[WITHDRAWN] Bowel scope screening: having a colonoscopy
Updated 9 July 2019

A man his partner at a bowel scope colonoscopy appointment, talking to the colonoscopist.
You have been invited to have a colonoscopy because small growths called polyps were found when you had NHS bowel scope screening. This means there is a chance you have polyps further up the bowel as well.
A colonoscopy checks further up the bowel. This leaflet gives you information about having a colonoscopy.
About NHS bowel scope screening
NHS bowel scope screening helps prevent bowel cancer. For every 300 people screened, it stops 2 from getting bowel cancer and saves 1 life from bowel cancer. The NHS offers bowel scope screening to all men and women aged 55.
NHS bowel scope screening uses a thin flexible tube to find and remove small growths called polyps in the lower part of the large bowel that could eventually turn into cancer. Some people who are found to have polyps during bowel scope screening are offered a colonoscopy.
1. Bowel cancer
Bowel cancer is the term used for cancer that begins in the large bowel. It is also called colorectal cancer. Bowel cancer often starts from small growths in the bowel called polyps. Polyps do not usually cause symptoms but some might turn into bowel cancer if they are not removed. The bowel, also known as the intestine, helps to digest the food you eat. After food has gone through the bowel, all that is left is poo.
The bowel has 2 parts – the small bowel and the large bowel. The large bowel is coloured pink in the picture below.
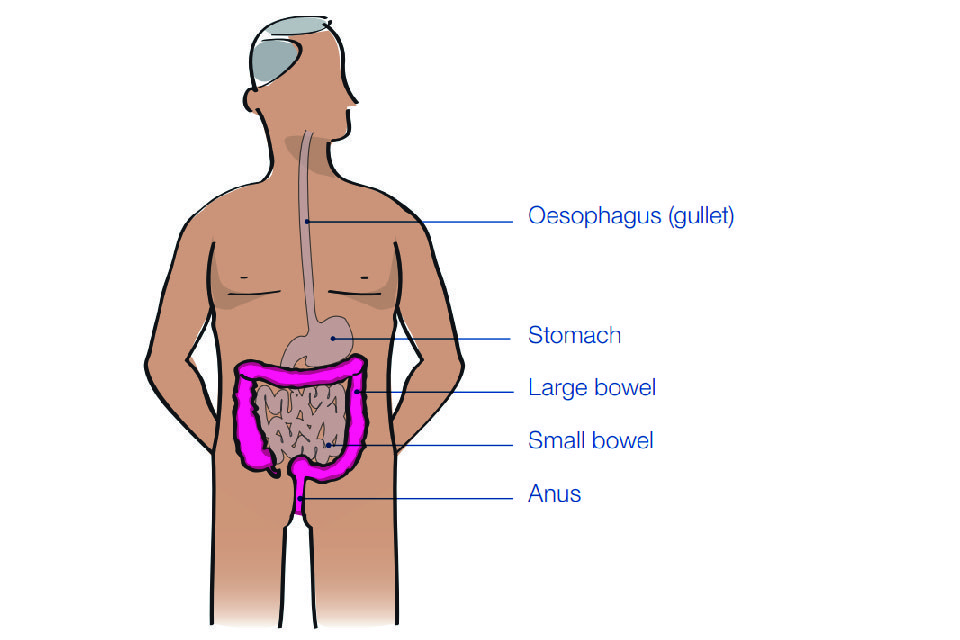
Diagram showing the large bowel (in pink)
Bowel cancer is the third most common cancer in the UK. About 1 in every 18 people in the UK will develop it during their lifetime. Both men and women can get bowel cancer. Bowel cancer is more common in older people – most people who get it are over the age of 55.
People can be at risk of bowel cancer even when nobody else in the family has had cancer.
2. What is colonoscopy?
Colonoscopy is a test similar to bowel scope screening. It checks further up your large bowel than bowel scope screening and takes a longer time. Colonoscopy is done by a colonoscopy specialist (usually a nurse or doctor) at an NHS bowel cancer screening centre. It should take between 30 and 45 minutes, although the whole appointment may take around 2 hours.
In a colonoscopy, the specialist uses a thin flexible tube (a colonoscope) with a tiny camera on the end to look inside your bowel and remove any small growths called polyps. They also use the colonoscope to check the bowel for cancer that has already started.
2.1 Who can have a colonoscopy
Some health problems mean that it might not be possible for you to have a colonoscopy. If this is the case, you will be offered another test instead. The other test will usually be a special type of bowel X-ray called CT (computed tomographic) colonography. This is a way of checking your bowel for polyps or cancer without putting a colonoscope inside your bowel. If polyps are found during CT colonography, they cannot be removed straight away. You would need to come back for another appointment to have them removed.
3. What is involved in a colonoscopy
Before having a colonoscopy, you will be offered a sedative. This is usually given as an injection into a vein in your arm. It is to make the colonoscopy more comfortable and to make you more relaxed. The colonoscopy specialist then puts the colonoscope (thin flexible tube) into your large bowel through your anus and looks inside using the tiny camera.
After putting the colonoscope into your bowel, they will gently pump some carbon dioxide gas inside. This opens up the large bowel so they can see the lining of your bowel clearly.
If they find any polyps, they usually remove them straightaway using a tiny wire loop passed through the colonoscope. The colonoscopy specialist may also take a tiny piece of the inside of your bowel (a biopsy) to look at under a microscope.
3.1 What will happen if I choose to have a colonoscopy?
Before your colonoscopy, you will be invited for an appointment with a specialist screening practitioner (usually a nurse) to talk about having a colonoscopy. They will:
- check that colonoscopy is right for you
- explain what having a colonoscopy is like and the possible benefits and risks
- listen to any concerns and answer any questions you may have about colonoscopy.
The specialist screening practitioner will give you instructions on how to prepare for colonoscopy. They will also give you a medicine to clear your bowel (a strong laxative), to take the day before your colonoscopy. Your bowel needs to be clear so that it can be seen properly during the colonoscopy.
Several days before your colonoscopy
You will need to avoid some foods. The specialist screening practitioner will give you instructions about this.
Arrange for someone to take you home after your colonoscopy as the sedative may leave you drowsy.
The day before your colonoscopy
Take the laxative to clear out your bowel. The laxative acts very quickly and will give you diarrhoea. You will probably need to poo several times and will want to stay near a toilet. We strongly suggest you stay at home that day.
The day of your colonoscopy
When you arrive at the NHS bowel cancer screening centre, you will be able to talk to the nurses and doctors about any concerns or questions you may have.
They will ask you to put on a hospital gown and lie down on a bed ready to have your colonoscopy.
After your colonoscopy
The colonoscopy specialist will tell you whether they removed any polyps or took any biopsies. You will probably feel like resting, so you may want to book the whole day away from your other commitments.
Within 3 weeks of your colonoscopy
You will be sent a letter explaining the results of your colonoscopy. Your GP will also get your results.
3.2 What happens if I choose to have the sedative?
The sedative is usually given by injection into your arm and may make you drowsy. You may be less alert than usual for up to 24 hours.
If you have the sedative, it is important that you:
- don’t drive home
- don’t drink alcohol for 24 hours
- don’t make important decisions for 24 hours
- don’t operate machinery
3.3 What it feels like to have a colonoscopy
Most people feel positive about their colonoscopy (about 89 out of 100). Colonoscopy can be painful, which is why you are offered a sedative.
If you do feel pain, let the colonoscopy specialist know. They can change what they are doing to make you feel as comfortable as possible. It is not usually painful to have polyps removed or a biopsy taken. The carbon dioxide pumped into the bowel is not harmful.
A few people say they found colonoscopy embarrassing (about 4 out of 100). The colonoscopy specialist will do their best to help you feel as relaxed as possible.
After the colonoscopy, sometimes people feel sick or have tummy pain or bloating for a day or two. You may also have some blood in your poo. If the symptoms are severe or don’t go away in 2 days, you should see your doctor straight away.
3.4 Finding polyps and detecting cancer in the bowel
Colonoscopy is a good test for finding polyps or cancer in the bowel. However, there is a small chance (about 5 out of 100) that colonoscopy misses cancer or a polyp that could later turn into cancer. This may be because the bowel was not completely empty or it was difficult to move the colonoscope around the bowel.
4. Possible risks of a colonoscopy
A colonoscopy is usually safe but in rare cases it can cause harm to the bowel. About 1 person in every 400 has bleeding after their colonoscopy but it is usually easy to stop. Rarely, the bleeding is more difficult to stop and means that the person needs to be admitted to hospital. This happens to about 1 in every 2000 people having a colonoscopy. Even more rarely, colonoscopy can cause a small tear in the bowel. This happens to about 1 in every 2500 people having a colonoscopy.
If you have bleeding that is difficult to stop or a tear in your bowel, you will be admitted to hospital straight away. Some people will need surgery to repair their bowel.
5. Possible results of a colonoscopy
5.1 No polyps or only small polyps found
About 2 in every 100 people who have a colonoscopy after bowel scope screening will have a normal result. This means that no polyps or only small polyps that are very unlikely to turn into cancer were found.
Even if you have a normal result, it is important to look out for symptoms of bowel cancer. This is because sometimes people can get bowel cancer even after a normal result. Please see page 11 for more about symptoms of bowel cancer.
If you have a normal result, you will be invited for another kind of bowel cancer screening at age 60 which looks for traces of blood in poo (also known as the faecal occult blood or FOB test). If you would like more information about the FOB test, please see the leaflet called ‘Bowel Cancer Screening: the facts’.
5.2 Polyps that need to be removed
About 92 in every 100 people who have a colonoscopy after bowel scope screening will be found to have polyps that need to be removed. Usually, the polyps are removed straightaway using a tiny wire loop passed through the colonoscope.
If you have polyps removed, you may be invited to have another colonoscopy to check your bowel again. The timing of this depends on how many polyps were found and how big they were.
Sometimes people have polyps that are too difficult to remove during colonoscopy. These people will be offered surgery at a later date to remove their polyps.
5.3 Bowel cancer found
About 6 in every 100 people who have a colonoscopy after bowel scope screening will be found to have bowel cancer.
If cancer is found, you will be given an appointment to see a specialist as soon as possible. If it is found at an early stage, you are more likely to survive bowel cancer.
6. Outcomes for 100 people who have a colonoscopy after bowel scope screening
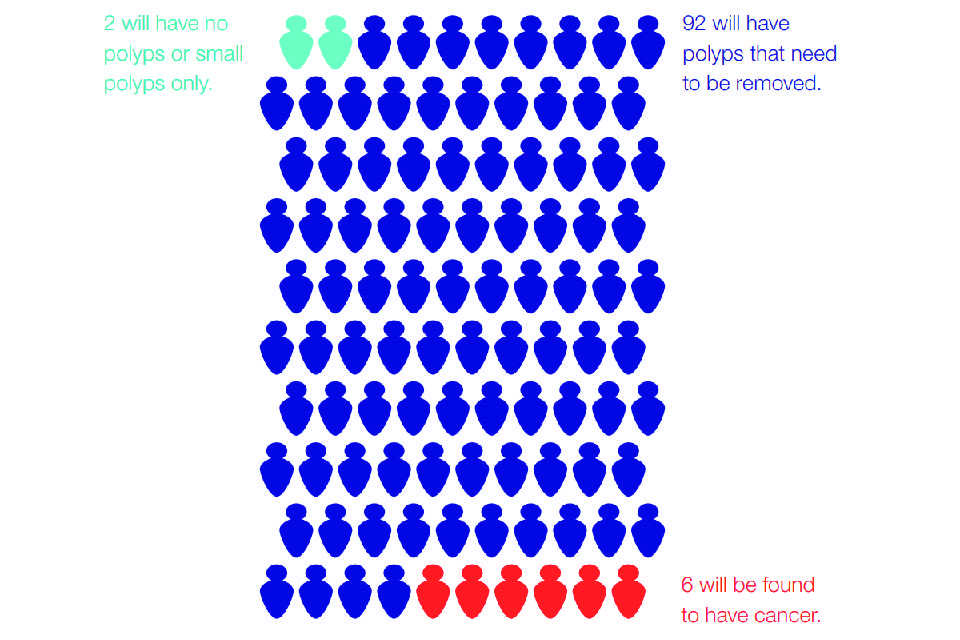
Diagram showing that for every 100 people having colonoscopy after bowel scope screening, 2 will have no polyps or small polyps only, 92 will have polyps that need removing, and 6 will have bowel cancer found.
7. Symptoms of bowel cancer
It is still possible to get bowel cancer after having a colonoscopy so it is important to look out for symptoms. The symptoms of bowel cancer are:
- blood in your poo
- any changes in your bowel habit
- an unexplained lump in your tummy
- poo that is looser than normal
- unexplained tiredness or weight loss
- bloating, swelling or pain in your tummy
If you have any of these symptoms for more than 3 weeks, you should make an appointment to see your GP.
Usually these symptoms won’t mean you have bowel cancer. But if you do, going to see your GP makes it more likely the cancer is found early. The earlier bowel cancer is found, the better the chance of survival.
7.1 Lowering your chances of getting bowel cancer
Bowel scope screening is the best way to lower your chances of getting bowel cancer. You can also:
- be physically active
- keep a healthy weight
- eat plenty of fruit and vegetables and other high fibre foods
- eat less red meat and less processed meat
- drink alcohol in moderation
- not smoke
7.2 Who to contact if you have a question
If you have any questions or concerns about having a colonoscopy, please call the NHS Bowel Cancer Screening Programme freephone helpline on 0800 707 60 60.
Find out how Public Health England and the NHS use and protect your screening information.
Find out how you can opt out of screening.
8. About this leaflet
Public Health England (PHE) created this leaflet on behalf of the NHS.
You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
The following images in this document are used under licence. Contact the copyright holder/s to obtain permission for any further use. Cover image by Alexander Raths (Shutterstock)
