Military medical techniques saving lives at home
A lifesaving process, inspired by military practices, has been introduced by a UK major trauma centre to treat critically ill patients.
![A Medical Emergency Response Team carrying out lifesaving work in Afghanistan (library image) [Picture: Sergeant Alison Baskerville, Crown copyright]](https://assets.publishing.service.gov.uk/media/5a617d9ae5274a0a1b10d118/s300_JMOCCCT-2011-068-221.jpg)
A Medical Emergency Response Team carrying out lifesaving work in Afghanistan
The major trauma centre at St Mary’s Hospital in Paddington, London, has launched a new streamlined patient pathway based on military medical techniques honed in Afghanistan to improve the survival rates of patients with gunshot or stab wounds. It is believed to be the first major trauma centre in the UK to take this new approach.
Based on a protocol developed at Camp Bastion in Afghanistan in 2005 to treat the most seriously injured casualties as quickly as possible, the process involves bypassing the resuscitation room and taking casualties straight to theatre for surgery to stem bleeding and improve the chances of recovery.
The pathway, called ‘rapid resuscitation transit’, was developed by senior trauma clinicians at St Mary’s Hospital in collaboration with military doctors hosted by the Imperial College Healthcare National Health Service (NHS) Trust to work in its hospitals.
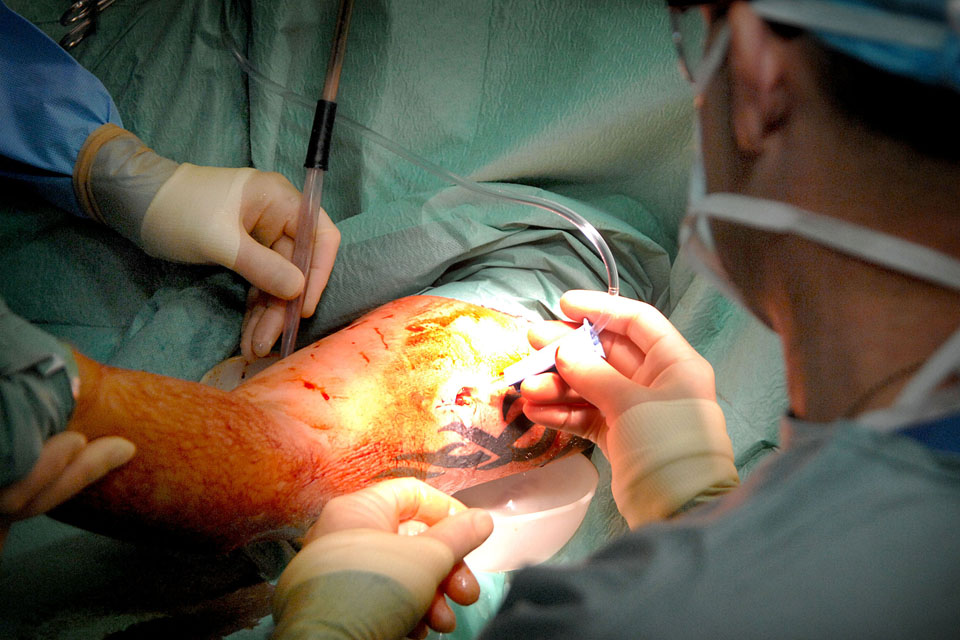
A soldier receives treatment for a gunshot wound to his upper arm on operations (library image) [Picture: Corporal Ralph Merry RAF, Crown copyright]
Rapid resuscitation transit aims to reduce the ‘knife to skin’ time – the length of time between a patient’s arrival at an emergency department and potentially lifesaving surgery – by streamlining medical investigations.
When a patient with gunshot or stab wounds arrives at the major trauma centre, investigations and tests are prioritised and limited to the most crucial, such as taking a single blood sample and carrying out essential scans.
The patient is then immediately transferred to a dedicated 24/7 theatre for major trauma cases. The theatre and its equipment are prepared in advance while the theatre team is mobilised with specific action cards on what to do when.
Major Danny Sharpe, an Army trainee in emergency medicine who has been hosted by St Mary’s Hospital for the past 2 years, was involved in introducing the protocol with the Trust’s major trauma centre clinicians. He said:
We know that stopping bleeding quickly improves survival and most of the cases managed in this way will involve critically unstable patients who are at risk of bleeding to death without very quick action.
I am really pleased to have been able to work with St Mary’s Hospital to bring this into the civilian medical world to help increase patients’ chances of survival after suffering serious injuries.

St Mary's Hospital's major trauma centre team [Picture: Crown copyright]
Michael Jenkins, lead clinician for St Mary’s Hospital’s major trauma centre, said:
The crucial thing is to try to reduce the time to theatre so that the source of bleeding can be surgically targeted as soon as possible in the hope of improving the patient’s survival and recovery.
The major trauma centre at St Mary’s Hospital sees a significant number of patients with stab or gunshot wounds and a number of patients have already been treated via the new pathway since it was introduced over the summer.
St Mary’s is one of the 3 top performing major trauma centres in the UK and, after major trauma centres were introduced 2 years ago, UK patients are now 20% more likely to survive life-threatening trauma.
The Surgeon General, Air Marshal Paul Evans, who is the senior medical officer in the British Armed Forces, said:
Adapting techniques that have been developed on operations, to be used by NHS colleagues to benefit patients, is an excellent example of the Defence Medical Services working in partnership with the NHS.