Clinical guidance and scope of practice for professionals involved in the provision of the ultrasound scan within AAA screening
Updated 8 January 2025
Applies to England
1. Overview
The main aim of the NHS Abdominal Aortic Aneurysm (AAA) Screening Programme is to reduce aneurysm-related mortality through the early detection, appropriate monitoring and treatment of aortic aneurysms.
The NHS AAA Screening Programme invites men for an abdominal ultrasound scan during the year (1 April – 31 March) they turn 65. The screening scans are performed by qualified screening technicians who follow a scanning protocol developed by the NHS AAA Screening Programme. This requires measurement of the aorta in transverse and longitudinal planes.
This document provides information about the screening test performed by screening technicians and accredited sonographers within the NHS AAA Screening Programme.
It provides a framework to help maintain consistency for all men having ultrasound scans within the NHS AAA Screening Programme. This document also outlines the scope of practice for screening technicians. They are not expected to scan outside the remit of these guidelines.
Clinical skills trainers (CSTs), Internal Quality Assurance (IQA) leads and programme coordinators/managers should use this document to help guide and support screening technicians during their initial training and as a reference tool for their professional development and on-going quality assurance.
This document is used in conjunction with/incorporated within a local operating procedure in-line with national protocols and standard operating procedures (programme guidance).
2. The scan
2.1 Accommodation requirements
Appropriate consideration must be taken when deciding on accommodation to provide screening within the NHS AAA Screening Programme. Risk assessments and any associated actions should be in place before starting screening at any location to ensure:
- equity of access to screening
- safety of men and screening staff
- mitigated risks of work related musculoskeletal (MSK) disorders.
The full list of clinic room requirements can be found in the standard operating procedures (programme guidance)[footnote 1].
2.2 Consent
Consent for the screening procedure, information retention and potential contact for research purposes must be performed for every man prior to screening. The man should be fully informed about the process and possible outcomes. This information should also include an explanation regarding the use of his data, including for research purposes. His full consent should be obtained prior to screening commencing. Please see the standard operating procedures (programme guidance) for further information regarding consent[footnote 2].
2.3 Positioning the man for screening
The man must be able to transfer and lie supine independently. If this is not possible, alternative arrangements should be in place within the local screening service to accommodate these men. This may involve screening at a different site with hoists and appropriate transfer equipment and staff available. Screening technicians must not attempt to lift or transfer men in screening locations without suitable training or equipment.
Screening technicians should only scan men using the transverse imaging plane (TP) and longitudinal imaging plane (LP) with the man in the supine position. At no time should the man be asked to turn on their side or moved from their supine position.
Technicians are advised that a slight sideways/oblique angle may be used to try to avoid bowel gas/aid imaging but beyond this, if an aorta is non-visualised in the supine position from an anterior approach, the technicians must refer the man for a re-scan in line with the management of non-visualisation.
2.4 Identification of the aorta
To initiate the scan and identify the aorta, the technicians should have the probe orientated to obtain images in the transverse plane (TP). This is normally achieved by placing the probe 3-4cm above the umbilicus but can be dependent on body habitus.
Following optimisation of image depth, the inferior vena cava (IVC) and anterior border of the lumber spine should be visible. The aorta can be differentiated from the IVC as it is typically more circular in shape and normally lies to the left of the patient when compared to the IVC.
In the upper abdomen, the presence of anterior branches (coeliac axis and superior mesenteric artery) can aid identification of the aorta although they are not aways seen. The aorta also has thicker walls than the IVC. The aorta is imaged from its supra renal level to its bifurcation into the common iliac arteries.
The aorta is next imaged in a longitudinal plane (LP) by rotating the probe from the TP image. The aorta is assessed from the level of the xiphisternum at the suprarenal level, to the bifurcation. Whenever possible, identification of the superior mesenteric artery (SMA) should be made as a landmark.
The aorta should be measured at its maximum anterior posterior diameter in TP and LP ensuring that the line of measurement is perpendicular to the aortic lumen at the point of measurement and not taken in an oblique plane (figure 1).
Further advice regarding imaging and image quality can be found in the AAA ultrasound image quality guidance[footnote 3].
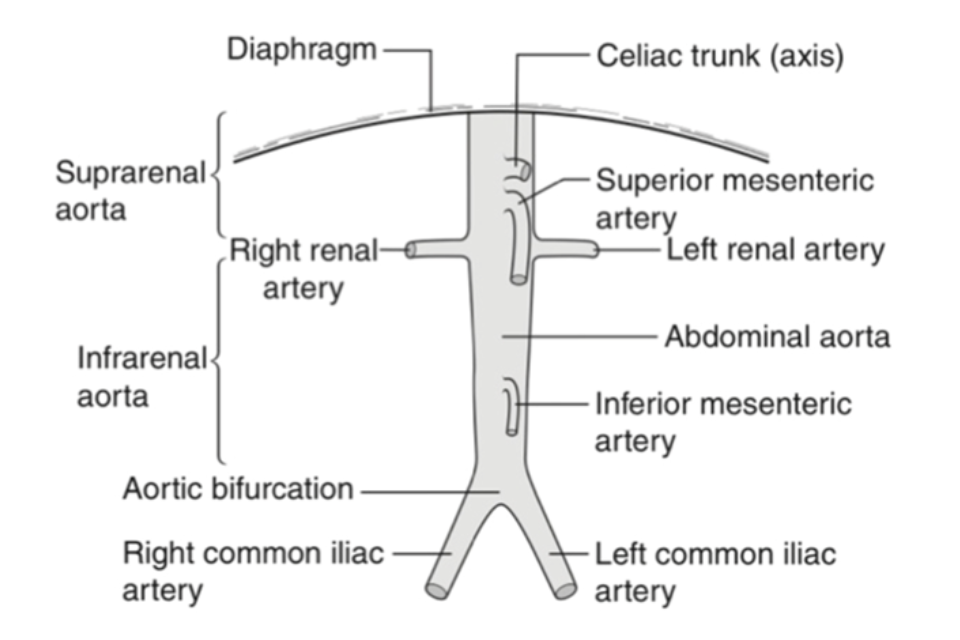
Figure 1. Anatomy of the abdominal aorta and its branches
2.5 Image optimisation
Prior to obtaining a measurement, screening technicians should optimise every image to ensure accuracy and quality of measurements.
Technicians need to understand how the individual image optimisation controls work in relation to image quality and basic physical principles. This is outlined in the initial training and annual competency assessment, as listed below:
- frequency
- depth
- gain
- time gain compensation
- harmonic imaging
- dynamic range
- focus/focal zone position
- number of focal zones
- sector width
- compound imaging
- edge enhancement.
Any other relevant adaptive imaging processing control specific to the scanner in use.
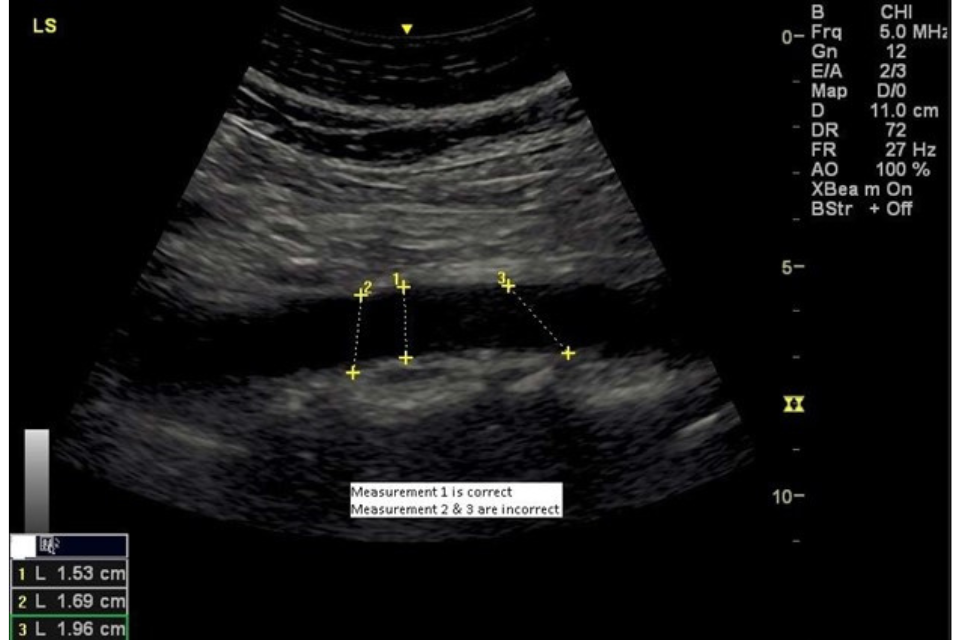
Figure 2. Measurement of the abdominal aorta showing the correct and incorrect lines of measurement
2.6 Image capture
A minimum of two images must be taken and saved in line with national and local protocols. However, there are occasions when several images may need to be recorded.
Examples include the presence of bowel gas obscuring a section of the aorta that subsequently clears or if there are features that require review or quality assurance by the CST.
The minimum requirements are as follows:
-
The maximum transverse (internal anterior wall to internal posterior wall) diameter of the aorta should be measured, and an image recorded and stored. The image should demonstrate the lumbar spine, and where visible the inferior vena cava. The images must be annotated to demonstrate the scan orientation, for example TP or LP.
-
The maximum longitudinal (internal anterior wall to internal posterior wall) diameter of the aorta should be measured, and an image recorded and stored (figure 2). The image should demonstrate the lumbar spine. The images must be annotated to demonstrate the scan orientation.
-
Annotation requirements should be determined locally. Further information can be found in the image quality guidance[footnote 3].
2.7 Length of examination
The length of the screening appointment is a local decision based on available resources. Local services should have policies and guidance to mitigate the risk of work related MSK disorders.
3. Scope of practice
The scope of practice for screening technicians within the NHS AAA Screening Programme is the identification and differentiation of the abdominal aorta and the inferior vena cava from the level of the xiphisternum to the level of the aortic bifurcation with the subsequent measurement of the abdominal aorta at its widest point.
3.1 Non-visualisation
In some situations, the screening technicians may not be able to clearly visualise the aorta. In these circumstances, the man will be invited to return for a repeat scan at the clinic or to the medical imaging unit or vascular laboratory associated with the local screening service.
Reasons for non-visualisation include:
- high body mass index, resulting in the screening technician being unable to identify all, or large segments of the abdominal aorta
- excessive bowel gas resulting in two or more failed examinations
- ambiguity regarding caliper placement and aortic diameter measurement
- unusual anatomy or pathology or previous abdominal wall surgery and scarring
- position of a stoma.
There are also instances of technical failure when screening technicians can visualise the aorta, but its diameter cannot be accurately measured.
This may be if the posterior wall of the aorta cannot be clearly differentiated from tissue between the posterior aortic wall and anterior border of the lumbar spine. This can result in ambiguity of caliper placement and accurate aortic diameter measurement. Further information can be found in the image quality guidance[footnote 3].
If the result of a second scan at a screening clinic is also non-visualised or technical failure, then the man must be referred to the imaging unit/vascular laboratory. The local AAA screening service should indicate the reason for requesting the scan on the man’s referral request following a non-visualisation.
The imaging unit/vascular laboratory should then notify the screening office of the outcome. It is the screening provider’s responsibility to send the screening result to the GP and action in line with the standard operating procedures (programme guidance)[footnote 1]. If the aorta cannot be visualised by the imaging unit/vascular laboratory then the individual case must be discussed with the local service director/clinical lead, and they will decide if alternative imaging is required.
Following receipt of positive screening results, local services should book future screening appointments for surveillance men within routine clinics unless otherwise advised.
Local services are expected to fund any imaging required following non-visualised results from their local screening provider budget.
It is expected that imaging units/vascular laboratories have clear governance and oversight arrangements in place with local screening services.
3.2 Test procedure and reporting
The man should be scanned, in accordance with protocols of the local imaging unit or vascular laboratory for imaging of the abdominal aorta. In line with screening guidelines, the person performing this scan should check, measure and clearly record:
- individual’s identification
- NHS number
- the maximum transverse (internal wall to internal wall) anterior-posterior (A/P) diameter of the aorta
- the maximum longitudinal (internal wall to internal wall) A/P diameter of the aorta.
These measurements should be clearly documented in the scan report as they need to be entered onto the SMaRT (Screening Management and Referral Tracking) AAA IT system.
Images should:
- show the patients name, DoB and NHS number
- include the lumbar spine as a landmark and where possible the vena cava
- be annotated to demonstrate the scan orientation, ‘TP’ or ‘transverse’ and ‘LP’ or ‘Longitudinal’.
A minimum of two images should be captured and stored.
Imaging reports should be sent to the local screening office ensuring the name of clinician performing the scan is recorded.
If the abdominal aorta is found to measure 5.5cm or more in diameter or has grown more than 1 cm in 1 year, the report should be sent within one working day, to the local screening provider office who will refer the man in line with national guidelines.
The imaging unit/vascular laboratory should follow their local protocol for dealing with any incidental findings. A copy of the report must be sent to the local screening provider for reference, ensuring the name of operator performing the scan is recorded.
The local screening provider must be informed if a man does not attend his imaging unit/vascular laboratory appointment.
3.3 Technical problems and non-visualisation of the abdominal aorta
Both the transverse and longitudinal measurements of the aorta are required for the screening test to be classed as successful. Occasionally it is impossible to obtain an adequate image of the aorta that enables the diameter to be measured in either, or both, of these planes. The reason for non-visualisation or technical failure should be stated in the report and sent to the local AAA screening provider for further decision by the director/clinical lead.
There will also be cases when a section of the aorta cannot be visualised. The NHS AAA Screening Programme has issued guidance to local screening services and the same advice should be followed by imaging departments.
3.4 Guidance for non-visualisation of the suprarenal aorta
Approximately 95% of all abdominal aortic aneurysms are found in the infrarenal aorta; isolated dilated segments of the suprarenal aorta are rarely encountered during routine scanning. However, wherever possible the suprarenal aorta should be imaged in addition to the infrarenal aorta (figure1).
If the suprarenal section cannot be fully visualised but the rest of the aorta is clearly seen, then this is acceptable, and the aortic diameter can be recorded (figure 3).
The suprarenal section is the part of the abdominal aorta above the renal arteries. These are not normally visible and the SMA can be used as an alternative landmark. Colour flow imaging, to aid the location of the renal arteries or SMA, can only be used by medical imaging departments.
If the SMA is also not visible, the suprarenal section approximates to the first 3cm of the abdominal aorta just below the xiphisternum or diaphragm.
If any part of the infrarenal aorta cannot be visualised (figure 4) then it should be recorded as a non-visualised scan and the appropriate pathway followed.
The following diagrams are for illustrative purposes:
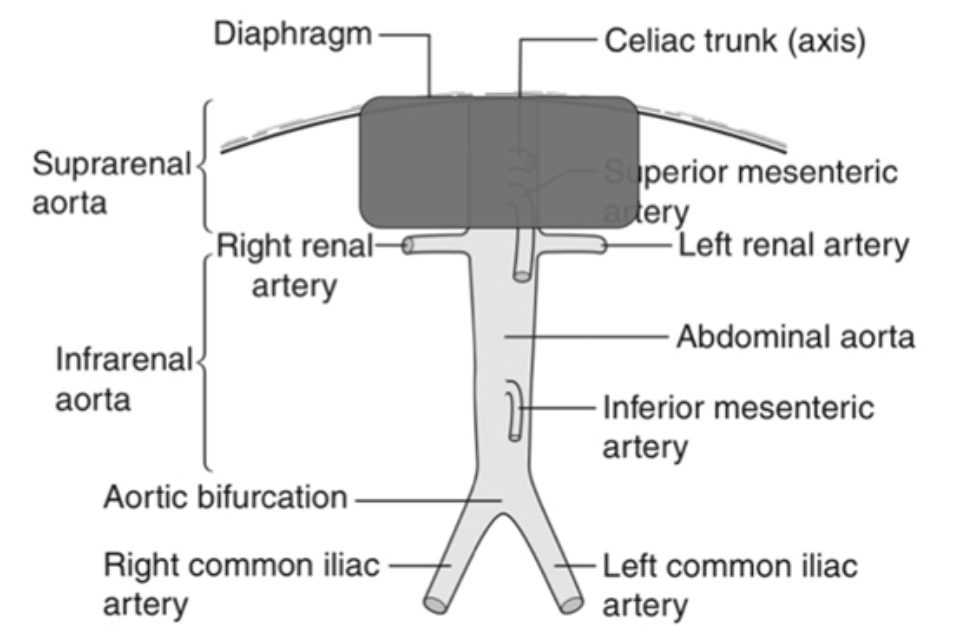
Figure 3. Non-visualisation of the supra-renal aorta
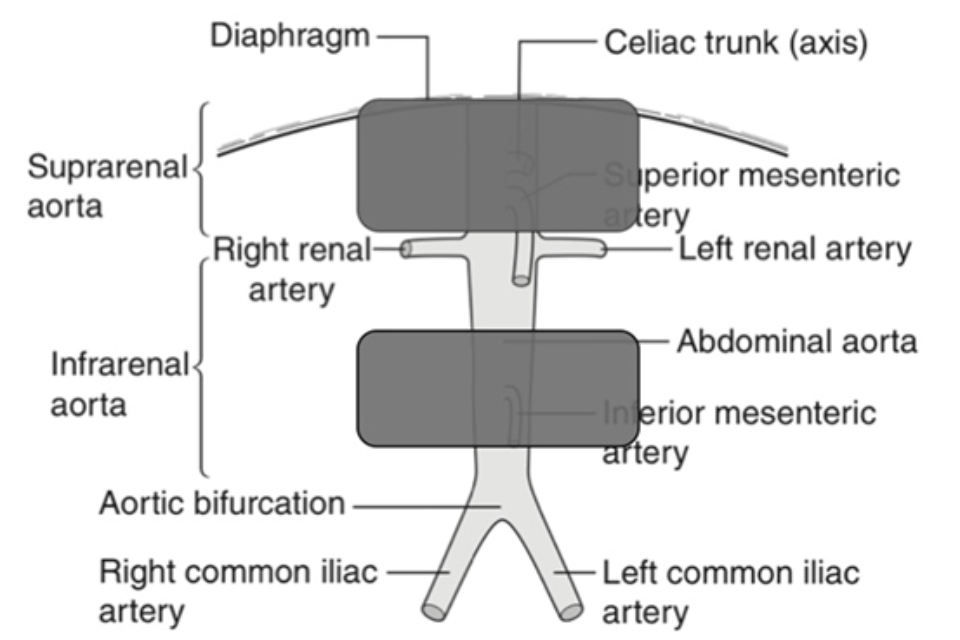
Figure 4. Non-visualisation of the supra and infrarenal abdominal aorta
To ensure that a consistent policy is applied across local screening services, screening technicians should also discuss the issue of non-visualisation with their local clinical skills trainer and quality assurance lead. Non-visualisation of the aorta is also a programme standard and screening services must meet performance thresholds and identify reasons for exceeding acceptable levels.
3.5 Incidental findings
Local screening services should have a local policy for the management of incidental findings. Screening technicians are not expected or required to measure or identify any other structures, pathology or physiology within the abdomen that is not outlined within this guidance.
Occasionally screening technicians observe anatomy that may appear unusual or different from their scope of practice. If this occurs, technicians should report these as incidental findings within SMaRT.
Screening technicians must add additional comments to the incidental finding box within the reporting software and must request a QA review. The CST/internal QA lead will review any additional images taken and decide the appropriate course of action.
If further investigation or follow up is required, this falls outside of the remit of the NHS AAA Screening Programme. For vascular incidental findings, these may be dealt with by the director/clinical lead of the local screening service. In other instances, the local screening service should contact the man’s GP suggesting the appropriate course of action. A copy of the communication should be sent to the director/clinical lead of the local screening service.
As a failsafe measure the local service must make sure that the communication has been received by the GP practice. Confirmation of this can be recorded within SMaRT inside the comments box for the specific patient record.
The local service is not responsible for ensuring that any advice is actioned by the GP.
If the proximal abdominal aorta appears aneurysmal as an extension of a thoracic aortic aneurysm, the visible aorta should be measured accurately at its widest point as per usual protocol and images captured. The images should also be flagged for image QA review by the CST.
The local incidental findings policy should then be followed for further investigation of any suspected thoracic aortic aneurysm. The man should remain within the screening programme with appropriate surveillance until informed otherwise via the director/clinical lead.
3.6 Governance and oversight arrangements with local screening services
In many cases, the clinical skills trainer and internal quality assurance lead for the local screening provider will be a member of the imaging unit or vascular laboratory undertaking non-visualisation imaging. Regular, direct contact between local screening services and imaging units/vascular laboratories is essential. As part of this process, formal arrangements should include:
- attendance of an imaging unit or vascular laboratory representative at local AAA screening provider team meetings
- audit of images and reports
- discussion and feedback regarding interesting cases or imaging problems.
3.7 External quality assurance review
Imaging units and vascular laboratories should be aware that local screening services are subject to external quality assurance (QA) reviews and should, therefore, work with the local screening provider to ensure that relevant information and documentation is available regarding the process for additional imaging. Regular meetings should be in place between the local screening provider and the imaging unit or vascular laboratory to discuss such arrangements and any potential problems with internal or external QA processes.
