
The UK represents only a small part of the global market for these drugs. For this to have the full effect, we need other countries to offer similar incentives in their own domestic markets. We hope that by leading the way and promoting the project internationally, they will do just that.
Immunisations
Vaccinations are one of the most cost-effective health interventions.[footnote 38] Not only are there substantial health gains – saving lives, protecting vulnerable groups and reducing disability – but they also reduce pressure on the NHS and improve productivity.[footnote 39] Despite this, there’s been a gradual decline in vaccine uptake in recent years, with too many people not getting the vaccines they need for themselves or their children.[footnote 40]
By spring 2020, we will launch a Vaccination Strategy, to maintain and develop our world-leading immunisation programme. The strategy will include action on:
-
Operational work to increase uptake of all recommended vaccinations across all communities and areas, to include the medium-term aim of reaching over 95% uptake for childhood vaccinations and continuing to increase uptake of the seasonal influenza vaccine. This includes implementing the UK measles and rubella elimination strategy to increase uptake of the second dose of the MMR vaccine to at least 95%, to match the aspiration for the first dose.
-
Enhanced use of local immunisation co-ordinators and primary care networks, ensuring the right mechanisms are in place to increase uptake (through the GP Vaccines review) including consistent application of call and recall, and improved data services.
-
Continued evolution of our immunisation programme, incorporating new, more effective and cost-effective vaccines and new uses for existing vaccines across the life course, as advised by our expert group, the Joint Committee on Vaccination and Immunisation.
The government will also continue to emphasise the preventative value of vaccines at every opportunity. This is to ensure that people have the facts they need, and that vaccine misinformation is addressed as effectively as possible.
Chapter 2: Challenges
When it comes to living a healthier life, the modern world presents many challenges. It can feel like the odds are stacked against us. This is particularly the case if you’re living on a low income or have a serious mental illness or learning disability. This green paper is not about nannying, but empowering people to make the decisions that are right for them. It’s about providing everyone with the chance to live happy, healthy lives.
By taking a few actions, we can reduce our chances of developing arthritis, dementia, diabetes and various other health conditions. This applies to people of all ages. Evidence suggests our biggest challenges are: being smoke-free, eating a healthy diet and staying active, and taking care of our mental health.[footnote 41]
Figure 5: Leading risk factors of years lived with disability, England, 2017[footnote 42]
| Risk factor | Percentage of total years lived with disability |
|---|---|
| High body-mass index | 6.4% |
| Tobacco | 5.9% |
| High fasting plasma glucose | 5.5% |
| Occupational risks | 3.3% |
| Dietary risks | 3.1% |
| High systolic blood pressure | 2.3% |
| Drug use | 2.3% |
| Alcohol use | 2.2% |
| Child and maternal malnutrition | 1.9% |
| Air pollution | 1.5% |
Being smoke-free
There has been good progress in moving towards a smoke-free society. Over the last 35 years, smoking rates in Great Britain have halved.[footnote 43] We now have one of the lowest rates in Europe,[footnote 44] with fewer than 1 in 6 adults smoking.
Figure 6: Adult smoking prevalence in England, 2011 to 2018[footnote 45]
19.8% in 2011; 19.3% in 2012; 18.4% in 2013; 17.8% in 2014; 16.9% in 2012; 15.5% in 2016; 14.9% in 2017; 14.4% in 2018
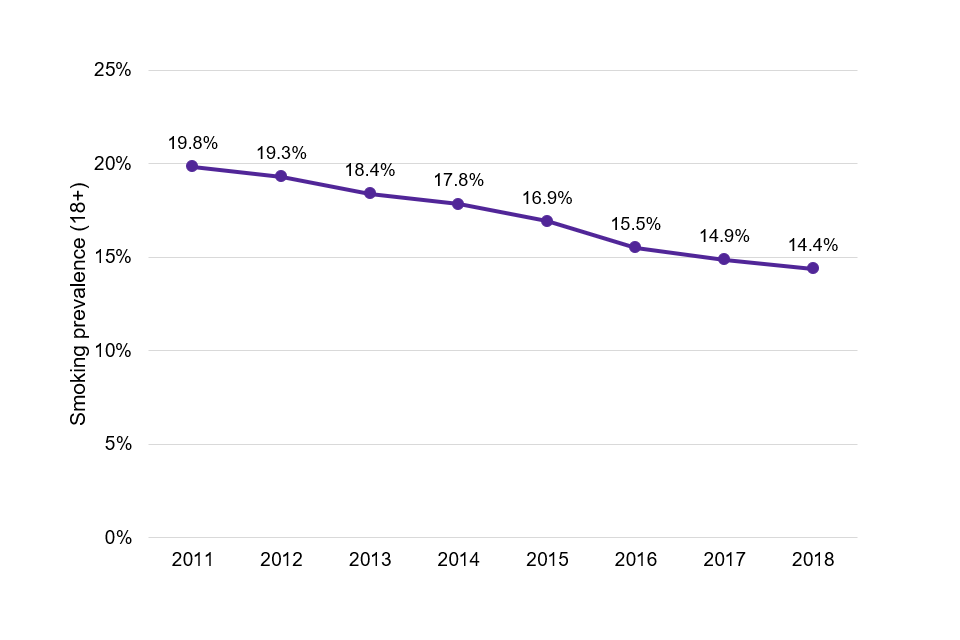
This remarkable change is the result of decades of concerted effort and government action. We were one of the first countries to ban smoking in public places (2007), we established education campaigns like Stoptober (2012), and introduced plain packaging for cigarettes (2016). Recently, the government also published a tobacco control plan, which included the goal of reducing smoking rates to 12% in adults by 2022.
The gains in tobacco control have been hard-won, and there’s still much to do. For the 14% of adults who are not yet smoke-free,[footnote 46] smoking is the leading cause of ill-health and early death, and a major cause of inequalities.[footnote 47] That’s why the government wants to finish the job.
We are setting an ambition to go ‘smoke-free’ in England by 2030.
This includes an ultimatum for industry to make smoked tobacco obsolete by 2030, with smokers quitting or moving to reduced risk products like e-cigarettes. Further proposals for moving towards a smoke-free 2030 will be set out at a later date.
This goal is extremely challenging. Although smoking rates are falling overall, they remain stubbornly high in certain groups, including:
-
in areas of deprivation. In Blackpool, 1 in 4 pregnant women smoke. In Westminster, it’s 1 in 50.[footnote 48] Rates are also higher among manual workers and social renters[footnote 49]
-
among people who identify as LGBT[footnote 50]
-
among people living with mental health conditions. A joint report from the Royal College of Physicians and the Royal College of Psychiatrists suggests that 1 in 3 cigarettes in England are smoked by somebody with poor mental health[footnote 51]
Tackling these inequalities is the core challenge in the years ahead. If we are to achieve this vision of a smoke-free future, we need bold action to both discourage people from starting in the first place, and to support smokers to quit.
Case study: Salford ‘Swap to Stop’
Social housing tenants are much more likely to smoke: 30% of adults in the social rented sector are estimated to be smokers, double the national average.
As part of comprehensive local action on smoking, Salford city council worked with a local housing association, stop smoking service, pharmacies and a registered vape shop on the Salford ‘Swap to Stop’ project, aimed at social housing and privately rented tenants in some of the most deprived areas in the city. A free e-cigarette starter-pack was given as well as behavioural support to quit smoking. Demand was high: over 1,000 smokers were recruited in 10 weeks, of whom 20% quit smoking altogether.
Discouraging people from starting
Two in 3 people who experiment with smoking go on to become smokers. Discouraging young people from trying cigarettes is an important priority.[footnote 53] In 2007 the government raised the age of sale for tobacco from 16 to 18. This helped contribute to lower teenage smoking rates, and forms part of wider government action to deter people from starting in the first place, including bans on:
- television advertising (1985)
- printed advertising (2003)
- sponsorship (2005)
Supporting smokers to quit
Help to quit is mostly delivered by the NHS or local authorities, paid for through general taxation. Given the pressure on local budgets, the government is considering other ways of ensuring people can get the help they need.
Other countries, such as France and the USA, have taken a ‘polluter pays’ approach requiring tobacco companies to pay towards the cost of tobacco control. We’re also open to other ideas for funding, including proposals to raise funds under the Health Act 2006.
We would aim to use any funds to focus stop-smoking support on those groups most in need, such as pregnant women, social renters, people living in mental health institutions, and those in deprived communities; and to crack down on the illicit tobacco market by improving trading standards enforcement.
We also believe that there could be a positive role for inserts in tobacco products giving quitting advice and will consider this as part of our review of tobacco legislation once we leave the European Union.
The government is committed to monitoring the safety, uptake, impact and effectiveness of e-cigarettes and to assess further innovative ways to deliver nicotine with less harm than smoking tobacco. There is a large amount of research now available to support e-cigarette use as a safer alternative to smoking and help people quit smoking, and we continue to monitor the evidence. There are also claims that heated tobacco products could be less harmful than smoking and help smokers quit. Heated tobacco products are relatively new to the UK market in comparison with e-cigarettes, and research is in its infancy and mainly led by the tobacco industry.
The latest evidence on heated tobacco (given by the independent Committee on Toxicity in December 2017 and in the February 2018 PHE evidence review)[footnote 54] stated that heated tobacco products still pose harm to users, but may be less harmful than smoking conventional cigarettes. Information on the impact on health is very limited and we recommend that smokers quit completely rather than move to these products.
As part of our commitment to evaluate the evidence on new products, we will run a call for independent evidence to assess further how effective heated tobacco products are, or are not, in helping people quit smoking and reducing health harms from smoking. We’ll keep the evidence on e-cigarettes under review.
Maintaining a healthy weight
For other areas, the trend is going in the wrong direction – with only a third of adults a healthy weight. Since 1993, rates of adult obesity have almost doubled (to 29%), and morbid obesity has quadrupled (to 4%)[footnote 55]. One in 3 children aged 10 to 11 are now overweight or obese and we know that obese children are 5 times more likely to become obese adults.[footnote 56]
Figure 7: Obesity – the scale of the problem[footnote 57]
Nearly 1 in 4 reception age children are overweight or obese; 1 in 3 Year 6 children are overweight or obese; 2 in 3 adults are overweight or obese
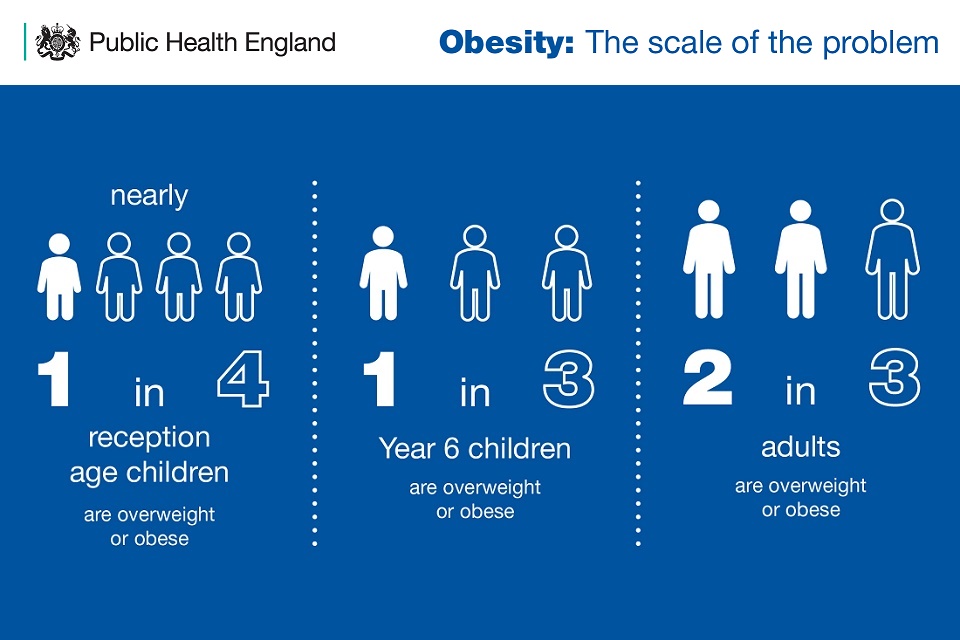
This is storing up health problems for the future, and is a cause for serious concern. This is because being overweight or obese is a major risk factor for a number of conditions, including diabetes, heart disease and stroke, and some cancers.[footnote 58] Improving our diet is one of the biggest health-related actions we can take to improve the health of the nation.[footnote 59]
Eating a healthy diet
As a country, we need to eat more fruit, vegetables, fibre and oily fish. We consume too many calories, as well as too much sugar, saturated fat and salt.[footnote 60] We know it can be difficult to eat healthily when unhealthy options are all around us. That’s why our focus must be on making healthier choices easier. This is not nannying, but reshaping the environment to provide people with more choice, not less.
We have demonstrated through our childhood obesity plan our commitment to take bold action. That’s why our plan for reducing childhood obesity by 50% by 2030 has focused on making the food and drink available to families healthier.
Energy drinks are soft drinks that are typically distinguished by their significantly higher caffeine content. Although diet versions are available, regular energy drinks on average contain more calories and sugar than other regular soft drinks.
Research has suggested that excessive consumption of energy drinks by children may affect some children adversely. In addition, energy drink consumption has also been associated with unhealthy behaviours and deprivation.
Last year we consulted on ending the sale of energy drinks to children. The consultation showed overwhelming public support, with 93% of consultation respondents agreeing that businesses should be prohibited from selling these drinks to children. Teachers and health professionals, in particular, were strong in their support for the government to take action.
Therefore, we can now announce that the government will end the sale of energy drinks to children under the age of 16.
We will be setting out the full policy in our consultation response shortly.
We have also consulted on making calorie labelling mandatory in the out-of-home sector, such as restaurants, takeaways and cafes. We will be setting out details of our policy in a consultation response shortly. In addition, we set out our intention to, and consulted on, banning promotions of foods and drinks high in fat, sugar and salt (HFSS) by price and by location. We have also consulted on introducing a 9pm watershed on TV advertising of HFSS products and similar protection for children viewing adverts online. We will be setting out the government’s response and next steps on both policies as soon as possible.
In Chapter 2 of our childhood obesity plan, we committed to deliver a Childhood Obesity Trailblazer Programme in partnership with the Local Government Association and PHE, working with local authorities to test the boundaries of their levers through innovative local action to tackle childhood obesity. Where we live has a huge role to play in tackling childhood obesity, whether it is the way our towns and cities are designed to ensure greater active travel or safe physical activity, or how many hot food takeaways can operate near schools. While local authorities have a range of powers to support local solutions to address childhood obesity, many face challenges. We want to make sure that all local authorities are empowered and confident in finding what works for them to tackle childhood obesity.
We have now selected 5 successful Childhood Obesity Trailblazer authorities, who together will have access to £1.5 million of funding and support over the next 3 years. They are: Blackburn with Darwen, Birmingham, Bradford, Lewisham and Nottinghamshire. Across the 5 areas, Trailblazer activity will support and create opportunities for future generations, from supporting families and children in the early years through to upskilling adolescents and young adults. Between them, they will test the potential for existing local levers to:
- restrict out-of-home HFSS advertising
- create healthier food environments through the planning system
- use community and faith assets
- incentivise businesses to improve their retail offer
- improve accessibility and affordability of healthier foods
- improve job opportunities and growth in health, food and physical activity sectors
This will help to inform further action the government can take in the future to enable ambitious local action. We will also share the learning from the programme to encourage and empower wider local action across the country.
While we know this represents a world-leading approach, we have always been clear that we need to go further and faster in ensuring everyone has a chance to lead a healthier life.
That’s why we’re publishing Chapter 3 of the childhood obesity plan as part of this green paper.
This sets out our plans for: infant feeding, clear labelling, food reformulation improving the nutritional content of foods, and support for individuals to achieve and maintain a healthier weight.
Infant feeding
To support families, it’s important to understand the choices they make when it comes to infant feeding. In England, most mums start breastfeeding. However, after 6 to 8 weeks, only 4 in 10 are still breastfeeding their babies.[footnote 61] The UK has one of the lowest breastfeeding rates in the world.[footnote 62]
Given the benefits of breastfeeding, we intend to commission an infant feeding survey to provide information on breastfeeding and the use of foods and drinks other than breastmilk in infancy. This will also provide the means to assess the impact of the actions we are taking on infant feeding which are outlined below.
Currently 18% of boys and 21% of girls aged 2 to 4 years are overweight or obese.[footnote 63] Therefore, we need to look at what we can do in the early years to help give children the healthiest start in life.
We know that 3 in 4 children aged 4 to 18 months have energy intakes that exceed their daily requirements.[footnote 64] This figure increases with age following the introduction of solids. Data shows that sugar levels in some commercial baby foods and drinks can be very high.[footnote 65] Around 9 in 10 children aged 1.5 to 3 years old exceed recommended daily sugar intake levels.[footnote 66] Consuming too much sugar, and too many foods and drinks high in sugar can lead to weight gain, which in turn increases the risk of heart disease, type 2 diabetes, stroke and some cancers in adulthood.[footnote 67] Added sugar in foods can have a negative effect on babies and young children’s health by putting them on this trajectory.[footnote 68]
High levels of sugar intake also increase the risk of tooth decay.[footnote 69] Just under a quarter of 5-year-olds in England have tooth decay[footnote 70] and almost 9 out of 10 hospital tooth extractions among children aged 0 to 5 could have been avoided.[footnote 71]
Because of this, we will challenge businesses to improve the nutritional content of commercially available baby food and drinks. PHE will publish guidelines for industry in early 2020.
Industry’s progress will be monitored and reported to the government. If insufficient progress is made, the government will consider other levers. PHE will also explore including baby food within the popular Change4Life Food Scanner app to help parents and carers make healthier choices for their infants.
Parents and carers want to know more about the nutritional value of the food and drink they buy for their families. This is particularly important in the early years, when parents and carers buying products marketed for infants and young children are making decisions about when and what to feed their baby.
Too many commercially available foods and drinks marketed for infants and young children have labels that do not align with the latest government scientific advice. They can also make a product appear healthier than it really is, or do not contain enough information about how they should be consumed.[footnote 72] All of this can be confusing to parents and carers.
We will therefore explore how we can improve the marketing and labelling of infant food. This is so that parents and carers have honest and accurate information on the products they feed their babies at this critical stage of life. We will seek views on how we do this.
Clear labelling
It’s important that everyone, regardless of their age, has access to the information they need to make informed decisions. But we know that identifying what food and drinks are healthy is not always easy. To support consumers in making healthier food and drink choices through labelling, we believe that people need 2 things:
- to know what’s in the food they’re buying
- for this information to be presented clearly and concisely, helping them to make quick, informed decisions about what to buy
Since 2013, the UK has led the way in recommending a voluntary nutritional labelling scheme, sometimes called ‘traffic light’ labelling. This uses colours, words and numbers to help UK consumers understand the amount of fat, saturated fat, sugar, salt and calories in a product. This scheme was the result of over 15 years of research to provide a label that meets the needs of UK shoppers.
As a nation, we’re proud of the success of this scheme. Front-of-pack labels feature on a significant proportion of pre-packaged food and drinks, and 9 in 10 shoppers agree it helps them make informed decisions when shopping.[footnote 73] We want to do more to ensure that our label still meets the needs of UK shoppers and that wherever people shop and whatever they buy they are presented with consistent front-of-pack nutritional labelling that they find helpful and easy to understand.
Since we introduced the UK scheme, a number of other countries around the world have introduced their own versions of front-of-pack nutrition labels. Some labels are similar to the UK approach, but many differ. For example, some countries like Sweden, Denmark and Norway choose to focus on signposting the healthier aspects of foods such as high fibre, while Chile chooses to alert shoppers to products that are high in nutrients such as fat, calories, salt and sugar that eaten in excess can be harmful to health.
We have previously committed in both Chapter 1 and Chapter 2 of the Childhood Obesity Plan to explore what additional opportunities leaving the European Union presents for front-of-pack food labelling in England.
As part of exploring this we will consult by the end of 2019 on how we can build on the successes of our current front-of-pack nutritional labelling scheme once we have left the European Union.
Our consultation will consider the evidence underpinning these many different forms of front-of-pack labelling. It will focus on ensuring that the UK continues to be world-leading in providing UK shoppers with simple nutritional information that they need to make healthier decisions, while taking into account the UK’s ambitions for trade once we have left the European Union.
Improving the nutritional content of food and drink
Central to our approach to improving diets is working with food and drink companies to make their products healthier. We often call this reformulation. Over time, these small changes can add up to big improvements in the nation’s health.
The Soft Drinks Industry Levy (SDIL) has been hugely successful in removing the equivalent of over 45,000 tonnes of sugar from our shelves. So far, we have not included sugary milk drinks within this ‘tax’. However, these drinks can also contribute to our sugar and calorie intakes, particularly given some of the larger portion sizes available.
Therefore, if the evidence shows that industry has not made enough progress on reducing sugar, we may extend the SDIL to sugary milk drinks.
We also need to do more to consume less salt. This is vital for reducing the risk of heart disease and stroke.[footnote 74] The government recommends that we should consume no more than 6g per day, well below the current average in England (8g per day).[footnote 75] This is mostly through salt that is already in the food we buy, rather than the salt we might add ourselves.
Case study: Salt reduction
Voluntary salt reduction targets for particular types of food were set for industry in 2014, building on 3 earlier sets of voluntary targets (in 2006, 2008 and 2011). These aimed to gradually reduce the levels of salt in the foods that contribute most salt to our diet.
PHE’s 2018 report showed that 81% of products were meeting the targets for 2017. Businesses achieving reductions include McCain Foods (GB) Ltd who have reduced the amount of added salt in their products by 22% since 2001, while Mars Food have reported an average reduction in salt of 30% since 2007 across their Dolmio and Uncle Ben’s cooking sauces, as part of meeting the 2017 targets across their products.
Our ambition is to reduce the population’s salt intakes to 7g per day.
To achieve this, we will publish revised salt reduction targets in 2020 for industry to achieve by mid-2023 and we will report on industry’s progress in 2024. Influencing consumer behaviour through marketing and providing advice, including within the NHS, will also help. We will keep all options open if a voluntary approach does not demonstrate enough progress by 2024. We will commission a urinary sodium survey in 2023 to measure progress towards the ambition and understand how much salt individuals are consuming.
Developments in food technology also offer opportunities to improve the nutritional content of food and drink in order to improve people’s health. For example, it is already possible to enrich eggs or milk with omega 3. Government will continue to examine the growing evidence in this area.
Support for individuals to achieve and maintain a healthier weight
We want to make it as easy as possible for people of all ages who want to lose weight to access the support they need. Access to the right services can help people achieve a healthier weight and reduce the cost to the NHS and public services further down the line.
Evidence shows that patients are receptive to brief interventions for obesity.[footnote 77] On average, they lose weight in the year following the intervention. Being able to deliver a brief intervention and provide opportunistic advice in a primary care setting presents an effective way for doctors to engage with obese patients about weight management and lifestyle.
We will work with NHS England to develop approaches to improve the quality of brief advice given on health issues, including weight management, in general practice. We will also explore the use of quality improvement approaches, and test any new, innovative proposals through the new NHS Primary Care Network Testbeds, as appropriate.
As more services go online, we will drive the digital market for weight management apps; helping health professionals to offer patients support in new, innovative ways that fit with how they live their lives.
We will work with NHS England, PHE and NHSX to review the current digital weight management offer on the NHS Apps Library, and promote the app marketplace to encourage the availability of more products and services.
We will also continue to develop Our Family Health, a digital approach to support families with children aged 4 to 7 years with lifestyle behaviour change. We will work with local authorities to explore how Our Family Health can support families living in some of our most deprived areas with high childhood obesity rates.
Every year, the National Child Measurement Programme (NCMP) measures the height and weight of over 1 million children aged 4 to 5 and 10 to 11 in state schools across England.[footnote 78]
The programme provides key opportunities for parents to be informed of their child’s weight status and to access support from health professionals and local services, where appropriate. However, there is currently no standard route to share this vital information with healthcare professionals; for example, through the health and care record. As such, it’s not done routinely.
Case study: Children’s weight services in Essex
Livewell Child is a local initiative led by Braintree District Council that is all about supporting children and families to eat well, keep active and feel good. Following the start of the programme in 2016, there has been 1.2% decrease in the number of overweight pupils in year 6 between 2016 to 2017 and 2017 to 2018 across the schools taking part in the Livewell Child programme. This contrasts with an increase in the number of pupils who were overweight in schools in Braintree that did not take part in the programme. Key to this approach has been the development of a lasting and trusted relationship with the 10 pilot schools, which has been built over the last 2 years.
To better enable families identified through the NCMP to access support, PHE will work with NHS England and NHS Digital to explore how NCMP data can be shared directly with digital child health records and presented appropriately so that it’s consistently accessible for both parents, carers and health professionals.
We will also explore how to embed Our Family Health within the NCMP, so that more families are getting the help they need.
We will also look to the latest behavioural science to understand how we can best communicate with parents and health professionals on obesity.
Staying active
Becoming more active is good for our mental and physical health, and reduces our risk of developing a number of health conditions. For example, regular activity can reduce our risk of hip fractures by 68%, type 2 diabetes by 40%, heart disease by 35%, and depression by 30%.[footnote 79]
It can also help us keep the weight off after a (diet-led) weight-loss programme. It can also help the third of people who are already a healthy weight to stay that way.[footnote 80] This has led some experts to suggest:
If physical activity were a drug, we’d talk about it as a miracle cure.
Professor Dame Sally Davies, Chief Medical Officer for England and Chief Medical Adviser to the UK government (2017)[footnote 81]
Case study: Grassroots football
The Football Association’s report on The Social and Economic Value of Adult Grassroots Football in England found that participants report significantly higher levels of happiness and general health compared with people who play no sport. People in lower-income groups also experience greater health benefits from football than higher-income groups.
Despite this evidence, many of us are not active enough to ensure we’ll remain healthy and independent for as long as possible: a third of adults do not meet guidelines of 150 plus minutes of aerobic activity a week;[footnote 83] and evidence suggests that the UK is less active than France, the Netherlands and Australia, and has twice the level of inactivity seen in Finland.[footnote 84]
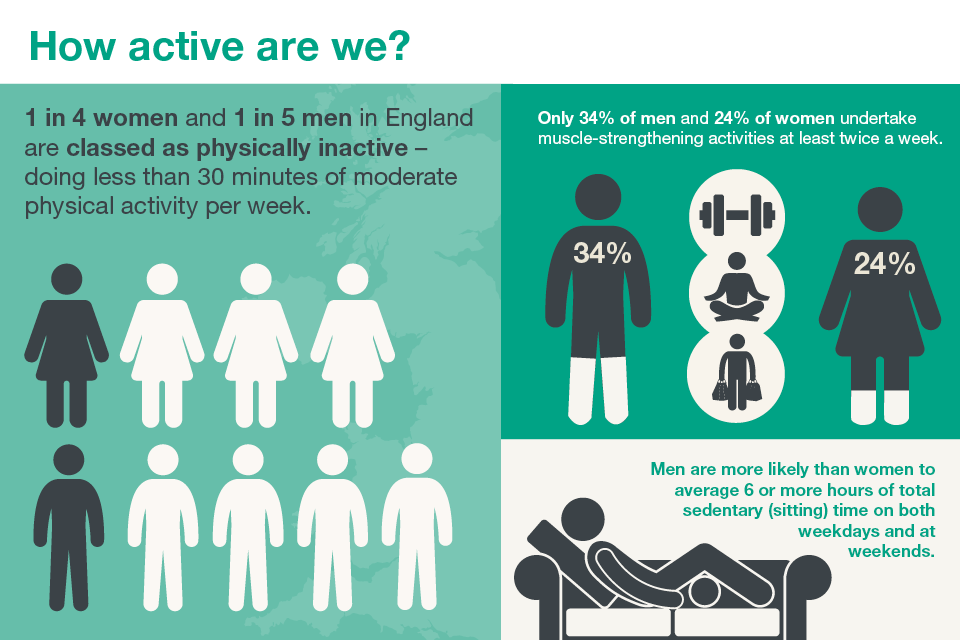
Figure 8: How active are we?[footnote 85]
1 in 4 women and 1 in 5 men are classed as physically inactive - doing less than 30 minutes of moderate physical activity per week. Only 34% of men and 24% of women undertake muscle-strengthening activities at least twice a week. Men are more likely than women to average 6 or more hours of total sedentary (sitting) time on both weekdays and at weekends.
The UK Chief Medical Officers have published guidelines that clearly state the amount of activity required for good health. One of the easiest ways to get active is to build physical activity into your daily commute to work or school. Walking and cycling are 2 of the top ways that people in England keep physically active[footnote 86] and are the most accessible and cheapest forms of transport.
Given the importance of physical activity we’ve asked the UK Chief Medical Officers to review the current guidelines. New guidelines will be published in September 2019.
The guidance states that all adults should aim to be active every day. This should include muscle-strengthening activity – such as exercising with weights, yoga or carrying heavy shopping – on at least 2 days a week. These types of activity are particularly important for people in or approaching later life. This is also the case for balance exercises, which are recommended twice a week for older people at risk of falls. Yet rates of strength and balance activity are particularly low, with just 1 in 4 women (and 1 in 3 men) meeting the recommended guidelines.[footnote 87]
We will work with partners to launch a new ‘digital design challenge’ for strength and balance exercises.
This will ask ‘how can we use digital to support the public to do regular activities to increase their strength and balance?’. The challenge will be focused on:
- older people
- those living with health conditions already
- people on low income, in deprived areas
The final product or service should be free to use and available across England. The design challenge will be launched in the autumn.
Physical activity can also help those living with a health condition to keep symptoms under control, and to prevent additional conditions from developing.[footnote 88] Yet we know that getting more active can be daunting, especially if you haven’t done much exercise before or you’re managing a health condition. In the 2020s, we want to get everybody active, including those of us who are already living with a health condition.
To support this, we are launching a second phase of the national Moving Healthcare Professionals partnership programme led by PHE and Sport England, which supports healthcare professionals to promote physical activity to their patients.
We will work with the UK’s leading health charities and Sport England to support the launch of a new physical activity campaign, which seeks to empower and inspire those living with health conditions to be more active. The campaign will be launched later this year and is supported by PHE.
We will also be working across government to encourage:
- local authority planning decisions to promote active lifestyles
- more people to switch from driving to public transport, cycling and walking – especially on the school run
- nurseries to build opportunities into their daily routine for physical activity such as energetic play, walking and skipping (pdf, 232 KB)
- strengthening the evidence base about the social and economic value of physical activity
Taking care of our mental health
Good health is much more than the absence of illness. It’s a state of wellbeing that includes our mental as well as our physical health. Parity of esteem was enshrined in law back in 2012. This requires the NHS and local authorities to consider the ‘whole person’, and their mental and physical health needs as equally important.
This government has provided people with greater access to mental health services.[footnote 90] And, in doing so, we began to close the ‘treatment gap’ between mental and physical health:
-
We are spending more on mental health services. The NHS Long Term Plan commits at least a further £2.3 billion a year by 2023 to 2024.[footnote 91]
-
One million people now have access to psychological therapies for common mental health problems.[footnote 92] The Long Term Plan promises to treat an extra 380,000 per year.
-
An additional 24,000 women per year will benefit from increased access to perinatal mental health care by 2023 to 2024, in addition to the extra 30,000 women getting specialist help by 2020 to 2021.[footnote 93]
-
At least 345,000 more children and young people will have access to mental health support including via new mental health teams in schools.[footnote 94]
We now need to close the ‘prevention gap’ and achieve parity of esteem, not just for how conditions are treated, but also for how they are prevented. When it comes to preventing health problems, much of our focus is still on people’s physical health. Less attention is given to the steps we can take to improve our mental health and wider sense of wellbeing. This is despite our physical and mental health being closely related – physical health problems increase the risk of poor mental health, and vice versa.[footnote 95]
Tackling risk factors and strengthening protective factors
We need to lay the foundations for good mental health across all parts of our society. This is because the circumstances we’re born into – and the conditions in which we live – all have a major bearing on our mental health. We need to take urgent action to tackle the risk factors that can lead to poor mental health, such as adverse childhood events, violence, poverty, problem debt, housing insecurity, social isolation, bullying and discrimination. We also need to invest in the protective factors that can act as a strong foundation for good mental health throughout our lives, such as strong attachments in childhood, living in a safe and secure home, access to good quality green spaces, security of income, and a strong set of social connections.[footnote 96] These will be considered in the next chapter.
Mental health problems can have a broader impact on society. Poor mental health at work costs the UK economy between £74 billion and £99 billion per year.[footnote 97] Mental ill-health is also associated with lower life expectancy, with some conditions associated with reductions in life expectancy of 10 to 20 years.[footnote 98]
Case study: Prevention Concordat for Better Mental Health for All and Thrive Bristol
The Prevention Concordat for Better Mental Health for All brings together a wide range of organisations that have committed to preventing mental health problems and promoting good mental health. The organisations that join the Concordat agree to work together to take local and national action to achieve the aim of better mental health for all.
‘Thrive Bristol’ is an example of the action taken by a signatory of the Prevention Concordat, Bristol City Council. It is a 10-year programme to improve the mental health and wellbeing of everyone in Bristol, with a focus on addressing inequality.
Thrive Bristol focuses on prevention of mental ill-health and early intervention. It aims to work with public services, businesses, charities and others, taking advantage of everything that is already available across the city to support mental health. Its ambitions include: creating a city free from mental health stigma and discrimination, maximising people’s potential, building a healthy and happy workforce and becoming a suicide safe city.
Twenty-five employers in the city – from senior corporate lawyers to city farm managers – have already committed to improve mental wellbeing in workplaces. In addition, some employers have signed up to the Time to Change Employer Pledge and are developing action plans for better mental health at work, including training on mental health and suicide prevention.
Taking action
There are actions we can take to improve our mental health. Many people know how to improve their physical health but are less confident taking positive action for their mental health and wellbeing. We want to create a society where people have high mental health ‘literacy’. Where everyone has the skills, knowledge and confidence to improve their mental health and wellbeing throughout life. We also want to raise awareness of mental health and wellbeing, so that everyone can recognise signs of distress in themselves and others and know where to seek help if needed.
The government has already published the green paper, Transforming Children and Young People’s Mental Health Provision, and made mental health a mandatory part of the school curriculum. Together, these amount to a transformation in how schools are supported to promote good mental health in their pupils and refer them for support when there are signs of illness.
DHSC will take additional actions, including:
-
Providing advice for children and young people on dealing with difficult emotions and situations that can lead to problems such as stress, bullying and self-harm, through the Rise Above programme in schools and online.
-
Encouraging all local authority areas to put in place mental health promotion plans and to sign up to the Prevention Concordat for Better Mental Health for All, building on the momentum of local authority suicide prevention plans.
-
Investing up to £600,000 in sector-led improvements to support local authorities to strengthen their suicide prevention plans and implement the recommendations identified by an independent evaluation of local plans.
-
Providing £1 million for the Office for Students to run a competition that will drive innovation in the way university students are supported with their mental health, including digital solutions.
-
Building on past work to address mental health stigma, we’re now taking the next step to support public action. We will launch the Every Mind Matters campaign nationally in October 2019 with the goal of making 1 million adults better informed and equipped to look after their mental health and support others. The campaign will include a new tool that asks a series of questions and then recommends simple, personalised actions to improve individuals’ mental health.
-
From 2020, the campaign will also include advice to parents on supporting their children’s mental health and wellbeing, which, for example, could include information on subjects such as stress, screen time, online bullying, body image and self-harm. This advice will complement and signpost parents to existing sources of support on self-harm.
These actions will be supported by wider efforts across other parts of government:
-
The government will establish a statutory Breathing Space scheme to provide respite to those in problem debt while they seek support – with regulations laid before the end of the year. This will include specific access arrangements for those receiving mental health crisis treatment.
-
Every school has to protect its pupils from harm and provide support for pupils with mental and physical health issues. The Department for Education will revise statutory guidance to make sure that schools understand how mental health is embedded in existing requirements so that they ensure staff can identify and support children with mental health issues and how this can be delivered within whole school approaches to mental wellbeing led by senior mental health leads.
-
The Department for Education will also be developing training for all new teachers on how to spot the signs of mental health issues, backed up by updated statutory guidance to make clear schools’ responsibilities to protect children’s mental wellbeing. We will also be updating professional standards for social workers across England to increase their knowledge and skills when helping those with mental health issues.
-
The Department for Education is introducing a requirement for all schools to teach about mental health and wellbeing, as part of compulsory Relationships Education for all primary pupils, Relationships and Sex Education (RSE) for all secondary pupils and Health Education for primary and secondary pupils in state-funded schools. Schools will be encouraged to teach the new subjects from September 2019 and required to teach them from September 2020
-
As part of its support for high-quality teaching of the new subjects, the Department for Education will put in place additional support to ensure schools have easy access to world class interventions, training and materials on mental health.
We also know that in the most deprived areas of England, people tend to have the poorest health and significantly less green space than wealthier areas.[footnote 99] Evidence shows that spending time in the natural environment can improve our mental health and wellbeing,[footnote 100] so in the 25 Year Environment Plan, published in 2018, the government sets out its aim to connect people more systematically with green space to improve mental health, using the natural environment as a resource for preventative and therapeutic purposes.
We want to embed nature-based interventions as part of strategies for preventing and treating mental ill-health.
The government is committed to helping more people connect with nature to support their health and wellbeing, as set out in the 25 Year Environment Plan. We will explore the potential to launch a programme in 2020 to protect and improve people’s mental health and wellbeing by connecting them to nature-based activities through social prescribing and the broader comprehensive model of personalised care.
The Department for Environment, Food and Rural Affairs is working with PHE, NHS England and Natural England to understand current practice in nature-based social prescribing and learn how the uptake of nature-based interventions can be improved, working in 8 localities in England. We would like this work to underpin an innovative follow-on programme that will help to enable the appropriate referral of people with mild-moderate mental health needs, or at risk of poor mental health, to local nature-based activities.
Wider factors
Of course, factors other than weight, smoking and resilience matter. For example, we know that problem gambling can have a major impact on health.[footnote 101] The government has an active agenda on this, which is set out elsewhere. Other factors include alcohol, drug use and sleep.
Alcohol
Most people who drink, do so responsibly. Looking at the data, we also know that overall consumption in England is falling, particularly among younger people.[footnote 102] Despite this good news, the harm caused by problem drinking is rising.[footnote 103]
Over 10 million people are drinking at levels above the official guidelines and putting themselves at extra risk. The heaviest drinkers make up just 4% of the overall population, yet account for 30% of all units of alcohol consumed.[footnote 104] In England, drinking at increased and higher risks of harm is twice as common among men (28%) than women (14%).[footnote 105] The impact of harmful drinking and alcohol dependence for a given level of consumption is also much greater for those in the lowest income bracket.[footnote 106]
The government has been working to reduce the harm from problem drinking by:
-
ensuring people are aware of the health risks through the One You campaign
-
including an alcohol risk assessment in the NHS Health Check
-
a £6 million investment to support children with alcohol dependent parents
Case study: Improving the lives of families affected by alcohol
PHE estimate that 200,000 children in England are growing up living with a parent who is dependent on alcohol. These children are at greater risk of harm, including neglect and maltreatment.
The government launched a £6 million 3-year programme to improve outcomes for these very vulnerable children in April 2018. This includes PHE working with 9 areas to explore how to reduce harm: testing innovative ways of finding and supporting children of parents dependent on alcohol. Funding of £4.5 million – provided by DHSC and the Department for Work and Pensions – is allowing these areas to test new ideas and improve services to better meet the needs of children and parents where there is an alcohol problem in the family. This includes:
- making sure schools and other services are aware of alcohol dependency and the problems it can cause
- closer working between alcohol treatment and children’s services
- working with families to reduce conflict between parents and help families deal with challenges more easily, and providing support for children and young people
There will be an independent evaluation to identify what we can learn from the programme. This will be published in 2021 to 2022.
Making alcohol-free and low-alcohol products more available would help to nudge the general drinking population towards lower strength alternatives. This is already the direction of travel, but we want to go further and faster:
-
we will work with industry to deliver a significant increase in the availability of alcohol-free and low-alcohol products by 2025
-
in order to support further innovation in the sector and encourage people to move towards alcohol-free products, we will review the evidence to consider increasing the alcohol-free descriptor threshold from 0.05% abv up to 0.5% abv in line with some other countries in Europe
Drug use
Drug misuse or dependency is associated with a range of harms including poor physical and mental health, unemployment, homelessness, family breakdown and criminal activity. The health of children, family members and carers can also be affected. Heroin and cocaine are associated with the majority of social costs associated with drug misuse and heroin dependence continues to be the common drug problem treated in England.[footnote 107]
The USA and Canada are in the grip of an opioid epidemic, with the numbers of opioid-related deaths having increased drastically in recent years.[footnote 108] Although there are key differences between the UK and the USA, the risk of a similar epidemic happening here is a real one and the experience of the USA demonstrates the importance of being prepared. Mitigation of the threat posed by illicit synthetic opioids includes work on early prevention to build resilience among young people. Especially important is ensuring the continuation of easy to access opioid substitution treatment with a reach into communities where there is a higher risk of dependence forming, as well as increasing the availability of naloxone (the opioid overdose antidote). Investing in drug treatment reduces mortality risk, improves quality of life and saves money. Estimates suggest every £1 spent on drug treatment is associated with a benefit to society of £4, increasing to £21 over 10 years.[footnote 109]
Once PHE’s review of Prescribed Medicines has been published, DHSC will work with the Home Office, PHE and other partners to undertake further policy development around issues related to prescribed and illicit opioid use, including considering opportunities to overcome barriers within the current system and promote the spread of good practice, as highlighted by a recent high-level roundtable on opioids convened by the Chief Medical Officer for England and Deputy National Security Adviser.
DHSC, working with a range of partners including the recently appointed Recovery Champion, will develop a shared understanding of the current challenges facing the substance misuse treatment and recovery workforce.
DHSC will assess the adequacy of responses to cannabis and related mental health problems and develop and implement an action plan, in relation to:
-
treatment for heavy cannabis users and people experiencing significant mental health problems
-
brief interventions for other cannabis users
-
initiatives aimed at raising awareness of cannabis-related harms.
Sleep
A topic that has received relatively little policy attention is sleep. There’s growing evidence on the health impacts of lack of sleep. Insufficient or poor quality sleep is associated with physical and mental health problems, including: increased risk of obesity, strokes and heart attacks, and depression and anxiety.[footnote 110] Lack of sleep may also have a negative impact on somebody’s recovery from illness or surgery.[footnote 111] Despite this, over one-third of hospital patients report being bothered by noise created by other patients. One in 5 report being bothered by noise created by staff.[footnote 112] However, it should be noted that the direction of causality is likely to run in both directions – with poor sleep leading to health problems, and health problems leading to poor sleep.[footnote 113]
Individuals, employers, schools, the NHS, local authorities and national government all have a role to play in helping support healthy sleeping. There are many examples of good practice. However, with some estimates suggesting up to three-quarters of adults in the UK regularly sleeping less than 7 hours per night, there’s much more left to achieve.[footnote 114]
As a first step, the government will review the evidence on sleep and health. This is with a view to informing the case for clear national guidance on the daily recommended hours of sleep for individuals in different age brackets, and to raise awareness of the key ‘sleep hygiene’ factors that can support healthy sleeping.
The NHS will also determine what more can be done to ensure those in care settings are getting the amount of rest that they need. This will include an assessment of whether changes are needed to existing guidance (such as national roll-out of ‘protected sleep time’ in hospitals, where staff leave patients sleeping unless clinically necessary).
Prevention in the NHS
If we are to achieve our mission, we need everybody’s help in preventing health problems from arising – including from those who are normally used to treating them. In its Long Term Plan, the NHS devoted a whole chapter to ‘prevention’.[footnote 115] Commitments include:
- obesity – the NHS will fund a doubling of the NHS Diabetes Prevention Programme over the next 5 years, and provide access to weight management services in primary care for people with diabetes or hypertension with a BMI of 30 plus
- smoking – by 2023 to 2024, all people admitted to hospital who smoke will be offered NHS-funded tobacco treatment services, including a new smoke-free pregnancy pathway for expectant mothers and their partners. A new smoking cessation offer will also be available as part of specialist mental health and learning disability services for long-term users
- alcohol – over the next 5 years, alcohol care teams will be fully established in those hospitals with the highest rates of alcohol dependence-related admissions
- inequalities – the NHS will set out specific, measurable goals for narrowing inequalities, including those relating to poverty, through the service improvements set out in the plan
Case study: Healthier You: The NHS Diabetes Prevention Programme
Five million people in England are at high risk of developing type 2 diabetes. If current trends continue, 1 in 3 people will be obese by 2034 and 1 in 10 will develop type 2 diabetes. NHS England, PHE and Diabetes UK joined forces in 2016 to launch the Healthier You NHS Diabetes Prevention Programme which provides advice on healthy eating, being more active and managing weight to those at high risk. In 2018 to 2019 the programme achieved full national coverage, becoming the first country-wide prevention programme in the world.
To date over 400,000 people have been referred to the NHS Diabetes Prevention Programme. The early findings show the programme has exceeded expectations with patients losing an average of 3.4kg, 1 kilogram more than originally predicted. Just under half of those signing up are men – a much higher proportion than typically attend weight loss programmes. Roughly a quarter are from black, Asian and minority ethnic communities – groups that are at significantly greater risk of developing type 2 diabetes.
Harry was diagnosed by his GP as being pre-diabetic and borderline obese when he was 56. Harry decided to take action, to review his sedentary and slow-paced lifestyle, and lost over 3 stone after being referred to the NHS Diabetes Prevention Programme. Harry said:
“The prevention programme has changed my life. Since I started it, I’ve gone through at least 3 different clothing sizes and from a waist 42 to a 28. Above and beyond the weight loss – I’m healthier and I’m happier”.
The next step is to move from a national treatment service (focused on illness) to a national ‘wellness’ service (focused on creating good health). This involves helping people to help themselves. We will make this vision a reality by:
- allowing people to connect their own data into the whole record if they choose
- giving people personalised advice based on aggregated data
- giving people the tools and motivation to make informed choices
The NHS is already working to give more people control of their care. For example, their Comprehensive Model for Personalised Care will support up to 2.5 million to benefit from personalised care by 2023 to 2024 (including 900,000 people receiving a social prescription referral and 200,000 personal health budgets).[footnote 117]
Social prescribing
Social prescribing is a way of GPs and other healthcare professionals referring people to ‘activities’ or services in their community instead of offering only medical solutions.
A new Social Prescribing Academy is being set up to help to champion social prescribing and support national plans to make it available throughout England. By 2020 to 2021, over 1,000 trained link workers will be recruited, so that over 900,000 people can benefit from social prescribing by 2023 to 2024.
The Social Prescribing Academy will help by brokering relationships across health, local government, justice, arts and culture, sport and the outdoors, and other sectors, to increase the range and availability of community-based activities and support that people can be connected to, including people living with dementia.
This is a strong start and will contribute towards us making the 2020s a decade of prevention. Further options to achieve scale and pace include:
- expanding the role of community pharmacists and other healthcare professionals to support more people in the community to manage and improve their health and wellbeing
- improving support options for people living with musculoskeletal conditions, and increasing the join-up across mental and physical health services
- strengthening links with councils, charities and other local players. Otherwise, the NHS will continue to be treating the symptoms of problems without influencing their causes
We are committed to delivering an expanded role for community pharmacies and want to see them become the first port of call for minor illness and health advice in England.
Government has now set out a Community Pharmacy Contractual Framework that, from October 2019, will redefine the integral role community pharmacies play in delivering healthcare over the next 5 years. This will see pharmacy staff trained to provide a wider range of health advice and support, including helping to identify and refer patients with unidentified health conditions, such as heart disease.
Over the course of the settlement period all pharmacies will become Healthy Living Pharmacies, which will require them to have trained health champions on site. These health champions will proactively deliver a wide range of lifestyle and health interventions to help more people live happier, healthier lives for longer.
We will commission more services from community pharmacies and support them to become further integrated into local NHS provider networks.
Chapter 3: Strong foundations
Good health is one of the country’s greatest assets. Just as we save for our retirement, we should be investing in our health throughout life – from early years, through to older age.
But we know that some people find this easier than others. Not because of innate differences in their decision-making, skills or values, but due to differences in the circumstances they are born into and the conditions in which they live.
We believe that everybody has the right to a solid foundation on which to build their health. Nowhere is this clearer than the early years.
The early years
We start building our health asset as a baby in the womb. The first 1,000 days of life are a critical time for brain development,[footnote 118] and parents and carers have a fundamental role to play in supporting their child’s early development. Most babies are born healthy and enjoy a safe and caring childhood that helps them develop. Some are born with a health condition or are raised in challenging circumstances, which can adversely affect their development. We know that a wide range of long-term outcomes are improved through the positive relationships established between parents and carers and their baby from pregnancy onwards.[footnote 119]
We are already working to make the NHS the safest place in the world to have a baby. In the last 5 years we’ve also seen improvements in school readiness, and a fall in the teenage smoking rate.[footnote 120] However, this progress has not been felt equally.[footnote 121] Children who live in more deprived areas are more likely to be exposed to avoidable risks and have poorer outcomes by the time they start school.[footnote 122]
Children are also affected by the wellbeing of their parent or primary carer. We need to recognise the impact that parental mental ill-health, parental drug and alcohol addiction and domestic abuse can have on a child’s life chances.[footnote 123] Providing timely and effective support to help parents overcome these issues, and fostering healthy and collaborative family relationships can have a positive impact on the health of both adult and child, and can help to overcome a cycle where some children grow up to repeat the harmful behaviours that they were exposed to in childhood. The £39 million Reducing Parental Conflict programme is working with councils across England to help them to integrate services and approaches that address parental conflict into their local services for families. With the right support and positive relationships, vulnerable children can thrive.
Because these challenges occur from birth onwards, it’s vital that families and their children who need extra support are identified early and receive tailored support. That way, we can prevent problems from arising in the first place, rather than dealing with the consequences.
We’re already working to provide families with the help they need through the Healthy Child Programme, the public health approach at the centre of our universal service for children and young people aged 0 to 19. This includes a set of health visits for 0 to 5-year-olds, and school nurse appointments for older children and some young people.
To support parents, we will modernise the Healthy Child Programme so it’s universal in reach and personalised in response.
This will enable effective, focused services where additional needs are identified; use of the latest evidence on effective practice; and help bring councils, the NHS and partners together to achieve priority outcomes for children and families.
We will modernise the programme by: making better linkages to other health records, including the digital red book; adding components including a digital support tool; and new pathways for speech and language development and pre-conception and pregnancy advice. We will also extend the upper age range of the programme (from 19 to 24-year-olds) for those young people needing extra support, and look to improve the way we support perinatal mental health and the healthy social and emotional development of babies and young children. We will seek views on this separately.
Speech, language and communication skills are an important indicator of children’s wellbeing. We know that a language-rich home learning environment is crucial to improving children’s life chances.[footnote 124] The government has launched a public-facing campaign Hungry Little Minds to improve the quality and quantity of parent-child interactions and make it easy for parents to adopt the positive behaviours we know will help their children to develop their communication, language and literacy skills. Health professionals have a key role to play in the success of the campaign and DHSC and PHE will work with the Department for Education to support them to play a full part in the campaign.
The government will continue to prioritise improving early speech and language outcomes as a preventative measure with strategic leadership across education, health and social care to narrow inequalities. If not addressed, we know that the long-term impact of language difficulties is likely to be high for individuals and families.[footnote 125] The government will also continue to work with local areas to support them to put in place joined-up strategies and services at local level that give children and families the support they need.
Children’s oral health
To give our children a good start in life, we need to do much better on oral health. Tooth decay is the most common oral disease among children in England – affecting 1 in 4 children by the time they start school, and the most common reason for hospital admission for children aged 5 to 9 years old – yet it is largely preventable.[footnote 126] Improving the oral health of children is a PHE priority, and a number of actions are already underway.
Case study: Leicester’s Healthy Teeth, Happy Smiles
In 2012, Leicester City Council had the highest prevalence of tooth decay in 5-year-olds across local authorities in England: 53%. It responded by prioritising help for preschool children as part of Leicester’s Healthy Teeth, Happy Smiles! programme. This evidence-based programme ensures that good tooth brushing behaviour with a fluoride toothpaste is established early in a child’s life and becomes part of their normal daily routine.
Almost 900 members of staff have been trained to deliver supervised tooth brushing with almost 9,000 children benefiting from daily supervised brushing. By 2017, the prevalence of tooth decay in Leicester had significantly reduced, to 39%.
There are 2 areas where the government is interested in going further and faster. Both are aimed at addressing the unwarranted variation in children’s oral health across the country. In 2016 to 2017, 1 in 6 children aged 5 had tooth decay in south-east England, compared with 1 in 3 in the North West. This variation is even greater between local authorities.[footnote 129]
We will consult on rolling out a school toothbrushing scheme in more pre-school settings and primary schools in England.
Evidence suggests that these programmes have the ability to reduce tooth decay, mitigate inequalities and establish lifelong behaviour to improve oral health. Half of all local authorities already have a version of the scheme in place, but they are not always focused on the children that would benefit the most. Next year, we’ll consult on proposals that will allow us to reach the most deprived 3 to 5-year-olds in all areas of the country. The aim would be to reach 30% by 2022.
We will explore ways of removing the funding barriers to fluoridating water to encourage more local areas that are interested to come forward with proposals. NHS England will actively seek partnerships between local authorities and the NHS, with councils rewarded for their fluoridation efforts by receiving a share of the savings from fewer child tooth fillings and extractions. This also includes examining the role that water companies can play in supporting fluoridation efforts.
Fluoride is a naturally occurring substance present in most water supplies, though typically at levels too low to improve dental health. It has a protective effect on teeth that lessens the impact of diets high in sugar and poor oral hygiene.
Six million people in England (1 in 10 of us) already drink fluoridated water because of where they live. A further 400,000 live in areas where fluoride levels in water are already naturally elevated due to the surrounding geology. There’s evidence that these areas have lower levels of dental disease than similar areas without fluoridation. For 5-year-olds living in the most deprived areas, the odds of tooth decay are reduced by a third.
Water fluoridation schemes such as this have been used for over 70 years internationally, and in England for over 55 years. In its 2018 report, PHE concluded, that “water fluoridation is an effective and safe public health measure to reduce the frequency and severity of dental decay, and narrow differences in dental health between more and less deprived children and young people”.
Creating healthy places
The transition into work is another important moment in our health journey. We know that good work is good for health.[footnote 132] A job can provide us with money in our pocket, social connections, and a strong sense of purpose and identity. Yet, for some, health problems can be a barrier to gaining and retaining employment. This is particularly the case for those living with long-term health conditions like musculoskeletal problems, mental ill-health, and other conditions.[footnote 133]
In the years ahead, we will continue to work towards the manifesto commitment to see a million more disabled people in work by 2027, as set out in Improving Lives: the Future of Work, Health and Disability. Employers have a critical role to play. In the 2020s, we urgently need more employers to act like the best. The Thriving at Work review led by Lord Stevenson and Paul Farmer set clear standards that all employers should follow to support people’s mental health at work. The government is committed to modelling these as an employer and ensuring other parts of the public sector do the same. The government will also create the right conditions for success.
The government recently published Health is Everyone’s Business: a consultation on measures to reduce ill health-related job loss. This includes proposals for improving access to occupational health. This activity will align with the government’s plan for implementing the recommendations from the Matthew Taylor Review of Modern Working Practices.
Looking beyond the consultation, the government will also explore how to align support for people with mental and physical health conditions across the NHS, employers and occupational health – so that boundaries and responsibilities are clear and good information about support is available.
Given the prevalence of musculoskeletal problems in the workforce, we want to ensure all businesses are equipped with the knowledge and tools they need. The government will assist by:
-
convening an MSK expert reference group to review existing guidance about what has worked well and what could be improved
-
developing a package of actionable MSK advice for employers, supported by free digital tools and promoted through health and safety inspections
-
launching and promoting these employer resources through multiple, existing channels
Given the scale and cost of MSK conditions – to individuals and the economy – we need to take further action.[footnote 134] Much is already being done at national and local level. Our forthcoming consultation on reducing ill-health-related job losses will set out proposals for strengthening action in the workplace. Some local areas are also already taking action, but we need to do much better at translating this evidence into action, and at greater scale. Key to this is understanding the evidence and what action to prioritise. There’s already robust evidence on various aspects of MSK health, including how conditions like back and neck pain and arthritis can be prevented and managed. The government already has research under way to explore this, but there is much further to go in terms of putting this into practice.
To help support future action, the government will be launching a call for evidence on MSK later in the year, building on the evidence we are already developing through research and trials.
This will be focused on priority areas for action, potentially including:
-
raising awareness of MSK conditions among the public
-
the role of physical activity
-
population-level behaviour change programmes
-
action to support staff in the workplace
-
links between mental and MSK health
We’re also interested in what data should be routinely collected on MSK conditions.
Homes, neighbourhoods and communities
The homes and communities in which we live have a big impact on our health. They influence our transport choices, how we spend our leisure time including keeping in touch with friends and family, and whether we feel safe and secure at home and in public.
Safer communities
Reducing knife crime and tackling serious violence is a government priority. In April 2018, the government published its Serious Violence Strategy, which set out a programme of action including the Early Intervention Youth Fund, the media campaign #knifefree, and the new National County Lines Co-ordination Centre. Since then, further measures have been delivered including:
-
£200 million investment in a Youth Endowment Fund to help prevent and support those at risk of violent crime
-
an Independent Review of Drugs which is now underway
-
a consultation on a proposed new statutory duty to underpin a public health approach to tackling serious violence
-
a £100 million investment to support increased police activity and establish violence reduction units
The Prime Minister chaired a cross-sector summit in April 2019 to bring over 140 stakeholders together to explore what can be done to reverse the rise in serious youth violence. The government is driving forward a public health approach to tackle serious violence with a focus on prevention and multi-agency working to tackle the issue. A wide range of agencies and organisations came together locally to identify people and communities at risk early and take action to reduce serious violence and protect people. The government will support efforts to tackle this issue. Health organisations will need to play their part in addressing the root causes of violence, including meeting the mental health needs of young people and playing a full and active role in multi-agency partnerships to tackle serious violence at a local level.
Case study: West Midlands Violence Prevention Alliance
West Midlands Police, the local Police and Crime Commissioner and PHE have started a West Midlands Violence Prevention Alliance. This involves bringing together organisations from local government, policing, health and education along with charities and community groups to take a public health approach to preventing violence. The alliance has used a range of existing information to understand where violence is most likely to happen, what puts people more at risk of being victims and perpetrators, and what the costs and consequences are.
They have used this information to promote, deliver and evaluate evidence-based approaches to reduce violence. These include secondary school children teaching their peers to speak out against all forms of violent and abusive behaviour; link workers in GPs to help those suffering domestic abuse to access specialist support; as well as youth workers based in hospitals to help young people break out of cycles of violence.
Connected communities
As set out in A Connected Society: a strategy for tackling loneliness in October 2018, feeling lonely often is linked to early deaths – with the effect of loneliness on a par with smoking or obesity. It’s also linked to increased risk of coronary heart disease and stroke, depression, cognitive decline and Alzheimer’s.[footnote 135] Supporting people to avoid or move out of loneliness before it becomes entrenched can help prevent the adverse health conditions associated with frequent loneliness. The loneliness strategy is an important first step but government is committed to long-lasting action to tackle the problem of loneliness. As set out in the strategy, we will publish annual reports on the loneliness agenda, with the first report planned for late 2019.
The government recently strengthened planning guidance to encourage more areas to consider cycling and walking within local development plans, and other ways of getting people more physically active. Work is also underway to make public transport more inclusive - so disabled people, including those with less visible disabilities such as autism, have the same opportunities to travel as everyone else.
Homes and neighbourhoods
For people living with a disability – or with some frailty, including those living with dementia – having a suitable home is particularly important. We know that 8 in 10 of the homes we’ll occupy in 2050 have already been built.[footnote 136] As such, it’s vital we look at existing homes, not just new builds. That’s why home repairs and adaptations are crucial. While evidence shows that only 7% of homes have all the access features required for people with limited mobility, 72% have the potential to reach ‘visitable standards’, for example so they could be visited by somebody living with a physical disability.[footnote 137]
In the 2020s, home adaptations, assistive technology and supported housing will be more important than ever; helping people to stay independent for longer and supporting those with complex needs including serious mental illness, learning disabilities and autism to lead good quality lives in communities. In the years ahead, the government has an opportunity to shape this emerging market and test new ideas and innovations.
Case study: Middlesbrough Staying Put
The Middlesbrough Staying Put home improvement agency is an advice and repair service that helps older people, people with disabilities, and those who are vulnerable, to live independently and safely within their own homes.
Staying Put works closely with other organisations and services, including health and social care. This means that people get co-ordinated support to help improve their health, wellbeing and quality of life.
The agency offers a range of practical solutions to problems with housing, including:
-
information and advice to help people live independently in their own homes
-
a handyperson service, which provides minor repairs and adaptations, and major adaptations for people with a disability
-
an assistive technology service, providing technology to help people to live independently and safely (such as falls sensors, door alarms or GPS trackers)
-
seasonal support, including a Winter Warmth programme that helps tackle fuel poverty
-
staff based in hospitals providing support to help people live safely so that they can return home more quickly and are less likely to need hospital treatment in future
There is a clear link between cold homes and ill-health, where existing conditions such as respiratory illnesses or mental health conditions are exacerbated.[footnote 138] The government wants all fuel poor homes to be upgraded to Energy Performance Certificate (EPC) Band C by 2030 and our aspiration is for as many homes as possible to be EPC Band C by 2035 where practical, cost-effective and affordable.
To support these aims, existing policies are in place to improve the energy performance of homes, such as the £3.6 billion of investment provided by the Energy Company Obligation. The government is undertaking a review of the Fuel Poverty Strategy and intends to ensure that work to improve the quality of homes is aligned with preventative healthcare, with everyone living in a warm and safe home that supports healthy and independent living.
Later this year, we’ll launch the ‘Home of 2030’ design competition, bringing together the Clean Growth and Ageing Society Grand Challenges. The competition will explore how the combination of innovative design and construction with new technology can create more energy efficient, accessible and adaptable homes designed to fit the needs of all generations.
NHS England launched the Healthy New Towns programme in 2015 to explore how the development of new places could provide an opportunity to create healthier and connected communities with integrated and high quality services. Lessons from 10 demonstrator sites have been used to develop a set of principles for ‘Putting Health into Place’, which will be published shortly. Local systems should use these principles as they plan, design and manage new neighbourhoods, streets, parks and buildings so that they prioritise health and wellbeing and incorporate new ways of providing health and social care services relevant to current and future population needs.
Case study: Changing Places toilets
Changing Places toilets give people with severe disabilities and their families the opportunity to visit public places which they otherwise would not be able to and can therefore make a huge difference to their quality of life. It is estimated that at least 250,000 people in the UK need Changing Places toilets in order to have their toileting needs met in a safe, dignified and humane way.
There are only between 30 and 40 Changing Places facilities on the NHS estate in England which are registered with the Changing Places Consortium (although there may be some facilities that aren’t registered). In December 2018, the Care Minister announced £2 million funding for NHS trusts in England to install Changing Places facilities in hospitals and significantly increase the number available. From 31 May 2019, NHS trusts have been able to bid for this funding, on a matched basis.
The government is also working to increase the number of other places with a Changing Places toilet. The Department for Transport’s Inclusive Transport Strategy is providing £2 million funding for Changing Places toilets in motorway service areas. In May 2019, the Ministry of Housing, Communities and Local Government launched a consultation on how we can increase the number of Changing Places toilets in new, large buildings commonly used by the public (such as cinemas, shopping centres, sports and music venues and transport hubs), including a potential change to the Building Regulations.
Green spaces and clean air
The outdoors can also help us grow our health asset. For example, evidence shows that spending time in the natural environment can improve our mental health and wellbeing. It can reduce stress, anxiety and depression, and encourage physical activity which in itself contributes to better mental health.[footnote 139]
Yet, air pollution is the top environmental risk to human health in the UK and one of the greatest threats to our health after cancer, heart disease and obesity. It affects people of all ages, but particularly at the beginning and later stages of life.[footnote 140] It is estimated that long-term exposure to man-made pollution in the UK has an annual effect equivalent to between 28,000 and 36,000 deaths.[footnote 141]
The government published an ambitious Clean Air Strategy in January 2019, which builds on the 25 Year Environment Plan commitments and complements the Industrial Strategy, Clean Growth Strategy. Analysis of the Clean Air strategy suggests that delivering on these commitments could cut the costs of air pollution to society by £1.7 billion every year from 2020, rising to £5.3 billion every year from 2030. This is because air pollution is associated with respiratory and heart diseases, and emerging evidence is increasingly pointing to a possible contribution to other wider health risks such as stillbirth, low birth weight and dementia.[footnote 142]
In the year ahead, we will be working with the Department for Environment, Food and Rural Affairs on 2 priority areas:
-
To improve public awareness about pollution sources, including campaigns about wood and coal, to empower people to take action to reduce their own impact on and exposure to, local pollution. This will be achieved by conducting and publishing independent research and national scale communication activities.
-
To improve data on health impacts, using syndromic surveillance and other health data routinely collected to support monitoring and evaluation of long-term trends in health impacts associated with air quality. This will be achieved through internal research and establishment of stronger links between health data sets and air quality monitoring undertaken across the public sector. We will align the work plans of our independent group (Committee on Medical Effects of Air Pollution – COMEAP) with the Department for Environment, Food and Rural Affairs’ independent advisory group (Air Quality Expert Group – AQEG).
PHE is currently undertaking a 5-year programme to ensure government has the best possible advice on the health burden linked to indoor and outdoor air pollution, and what might be done to reduce this. This includes research and interpretation of the available scientific evidence around the effects on the length and quality of people’s lives.
Active ageing
Active ageing is about creating opportunities for people to live well throughout their lives. The decisions we take at midlife (around 45 years old) will have an important bearing on our later lives. Hence, there are steps we can take – both as individuals and as a society – to set ourselves up for longer, happier lives.
The menopause and women’s health
Women can lose up to 20% of their bone density in the 5 to 7 years after the menopause. This risk of osteoporosis (weak bones) and fractures stays relatively low until women get much older, however the menopause provides a useful time to take stock and adopt a healthier, bone-friendly lifestyle.
The risk of osteoporosis and fractures can be reduced by staying active through moderate-intensity activity (150 minutes is recommended per week), having a healthy diet, limiting alcohol intake and not smoking. Effects of the menopause such as this – as well as the benefits of Hormone Replacement Therapy (HRT) – reflect how it is a multifaceted health issue, with longstanding consequences for women. This and other effects have been highlighted during meetings of the Women’s Health Taskforce, established and co-chaired by the Parliamentary Under Secretary of State for Mental Health, Inequalities and Suicide Prevention.
We also need to do more to educate both men and women on healthy periods. An estimated 1 in 3 women are affected by fibroids, and 1 in 10 women of reproductive age have endometriosis. Early intervention and education on these conditions can prevent them becoming debilitating.
The population of England is becoming older.[footnote 145] As older people make up a larger proportion of the population, they will also make an increasing contribution to society. They are our workers, volunteers, taxpayers and carers.
As a country, we’re not always making the most of the opportunities afforded by an ageing population. Too many people are forced out of work by poor health or unwelcoming employers. Too few have access to the training they need to change careers. Too many families face the hard choice between working or caring for a loved one. And too few homes and neighbourhoods meet the needs of older people.[footnote 146]
If an older population means fewer workers and higher demands for public services, this raises important questions about future sustainability. In the decades ahead, the challenge will be to ensure the growing number of people in later life are healthy, empowered and able to continue making a full contribution to society, and to enjoy their lives.
We know that people age differently and there is no typical experience of later life. Many people age well and have a well-connected, purposeful older age with good health and a strong sense of belonging. But there can be a negative discourse on ageing that’s unhelpful – one that describes older people as a burden, and later life as a time of ill-health and loneliness. This negative narrative has an impact on attitudes towards ageing not only among older people themselves, but also among some health and social care professionals. We need to urgently reframe this narrative to an asset-based model.
Case study: Homeshare and Shared Lives Plus
Homeshare organisations bring people with spare rooms together with people who are happy to chat and lend a hand around the house in return for affordable, sociable accommodation. Together, Householders and Homesharers share home life, time, skills and experience. Householders are often older people who need a bit of help around the house or garden, a lift to the shops or just someone to have a meal with and chat to. Homesharers might be new to a city, studying or in low-income employment.
Charlotte, who is in her 90s and has lived, worked and raised a family in Oxford, says: “Now I have a Homesharer, my middle-aged children feel reassured because there is someone else in the house with me. Esme is a great help with the telephone, as I am quite deaf. She also helps with my computer and with online food shopping.”
Where there is no local Homeshare service, councils can develop their own, commission a new one, or develop a formal partnership with one or more existing programmes.
This government believes the 2020s needs to be a decade of active ageing. A decade where ageist stereotypes are forgotten, and replaced with a more positive and nuanced view of older age. A view that better reflects reality.
To support this shift, PHE with the Centre for Ageing Better and national partner organisations is developing a Consensus Statement on Healthy Ageing to set out key principles and ways of working together, as well as carrying out a review of how we can focus more attention on older people’s issues.
-
Support people with staying in work
-
Support people with training to change careers in later life
-
Support people with caring for a loved one
-
Improve homes to meet the needs of older people
-
Improve neighbourhoods to meet the needs of older people
-
Other:
National action
Prevention in wider policies
Given the variety of factors that affect our health, many of the relevant policies sit outside DHSC, in other departments like: HM Treasury, the Department for Education, the Department for Work and Pensions, the Department for Transport, the Department for Environment, Food and Rural Affairs, the Ministry of Housing, Communities and Local Government, and the Department for Digital, Culture, Media and Sport.
Many wider government policies already contribute towards the prevention agenda. For example, the Cycling and Walking Investment Strategy aims to get people more active in their transport choices, for example by doubling the rates of cycling by 2025.
In the 2020s, we believe that all of government should be ‘pulling in the same direction’ on prevention. This requires sustained focus over the long term, but there are a number of actions we can take now to lay the foundations for good health in the years to come.
As recommended by the Chief Medical Officer for England in her 2018 Annual Report, we will develop and launch a new Composite Health Index. The index will provide a visible, top-level indicator of health, and can be tracked alongside our nation’s GDP. It will measure changes in health over time and, along with other indicators, can be used by the government to assess the health impacts of wider policies. This is part of a broader shift towards viewing health as one of the primary assets of our nation, contributing both to the economy and to the happiness of the population.
Alongside this we’ll be expanding PHE’s capacity to project and model the impact of future trends in health, building on the foundation of its existing work to publish an annual Health Profile for England.
We will also work across government to build on existing appraisal tools and improve the quality and coverage of health impact assessments of non-health policies.
Value for money
Prevention is common sense. We also know it represents extremely good value for money. A recent systematic review found that for every £1 spent on public health interventions, there was an average £14 of benefit to wider society. This includes healthcare savings, but also the longer-term gains in health and to wider society.[footnote 147]
Prevention forms around 5% of all public funding on health. This means in the UK we are spending over £101 billion a year treating disease, and £8 billion preventing it.[footnote 148]
As a country, we need to ask ourselves some fundamental questions about how much we value prevention, and what this means for our public services. Using obesity as an example, each year we spend more on treating health problems than preventing them in the first place.
World-class research
Transformative change in prevention will only be achieved if it is underpinned by high-quality research. We aim to build on existing strengths to make the UK the world leader in public health and prevention research. This must deliver an evidence base that is much more ambitious and draws on a whole new range of disciplines.
To achieve this, we will:
-
set clear ambitious goals and principles for the research community based on the future needs of the nation – for example, understanding how to create and maintain built and natural environments that support better health; focused national and local solutions to meet the needs of excluded and vulnerable populations within their communities and across different geographical locations
-
spark a culture shift, increasing the input from disciplines such as engineering or education, co-producing research with the public, policy makers and practitioners; answering the most important questions facing local authorities and service providers
-
focus research on the areas in the country where the public health challenges are greatest, tackling some of the biggest and most entrenched issues in the populations where the need for action is greatest
-
inspire the next generation of researchers, attracting the best people into prevention research; combining academic research with practice as a career pathway
Local action
Prevention policies are not experienced in the abstract, but in the neighbourhoods and communities in which people live. That’s why the role of ‘place’ will be an integral part of any prevention strategy. Local authorities will have a key role to play, given that they:
- have specific responsibilities around prevention, for example sexual health, children’s health, adult social care and support, and drug and alcohol services
- control many of the assets for good health, for example parks and green spaces, leisure facilities, and cycling and walking infrastructure
- have decision-making power for areas like housing policy, planning and social care and support, which have a big impact on people’s health
- shape other policies relevant to health, including economic development, education, and growing the voluntary and community sector
Since they assumed their public health responsibilities in 2013, local authorities have commissioned creatively and energetically. They have secured real improvements and efficiencies by challenging historic service models and finding new ways of doing things, including through ‘digital first’ service offers in areas such as sexual health.
In December 2017, the government announced its aim to increase business rates retention to 75% by devolving grants of equivalent value, including the Public Health Grant. The government is continuing to engage stakeholders on the implementation of this aim. This includes consideration of what more needs to be done to build a full range of assurance arrangements for delivering public health services and outcomes. The government will take a final decision on these matters in due course.
Case study: The Wigan Deal
Wigan has worked to improve the health and wellbeing of local people through an ‘asset-based approach’. This aims to understand the existing strengths that communities have and make best use of them.
Wigan Council, the local NHS, charities and community groups have taken a new common approach to working with people, families and communities. This has included prioritising wellbeing, prevention and early intervention. Significant effort has been put into communicating this to staff and local people, so that everyone has a common vision of what to expect. This has led to ‘The Deal for Health and Wellbeing’ in which local services and organisations make commitments to local people, including:
-
ensuring there are a wide range of facilities within local communities, including timely access to good quality GP services
-
supporting families to give their children the best start in life
-
helping those who are unemployed into work, and supporting older people to stay independent for as long as possible
In return people are asked to contribute by:
-
keeping active at whatever stage of life, quitting smoking, drinking and eating sensibly, and registering with a GP and going for regular check-ups
-
taking time to be supportive parents or guardians
-
taking advantage of training and job opportunities, and setting high aspirations, and supporting older relatives, friends and neighbours to be independent for as long as possible
Since 2012 to 2014, healthy life expectancy in Wigan has increased by approximately 17 months for women and 12 months for men – both around 10 months more than the average for the North West over that same time period.
The role of local Health and Wellbeing Boards is to bring together the local partners in local government, the NHS and more widely, to assess needs and to develop effective strategies that meet them. The potential of local authorities to influence the wider determinants of health and provide local leadership for health improvement action was one of the key factors for returning a major health role to them in 2013. There are already examples of integration working well across the country.
The shift towards Integrated Care Systems (ICSs) should help deliver more progress in this area by bringing together commissioners, providers and local authorities, to make decisions that are in the best interest of the entire health economy, not just individual organisations. Health and Wellbeing Boards should form a key part of the local infrastructure on prevention, working with ICSs. We believe that the key tools that are needed – such as flexibility to pool budgets – already exist, and that Health and Wellbeing Boards in particular should have an important role to play in the new structures.
Directors of public health provide expertise and leadership for improving and protecting the health of their local populations. They have a key role to play in raising awareness and knowledge of both core public health issues and the impact of the wider determinants of health (such as housing, planning and transport). Since 2015, PHE has been running a ‘Future Directors’ leadership programme and providing support for newly appointed directors of public health across the country.
Modern healthcare is complex, and there are some areas where concerns have been raised about the effects of dividing responsibility between different NHS and local government agencies. That’s why the NHS Long Term Plan committed the government to reviewing the commissioning arrangements for sexual and reproductive health, health visiting and school nursing services, to ensure that they can deliver the best outcomes for the people who need them.
We have now confirmed that local authorities will continue to be responsible for commissioning these services, but that the NHS and local authorities must work much more closely together on these services to deliver joined-up care for patients and to embed prevention into the full range of health and other public services.
Throughout the review people told us the importance of local authorities and the NHS working together to plan and deliver these services. This is a complex task and while there are some inspiring examples of success, this is too often dependent on the efforts of particular individuals or favourable local circumstances. As a result, the extent and nature of collaborative commissioning arrangements varies dramatically.
We want to see the NHS and local authorities working more closely with more collaborative commissioning. In some areas – such as sexual and reproductive health – we want collaborative commissioning to become the norm, building on best practice from across the country. This will require local authorities and the NHS to work closely together at both the national and local level.
Case study: ‘Our Dorset’: Prevention in an Integrated Care System
‘Our Dorset’ was one of the NHS’s first ICSs. Dorset’s NHS organisations came together, in partnership with local councils and others, to take collective responsibility for improving the health of local people and meeting NHS standards for healthcare.
Dorset put prevention at the heart of its plans for becoming an ICS. It recognised that staff were key to making this work and so developed a culture of promoting and valuing prevention. By challenging staff to work and think differently, great improvements have been made in the number, size and results of actions to prevent ill-health. This includes:
-
healthy living advice and coaching to help people get active, lose weight, stop smoking and drink less, based on the evidence of what works
-
working with schools to improve health, particularly focusing on mental health and wellbeing, and increasing physical activity
-
helping people stay warm through installing insulation for older people and those with health conditions likely to deteriorate where their housing is cold and damp
The move towards ICSs creates the opportunity to co-commission an integrated sexual and reproductive health service. In fact, some areas like Hampshire are already doing this. Throughout the review, we saw different ways of doing this, for example designating a lead commissioner or pooling budgets via local arrangements. We recognise that local areas need to be able to decide what suits them best. However, we want to encourage more places to use the powers and levers they already have to develop joint approaches. This might include more consistent co-commissioning arrangements, and making the best use of Health and Wellbeing Boards.
Sexual and reproductive health
Sexual health services are core to prevention. Good progress has been made in a number of areas. Most significantly, we have seen new diagnoses of HIV reduce by 28% since 2015[footnote 150] and teenage pregnancy rates at an all-time low.[footnote 151] The UK was one of the first countries to meet the UN’s global goals on HIV[footnote 152] and we are already committed to going further and achieving zero infections by 2030 as announced by the Secretary of State in January this year. We are considering how we move to mainstream commissioning of HIV Pre-Exposure Prophylaxis.
More challenging is 2018 data published by PHE, which shows that rates of some sexually transmitted infections, most notably gonorrhoea, are increasing.[footnote 153] This underlines the need to continue to promote condom use and ensure that those at risk can rapidly access services, including on-line testing.
We need to actively address how we maintain momentum in those areas where we are doing well and to respond to the challenges where progress has stalled or been too slow. We are therefore considering calls from the Health and Social Care Committee (HSCC) and others to develop a new Sexual and Reproductive Health Strategy for England. A full response to the select committee report will be published shortly. We want your views on the development of a new strategy, and the areas that any new strategy should prioritise.
Conclusion
For the first 70 years of the NHS, we have concentrated on helping people live longer – and we have been hugely successful. Now we must move from simply thinking about life span to health span: the number of years we can keep people living healthy, independent lives free from illness or disability.
The commitments outlined in this green paper signal a new approach to public health. One that involves a new personalised, prevention model. It will mean the government, both local and national, working with the NHS, to put prevention at the centre of our decision-making.
These commitments will help us towards our mission of ‘5 more years of healthy, independent life by 2035 while reducing the gap between richest and poorest’. However, we’ve been clear that they won’t deliver the whole 5 years, and that further action will be needed. That’s why we’ll aim to publish a government response to the green paper by spring 2020, setting out our proposals in more detail.
The government is committed to delivering the Ageing Society Grand Challenge – where the ‘5 more years’ ambition comes from – and ensuring the UK is at the cutting edge and world-leading in our approach to demographic changes. We recognise that this requires action across government and through the spending review process we will establish how we best co-ordinate and drive delivery of this work, for example, through the creation of an office to support healthy ageing.
For prevention to succeed, and to improve the nation’s health over the next decade, individuals and communities must play their part too. This involves making healthier choices for ourselves and our families – eating well, staying active, being smoke-free, and taking care of our mental health – and laying the foundations for good health throughout our lives. Health is a shared responsibility. Only by working together can we achieve our vision of healthier, happier lives for everyone.
References
-
Office for National Statistics (2018) 'Past and projected data from the period and cohort life tables, 2016-based: England and Wales, 1841 to 2066'
Office for National Statistics (2017) '2016 single year national life tables'
Period life expectancy for England and Wales 1916 - 2016 ↩ -
Office for National Statistics (2019) 'Cancer survival in England: national estimates for patients followed up to 2017' ↩
-
Public Health England (2018) 'Health Profile for England 2018: Chapter 2: trends in mortality' ↩
-
Office for National Statistics (2018) 'Changing trends in mortality in England and Wales: 1990 to 2017 (Experimental Statistics)' ↩
-
Office for National Statistics (2018) 'Health state life expectancies, UK: 2015 to 2017'
'Poor health' relates to self-reported 'fair', 'bad' and 'very bad' general health, whereas 'good health' refers to self-reported 'good' and 'very good' general health. Estimates are for Healthy Life Expectancy at birth in England. ↩ -
Office for National Statistics (2019) 'Health state life expectancies by national deprivation deciles, England and Wales: 2015 to 2017'
Deprivation deciles are based on the Index of Multiple Deprivation 2015 which is the official measure of relative deprivation. Estimates shown for England. Please note figures will not sum due to rounding. ↩ -
Heslop, P. et al (2013) 'Confidential Inquiry into premature deaths of people with learning disabilities (CIPOLD)'
Public Health England (2016) 'People with learning disabilities in England 2015: Main report'
NHS Digital (2019) 'Health and Care of People with Learning Disabilities, Experimental Statistics: 2017 to 2018' ↩ -
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19)
Bull, FC. and the Expert Working Groups (2010) 'Physical Activity Guidelines in the UK: Review and Recommendations' ↩ -
Steel, N. et al (2018) 'Changes in health in the countries of the UK and 150 English Local Authority areas 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016' ↩
-
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19) Percentage of total years lived with disability in England by level 2 cause (all ages, both sexes) - 2017
Years lived with disability (YLDs) is a measure of morbidity used in the Global Burden of Disease study (GBD) that combines the prevalence of each disease with a rating of the severity of its symptoms, to give an overall measure of the loss of quality of life. ↩ -
Ibid ↩
-
Versus Arthritis, formerly Arthritis Research UK (2018) 'State of Musculoskeletal Health 2018' ↩
-
Ibid ↩
-
Heuch, I. et al (2013) 'Body mass index as a risk factor for developing chronic low back pain: a follow-up in the Nord-Trøndelag Health Study' Spine, vol. 38, no. 2, pp.133-139, 2013
Smuck, M. et al (2014) 'Does physical activity influence the relationship between low back pain and obesity?' The Spine Journal, vol. 14, no. 2, pp. 209-216, 2014 ↩ -
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19) Percentage of total years lived with disability in England by level 2 cause (all ages, both sexes) - 2017 ↩
-
NHS Digital (2015) 'Health Survey for England 2014'
NHS Digital (2016) 'Adult Psychiatric Morbidity Survey: Survey of Mental Health and Wellbeing, England, 2014'
This estimate reflects the balance of evidence across both the Health Survey for England and the Adult Psychiatric Morbidity Survey. ↩ -
NHS Digital (2015) 'Health Survey for England 2014'
Please note that these are self-reported diagnoses of mental health issues. The 2014 Adult Psychiatric Morbidity Survey further shows that 1 in 6 adults had a common mental disorder. This covers depression, generalised anxiety disorder (GAD), panic disorder, phobias, obsessive compulsive disorder (OCD), and common mental disorders not otherwise specified (CMD-NOS). ↩ -
NHS Digital (2015) 'Health Survey for England 2014'
NHS Digital (2016) 'Adult Psychiatric Morbidity Survey: Survey of Mental Health and Wellbeing, England, 2014' ↩ -
NHS Digital (2015) 'Health Survey for England 2014'
NHS Digital (2016) 'Adult Psychiatric Morbidity Survey: Survey of Mental Health and Wellbeing, England, 2014'
Chakraborty, A. et al (2011) 'Mental health of the non-heterosexual population of England'. Journal of Psychiatry, 198, 143–148. ↩ -
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19) Percentage of total years lived with disability in England by level 2 cause (all ages, both sexes) - 2017 ↩
-
The Richmond Group of Charities (2018) 'Multimorbidity - Understanding the Challenge' ↩
-
The Richmond Group of Charities (2018) 'Multimorbidity - Understanding the Challenge'
Fortin, M. et al (2014) 'Lifestyle factors and multimorbidity: a cross sectional study', BMC Public Health, 14, 686–694
Dhalwani, N. et al (2016) 'Association Between Lifestyle Factors and the Incidence of Multimorbidity in an Older English Population', The Journals of Gerontology: Series A, Volume 72, Issue 4, 528–534 ↩ -
Department for Business, Energy and Industrial Strategy (2019) 'The Grand Challenge missions: Ageing Society' ↩
-
Office for National Statistics (2018) 'Health state life expectancies, UK: 2015 to 2017'
Disability-free life expectancy is a measure of the average number of years a person would live without a long-lasting physical or mental health condition that limits daily activities. Please note that it is based on current age-specific mortality and disability rates and does not allow for future projected changes in mortality or disability. ↩ -
Ibid; estimates are for Disability-Free Life Expectancy at birth in England. ↩
-
Ibid ↩
-
Adapted from McGinnis J., Williams-Russo P., Knickman J.R. (2002) 'The case for more active policy attention to health promotion' ↩
-
Canadian Institute of Advanced Research (2002), quoted in Kuznetsova, D. (2012) 'Healthy places: Councils leading on public health' ↩
-
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19)
Percentage of total years lived with disability in England by level 2 causes and risks (all ages, both sexes) - 2017 ↩ -
NHS Healthcheck (2019) 'Explore NHS Healthcheck data', healthcheck.nhs.uk (viewed 10/6/2019) ↩
-
For example: Lindbohm, J.V. et al (2019) '5-year versus risk-category-specific screening intervals for cardiovascular disease prevention: a cohort study' ↩
-
O'Neill, J (2016) 'The Review on Antimicrobial Resistance: Tackling drug-resistant infections globally: Final report and recommendations', Wellcome Trust & HM Government ↩
-
OECD (2019) 'Health and economic burden of antimicrobial resistance', in Stemming the Superbug Tide: Just A Few Dollars More
Average number of deaths due to AMR infections in the UK over 2015 to 2050 is estimated to be 2,126. Average annual health care expenditure associated with AMR in the UK over 2015 to 2050 is estimated to be $179,183.10 per 100,000 persons (USD PPP). Scaling to the mid-2018 UK population of 66,435,550, and converting to GBP gives an annual cost of approximately £95 million (to nearest £5 million). This fluctuates depending on the exchange rate. For example, looking at the range in rates over the last year, this could range from £89 million to £95 million. ↩ -
World Health Organization (2019) 'Immunization' (viewed 05/07/2019)
Plotkin S.L., Plotkin S.A. (2004) 'A short history of vaccination', Vaccines; via WHO (2008) 'Vaccination greatly reduces disease, disability, death and inequity worldwide' ↩ -
For example, the measles vaccination has prevented an estimated 20 million cases and 4,500 deaths in the UK since its introduction in 1968.
Public Health England (2018) '50 years of measles vaccination in the UK' (viewed 10/6/2019) ↩ -
NHS Digital (2018) 'Childhood Vaccination Coverage Statistics- England 2017-18' ↩
-
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19)
Percentage of total years lived with disability in England by level 2 causes and risks (all ages, both sexes) - 2017 ↩ -
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19)
Percentage of total years lived with disability in England by level 2 risks (all ages, both sexes) - 2017 ↩ -
Office for National Statistics (2019) 'Adult smoking habits in the UK: 2018' Adult smoking habits in Great Britain 1974-2018'
Estimates are for GB and based on the Opinions and Lifestyle Survey. Please note that estimates prior to 2000 are unweighted. ↩ -
OECD (2018) 'Health at a Glance: Europe 2018': Smoking among adults
Please note that this international comparison is for Great Britain/UK (not England). Estimates are based on the Opinions and Lifestyle Survey for Great Britain. No data has been supplied by NISRA for NI for 2006 onwards, so current OECD figures for the UK relate to Great Britain only.
Office for National Statistics (2019) 'Adult smoking habits in the UK: 2018'
14.4% of adults in England (14.7% in UK) smoked in 2018 (Annual Population Survey).
The statement 'fewer than 1 in 6' is also consistent with Great Britain data from the Opinions and Lifestyle Survey (16.6% of adults). However, please note that headline prevalence figures for smoking are usually taken from the Annual Population Survey due to its greater precision. ↩ -
Office for National Statistics (2019)'Adult smoking habits in the UK: 2018'
14.4% of adults in England smoked in 2018 (Annual Population Survey) ↩ -
Ibid ↩
-
NHS Digital (2019) 'Statistics on Smoking, 2019' ↩
-
NHS Digital (2019) 'Statistics on Women's Smoking Status at Time of Delivery, England - Quarter 4, 2018-19' ↩
-
Office for National Statistics (2019) 'Adult smoking habits in the UK: 2018': Smoking habits in the UK and its constituent countries (Annual Population Survey) ↩
-
Office for National Statistics (2019) 'Adult smoking habits in the UK: 2018'
15.6% of adults who identified as heterosexual in England smoked in 2017, compared to 22.4% of those identifying as gay or lesbian, and 24.0% of those identifying as bisexual (Annual Population Survey) ↩ -
Royal College of Physicians and Royal College of Psychiatrists (2013) 'Smoking and mental health' ↩
-
Birge, M., Duffy, S., Astrid Miler, J. and Hajek, P. (2018) 'What Proportion of People Who Try One Cigarette Become Daily Smokers? A Meta-Analysis of Representative Surveys', Nicotine & Tobacco Research, 20(12), 1427–1433 ↩
-
Committee on Toxicity (2017) 'Statement on heat not burn tobacco products'
Public Health England (2018) 'E-cigarettes and heated tobacco products: evidence review' ↩ -
NHS Digital (2018) 'Health Survey for England 2017' ↩
-
NHS Digital (2018) 'National Child Measurement Programme, England - 2017/18 School Year'
Simmonds, M., Llewellyn, A., Owen, C.G. and Woolacott, N. (2016) 'Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis' Obesity reviews, 17(2), 95-107. ↩ -
NHS Digital (2018) 'National Child Measurement Programme, England - 2017/18 School Year'
NHS Digital (2018) 'Health Survey for England 2017' ↩ -
Public Health England (2017) 'Health matters: obesity and the food environment'
Public Health England (2019) 'Adult obesity: applying All Our Health' ↩ -
Public Health England (2018) 'Health Profile for England 2018: Chapter 3: trends in morbidity and risk factors'
Institute for Health Metrics and Evaluation (IHME). GBD Compare. Seattle, WA: IHME, University of Washington, 2015. Available from http://vizhub.healthdata.org/gbd-compare (viewed 19/06/19)
Percentage of total years lived with disability in England by level 2 risks (all ages, both sexes) - 2017
Diet and metabolic risk factors include obesity (high BMI), high blood glucose levels, high blood pressure and high cholesterol. ↩ -
Food Standards Agency and Public Health England (2018) 'NDNS: results from years 7 and 8 (combined)'
Public Health England (2018) 'Calorie reduction: The scope and ambition for action'
Public Health England (2016) 'National Diet and Nutrition Survey: assessment of dietary sodium, adults in England 2014' ↩ -
Public Health England (2019) 'Child Health Profiles': Indicator 2.02ii Breastfeeding prevalence at 6-8 weeks after birth, fingertips.phe.org.uk (viewed 19/06/19) ↩
-
Victora, C.G. et al (2016) 'Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect' ↩
-
NHS Digital (2018) 'Health Survey for England 2017' ↩
-
Department of Health and Social Care (2013) 'Diet and nutrition survey of infants and young children, 2011' ↩
-
Public Health England (2019) 'Foods and drinks aimed at infants and young children: evidence and opportunities for action' ↩
-
Food Standards Agency and Public Health England (2018) 'NDNS: results from years 7 and 8 (combined)' ↩
-
Public Health England (2017) 'Health matters: obesity and the food environment'
Public Health England (2019) 'Adult obesity: applying All Our Health' ↩ -
Public Health England (2019) 'Foods and drinks aimed at infants and young children: evidence and opportunities for action' ↩
-
Moynihan, P.J. and Kelly, S.A.M. (2013) 'Effect on Caries of Restricting Sugars Intake: Systematic Review to Inform WHO Guidelines'. Journal of Dental Research,93(1):8–18 ↩
-
Public Health England (2018)'Oral health survey of 5 year old children 2017' ↩
-
Public Health England (2019) 'Hospital tooth extractions of 0 to 19 year olds' ↩
-
Public Health England (2019) 'Foods and drinks aimed at infants and young children: evidence and opportunities for action' ↩
-
Based on unpublished results of DHSC commissioned research by Kantar Worldpanel in 2014. 2,525 products were checked for front-of-pack labelling.
Diabetes UK (2018) 'People with diabetes say all companies should use the same food labelling' , diabetes.org.uk (viewed: 10/06/2019) ↩ -
Strazzullo, P., Kandala, N.B. and Cappuccio, P. (2009) 'Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies' ↩
-
Public Health England (2016) 'National Diet and Nutrition Survey: assessment of dietary sodium, adults in England 2014' ↩
-
Retat, L., Pimpin, L., Webber, L. et al (2019) 'Screening and brief intervention for obesity in primary care: cost-effectiveness analysis in the BWeL trial'. International Journal of Obesity ↩
-
NHS Digital (2018) 'National Child Measurement Programme, England - 2017/18 School Year' ↩
-
Public Health England (2016) 'Health matters: getting every adult active every day' ↩
-
NHS Digital (2018) 'Health Survey for England 2017' ↩
-
Davies, C. (2017) Twitter.com (viewed: 10/06/2019) ↩
-
NHS Digital (2019) 'Statistics on Obesity, Physical Activity and Diet, England, 2019: Part 5: Physical activity' ↩
-
World Health Organization (2018) 'Global Health Observatory - Insufficient Physical Activity'
Age-standardised estimates for 18+; both sexes ↩ -
NHS Digital (2017) 'Health Survey for England 2016' ↩
-
Sport England (2019) 'Active Lives Adult Survey November 2017/18' ↩
-
NHS Digital (2017) 'Health Survey for England 2016'
In 2016, 31% of men and 24% of women aged 19+ met the guidelines for muscle-strengthening exercises. This includes those who met both the guidelines for moderate/vigorous physical activity and muscle-strengthening activities, and those who met guidelines for the latter only. ↩ -
Public Health England (2016) 'Health matters: getting every adult active every day' ↩
-
Access to mental health services in primary care settings: NHS England (2019) 'Mental Health Five Year Forward View Dashboard Q3 2018/19'
NHS Digital (2019) 'Psychological Therapies: Annual Report on the use of IAPT services - England, 2018-19'
Time-series data on access to mental health services in secondary care settings is not currently available. The estimated number of contacts to secondary services has increased.
NHS Digital (2018) 'Mental Health Bulletin 2017-18 Annual Report' ↩ -
NHS England (2019) 'The NHS Long Term Plan' ↩
-
NHS Digital (2019) 'Psychological Therapies: Annual Report on the use of IAPT services - England, 2018-19' ↩
-
NHS England (2019) 'The NHS Long Term Plan' ↩
-
Ibid ↩
-
The King's Fund and Centre for Mental Health (2012) 'Long-term conditions and mental health - the cost of co-morbidities' ↩
-
Department of Health and Social Care (2014) 'Annual Report of the Chief Medical Officer 2013 - Public Mental Health Priorities: Investing in the Evidence'
Royal College of Psychiatrists (2010) 'No health without public mental health' ↩ -
Department for Work and Pensions and Department of Health and Social Care (2017) 'Thriving at work – The Stevenson / Farmer review of mental health and employers' ↩
-
Chesney, E., Goodwin, G.M. and Fazel, S. (2014) 'Risks of all-cause and suicide mortality in mental disorders: a meta-review' World Psychiatry 13:2. ↩
-
Public Health England (2018) 'Health profile for England: 2018: Chapter 5 (inequalities in health)'
Public Health England (2014) 'Local action on health inequalities: Improving access to green spaces' ↩ -
Public Health England (2014) 'Local action on health inequalities: Improving access to green spaces'
Braubach, M. et al (2017) 'Effects of Urban Green Space on Environmental Health, Equity and Resilience'. In: Kabisch, N., Korn, H., Stadler, J. and Bonn, A. (eds) 'Nature-Based Solutions to Climate Change Adaptation in Urban Areas'. Theory and Practice of Urban Sustainability Transitions. Springer, Cham ↩ -
Gambling Commission, Responsible Gambling Strategy Board and GambleAware (2018) 'Measuring Gambling-related Harms: a framework for action'
Institute for Public Policy Research (2016) 'Cards on the table: The cost to government associated with people who are problem gamblers in Britain' ↩ -
NHS Digital (2018) 'Health Survey for England 2017' ↩
-
NHS Digital (2019) 'Statistics on Alcohol, England, 2019' ↩
-
Public Health England (2016) 'The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies: an evidence review'
This relates to self-reported consumption of alcohol. ↩ -
NHS Digital (2018) 'Health Survey for England 2017' ↩
-
Katikireddi, S. et al (2017) 'Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data'
Bellis, M. et al (2016) 'The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals' ↩ -
Public Health England (2017) 'An evidence review of the outcomes that can be expected of drug misuse treatment in England' ↩
-
Centers for Disease Control and Prevention (2019) 'Drug Overdose Deaths', cdc.gov (viewed 24/06/19)
Scholl, L. et al (2019) 'Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017'
Public Health Agency of Canada - Special Advisory Committee on the Epidemic of Opioid Overdoses (2019) 'National report: Apparent opioid-related deaths in Canada (January 2016 to December 2018)' ↩ -
Public Health England (2018) 'Alcohol and drug prevention, treatment and recovery: why invest?' ↩
-
NHS (2018) 'Why lack of sleep is bad for your health', nhs.uk (viewed 05/07/2019)
Medic, G., Wille, M. and Hemels, M.E.H. (2017) 'Short- and long-term health consequences of sleep disruption' Nat Sci Sleep. 2017; 9:151–161
Royal Society for Public Health (2016) 'Waking up to the health benefits of sleep' ↩ -
Kamdar, B.B, Needham, D.M and Collop, N.A (2012) 'Sleep Deprivation in Critical Illness: Its Role in Physical and Psychological Recovery', Journal of Intensive Care Med. 27(2), 97–111 ↩
-
Care Quality Commission (2018) 'Adult inpatient survey 2017' ↩
-
Medic, G., Wille, M. and Hemels, M.E.H. (2017) 'Short- and long-term health consequences of sleep disruption' Nat Sci Sleep. 2017; 9:151–161
Ibarra-Coronado, E.G. et al (2015) 'The Bidirectional Relationship between Sleep and Immunity against Infections', Journal of Immunology Research ↩ -
The Sleep Council (2017) 'The Great British Bedtime Report, 2017' ↩
-
NHS England (2019) 'The NHS Long Term Plan' ↩
-
NHS England (2019) 'Comprehensive model of personalised care', england.nhs.uk (viewed 24/06/19)
NHS England (2019) 'The NHS Long Term Plan' ↩ -
Center on the Developing Child (2007) 'The Science of Early Childhood Development (InBrief)'harvard.edu (viewed 13/06/2019) ↩
-
Joseph Rowntree Foundation (2007) 'Parenting and outcomes for children' ↩
-
Source data from Department for Education (2018) 'Early years foundation stage profile results: 2017 to 2018', but specific indicator accessible at Public Health England (2018) 'School Readiness: the percentage of children achieving a good level of development at the end of reception', fingertips.phe.org.uk (viewed 13/06/2019)
NHS Digital (2017) 'Smoking, Drinking and Drug Use Among Young People in England - 2016' ↩ -
Public Health England (2018) 'Health profile for England: 2018': Chapter 5 (inequalities in health) and 6 (wider determinants of health) ↩
-
Department for Education (2018) 'Early years foundation stage profile results: 2017 to 2018' ↩
-
Bellis, M.A. et al (2014) 'National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England', BMC Medicine, 12,72 ↩
-
Early Intervention Foundation (2017) 'Language as a child wellbeing indicator' ↩
-
Early Intervention Foundation (2017) 'Language as a child wellbeing indicator'
Law, J. et al (2009) 'Modelling developmental language difficulties from school entry into adulthood: literacy, mental health, and employment outcomes' ↩ -
Public Health England (2018) 'Oral health survey of 5 year old children 2017'
Public Health England (2017) 'Health matters: child dental health'
Estimates for hospital admissions are for 2015-16 ↩ -
Ibid ↩
-
Waddell, G., Burton, A.K. (2006) 'Is work good for your health and wellbeing?' ↩
-
NHS Digital (2019) 'NHS Outcomes Framework Indicators - May 2019 Release: 2.2 Employment of people with long-term conditions' ↩
-
Versus Arthritis, formerly Arthritis Research UK (2018) 'State of Musculoskeletal Health 2018' ↩
-
HM Government (2018) 'A Connected Society: A Strategy for tackling loneliness – laying the foundations for change'
Holt-Lunstad, J. et al. (2015) 'Loneliness and social isolation as risk factors for mortality: a meta-analytic review' Perspectives on Psychological Science, 10(2), 227–237
Valtorta, N.K. et al. (2016) 'Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies' Heart. 2016; 102(13): 1009–1016
Cacioppo, J.T, Hawkley, L.C and Thisted, R.A (2010) 'Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study' Psychol Aging. 2010;25(2):453–463 ↩ -
Institution of Engineering and Technology & Nottingham Trent University (2018), Scaling Up Retrofit 2050 ↩
-
Ministry of Housing, Communities and Local Government (2016) 'English Housing Survey 2014 to 2015: Adaptations and Accessibility of Homes Report' ↩
-
Public Health England (2014) 'Local action on health inequalities: Fuel poverty and cold home-related health problems' ↩
-
Public Health England (2014) 'Local action on health inequalities: Improving access to green spaces'
Braubach, M. et al (2017) 'Effects of Urban Green Space on Environmental Health, Equity and Resilience'. In: Kabisch, N., Korn, H., Stadler, J. and Bonn, A. (eds) 'Nature-Based Solutions to Climate Change Adaptation in Urban Areas'. Theory and Practice of Urban Sustainability Transitions. Springer, Cham ↩ -
Department for Environment, Food and Rural Affairs (2019) 'Clean Air Strategy 2019' ↩
-
Public Health England (2018) 'Associations of long-term average concentrations of nitrogen dioxide with mortality' ↩
-
Department for Environment, Food and Rural Affairs (2019) 'Clean Air Strategy 2019' ↩
-
Office for National Statistics (2019) 'Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2018' ↩
-
Ministry of Housing, Communities and Local Government (2016) 'English Housing Survey 2014 to 2015: Housing for Older People Report'
Ministry of Housing, Communities and Local Government (2016) 'English Housing Survey 2014 to 2015: Adaptations and Accessibility of Homes Report' ↩ -
Masters, R. et al (2017) 'Return on investment of public health interventions: a systematic review', Journal of Epidemiology and Community Health,71(8), 827–834
The return on investment estimate is a median of a review of published interventions worldwide (and not just limited to health interventions). It relates to the societal return, and not simply medical costs. ↩ -
Office for National Statistics (2019) 'Healthcare expenditure, UK Health Accounts: 2017'
Estimated government expenditure on healthcare is for the UK, not for England. Total government-financed healthcare expenditure in 2017 was £155.6 billion. ↩ -
Public Health England (2018) 'Trends in new HIV diagnoses and people receiving HIV-related care in the United Kingdom: data to the end of December 2017' ↩
-
Office for National Statistics (2019) 'Conceptions in England and Wales: 2017' ↩
-
Public Health England (2018) 'Progress towards ending the HIV epidemic in the UK: 2018 report' ↩
-
Public Health England (2019) 'Sexually transmitted infections and chlamydia screening in England: 2018' ↩
