Acute hepatitis B: national enhanced surveillance report April to June 2023
Updated 24 April 2025
Applies to England
Background
Hepatitis B is a blood borne infection of the liver caused by the hepatitis B virus (HBV). The virus can cause an acute illness characterised by nausea, malaise, abdominal pain, and jaundice but can also result in a chronic persistent infection that is associated with an increased risk for chronic liver disease and hepatocellular carcinoma.
Surveillance of acute hepatitis B is essential as this represents recent transmission of HBV and therefore incidence. Surveillance guides targeted prevention and control activities such as the selective immunisation programme of people at higher risk of exposure and complications of HBV infection.The quarterly reporting of enhanced molecular surveillance of acute hepatitis B is based on clinical reports of acute cases to regional Health Protection Teams (HPTs) in UK Health Security Agency (UKHSA) and corresponding samples being submitted to the UKHSA Blood Borne Virus Unit (BBVU) in the Virus Reference Department (VRD) at Colindale.
Methods
Acute infectious hepatitis is a notifiable infectious disease, and clinicans suspecting an acute hepatitis B diagnosis are required to report the case to their regional HPT. Information on individuals reported with acute hepatitis B is capured through the UKHSA case management system (HPZone). Following the reporting of clusters of acute hepatitis B in 2015-2016, an HPZone Context ‘Acute hepatitis B’ was added for monitoring of acute cases.
For surveillance purposes an acute hepatitis B infection is defined as HBsAg positive and anti-HBc IgM positive with abnormal liver function tests plus a clinical pattern consistent with acute viral hepatitis. As acute hepatitis B flares can occur during chronic persistent infection, HBV core avidity testing may be done to differentiate between an acute and chronic infection.
In 2016, VRD re-introduced HBV anti-core avidity testing alongside genotyping of samples from patients diagnosed with acute hepatitis B, a service that is offered free of charge. Hospital microbiology and virology departments are requested to send samples to Colindale for confirmation, avidity testing and genotyping as part of the national enhanced surveillance of acute hepatitis B (see Acute hepatitis B: guide to national enhanced surveillance).
Records of any ‘Acute Hepatitis B’ reported between April and June 2023 were collated from HPZone, and linked to samples submitted to the UKHSA BBVU at Colindale, using a combination of Surname, First name, Date of birth, Sex, and NHS number.
Results
Between April and June 2023, 52 cases of acute hepatitis B were entered onto HPZone across England (confirmed, probable and possible). Overall, the cases entered on HPZone have been declining from 297 in 2018 to 213 in 2022. Monthly cases since 2018 in England are shown in figure 1. It is likely that the number of cases observed during 2020 (199) and 2021 (201) were lower as a result of SARS-CoV-2. Precise causes are likely to have been multifactorial including, but not restricted to, disruption to and/or reconfiguration of health services, reduced access to testing and the impact of social and physical distancing measures resulting in fewer opportunities for onward transmission.
Figure 1. Cumulative cases of acute hepatitis B in England entered on HPZone: 2018 to June 2023
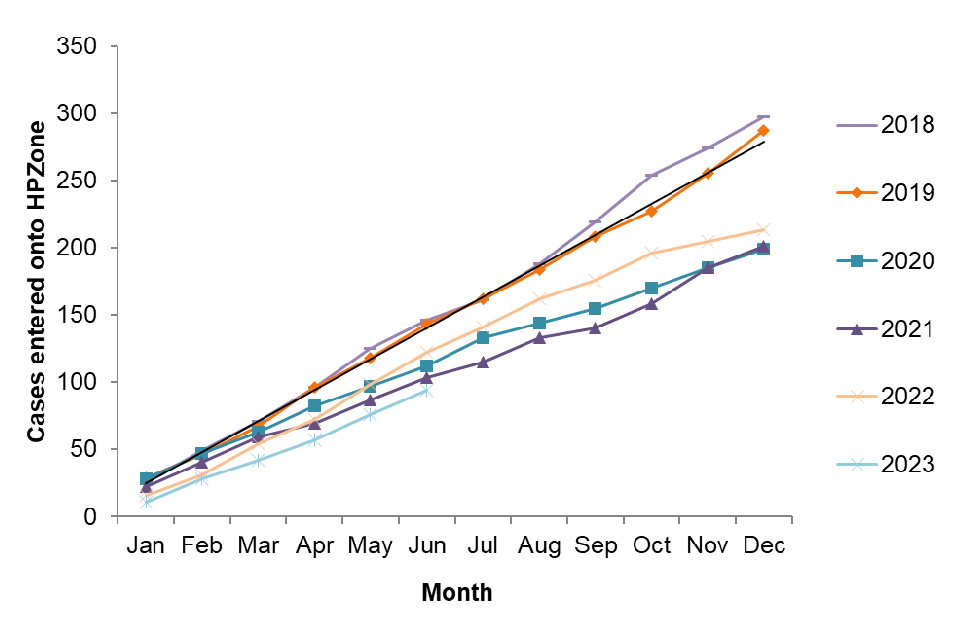
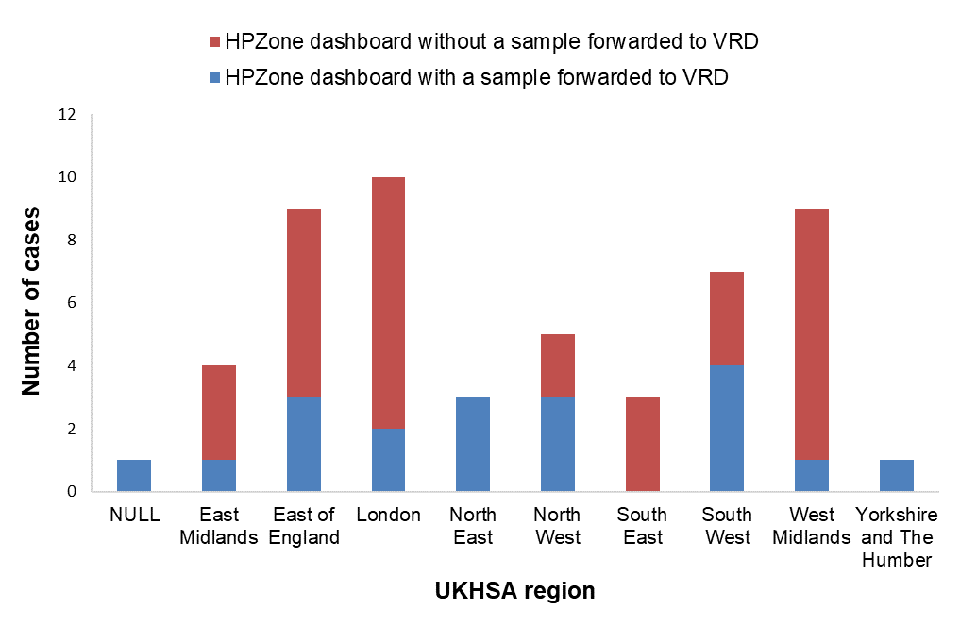
Figure 2 shows the number of cases entered onto HPZone by month and the number where a residual sample was received by the laboratory for avidity and molecular characterisation. Figure 3 shows this distribution by region.
Figure 2. April to June 2023 cases by month entered onto HPZone with or without a sample forwarded to VRD for avidity and molecular characterisation
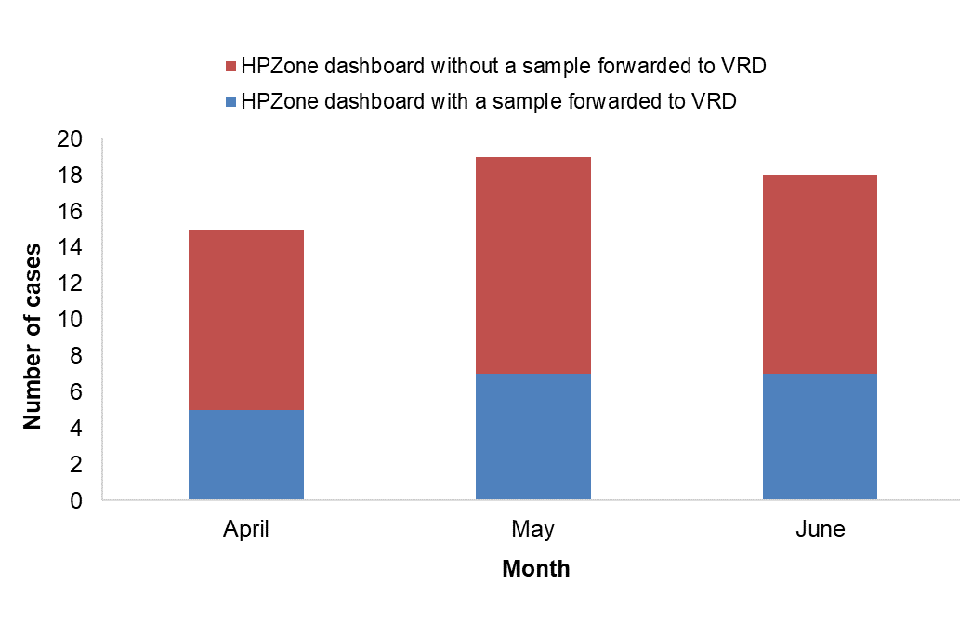
Figure 3. April to June 2023 cases by UKHSA region entered onto HPZone with or without a sample forwarded to VRD for avidity and molecular characterisation
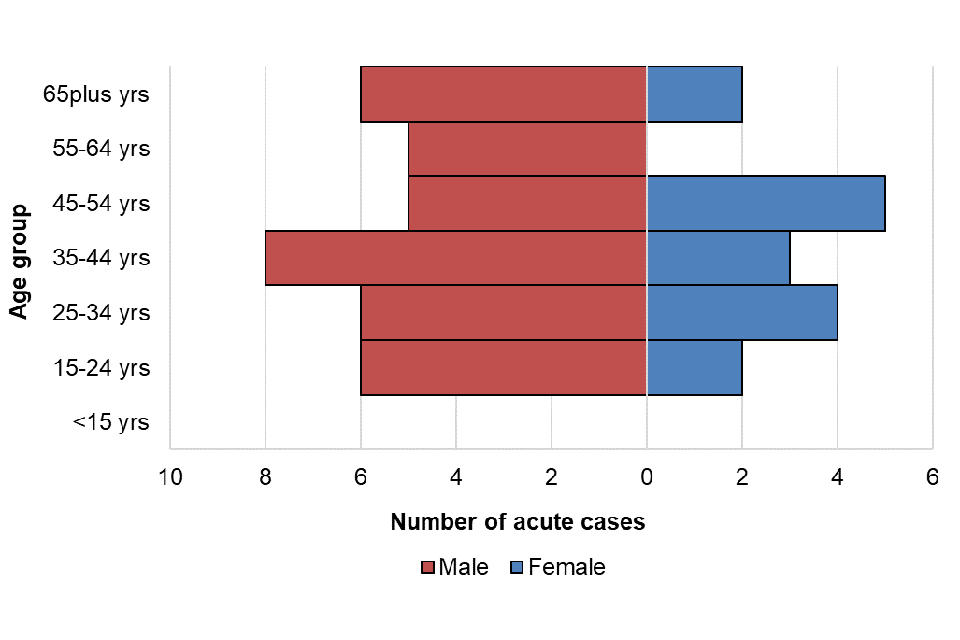
For cases entered onto HPZone between April and June 2023, age and sex was well reported (95%). Where sex was known males accounted for 69% of cases (36 out of 52) and females 31% (16 out of 52). The median age of persons with acute HBV infection was 39 years old (IQR: 29 to 55): 40 (IQR: 29 to 59) for males and 37 (IQR: 30 to 49) for females. The age distribution by sex is presented in figure 4; the highest proportion of cases was seen in the 35 to 44 year age group followed by 25 to 34 and 45 to 54 age groups. The highest proportion in males was seen in the 35 to 44 year age group; for females in the 45 to 54 year age group. Where reported, 53% (26/49) of persons with acute HBV infection were resident in the two most deprived quintiles. Where ethnicity was available (42; 81%), 25 (48%) of those with acute HBV were of white British ethnic origin, followed by those of black or black British ethnic origin (29%; 9) and Asian or Asian British ethnic origin (13%; 4).
Figure 4. Age/sex pyramid of acute HBV cases from HPZone: April to June 2023
Avidity testing and molecular characterisation investigations were undertaken on samples linked to cases to confirm the acute hepatitis B diagnosis with additional genotyping and phylogenetic analysis to inform on the diversity of the circulating viruses.
Of the 19 samples submitted to the VRD as part of the enhanced surveillance programme, 2 samples (11%) were confirmed to be from an individual with chronic hepatitis B and 16 (84%) were confirmed to be from individuals with acute hepatitis B infection. One sample was not tested for anti-HBc avidity due to insufficient sample volume. Not all cases with samples forwarded to the VRD could be matched to cases in HPZone; this could either be due to a case not being entered on HPZone or it could be due to the case being entered in a previous quarter.
A total of 12 out of 16 confirmed acute cases could be genotyped during April to June 2023; the distribution of genotypes is shown in table 1. The distribution of genotypes seen in UKHSA regions is shown in figure 5.
Table 1. Genotype distribution and proportions of acute hepatitis B cases tested at VRD in April to June 2023
| Acute genotype | Number of cases | Proportion of cases | Culumative Jan to Jun |
|---|---|---|---|
| A [Note 1] | 3 | 25% | 4 (19%) |
| B | 0 | – | 0 |
| C [Note 1] | 3 | 25% | 3 (14%) |
| D/E Recombinant | 0 | – | 1 (5%) |
| D [Note 1] | 2 | 17% | 5 (24%) |
| E [Note 1] | 4 | 33% | 4 (19%) |
| F | 0 | – | 4 (19%) |
| Total | 12 | – | 21 |
Note 1. For April to June genotype A includes (A1=1,A2=2), C includes (C1=2, C5=1), D includes (D1=2), E includes (E=4).
Figure 5. Genotypes of acute samples sent to VRD by UKHSA region: April to June 2023

Discussion
Quarterly publication of enhanced molecular surveillance using matched HPZone and reference laboratory confirmatory and typing data with a regional breakdown allows near real-time monitoring of acute hepatitis B transmission. The number of acute hepatitis B cases between April and June 2023 remained low and consistent with annual trends for the same timeframe. It is likely that the number of cases observed during 2020 and 2021 were lower as a result of SARS-CoV-2. Ascertainment of cases on HPZone through health protection investigations and HBV anti-core avidity testing provides assurance that this decrease in cases is likely to have been real. Molecular analysis provides insight into the current hepatitis B genotypes circulating in England, although interpretation is limited by the small proportion of samples submitted to VRD. A broad genotype distribution was noted with most of the major HBV genotypes noted in this quarter. Genotype characterisation can indicate a geographical origin which can contribute to understanding sources of infection and transmission routes. Improved submission of samples for molecular characterisation will allow for more comprehensive monitoring and interpretation of acute HBV infection trends in England.
