Making vaccination a condition of deployment in care homes: government response
Updated 9 November 2021
1. Introduction
1.1 Background and objectives
The rollout of the COVID-19 vaccination to care homes has been phenomenal, thanks to effective leadership and collaboration across the NHS and social care sector, in partnership with local authorities, as well as the dedication of care home managers in supporting and encouraging staff. More than 1.2 million social care workers in England have now taken up the vaccination - an important step to protect themselves, their loved ones, and the people they care for, from becoming seriously ill or dying from COVID-19.
The independent Scientific Advisory Group for Emergencies (SAGE) Social Care Working Group has highlighted that people living in care homes have been particularly impacted by the COVID-19 pandemic, due to a combination of a heightened risk of severe outcomes following COVID-19 infection and the risk of outbreaks in these closed settings. Ensuring and sustaining very high levels of vaccination of people living and working in these settings is an essential public health intervention for a serious vaccine-preventable disease. Environments in which the same group of people come into close contact with one another, numerous times a day, will lead to faster and more comprehensive transmission of the virus to all occupants (workers and residents) than other more open settings.
The SAGE Social Care Working Group has also advised that at least 80% of staff and 90% of residents in a care home should have had a first vaccination dose to provide a minimum level of protection against outbreaks of COVID-19[footnote 1], recognising that current or emergent variants may require even higher levels of coverage and/or new vaccines to sustain levels of protection. The dual 80% or 90% threshold provides only a minimum level of protection; higher coverage and both doses would increase that level of protection.
The overall figure of 84.1% for staff vaccination uptake masks significant variation at a regional, local and individual care home level. As of 13 June, only 64.7% of older adult homes in England are currently meeting the dual threshold as set out by the SAGE Social Care Working Group for the first dose, falling to 44.1% for London. While the SAGE Social Care Working Group advice is specifically about first doses, it should be noted that, for second doses, only 40.5% of homes are reaching this 80/90% level of coverage. Again, London has the lowest coverage, with only 23.0% of care homes reaching the dual threshold for second doses[footnote 2].
Therefore, there remains a strong case for introducing, in the first instance in care homes, a new requirement for vaccines, in order to make these high-risk environments as safe as possible from the devastating effects of COVID-19.
The Department of Health and Social Care (DHSC) conducted a public consultation regarding an amendment to the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014. The amendment which we consulted on would require older adult care home providers to deploy only those workers who have received their COVID-19 vaccination in line with government guidance (unless medically exempt). We consulted on the amendment from 14 April to 26 May 2021 and the full consultation document is available online. This is the formal government response to that consultation.
The consultation posed a series of questions about the government’s proposals, which covered the following areas:
- proposed legislative change (views on whether to proceed with the policy)
- policy scope (which settings should be included and which people in those settings)
- who should be exempt
- implementation and proof of vaccination status
- the impact and implications on the workforce and on those with protected characteristics
The consultation was available through an online survey hosted on GOV.UK and over 13,500 responses were submitted. A total of 26 responses to the consultation were received outside of the online platform, which were also accepted and analysed. The government is grateful for the responses received from individuals and organisations and values the comments and views submitted.
This document summarises the responses to that consultation and sets out the government’s response to the issues raised in each section.
In the government response sections, ‘we’ refers to the UK government.
1.2 Stakeholder Engagement
To supplement the views provided in the consultation, DHSC conducted extensive engagement with stakeholders. We are grateful to all those who joined our senior level working group comprising social care providers, representatives of small and medium sized care providers, local government and regulators. Three meetings convened by DHSC took place between 28 April and 17 May 2021. The topics discussed included:
- the rationale behind the policy proposal
- proposed scope of the regulations
- equality issues
- workforce impacts
- impacts on providing a safe service
The Minister of State for Social Care has met with stakeholders to discuss the proposal. This has included representative groups of care users such as Think Local Act Personal, ambassadors with lived experience of care, and representatives of unpaid carers, for example Carers UK.
DHSC representatives met with a patient group on Monday 24 May to hear more from the perspectives of patients, residents, their families and their carers.
We have raised awareness of, and encouraged participation in, the consultation through our DHSC communications channels and through targeted communications delivered directly to all registered care homes, social care agencies, and membership bodies.
We have also analysed a sample of organisational responses in detail, the qualitative summary of which is included in the analysis sections.
2. Executive summary
There is a clear public health rationale for the proposed policy, which aims to protect people who are most at risk from COVID-19 and its complications, by driving vaccination uptake in high-risk settings and ensuring high staff vaccination levels are maximised and maintained.
Residents in care homes are particularly vulnerable to severe illness and death from COVID-19: Based on Office for National Statistics (ONS) data, around a third (31%) of registered deaths from COVID-19 in England were care home residents, as of 2 April 2021[footnote 3]. However, there is also a case for considering the application of this policy to other high-risk groups and settings such as hospitals. The potential for wider application across health and social care will be subject to a public consultation in the coming weeks.
Making vaccination a condition of deployment in care homes will help ensure that residents at high risk from COVID-19 either due to their age, underlying health conditions, or disability are better protected against the virus. The consultation set out our proposal to amend regulations to require care home providers with at least one resident over the age of 65 to deploy only those workers who have received their COVID-19 vaccination (or have a legitimate medical exemption from vaccination).
The consultation asked for views on whether people supported the proposed legislative change, the scope of the policy, proposed exemptions, implementation methods; and sought views on equality impacts and impact on maintaining safe levels of staffing and the workforce.
DHSC undertook thorough analysis of the more than 13,500 consultation responses and considered the feedback received. Overall, the consultation showed that, while a majority (57%) of respondents did not support the proposal, the responses from the adult social care sector were mixed, with some group, for example care home providers mostly supporting the proposed legislative change while others, such as service users and relatives of service users were mostly opposed.
Regarding policy scope, the consultation has shown very clearly that the initial scope of including only CQC-registered care homes with at least one resident over the age of 65 would be extremely challenging to implement (a birthday or a death could see a home moved into or out of scope, respectively), that it would not protect all residents who are clinically vulnerable to COVID-19, and that it might give rise to unintended consequences such as the risk of someone turning 65 being moved to avoid a home falling within scope of the policy.
Similarly, respondents were not in favour of limiting the scope to include only paid staff deployed in the care home and volunteers deployed to carry out regulated activities. There was significant support for broadening the policy to include all those coming into close contact with residents or all those entering care homes, in any capacity. There was also some support for broadening the policy to all health and social care staff, in any NHS or social care setting.
The majority of respondents agreed with our proposal to grant exemptions on medical grounds, as outlined in the proposal. There were also calls for exemptions for visiting emergency services who need to enter care homes and for women of childbearing age who are trying to get pregnant, are pregnant or are breast-feeding. There was a call for ensuring that the system for demonstrating vaccination status or exemption from vaccination is as simple and clear as possible.
The consultation showed that respondents were concerned about the potential impact of the policy on staffing levels, as well as the potential for disproportionate impact on those with protected characteristics, such as pregnant women and people from particular ethnic minority backgrounds. We will set out our proposals for mitigating actions in relation to each of these concerns under the relevant sections of this report.
In response to the consultation, and in order to protect all care home residents who are clinically vulnerable to COVID-19, the government will be bringing forward regulations to require all CQC-regulated service providers of nursing and personal care, in care homes in England, to allow entry to the premises only to those who can demonstrate evidence of having had a complete course of an authorised COVID-19 vaccine (or evidence that they are exempt from vaccination). The requirement will only apply indoors and will exclude residents; friends or relatives of residents who are visiting; persons providing emergency assistance or urgent maintenance work in the care home; and those under the age of 18. We are working with NHSX to explore the use of the NHS App (and its web-based or non-digital alternative) as evidence for demonstrating vaccination or exemption status.
Based on feedback received during the consultation, we have made three key changes to the proposals set out in the original consultation document:
- we are extending the scope of the policy to all CQC-registered care homes, in England, which provide accommodation for persons who require nursing or personal care, not just those care homes which have at least one person over the age of 65 living in their home
- we are extending the requirement to be vaccinated to include all persons who enter a care home, regardless of their role (excluding those that have medical exemptions; residents of that care home; friends and family of residents who are visiting; those entering to assist with an emergency or carrying out urgent maintenance work ; and those under the age of 18). The requirement will apply to any professionals visiting a care home, such as healthcare workers, tradespeople, hairdressers and beauticians, and CQC inspectors. The requirement will not apply to people who only work in the outdoor surrounding grounds of care home premises
- the initial proposals set out that individuals will be exempt from the requirement if they have an allergy or condition that the Green Book lists (COVID-19: the green book, chapter 14a) as a reason not to administer a vaccine. We will also provide exemptions for those entering to assist with an emergency or carrying out urgent maintenance work; those under the age of 18; and clinical trial participants. We intend to publish further guidance to describe, in more detail, the scope and process for granting exemptions, which will continue to be informed by the Green Book
3. Methodology
The survey hosted on GOV.UK comprised three different types of questions: (i) quantitative, (ii) qualitative and (iii) open-ended. Responses to the open, qualitative questions were analysed using a topic modelling and tagging system. This identified and labelled emerging themes and topics in the responses for every question and allowed responses to be tagged with multiple themes.
Responses to the consultation are not representative of the groups referenced, but only of those who chose to respond to the consultation. Where particular groups are referred to or compared for example, adult social care workers are most likely to say… it is understood that this refers only to adult social care workers responding to the consultation and cannot be taken to represent the views of the adult social care workforce more generally. As such, statistical significance testing has not been used to analyse results. Differences between responding groups have been highlighted using judgement.
The accompanying data tables compare the demographics of the responses to the consultation to the English population and English social care workforce demographics. Notably, 72% of respondents identified as female and 18% as male. While this is not representative of the general population, 82% of the social care workforce identify as female and 18% as male[footnote 4].
Due to a technical problem, 5 questions (plus 2 follow-up questions) were inadvertently hidden from respondents over the first week of the consultation and had received no response. On 21 April 2021, this was rectified for all further respondents. We had received 6,543 responses on or before that date. The previously missing questions were subsequently emailed to respondents who both had not been able to answer them and who had given us permission to contact them. We received 958 responses to the emailed question set.
All the responses received were classified into 8 categories of respondents:
- Care home providers
- Adult social care representatives
- Other adult social care providers
- Members of the adult social care workforce
- Local government representatives
- Service users/relatives of service users
- Health care providers
- Members of the public.
The number of respondents in each of the categories is set out in the accompanying Excel tables. Over a quarter of respondents (28%) told us they were responding as a member of the social care workforce. A further 11% stated that they were responding as a care home provider and approximately 3% as another adult social care provider.
Respondents who answered as an individual receiving personal care or support; as the family, friend or carer of a person receiving care; and respondents who answered as a member of the public each comprised 23% of the total. Finally, 3% of respondents said they were responding as a representative of local government or an NHS partner; and 2% said they were an adult social care representative organisation or group.
4. Detailed government response to the issues raised
4.1 Proposed legislative change
The consultation responses showed clearly that opinions differ on whether to make vaccination a condition of deployment in care homes. This mirrors the views reflected through our engagement with stakeholders. We also note that support varies greatly by type of respondent. While, overall, a majority of respondents (57%) did not support the proposal, the views of the adult social care sector were mixed. Care home providers were most likely to support the policy (76% supportive or rather supportive). Others who tended to support the proposal included other adult social care providers (52%), adult social care representative bodies (52%) and representatives of local government (50%) who were all more likely to support the policy. Others, such as service users and relatives of service users were mostly opposed to the proposal. The most divided group was members of the adult social care workforce, with just under half (47%) supporting the policy and half (50%) not supporting the policy.
Noting the concerns of some respondents about vaccine safety, efficacy and potential side effects, we want to emphasise that vaccines are the best way to protect people from COVID-19 and have saved thousands of lives. Any vaccine available in the UK will be approved by the independent regulator, the Medicines and Healthcare products Regulatory Agency (MHRA), only when it has met robust standards of effectiveness, safety and quality. Approved COVID-19 vaccines will be monitored continuously after roll-out, by the MHRA and Public Health England (PHE), to ensure that the benefit of the vaccines continues to outweigh any risk, and to review vaccine effectiveness in response to new variants of concern.
We recognise that some respondents who did not support the proposed policy felt that workers should have freedom of choice with regard to vaccines, while others who did support the proposal expressed the view that there is a duty of care to protect people who are most at risk of serious illness from COVID-19 by having a vaccine. We want to emphasise that we never again want to return to a position of widespread COVID-19 outbreaks in care homes in which too many people living and working in care homes lost their lives. We are not forcing anyone to take the vaccine, but we must ensure the safety of the people in our society who are most at risk from COVID-19, as our first priority. Throughout the pandemic we have had to take difficult decisions, balancing individual choices against the wider risks to those people most vulnerable to COVID-19. Vaccination is a safe and effective way of preventing the spread of COVID-19 - the majority of care home workers have already taken it up. It is essential that all those who can have the vaccine to take it, in order to protect people in their care who are at risk from COVID-19 and its complications.
As set out in the introduction to this document, we have received advice from the SAGE Social Care Working Group that 80% of staff and 90% of residents, in a care home, need a first vaccination dose to provide a minimum level of protection against outbreaks of COVID-19[footnote 5], and that higher coverage and having a second dose of the vaccine would result in more protection.
Since we launched the consultation, further evidence has emerged of the effect of vaccination on transmission of COVID-19. Research by PHE[footnote 6] shows that those who do become infected 3 weeks after receiving one dose of the Pfizer-BioNTech or AstraZeneca vaccine were between 38% and 49% less likely to pass the virus on to their household contacts than those who were unvaccinated.
Taking the evidence above into account, we see a clear public health rationale to protect residents in high-risk settings who are most at risk from COVID-19 and its complications by driving vaccination uptake in care homes and ensuring high staff vaccination levels are maintained. We also note that significant parts of the adult social care sector (providers and workforce) do support the proposal.
It is our view that this combination of consultation responses and clear public health evidence provides a strong foundation on which to proceed with the policy. This is based upon minimising transmission of COVID-19 and protecting residents in high-risk settings who are most vulnerable to severe illness and death as a result of contracting the virus. We have also carefully considered how to ensure that the policy is proportionate and have provided exemptions for certain groups of people, including medical exemptions.
4.2 Policy scope
The majority of respondents did not agree with the proposed definition of “any care home which has at least one person over the age of 65 living in their home in England and which is registered with the Care Quality Commission” to determine which care homes these regulations would apply to, and specifically had concerns with limiting the policy to care homes with older adults.
We note the calls for staff caring for younger adults with people with a learning disability and autistic people or other vulnerabilities to be treated in the same way as staff caring for older adults. We recognise that respondents and stakeholders made the case that, if the policy were to proceed, it should be broadened to cover these groups. The case for broadening the scope has also been advocated by representatives of the learning disability sector. Analysis by Public Health England[footnote 7] showed that the pattern and number of deaths in care homes for people with a learning disabilities and autistic people (which are typically small, often with less than 10 beds) in the spring of 2020 was similar to the number of deaths in small care homes registered for other groups (mainly older people).
We have also received further advice from the SAGE Social Care Working Group, which has identified care homes for adults with a severe disability at any age, as well as care homes for older adults, as being high-risk settings for outbreaks of COVID-19; and where maintaining high levels of staff vaccination could prevent severe disease and transmission. Therefore, there is a strong clinical rationale for implementing the policy in all residential care homes, in the first instance, since they are all closed settings.
We have taken on board feedback from the Care Quality Commission (CQC) that its registration data does not record the age profile of service users, as well as concerns from stakeholders that a care home could move into or out of the scope of this policy overnight, following the 65th birthday of a service user or if a service user aged over 65 were to die.
We recognise the concerns raised that the rationale for protecting residents is not limited to people over 65, as there are many individuals vulnerable to COVID-19 outside of this group. We recognise the calls that, if the rationale is to protect those most vulnerable to COVID-19, then this policy should be extended to other settings where these people receive care.
We note that some respondents would like to see the requirement extended even further, so that it applies across all health and social care settings both for simplicity and for parity between health and social care staff (across NHS, domiciliary care etc.).
According to advice from the SAGE Social Care Working Group, there is no clinical evidence to suggest any difference in workplace transmission between social care and NHS settings. That said, older people in care homes are at the highest risk of severe outcomes from COVID-19, which is why we have consulted on these settings initially. However, it has become clear that there is a case for extending the scope of the policy to other high-risk groups and settings such as younger people’s care homes and hospitals. We are therefore considering whether this should be an ongoing requirement which could be applied across health and social care. There is also the question of whether the policy should be extended to other vaccines, such as the flu vaccine.
Widening the scope to cover the healthcare sector and all of social care, or the flu vaccine, is beyond the scope of this consultation. Therefore, we have decided, initially, to proceed with applying the policy in all care homes providing accommodation for persons who require nursing or personal care, while also launching a public consultation in the coming weeks on making COVID-19 and flu vaccination a condition of deployment in healthcare and the wider social care sector, to protect patients and the people they care for from becoming seriously ill or dying from these deadly diseases. This is a complex and important issue, which is why we want to gather a wide range of perspectives from across the health and care sector about whether this should be introduced and how it could be implemented.
On the basis of the consultation, we have made the following change to the initial proposal:
Change 1: We are extending the scope of the policy to all CQC-registered care homes, in England, which provide accommodation for persons who require nursing or personal care, not just those care homes which have at least one person over the age of 65 living in their home.
Regarding which people working or visiting a care home should be covered by the scope of the policy, we note that the baseline proposal of “only paid staff deployed in the care home” was the least popular option (30% support).
We recognise that there was significant support for broadening the scope of the policy to include all those coming into close contact with residents; or all those entering care homes, in any capacity. We have carefully considered a range of options regarding the extent to which the policy should be extended to other working or visiting adults in care homes.
While we recognise calls that the policy should include family members who are designated as essential care givers, visits from family and friends are vital for the health and wellbeing of people living in care homes. Public Health England have advised that members of this group should be encouraged to get vaccinated; but if they cannot or will not, it would be unjustifiably detrimental to residents to deprive them of contact with, and care from, their loved ones. In these cases, other Infection Prevention and Control mitigations should be used.
Similarly, we note that respondents feel that the most important criterion was the closeness of contact with care home residents and the length of time the contact is likely to last. However, we have been advised by the SAGE Social Care Working Group that, given what is known about within-workplace social networks, vaccination of staff who do not provide direct personal care should be strongly encouraged. Depending on the size and configuration of the care home, there may be staff on site who never come into contact with clients. However co-worker networks have been shown to be an important factor in transmission[footnote 8] and, where there is co-location, unvaccinated staff remain a potential source of introduction, though direct transmission to residents.
We note the concerns of some respondents that, if all visiting professionals were to be included, the requirement could prevent emergency services from operating. We can provide assurance that there will be an appropriate exemption for persons coming into care homes for the purposes of providing emergency assistance, including urgent maintenance work.
Based on feedback on who should be within scope of the policy, we made the following change to the original proposal:
Change 2: We are extending the requirement to be vaccinated to include all persons who enter a care home, regardless of their role (excluding those that have medical exemptions; residents of that care home; friends and family of residents who are visiting; those entering to assist with an emergency or carrying out urgent maintenance work ; and those under the age of 18). The requirement will apply to any professionals visiting a care home, such as healthcare workers, tradespeople, hairdressers and beauticians, and CQC inspectors. The requirement will not apply to people who only work in the outdoor surrounding grounds of care home premises.
4.3 Exemptions
We note that the majority of respondents agreed with our proposal in the consultation to grant exemptions on medical grounds. We also recognise that a significant proportion of all respondents feel that there should be no exemptions and that all visitors to care homes should be vaccinated, while others advocate that we should widen the exemptions (e.g. to those who are pregnant, breastfeeding or hoping to conceive; and on religious grounds).
We have carefully considered the different options, to strike a balance between the range of views submitted, on what is a complex issue. Permitting limited exemptions will help to ensure that the requirement does not exclude, or impose a disproportionate burden on, certain individuals. It is also important to ensure that the scope of exemptions does not undermine the public health benefits of the policy, or create a system that can be used by individuals to circumvent the requirement.
The requirement will only apply indoors and will exclude residents; friends or relatives of residents who are visiting; persons providing emergency assistance or undertaking urgent maintenance work in the care home; and those under the age of 18.
We will also provide exemptions for individuals where vaccination is not clinically appropriate, for example a pre-existing diagnosis of anaphylaxis. Guidance will give more detail about exemptions, which will reflect the Green Book on Immunisation against infectious (COVID-19: the green book, chapter 14a) and clinical advice from the Joint Committee on Vaccination and Immunisation (JCVI). The guidance will also set out suitable grace periods after a temporary exemption has expired.
For those who are exempt, who will be able to be deployed in the care home, we will work with stakeholders to produce guidance on steps that should be taken to mitigate the risk of COVID-19 transmission to residents.
We have considered exemptions for those who hold, and refuse the vaccine due to, religious beliefs and opted not to provide this exemption. Such an exemption would be difficult to implement and prove and would likely significantly reduce the impact of the policy in achieving its aims of increasing levels of protection for both residents and staff. It may also cause tension between those who have been exempted, and other staff who have received the vaccine, as a condition of deployment.
Noting the concerns raised about rare blood clots as a side effect of vaccinations, we will ensure people under the age of 40 will be offered an alternative to the Oxford/AstraZeneca vaccine, in line with the Green Book on Immunisation against infectious diseases (COVID-19: the green book, chapter 14a) and clinical advice from JCVI.
We have considered the concerns raised about pregnancy. We have been assured by clinicians that vaccines are safe for the majority of pregnant women, however we recognise that in some circumstances, vaccination may not be appropriate during pregnancy and we will consider that in our guidance regarding granting exemptions.
Change 3: The initial proposals set out that individuals will be exempt from the requirement if they have an allergy or condition that the Green Book lists (COVID-19: the green book, chapter 14a) as a reason not to administer a vaccine. We will also provide exemptions for those entering to assist with an emergency or carrying out urgent maintenance work; those under the age of 18; and clinical trial participants. We intend to publish further guidance to describe, in more detail, the scope and process for granting exemptions, which will continue to be informed by the Green Book.
4.4 Implementation
We note that there is very strong support among both managers and staff for the use of a digital solution or app to demonstrate vaccination status. We have recognised this and plan to offer an option to evidence vaccination status via the NHS App.
In response to concerns that not all people covered by the policy have access to a smart phone, we can provide reassurance that we intend to provide a web-based solution for people who do not have access to the app, as well as a non-digital solution, in the form of a letter.
While, overall, respondents were split on whether the policy would be easy or difficult for managers to implement, we take on board feedback that small care homes will find the policy much more challenging to implement. We are exploring steps to mitigate this risk, including working with Skills for Care to ensure that local authorities and providers will have access to guidance and resources to support workforce capacity and resilience, in light of this policy.
We have taken on board the need for a suitable grace period for implementation of the policy and have amended the legislation accordingly to include a 16-week grace period from when the regulations come into force. We have recognised the calls for an Impact Assessment and intend to publish this as soon as it is possible to do so.
5. Impact and implications
We recognise that there are concerns about the potential impact of the policy on maintaining safe staffing levels if staff decide to leave as a result of the policy, and the concerns of Local Authorities and NHS partners about the impact of the requirement on their ability to commission services.
We want to emphasise that the majority of those who work in care homes have already taken up the vaccine and we will continue to encourage people working in care homes to take up the offer going forward.
To mitigate the risk of an immediate effect on capacity, we have included a 16-week grace period. This would enable the vast majority of workers to receive both vaccination doses and should therefore minimise the risk of sudden departures from the workforce. We are looking to deliver another National Recruitment Campaign in order to attract people into the sector and promote adult social care careers.
We are working with Skills for Care to ensure that resources such as guidance and best-practice are available to support providers and local authorities with capacity and workforce planning, recruitment and well-being. Skills for Care will also provide local and national workforce support to local authorities and employers. We will also work with local authorities to ensure they are contingency planning and accessing additional support, as well as promoting joint working across a region to assist with targeted recruitment.
DHSC continues to liaise with local authorities and stakeholders to continue to learn about the guidance needed to smooth the process for implementation.
A number of respondents have raised concerns that younger adults with a learning disability and autistic people who live in care homes would be disproportionately affected if they were not included in the policy. We have taken this feedback on board and have extended the requirement to all CQC registered care homes in England (see change 1).
We are addressing concerns about access to vaccination and will continue to promote access for care workers and other people who are within scope of the policy to make it as easy as possible to take up the offer of vaccination. We will also continue to ensure that vaccine guidance and information is readily available in a variety of formats such as easy-read, large print and Braille, as well as being accessible via screen readers and in different languages.
We recognise concerns that certain groups within the workforce may be more vaccine-hesitant and therefore could be negatively impacted by the policy. We are also providing tailored support to key groups in the workforce. This is designed to build confidence among:
- women of childbearing age. We are working with clinical experts to address their questions and concerns about the vaccine, including concerns around pregnancy and fertility, for example these issues were addressed during a webinar for social care workers on 21 May 2021, hosted by Minister Zahawi
- people from Black, Asian and Minority Ethnic groups who may be hesitant about taking the vaccine. We are delivering tailored communications and working in partnership with trusted community leaders
- people with concerns about the vaccine, based on religion or belief, including, for example, by sharing information to tackle common concerns about vaccine ingredients or the safety of vaccines
We have published a Public Sector Equality Duty (PSED) Assessment alongside this response and will carefully track the impact of the policy on vaccine uptake, once it has been implemented.
To address the concerns raised by care providers regarding potential inadvertent breaches of data protection law, we have inserted a provision in the regulations so that a service provider may process information provided by a person wanting to prove their vaccination status, in accordance with the Data Protection Act 2018.
6. Analysis
The full data used in this section can be found in the accompanying Excel tables.
6.1 Proposed legislative change
How do you feel about the proposed requirement for workers in older adult care homes to have a COVID-19 vaccination?
Over 13,500 responses were received to the consultation, of which over 80% were from individuals.
Overall, around three in five respondents did not support the proposed policy (57% not supportive or slightly unsupportive), and two in five (41%) said they were supportive or rather supportive. Respondents to the consultation expressed strong feelings on this subject, with the proportion who were supportive or not supportive being substantially greater than the proportion who were rather supportive or slightly unsupportive.
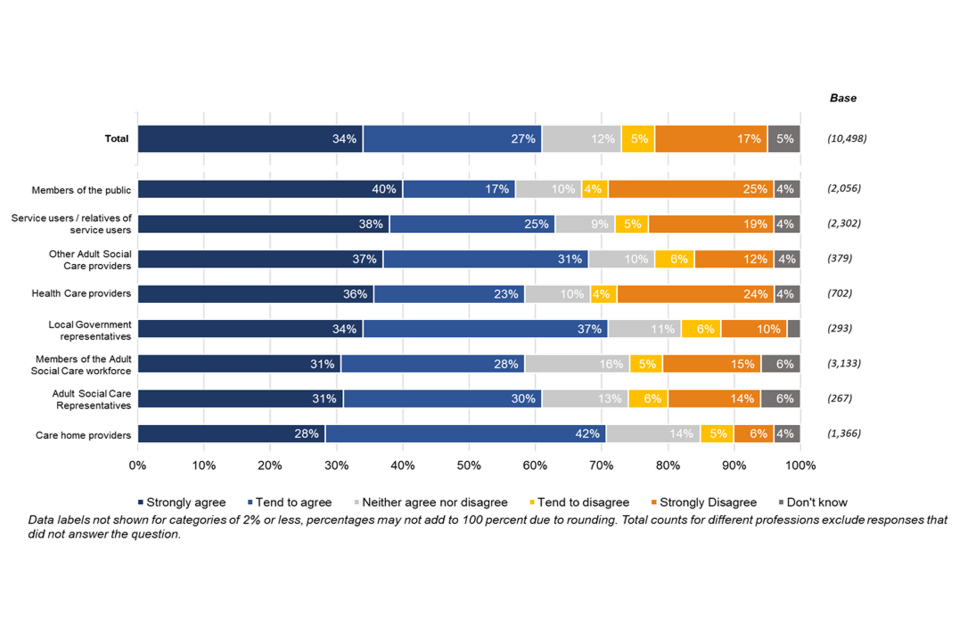
Figure 1: How do you feel about the proposed requirement for workers in older adult care homes to have a COVID-19 vaccination? By type of respondent
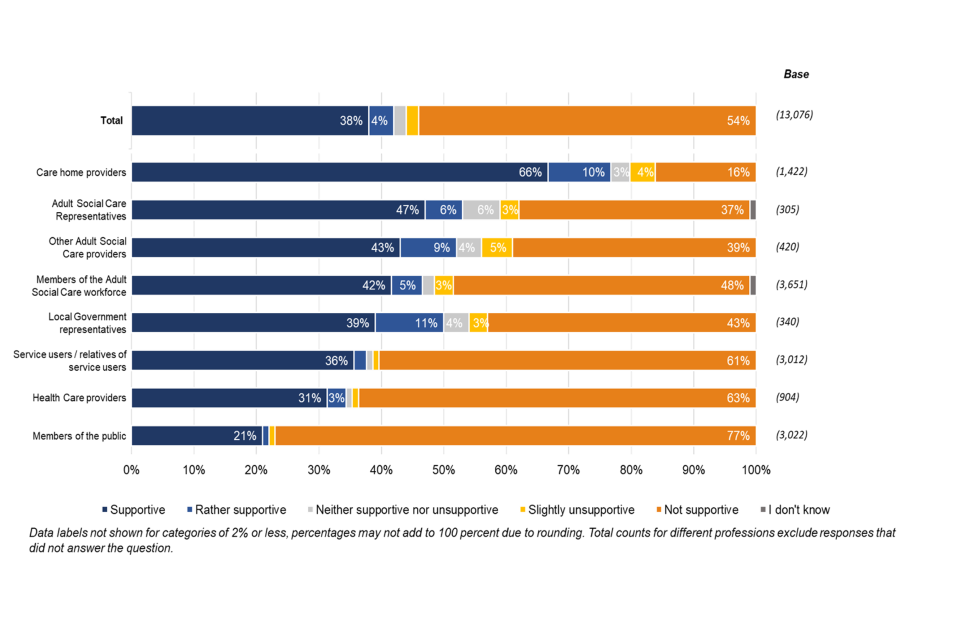
Support differed greatly by type of respondent, with care home providers most likely to support the policy (76% supportive or rather supportive). Others who tended to support the proposal included other adult social care providers (52%), adult social care representative bodies (52%) and representatives of local government (50%) who were all more likely to support the policy. Members of the public were least likely to express support, with only around one in five in support (22%) compared to more than three in four (77%) who did not. Members of the adult social care workforce were split in their support, with 47% in support and 50% not supporting it.
Among those who did not support the policy, the main reasons mentioned were that the policy is potentially an infringement of the human rights of workers and that workers should be free to choose whether to have the vaccine, together with concerns about its morality, legality and impact on people’s bodily autonomy.
A notable number of respondents also expressed scepticism and suspicion about the vaccine itself. Members of the public were more likely to express vaccine suspicion than other groups.
Other reasons mentioned for not supporting the policy were the difficulty of recruiting new staff under the proposed requirements and concerns around the safety, necessity and effectiveness of vaccination. Those who supported the policy cited a belief that there should be a professional duty of care incumbent on care workers and the need to protect the vulnerable residents they look after. A large number of those who supported the policy felt that it should apply to health and social care workers alike. Care home providers were the most likely to support widening the deployment conditions of the policy.
Views from organisations that responded to the consultation
The views from the organisations responding to the consultation were broadly in line with those of care home providers. They highlighted the increased protection offered to vulnerable residents and to their carers by the vaccine.
We support the right of care home residents to be kept safe in their home. Workers too deserve to be kept safe and vaccination can help with that.
They also noted that making vaccination as a condition of deployment would offer a clear and unified approach that ensures consistency across providers, particularly given the significant regional variation in uptake.
Mandating vaccines for staff who do not have a medical exemption would be the next step along the road to increasing safety within our homes.
However, they questioned whether changing the condition of deployment is a proportionate, fair and effective strategy to achieve greater protection from COVID-19.
Visiting professionals, families and friends, external medical services, day centre, workplaces etc. are all part of the world our service users inhabit, so let’s create pathways which encompass the whole, not just part, of the lives of our service users and residents.
It was highlighted that, despite regional variation, voluntary vaccination uptake is rising. Respondents suggested that other, less intrusive methods could suffice to further increase uptake.
There is an ethical imperative to prioritise and pursue the least intrusive means of achieving high vaccine coverage in the first instance, before considering other interventions.
Examples of such interventions included declination statements (used to express the decision to not get vaccinated), providing more education, encouraging communication, easing access to the vaccine, and providing financial incentives. The benefit of vaccination was acknowledged, but it was not deemed to be the only option to create a safe environment. Some respondents expressed unease over the ethical implications of the policy, highlighting concepts such as individual autonomy, dignity, privacy and equality.
Putting pressure on people to be vaccinated would have a detrimental effect on uptake because having choice is perceived to be important.
Respondents had concerns about the scope of staff affected by the proposed regulations and the resulting impact on the workforce.
Care home staff have been under an extraordinary amount of pressure during the pandemic – they are a skilled workforce which is under-staffed, under-paid and under-appreciated.
Some respondents proposed mitigating the impact on the workforce by enforcing the condition of deployment for new starters only, as part of their occupational health screening. Others mentioned the need to integrate other health care professionals into the scope of the policy, such as the wider social care workforce and NHS staff. This argument was based on health security concerns, for example GPs, nurses and other health and care professionals would be in contact with multiple vulnerable residents across various settings Limiting this policy to part of the social care workforce would discriminate against this workforce. It was also mentioned that the vaccination of agency staff, staff working under zero-hour contracts, and staff vaccinated abroad should be regulated equally.
Respondents mentioned concerns about the impact on staffing levels.
Some members reported a dissonance around not wanting to support the consultation because of its potential impact on critical sector issues such as the ability to recruit and retain a social care workforce yet recognising the importance of protecting the people they support.
Concerns included the loss of skilled and experienced staff and increasing difficulty of recruitment in the future. Respondents highlighted the risk that staff shortages could lead to a shortage of care options and further increase the pressure on the sector. Providers in particular expressed concern about the likelihood of facing employment tribunals and of increased staff movement if their standard workforce were to decrease.
Concern was expressed about the lack of clarity on the duration and scope of the policy. These respondents were unsure whether the policy applied only to the first two doses of the vaccine or whether it also included boosters or further vaccinations that might become necessary due to new variants of the virus.
Additional concerns included the extension of the policy to cover seasonal flu vaccination and the implications for further restrictions on care homes. Questions were also asked about the role of CQC and the definition of deployment. There were also some requests for a Regulatory Impact Assessment to be carried out.
6.2 Policy scope
Do you agree with using this definition to determine which care homes this regulation would apply to?
Nearly two in five (37%) respondents agreed that the definition of the care homes to which this regulation would apply is correct, while nearly three in five (57%) thought that it is not correct.
Figure 2: Do you agree with using this definition to determine which care homes this regulation would apply to?
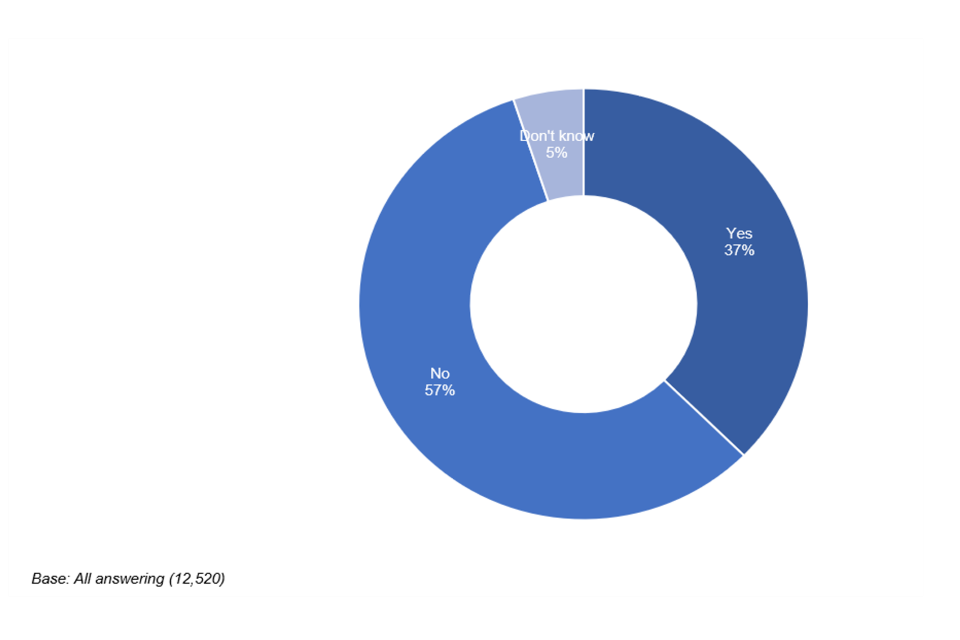
Care home providers (66%), and adult social care representative organisations (47%) were both more likely to agree than to disagree that the definition is correct. Members of the public were most likely to disagree with the definition (74%). Healthcare providers (65%), representatives of local government (63%) and care service users and their relatives (62%) were also more likely to disagree.
Half the members of the adult social care workforce (50%) who responded did not agree with the definition. Of this group, 68% of registered managers and 63% of directors or proprietors agreed. However, 63% of other frontline health or social care workers disagreed.
What concerns do you have about this definition?
Respondents who voiced concerns about the definition repeated concerns on the overall policy proposal, human rights, bodily autonomy and believed the proposal to be unethical or immoral. A substantial number quoted concerns around the safety or efficacy of the vaccine or were suspicious of vaccines in general.
Among those respondents who focused specifically on the definition of care homes within the policy, the most frequently expressed concerns were that all care and healthcare settings should be included and that younger adults with a learning disability or other vulnerabilities and autistic people should also be in scope of the policy. These were raised both by supporters and non-supporters of the policy proposals overall.
Views from organisations that responded to the consultation
Among these organisations, some respondents expressed concern about the definition in this proposal, which was deemed too narrow and unclear.
As such, what constitutes an ‘older persons care home’? Therefore, there will not be a clear line drawn as to which care settings meet the eligibility criteria for this policy.
Do you have any concerns about the proposal to limit this policy to older adult care homes?
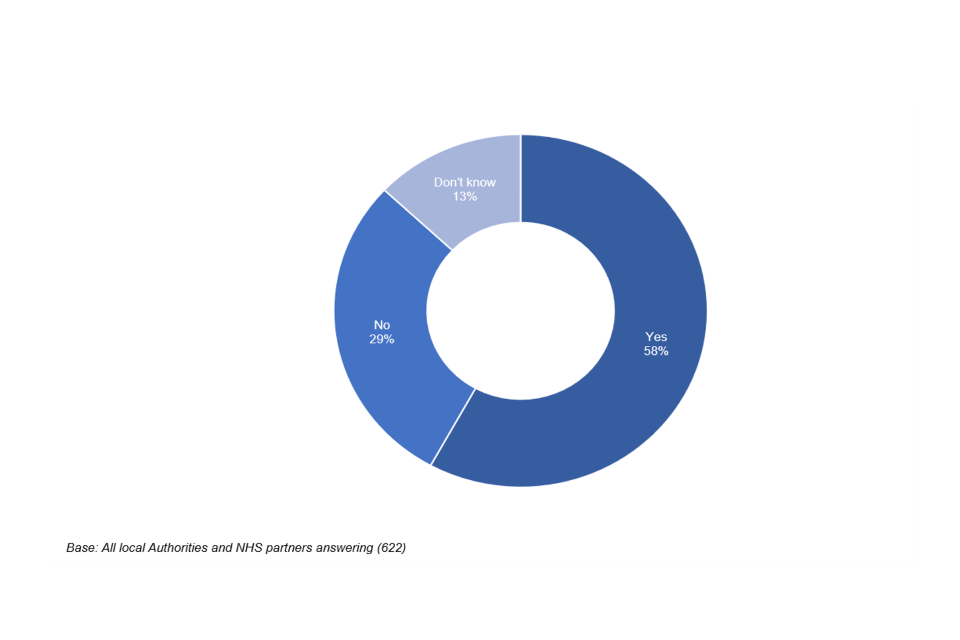
Almost three in five (57%) respondents said that they had concerns about the proposal to limit this policy to older adult care homes. One in three (29%) said that they had no concerns. Just over one in ten (13%) did not know.
Figure 3: Do you have any concerns about the proposal to limit this policy to older adult care homes?
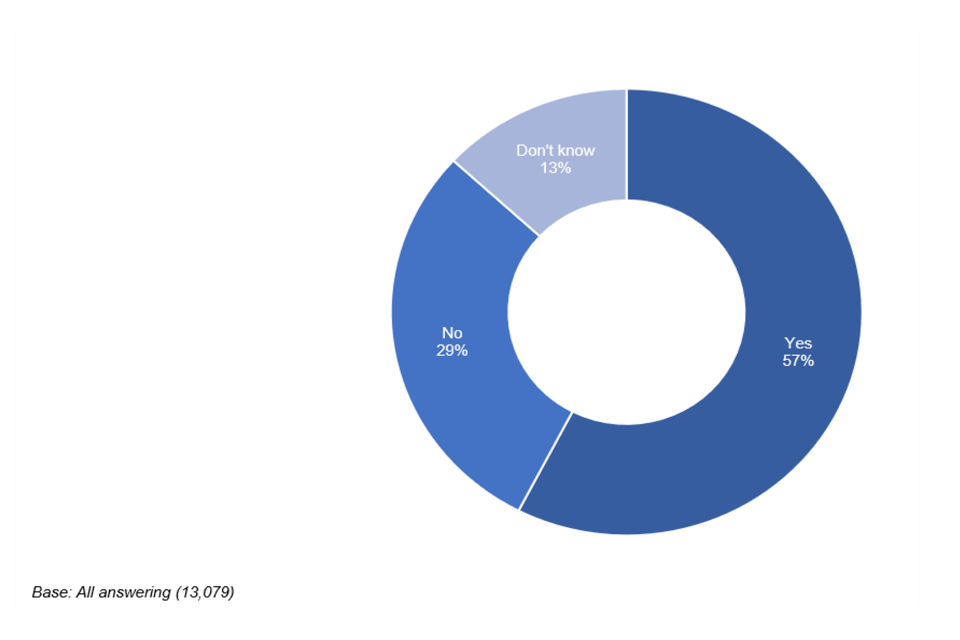
Similar concerns were raised by those who did not support the policy overall - human rights, bodily autonomy and concerns about the vaccine itself. Several respondents, among those who supported the policy proposals as well as among those who did not, said that younger adults with a learning disability or other vulnerabilities and autistic people as well as other health and care settings should be included.
Views from organisations that responded to the consultation
There was a general view from organisations that, should the conditions of deployment change, this policy should be applied to all carers of vulnerable people, including all types of care homes. Some respondents highlighted that, in addition to older age, learning difficulties, mental impairment and physical disabilities in younger adults are also vulnerabilities that deserve increased protection.
The policy should cover all health and care staff in all settings who come into contact with people receiving care and support (including health care settings and other care settings).
There were concerns that limiting this policy to older care homes will risk establishing double standards for NHS staff and care staff.
The risk with this selective approach is that older adult care home workers will feel alienated and marginalised, potentially adversely impacting recruitment and retention, which is so essential for the delivery of safe and quality care.
Other respondents mentioned the risks associated with unvaccinated NHS staff providing care or services, particularly with many healthcare staff working across multiple care homes.
Which people working or visiting in an older adult care home should be covered by the scope of the policy?
The majority of respondents did not agree that the other proposed groups should be added into the scope of the proposed policy, although the following were most likely to be selected as potentially within scope: roles involving the provision of close personal care to residents, such as health professionals (49%), friends or family providing essential care (46%) and ‘other professionals’ providing personal care, such as hairdressers (46%).
Figure 4: Which people working or visiting in an older adult care home should be covered by the scope of the policy?
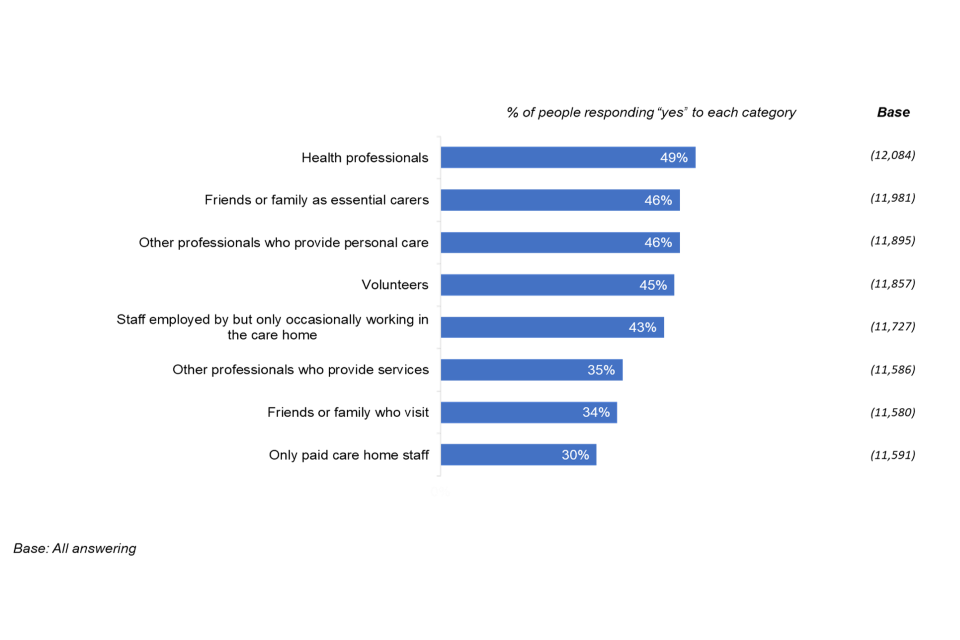
Views from organisations that responded to the consultation
There was a very wide range of opinions regarding the extent to which the policy should be extended to other working or visiting adults in care homes. Many responses suggested extending it to all staff providing close contact care, such as district nurses, occupational therapists and other visiting professionals but not to administrative staff. Others said that all staff, whether regular or visiting staff, care or administrative staff (such as CQC inspectors) should be included.
Other respondents believed the policy should include family members who are designated carers. Some also thought that this should extend to hairdressers and visiting family members, even those without dedicated carer status.
It is our belief, that if vaccination is mandated, then it must be mandated for all groups that have access to care home residents, including NHS staff, third parties, visitors and family members.
Some were concerned that limiting the scope of the policy vaccination to social care staff would increase discrepancies with the NHS.
The proposed change in regulation highlights the disparity between the health and social care sector, NHS staff are not being subjected to the same requirements as adult social care staff.
All respondents felt that a proportionate response was needed to address this issue, and that further clarification on temporary staff such as contractors was needed.
6.3 Exemptions
Do you agree or disagree with the groups of people who would be exempt from this requirement?
Three in five (61%) respondents agreed that these groups should be exempt from the requirement. Just over one in five (22%) disagreed. Local government representatives (71%) and care home providers (70%) were most likely to agree with exemptions for these groups. Members of the public, members of the adult social care workforce and healthcare providers were least likely to agree (57%, % and 59% respectively).
Figure 5: Do you agree or disagree with the groups of people who would be exempt from this requirement? By type of respondent
Who else should be exempt from this requirement?
The majority of respondents those who disagreed with the proposed policy felt that everyone should be exempt, while a substantial number of those who supported the proposals felt that there should be no exemptions and that all visitors to care homes should be vaccinated.
A number of respondents mentioned that other groups such as those with allergies or medical exemptions, those who are pregnant, breastfeeding or hoping to conceive and those seeking an exemption on medical or religious grounds should also be exempt.
Views from organisations that responded to the consultation
Respondents wanted an implementation period whereby everyone would be exempt for a short period to consider their options. There were also calls for exemptions for visiting emergency services and for women of childbearing age, who are trying to conceive, or who are pregnant or breast feeding.
Allowing a grace period so that a worker can be vaccinated a suitable period after their pregnancy is a considerably more preferable option.
Some respondents fundamentally disagreed with the proposal and believe that all staff members should be exempt.
6.4 Implementation
Your staff would need to be able to show that they have been vaccinated. How would you prefer that they do this?
You would need to be able to show that you have been vaccinated. How would you prefer to do this?
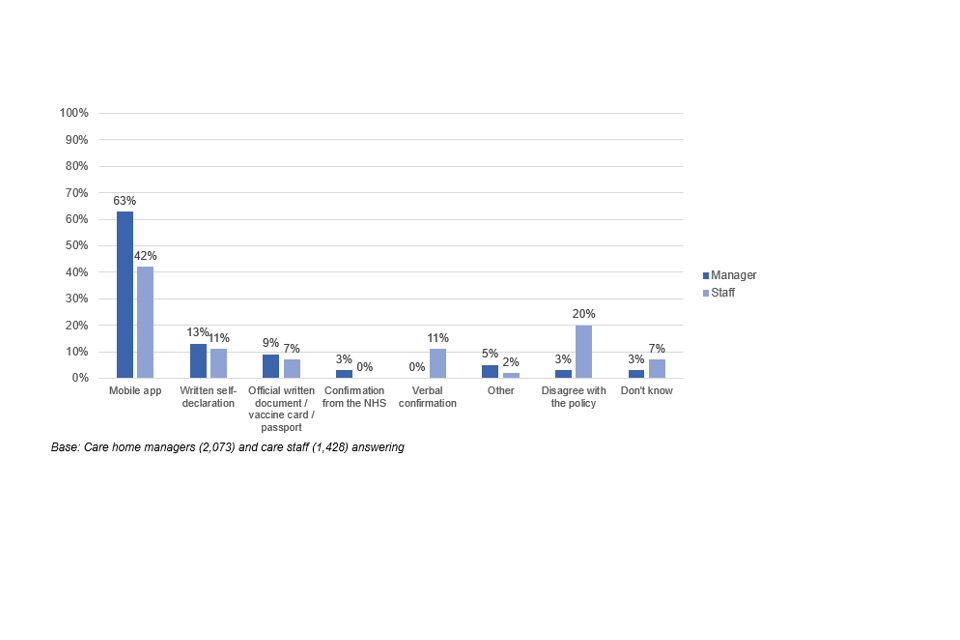
Nearly two in three (63%) care managers and two in five (42%) care staff said they would prefer to use a mobile app to show vaccination status. Although the app was by far the most popular option, many respondents commented that not everyone covered by the policy would have access to a smart phone, and therefore if a mobile app were to be used, another option would also need to be available.
Just over one in ten in both groups would prefer a written self-declaration (13% of managers and 11% of care workers) and just under one in ten would like to see an official written document such as a vaccine card or passport (9% of managers and 7% of care workers).
Requests to use a vaccine card specifically mentioned a card such as a blood donor or ATM card, which could provide vaccine status on request or the card issued when the vaccine was administered. Some responses did not distinguish between these two methods.
Figure 6: Your staff or you would need to be able to show that they had been vaccinated. How would you prefer that they do this?
How easy will this policy be for managers in older adult care homes to implement?
All respondents were asked how easy or difficult they felt the policy would be for managers in older adult care homes to implement. Responses were fairly evenly split, with two in five respondents saying it would be easy for managers to implement (37%) and a similar proportion saying that it would be difficult (40%).
Figure 7: How easy will this policy be for managers in older adult care homes to implement? By adult social care role
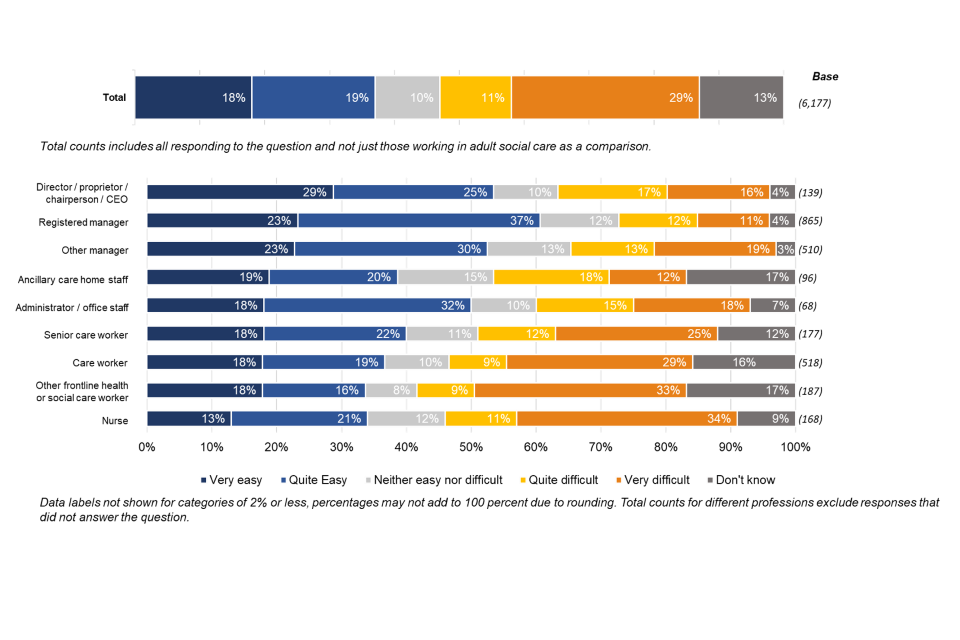
Registered managers were most likely to say that the policy would be easy for managers in older adult care homes to implement (60%), along with at least half of directors and proprietors (54%), other managers (53%) and administrative and office staff (50%). Nurses (34%), care workers (37%) and other frontline health and care workers (3%) were least likely to agree that the policy would be easy to implement.
Figure 8: How easy will this policy be for managers in older adult care homes to implement? By care home size
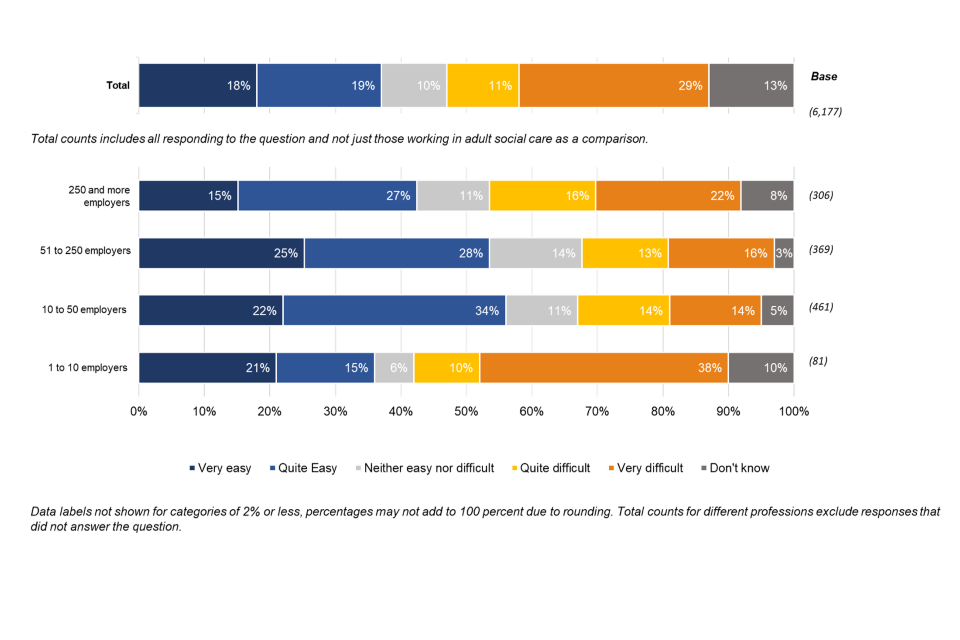
Medium-sized care homes (with 11-50 employees) and large care homes (with 51-250 employees) were most likely to say that the policy would be easy to implement – 56% of medium-sized homes and 53% of large homes said they thought this would be the case. Very large providers (250+ employees) were more cautious, with two in five (42%) saying that they would find the implementation easy. A few small care homes (10 or fewer employees) also responded. These were most likely to say that implementing the policy would be difficult (48%, compared with 36% who thought it would be easy).
Views from organisations that responded to the consultation
Care home providers asked for more clarity on the specific regulations and the division of responsibilities, mentioning, for example, that the definition of deployment is not clear. A key question related to the role of the Care Quality Commission (CQC) in guiding the implementation, providing resources and overseeing and regulating the policy. Respondents also asked for a Regulatory Impact Assessment to be carried out.
Care home providers wanted more support on how to manage and address concerns. For example, they expected to see clear reasoning for the condition of deployment as well as guidance on how to communicate this to their staff. Concerns identified by care home providers echoed the concerns raised by members of the adult social care workforce and members of the public throughout the consultation.
Concern about the longer-term impact of the vaccine on the individual; concern that the vaccine has not been tested effectively and was ‘rushed through’; concerns about the safety of the AZ vaccine linked to news reports of blood clots; “fake news” being disseminated via social media about the vaccine and COVID-19 more generally; people wanting to more time to decide on whether to take the vaccine rather than feeling pressured into it; and particularly perceived concern around the impact on fertility and pregnancy
Further, care home providers asked for more advice and guidance to cover situations where staff refused the vaccine, and support for those who decide not to be vaccinated.
Concerns were raised about the perceived differential implications of realising this policy, depending on the size of the care home, the location (areas with low vaccine uptake would make implementation harder), the levels of staff turnover (the greater the rate of staff turnover the higher the administrative effort), and the reliance on agency staff (where implementation is perceived to be more difficult to administer).
Respondents expressed concern about the legal and contractual issues around implementation.
[It will be] quite difficult to implement for managers given that they will need to consider various data protection requirements, health and safety requirements, equality and human rights issues, and the employment contracts of its employees, before such a policy could be implemented.
Care home providers mentioned the need for administrative support, for example to establish systems to capture and manage the data on vaccinations, including the need for additional funding to help manage the implementation.
The challenge of producing accurate and timely data across the care home sector is increased by the lack of digitisation within care homes […] These difficulties are compounded by: the large but fragile provider market; the reluctance of some care providers to share data that might have consequences on their finances; workforce shortages; complex financial models; and ongoing flow of residents between acute, primary, community and informal care settings.
Respondents asked for a grace period to enable care settings to implement the revised condition of deployment and to launch campaigns to bring additional resource into the care sector. They also mentioned the need for an assessment of the impact on liability insurance.
Respondents suggested that staff support for the policy would help with its implementation. Providers highlighted that voluntary vaccination uptake is high and still increasing, suggesting that with more time the desired levels would be reached without intervention. Providers mentioned their staff’s preference for working with others who were vaccinated, which would incentivise other members of staff to be vaccinated also.
6.5 Impact and implications
Do you have any concerns about the impact of the proposed requirement on your ability to commission services?
Local authorities and NHS partners were asked whether they had concerns about the impact of the proposals on the ability to commission services. Just under three in five (58%) said they did have concerns, while fewer than one in three (29%) said they did not.
Figure 9: Do you have any concerns about the impact of the proposed requirement on your ability to commission services?
The key concern among both those who supported and did not support the overall policy proposal was staffing. Respondents mentioned the potential difficulty in retaining staff due to the policy, as well as the impact on those staff who might feel compelled to leave due to implementation. There is also concern about the administrative burden of verifying the requirements, particularly in bulk in the first instance.
Many of those who did not support the policy overall cited disagreement with the policy and infringement of human rights as their main concerns.
Views from organisations that responded to the consultation
There were general concerns that the impact on staffing levels could impact the ability to commission services. One local authority noted the potential that this had to reduce the overall potential workforce.
The potential impact of mandatory vaccination in depressing the number of staff retained or applying to work in the care market, may require even higher investment in these interventions so as not to result in destabilised market and potentially put safe services at risk.
It was also mentioned that local authorities would need to establish exit routes to terminate their work with providers that do not ensure compliance with this potential legislation. This could lead to discontinuity in the provided service.
Are there particular groups of people, such as those with protected characteristics, who would particularly benefit from or be negatively impacted by this policy?
Over one in five (22%) of respondents thought that particular groups of people with protected characteristics would benefit from the policy. A much larger proportion (46%) thought that groups with protected characteristics would be negatively affected.
Figure 10: Are there particular groups of people, such as those with protected characteristics, who would…
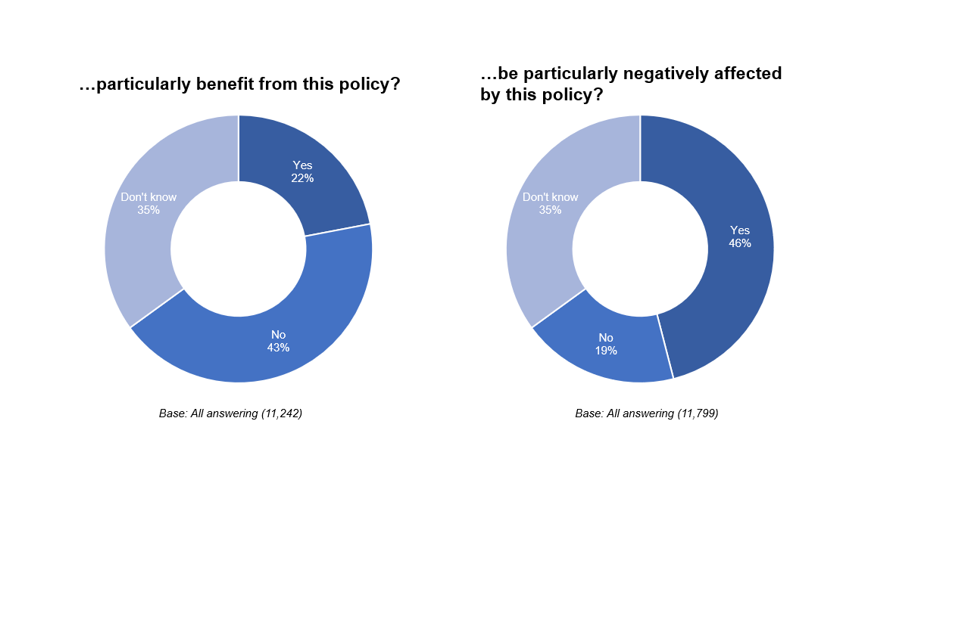
According to those in support of the policy, those who were most likely to benefit were identified as those who would not otherwise get the vaccine, with respondents identifying low uptake groups in particular, for example Black, Asian and Minority Ethnic groups, and women. They identified these groups as potentially benefiting through access to protection against the virus through vaccination, that they might not otherwise have had. Many of those who did not support the policy overall still mentioned these groups as potential beneficiaries.
Respondents also mentioned vulnerable/older people as beneficiaries of the policy.
Those who did not support the policy were more likely to think that people with protected characteristics would be negatively impacted. The majority of this group expressed general disagreement with the policy. In terms of specific groups who might be negatively affected, staff who refuse the vaccination were identified as potentially facing unemployment and associated difficulties. Respondents felt that this would fall disproportionately on Black, Asian and Minority Ethnic groups and on women, as the groups who are thought to be more vaccine hesitant. Women who are pregnant or hoping to become pregnant were also cited as being at risk of negative impact.
Respondents mentioned the possibility of negative impact on care home residents due to the potential for staff shortages and the loss of skilled staff from the workforce the welfare of residents.
Views from organisations that responded to the consultation
It was broadly accepted that the greater the number of people vaccinated, the greater the general protection against COVID-19, with older people benefitting most.
We recognise that higher take-up of the vaccine will have a positive impact across all groups and individuals with protected characteristics.
Staff and residents with immune disorders, long-term conditions and other vulnerabilities were also identified as potential beneficiaries of this policy.
Black, Asian and Minority Ethnic groups were also mentioned as benefiting from the increased protection of the vaccine, on the assumption that vaccination of care workers in this group is lower than that among white care workers.
A general point was made about the possibility of indirectly discriminating against certain members of staff by implementing this policy:
Vaccination status itself is not typically understood as a protected characteristic, but an individual’s reason for declining vaccination may be related to a protected characteristic (such as religion), [therefore] a mandatory vaccination scheme could plausibly involve indirect discrimination, even if would be unlikely to involve direct discrimination.
Respondents identified that Black, Asian and Minority Ethnic staff were most likely to be disproportionally affected by the policy.
[The policy should] be informed by understanding the particular concerns and contexts of care home employees, who are disproportionately from Black, Asian, mixed, or minority ethnic backgrounds and more likely to be vaccine hesitant, often as a result of scepticism of the government, or less able to access vaccination because of challenges relating to their employment.
Several respondents raised age-related concerns, such as the need to include other vulnerable populations aged under 65 in care homes. Some respondents said that limiting the policy to residents aged 65+ meant that any potential negative impacts on care giving, such as reduced staffing levels, would affect older care homes in particular and create disparities between care home types. Age-related concerns were also expressed about younger care staff, who might be too young to be eligible to receive the vaccine at this time.
Women were identified as being at greater risk of negative impact from the policy, as a large proportion of the workforce identify as female, and because pregnancy and maternity are protected characteristics. Respondents mentioned possible unknown impacts of the vaccine on fertility and during early pregnancy, echoing concerns raised by members of the adult social care workforce and members of the public in the consultation responses.
Some individuals within this group might feel concerned about any as yet unknown effects of the vaccine upon fertility or upon early pregnancy.
One respondent mentioned hearing reports about women being unable to access the vaccines recommended for pregnant women, potentially causing disadvantages for this group.
We are concerned (…) that they are pressured into taking up an offer of the AstraZeneca vaccine where there is no alternative in order to keep their employment; and second, that they risk losing employment because they want to retain their right to choice around vaccination.
Care home staff with disabilities which are not included on the exemption list were also mentioned as a group likely to experience negative impacts, due to vaccine hesitancy arising out of concerns about impact on their disabilities.
Respondents also mentioned the potential challenge to some religious and personal beliefs that care home staff might hold. There were wider concerns that the policy risks discriminating against and stigmatising those in the most deprived communities and thus increasing existing inequalities.
What could we do to make sure they are not negatively impacted?
Among those who did not support the policy, the most frequently mentioned way of avoiding negative impact was not to implement the policy. Other suggestions for mitigating negative impacts included financial incentives for vaccinations, and increased support to staff who are vaccine-hesitant along with better information to address specific concerns. Respondents also suggested that staff who decided not to be vaccinated should have support with redeployment.
Views from organisations that responded to the consultation
Increasing access to information about the vaccine and to the vaccine itself were both seen as ways to ease negative impacts.
Staff working with vulnerable people in all settings should have easy access to the vaccines and be able to have supportive and sensitive conversations to help them understand the value of vaccination and accept vaccines offered to them.
Suggestions included reopening the national booking system, providing travel costs to vaccination centres and providing paid leave to staff suffering any side effects due to vaccination. Redundancy support for workers was also recommended. Communicating facts and information regarding the vaccine and the need for the deployment requirements, through community leaders, faith leader and more experienced peers was also seen to be key to addressing vaccine hesitancy.
Many respondents suggested a delay to implementation to allow care homes time to manage workforce pressures and to make any necessary adjustments such as recruiting and redeploying staff where necessary.
Respondents suggested that if pregnant female staff were unable to access the recommended type of vaccine or decided not to have the vaccine due to concerns about its effect on pregnancy, those women should be offered suitable alternative working arrangement or suspension on full pay, equal to the options offered through workplace risk assessments for pregnant women. Other responses called for grace periods assessed on a case by case basis, for example for women who are breastfeeding.
How do you anticipate you would respond to the requirement, thinking about staff who are not vaccinated?
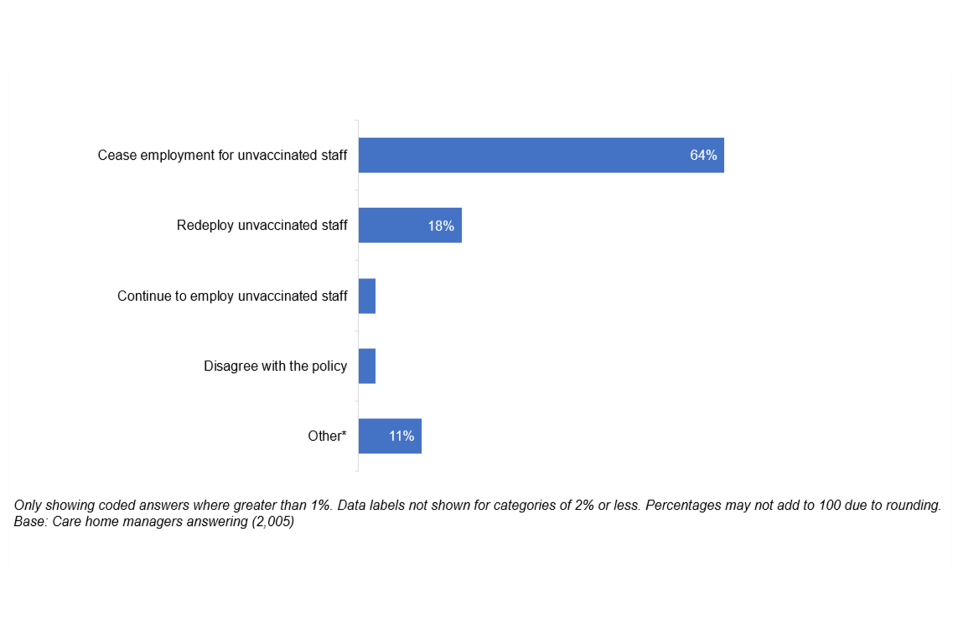
Care home managers were asked how they would respond to staff who did not receive the vaccine. Two in three (64%) would cease employment for unvaccinated staff and around one in five (18%) would redeploy unvaccinated staff. A very small proportion (three percent) would continue to employ unvaccinated staff in their current roles even if the policy is implemented.
Figure 11: How do you anticipate you would respond to the requirement, thinking about staff who are not vaccinated?
Do you have any concerns about the impact of the policy on the ability of older adult care homes to maintain a safe service?
Three in five (61%) respondents had concerns about the impact of the policy on the ability of older adult care homes to maintain a safe service. One in three (33%) have no concerns.
Figure 12: Do you have any concerns about the impact of the policy on the ability of older adult care homes to maintain a safe service?
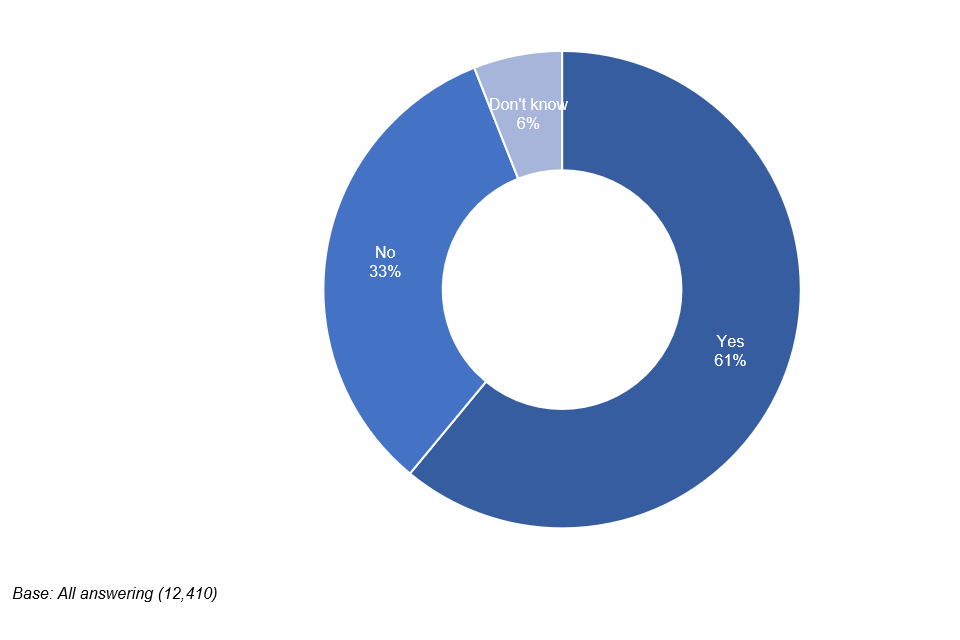
Members of the public (69%), health care providers (69%) and representatives of local government (66%) were most likely to have concerns, with care home providers (50%) and adult social care representative organisations (40%) most likely not to say they had no concerns.
Among those who work in adult social care, other frontline health and social care workers (66%), nurses (65%) and senior care workers (62%) were most likely to say they had concerns. Registered managers (52%) and directors or proprietors (50%) were most likely to say they had no concerns.
Which of the following are concerns that you have about the impact of the policy on the ability of older adult care homes to maintain a safe service?
The biggest concern among respondents was that staff might refuse the vaccine and resign, with four in five (81%) of respondents citing this. Three in four (75%) raised a similar concern, that staff might resign in protest. Around two in three (63%) cited staff seeking to challenge care homes in court and the time taken to recruit new permanent staff as key concerns about the impact of the policy on the ability to provide safe care.
Figure 13: Which of the following are concerns that you have about the impact of the policy on the ability of older adult care homes to maintain a safe service?
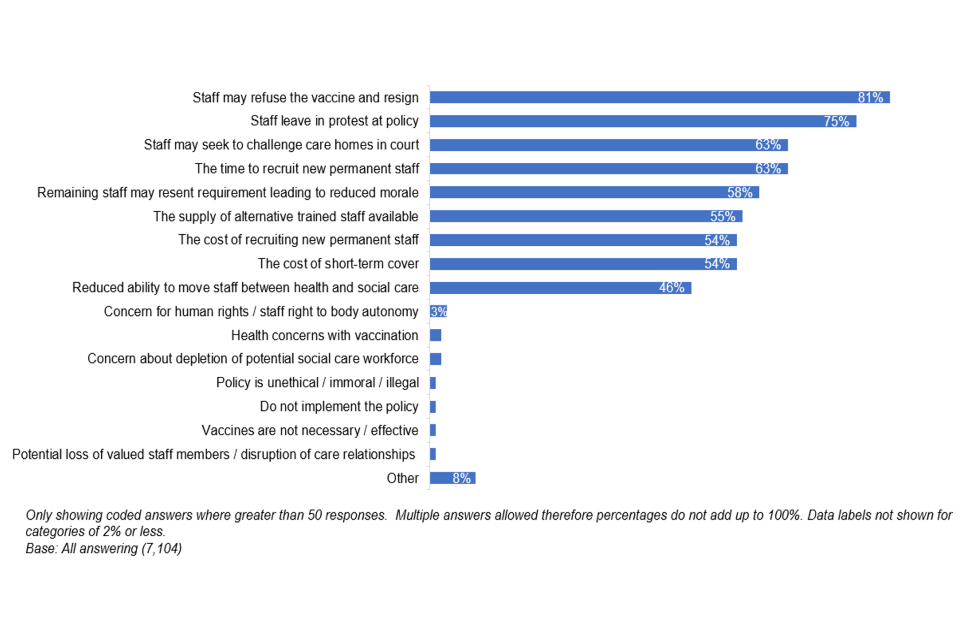
There is little difference among different groups of respondents in the types of concerns provided.
Please share any evidence and your sense of the scale of these impacts here:
Around half (51%) of respondents think that their concerns will have a severe impact, three in ten (31%) a moderate impact and just under one in five (18%) think they will have minimal impact.
Figure 14: What is your sense of the scale of these impacts?
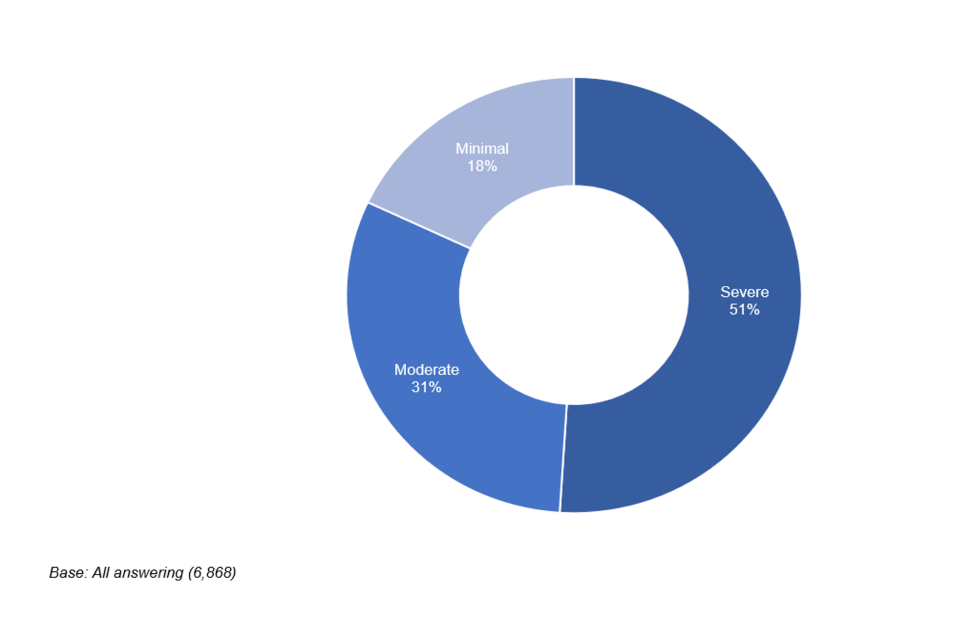
Members of the public (74%), care service users and their relatives and healthcare providers (both 62%) were most likely to report expectations of severe impacts. Care home providers (31%) and adult social care representative bodies (25%) were most likely to say that the expected impacts would be minimal.
Among the adult social care workforce, other frontline health and care workers (60%) and care workers (56%) were most likely to think that impacts would be severe. Directors or proprietors (34%) and registered managers (31%) were most likely to think the impact would be minimal.
Views from organisations that responded to the consultation
Many respondents mentioned challenges regarding resourcing. Concerns were raised about existing shortages of care staff being amplified due to staff employment being terminated as a result of refusing the vaccine. Further, it was mentioned that this may lead to a loss of experienced and specialised staff within the workforce.
The redeployment of unvaccinated staff to other roles is not an option available to care home employers.
Recruitment of new carers is expected to be more challenging with the additional requirement of being vaccinated, especially if this policy is not extended to staff in other care settings or the health sector.
We fear that placing barriers like mandatory vaccination on this workforce will result in people seeking employment elsewhere, exacerbating the existing staff shortages in care homes.
Respondents asked for regulation to make the vaccination requirement as transparent as possible in the recruitment process. Further, respondents felt that the responsibility for the vaccination of agency staff remains unclear and were at the same time aware that they might have to increasingly rely on agency staff if they experience staff shortages.
Another concern was about the requirement possibly increasing the fear of being vaccinated among care staff.
Threatening care workers with loss of livelihood does nothing to address concerns - rather the opposite, it is likely to confirm a conviction that there is something to fear.
This concern was distilled out of conversations that care home managers had with their staff. This development would be counterproductive to the intention of the policy.
Providers highlighted the amount of pressure they already experience, further increased by the pandemic and resulting in fatigue among managers and care staff. Implementing the requirement for deployment would add more administrative challenge and pressure on the service, for example through staff shortages. The possibility of that providers, especially the smaller and medium ones, might have to close down, was also noted.
Respondents suggested that the impact of implementing the policy could be mitigated through the provision of infrastructure support for care homes. Insurance and legislation were two areas where support was requested.
Clearer regulations about the vaccination of agency staff and established responsibilities would ease the administrative as well as executive burden for care. There was also a desire to see a ‘sunset clause’ in any legislation to ensure that this policy would be in place for a defined period only, after which new legislation would be needed to extend it.
How do you think we can minimise the impact of this new policy on the workforce?
Respondents note that ease of access to vaccinations (43%), access to up-to-date information about vaccines (42%), specific funding to cover costs associated with vaccination such as administrative costs and costs of sick leave due to result of vaccine side effects (38%) and support for clinical leads linked to care homes (38%) as the top ways to mitigate the concerns raised.
Just under one in three (31%) of respondents said that the policy should not be implemented.
Figure 15: How do you think we can minimise the impact of this new policy on the workforce?
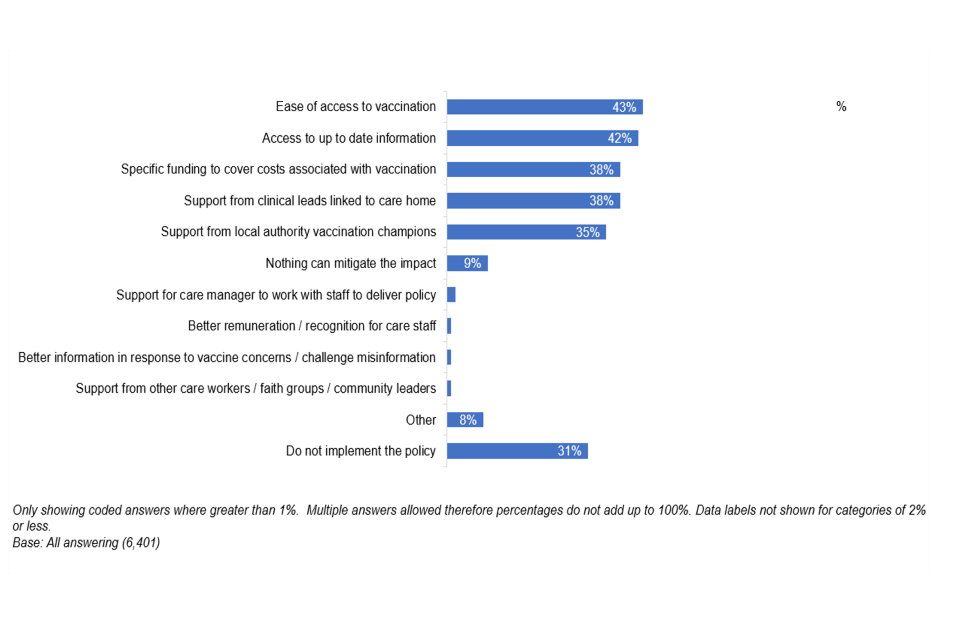
Different groups of respondents are in broad agreement over methods to mitigate concerns. Social care representatives, care home providers, local government representatives and NHS partners are more likely than other groups to say they believe ease of access to vaccination would be effective mitigations.
Views from organisations that responded to the consultation
Respondents suggested that the impact of implementing the policy could be mitigated through the provision of infrastructure support for care homes, with insurance and legislation being two areas for desired support. Clear regulations about the vaccination of agency staff and established responsibilities would ease the administrative as well as the executive burden for care. The wish for a ‘sunset clause’ in the proposed legislation was also expressed.
Do you think this new policy could cause any conflict with other statutory requirements that care homes must meet?
Two in five (42%) respondents feel that the policy could conflict with other statutory requirements on care homes. One in four (25%) did not think that it would and one in three (33%) did not know.
Figure 16: Do you think this new policy could cause any conflict with other statutory requirements that care homes must meet?
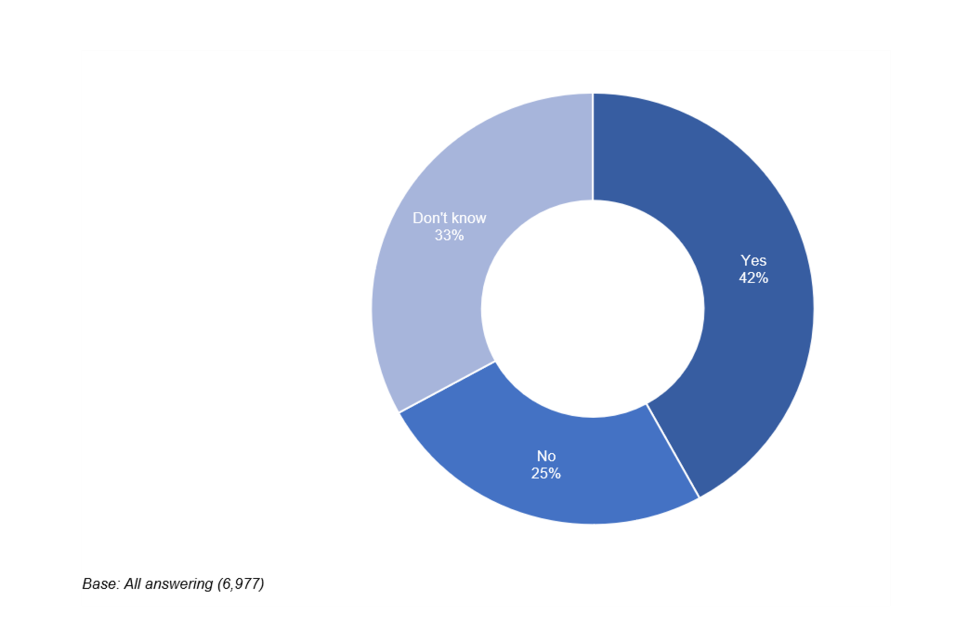
Members of the public (55%) and healthcare providers (47%) were most likely to report that the policy would conflict with other statutory requirements. Care home providers (40%) were most likely to say that there would be no conflict.
Of those working in adult social care, senior care workers (52%) and care workers (47%) were most likely to say that the new policy could conflict with existing statutory requirements. Directors or proprietors (44%) and registered managers (43%) were most likely to say they did not see any potential conflict.
Please give further detail on other statutory requirements that this new policy could conflict with
The statutory requirements mentioned revolve primarily around safe staffing levels. Respondents mentioned the Care Act 2014, infection prevention and control (IPC) standards and the Health and Social Care Act 2008. GDPR and the Data Protection Act were mentioned by members of the public.
Views from organisations that responded to the consultation
Respondents mentioned concerns about their ability to provide a safe and efficient service with a reduced workforce because staff refused to accept the policy. The potential loss of experienced and highly specialised members of staff was highlighted as a key risk. Concerns about the loss of staff were linked to questions about whether staff movement might increase as a result of the requirement for deployment. This could result in higher reliance on agency staff, with increased risk of spreading infections across locations.
Another worry related to care homes’ statutory requirements towards staff, residents and visitors.
[Care homes have a] number of legal obligations which they owe to their residents, staff and visitors. The proposed requirement for workers in older adult care homes to have a COVID-19 vaccination raises a number of employment law considerations.
Respondents mentioned that legal challenges could include claims of unfair dismissal under the Employment Rights Act 1996. Besides concerns about employment law, data protection rights were another frequently mentioned example.
We are also concerned by the requirement to verify and store the vaccination status of employees, which as well as engaging data protection issues, could normalise health surveillance by employers.
Other pieces of legislation that were mentioned are the Health and Social Care Act 2008 and existing CQC regulations, as well as section 60 of the Equality Act. The concerns were about reconciling this new policy proposal with existing laws and regulations.
7. Appendix: amendment of the Code of Practice
As part of the consultation, we have also consulted on a proposed amendment of the Code of Practice on Infection Prevention and Control and its associated guidance, which is issued by the Secretary of State under section 21 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 and to which providers must have regard when complying with their obligations under regulation 12[footnote 9] of the Regulations.
We have received limited feedback on the wording of the proposed amendment during the consultation. A draft of the text for the Code of Practice is set out below. It provides an explanation of the regulations and reflects the policy decisions being made as a result of the consultation.
The draft text below will be updated prior to the Code of Practice being issued to provide further practical information to assist service providers with the operational aspects of the policy. This will include examples of the types of evidence that can be provided to service providers to demonstrate a person’s vaccination status. The text relating to the policy will remain substantively the same.
7.1 Addition to criterion 10
Registered providers of the regulated activity of providing accommodation for persons who require nursing or personal care in a care home should ensure policies and procedures are in place with regard to COVID-19 vaccination such that:
- They do not allow anyone entry into the indoor premises of the care home unless:
- they are a service user of regulated activity of providing accommodation for persons who require nursing or personal care in that care home
- they can provide evidence that they have either been vaccinated with the complete course of doses of an authorised COVID-19 vaccine (in this instance, a full course does not include booster vaccines), or evidence that it is not clinically appropriate for them to be vaccinated with any authorised vaccine.
- it is reasonably necessary for them to provide emergency assistance in the care home
- it is reasonably necessary for them to provide urgent maintenance assistance with respect to the premises of the care home
- they are friend or relative of a service user and are visiting that service user
- they are under the age of 18
-
A service provider will need to apply the above requirements to all persons wishing to enter the premises of the care home including health care professionals, CQC inspectors, tradespeople, hairdressers, beauticians etc. Compliance with the regulations would amount to a reasonable excuse for not giving access to a CQC inspector.
-
If inspected, the provider will be able to demonstrate that:
- there is a record to confirm the evidence stated above has been provided. This record will be kept securely by the registered manager (or equivalent person) in compliance with the Data Protection Act 2018
- the eligibility for immunisation of workers is regularly reviewed in line with Regulation 12
- there is appropriate support and education of workers in relation to the vaccine
- workers are provided with the appropriate support to access vaccination
-
Social Care Working Group consensus statement, March 2021 - GOV.UK (www.gov.uk) ↩
-
Care home resident deaths registered in England and Wales, provisional - Office for National Statistics (ons.gov.uk) ↩
-
The state of the adult social care sector and workforce in England (skillsforcare.org.uk) ↩
-
Social Care Working Group consensus statement, March 2021 - GOV.UK (www.gov.uk) ↩
-
One dose of COVID-19 vaccine can cut household transmission by up to half - GOV.UK (www.gov.uk) ↩
-
COVID deaths of people with learning disabilities (publishing.service.gov.uk) ↩
-
PHE: Factors contributing to risk of SARS-CoV2 transmission in various settings, 26 November 2020 - GOV.UK (www.gov.uk) ↩
-
Regulation 12 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 requires care and treatment to be provided in a safe way for service users. This includes an obligation on the registered person to assess the risk of, and prevent, detect and control the spread of infections, including those that are health care associated (regulation 12(2)(h)). ↩
