Bowel cancer screening: having a colonoscopy
Updated 23 June 2025
Applies to England
This information is for people invited for colonoscopy after bowel screening. You can choose if you have a colonoscopy. This leaflet aims to help you decide.
Why the NHS offers colonoscopy
Colonoscopy can help to find polyps and bowel cancers because they can develop without symptoms.
Polyps are small growths on the lining of the large bowel. Most polyps are harmless, but some are more likely to change into a cancer. Bowel cancer is cancer that’s found anywhere in the large bowel. This includes the colon and rectum.
We offer a colonoscopy if we find a certain amount of blood in your poo sample. Polyps and bowel cancers sometimes bleed but you cannot always see this. Most people will not have bowel cancer, but having a colonoscopy helps us check the cause of the blood.
If you have any polyps, we can usually remove them during colonoscopy. This can greatly reduce your risk of getting bowel cancer. If there are signs of bowel cancer, we may be able to offer treatment. Finding bowel cancer early can make it more likely that treatment will be effective.
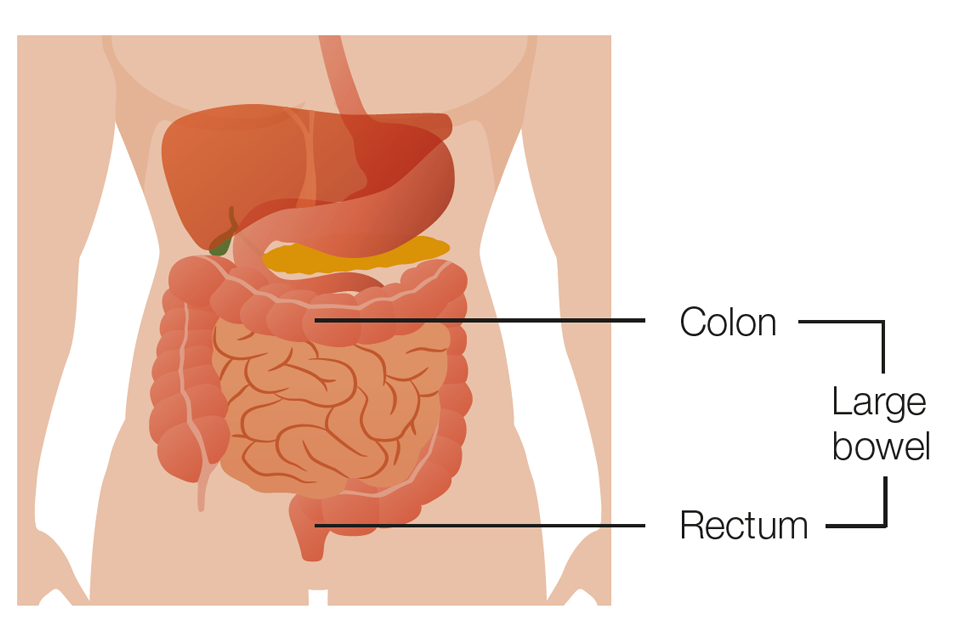
The colon and rectum make up the large bowel
The bowel is part of your digestive system. It takes nutrients and water from food and turns what’s left into poo.
Colonoscopy
A colonoscopy is a test to check inside your bowels for polyps and bowel cancers. It also helps to confirm if you have a bowel condition that’s not bowel cancer.
A specially trained clinician called a colonoscopist will do the test.
They will put a thin, flexible tube with a small camera into your bottom. It’s called a colonoscope. You may feel it go in, but most people do not find it painful. It will show the inside of your bowels on a screen.

The colonoscopist looks at images from inside the bowel on a screen
A colonoscopy usually takes 30 to 45 minutes. Your whole appointment may take around 2 hours.
Your appointments
Your first appointment will be to discuss having a colonoscopy. This is called a specialist screening practitioner (SSP) appointment. The specialist will:
-
talk to you about your screening results
-
describe what a colonoscopy is
-
explain the possible risks and benefits
-
discuss options available to make you more comfortable
-
answer any questions you have.
They will check if colonoscopy is suitable for you. They will ask about any health conditions you may have and if you take medication. Some people cannot have a colonoscopy. The specialist will assess if a virtual colonoscopy called a CT colonography (CTC) scan may be suitable instead. It uses X-rays to check the health of your bowel. Read more about having a CTC scan at GOV.UK.
If you are fit enough to have a colonoscopy, you can choose if you go ahead with the procedure. If you do, it will usually take place in hospital. This should be within 2 weeks of your first appointment.
Please tell the specialist if you have any additional requirements. For example, you may need someone to help you at your appointment, such as a carer or an interpreter.
You can ask for a male or female colonoscopist. We will try to accommodate your preference, but this is not always possible.
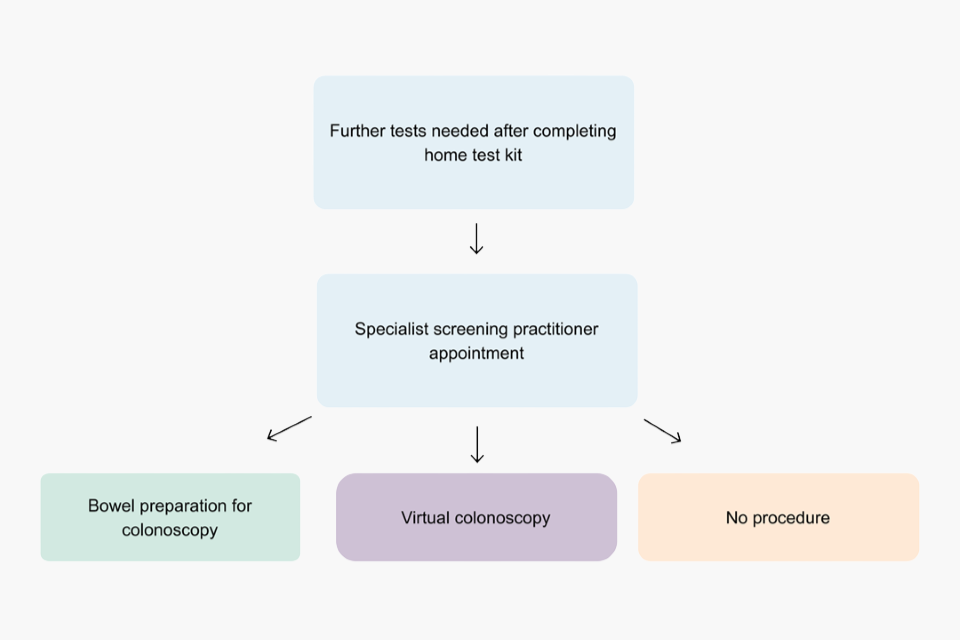
Diagram showing the bowel screening appointment pathway
Before your colonoscopy
You will get some instructions at your specialist screening practitioner appointment. These will help you prepare for your colonoscopy.
Your bowels will need to be empty to have the procedure. Please follow the instructions carefully. These will include:
-
what you need to eat and drink in the days before your colonoscopy
-
when you should stop eating and drinking
-
giving you sachets of laxatives to drink, or information on how to get them
-
how and when to take the laxatives.
Laxatives will make you go to the toilet more often than usual to help you empty your bowels. This will usually be the day before and sometimes on the day of the procedure.
You are usually awake during a colonoscopy. You can choose to have:
-
painkillers
-
gas and air
-
sedation – medicine given through a small tube (cannula) in your arm.
Some hospitals may not offer all these options.
Having your colonoscopy
Your colonoscopy will take place in the endoscopy unit.
On the day, a nurse or specialist will explain what’s going to happen and possible risks. You’ll be asked to sign a consent form. This is to confirm you understand the risks and agree to have the procedure.
If you agree, they will ask you to change into a hospital gown. You will be covered up for your procedure. The gown has a slit in the back.
They should offer you pain relief options.
To have the test, you lie on your left side with your knees slightly bent up.
The tube goes into your bottom and is guided to the top of your large bowel. The tube bends easily so it can pass around the curves of your bowel.
The colonoscopist will gently pump water or gas (carbon dioxide) in. This opens up your bowels and helps them to see. You may feel like you need the toilet, but your bowels should already be empty so do not worry. It’s normal to feel a bit bloated.
You may have some stomach cramps. Having a colonoscopy may be uncomfortable but it should not be painful. If you feel any pain, let them know. They can make adjustments to make you more comfortable.
They may remove polyps in your bowels or take a small sample of body tissue for a closer look under a microscope. This is called a biopsy. You will not feel anything if this happens because there are no nerves in your bowels.
After your colonoscopy
You will go to a recovery area to rest. Nurses will monitor you until you are ready to go home. You will be told if the colonoscopist removed any polyps or took a biopsy.
You may need:
-
someone to take you home because you could be drowsy, particularly if you have sedation
-
to rest, so you may want to take the day off work or other commitments.
You may feel bloated or have stomach cramps after a colonoscopy. This usually only lasts for 2 to 3 hours.
If you have sedation, you should:
-
have a responsible adult to stay with you for at least 12 hours
-
not drive, drink alcohol or operate machinery for 24 hours.
You may have some blood in your poo or bleeding from your bottom for a couple of days. These things are common. If the symptoms do not go away after 2 days, you should see your GP.
Call 111 or the hospital where you had a colonoscopy if you have:
-
heavy bleeding from your bottom
-
bleeding that does not go away or gets worse
-
severe stomach pain or pain that gets worse
-
a high temperature or you feel hot or shivery.
Possible risks of colonoscopy
In very rare cases, colonoscopy could miss cancer or a polyp that could later turn into cancer. This is more likely to happen if:
-
your bowels are not completely empty
-
it’s difficult to move the camera around your bowels.
See a GP if you have symptoms of bowel cancer. This is important even if you have recently had bowel cancer screening. Read more about bowel cancer symptoms on NHS.UK.
In rare cases, complications can happen during a colonoscopy if you:
-
have a reaction to the sedation
-
have heavy bleeding after colonoscopy
-
get a bowel perforation (small tear or pinhole) on your bowels.
Around 1 person in every 2,500 having a colonoscopy needs a blood transfusion.
Bowel perforations happen in around 1 in every 1,700 colonoscopies. If this happens, you may need surgery to repair it. This will depend on the size and position of the perforation. Some do not need any surgery.
In very rare cases, complications after a colonoscopy may result in death. Colonoscopists are highly trained and this is very unlikely.
These statistics are only a guide for the general population. The specialist screening practitioner will advise you on your personal risk. This will be based on your age and health.
Colonoscopy results
You may get your results on the day, or it could take a few weeks. We also send your GP a copy of your results.
There are 4 main results:
-
normal results
-
polyps found – no further monitoring needed
-
polyps found – further monitoring needed
-
bowel cancer.
Sometimes we find other bowel conditions. It’s possible to find polyps or bowel cancer and other bowel conditions in the same colonoscopy.
Normal results
Around 11 in 100 people have this result.
It means we:
-
did not find any polyps, and
-
there were no signs of other bowel conditions.
We’ll offer you bowel cancer screening again in 2 years if you are still under the age of 75.
Polyps found – no further monitoring needed
Around 50 in 100 people (half) have this result.
It means we:
-
removed polyps during your colonoscopy, or
-
took a sample of cells (biopsy) from your bowels for testing.
After testing your sample, you do not need further treatment or check-up colonoscopies.
We’ll offer you bowel cancer screening again in 2 years if you are still under the age of 75.
Polyps found – further monitoring needed
Around 11 in 100 people have this result.
It means we found a high-risk type of polyp. These are more likely to turn into bowel cancer.
Sometimes polyps are too difficult to remove during a colonoscopy. If this happens, you may need another specialist colonoscopy or surgery.
We will then offer you more regular colonoscopies in the future. This is to check your bowel health and see if you have any new polyps.
Bowel cancer
Between 7 and 10 in 100 people have this result.
If we find bowel cancer, you’ll see a cancer specialist to discuss treatment options and support.
Most people (around 9 in 10) with bowel cancer at the earliest stage have successful treatment.
If you have advanced bowel cancer, it may be hard to treat and not possible to cure.
Other bowel conditions
Sometimes colonoscopy finds no polyps or bowel cancer, but we find other bowel conditions such as:
Around 18 in 100 people have this result.
You can find out more about these conditions on NHS.UK. If we find signs of other bowel conditions, your GP will explain what this means and next steps. You may need treatment or monitoring outside of the bowel cancer screening programme.

Diagram showing results for every 100 people having a colonoscopy
More information and support
For advice about having a colonoscopy, you can phone our free helpline on 0800 707 60 60. If you have hearing or speech difficulties, you can use the Relay UK service to contact us. Dial 18001 then 0800 707 60 60 from your textphone or the Relay UK app.
This information is available in alternative formats, including easy read and other languages. To request another format, you can phone 0300 311 22 33 or email england.contactus@nhs.net.
You can also:
-
talk to your GP
-
read information for transgender and non-binary people about NHS screening programmes.
If you are 75 or over, you can still take part in bowel cancer screening every 2 years, but you will not be invited. You can phone the helpline on 0800 707 60 60 to ask for a home test kit.
We use personal information from your NHS records to invite you for screening at the right time. NHS England also uses your information to ensure you receive high quality care and to improve the screening programmes. Read more about how we use and protect your information.
Find out how to opt out of screening.
