Achieving and maintaining the 36 month round length
Updated 24 July 2025
Applies to England
1. Introduction
This publication provides a good-practice guide for breast-screening services on attaining and maintaining the 36-month round length. It gives information on the principles of planning a screening round. This should ensure services plan enough capacity and resources to screen their eligible population.
Organising screening-round length is a dynamic activity due to:
- population changes
- GP practice reconfigurations
- availability of sites for mobile vans
- availability of static screening sites
- staffing levels
- other organisational factors (administrative and equipment)
It also provides advice on methods to ensure round-length targets are achieved by using intelligent appointment-booking techniques. This guide provides possible solutions to any problems you may experience in achieving and maintaining round-length targets.
2. Background
2.1 Basic principles of screening
The NHS routinely invites all people registered with their GP as a woman[footnote 1], aged between 49 years and 8 months and up to 70 years and 11 months, for breast screening with mammography every 3 years. In addition, 68 services are participating in the age extension trial (AgeX) assessing the impact of 2 additional rounds of screening invitations. At these services, all eligible people in the age range 46 years and 10 months and up to 73 years and 11 months are selected into each screening batch. The Breast Screening Select (BSS) system (the call and recall IT system linked to the National Breast Screening System (NBSS)) randomly allocates either the lower or upper age group to be screened. Screening batches therefore either contain eligible people in the age range 46 years 10 months to 70 years 11 months, or 49 years 8 months to 73 years 11 months.
The screening programme sends eligible people, including those randomised into the trial, a letter giving details of the time, date and location of their screening appointment. People are called to attend screening according to their GP practice, postcode area (outcode), next test due date for screening (NTDD), year of birth, month of birth or a mixture of these. An eligible person receives their first screening invitation any time between the age of 46 years 10 months and 52 years 11 months, depending on the age range randomised in. All eligible people should receive a screening invitation before their 53rd birthday.
2.2 Explanation of terms
Screening round length (SRL)
Screening round length is the interval between the date of a person’s previous screening mammogram and the date of their next first offered appointment. Round length is measured by the percentage of eligible people whose first offered appointment is within 36 months of their previous screen. Achieving the national standard for round length is not affected by people choosing to alter their screening appointment. A person’s round length is determined by the date of their first offered appointment (DOFOA) prior to attendance.
Round length is measured for recall people (those who have been invited at least once). The round length for a recall person who did not attend their previous appointment is measured from DOFOA to DOFOA.
Screening round plan
The screening round plan sets out how the service manages to screen all its eligible population within 36 months. Failure to maintain the screening round plan with up-to-date information (for example, population figures and GP practice details) can lead to poorly planned and under-resourced screening services (see Appendix 2).
Age range
Services invite eligible people from aged 49 years and ≥8 months to 70 years and 11 months and, for those services participating in the AgeX trial, 46 years and 10 months to 73 years and 11 months. For the purposes of batch specification (choosing which age ranges will be in a batch), individuals should be no younger than 46 years and 10 months (if in AgeX) or 49 years and 8 months. At the upper-age limit, all eligible people should be included up to 70 years 11 months or up to 73 years and 11 months (if in AgeX). This is based on age at selection in the batch, rather than the person’s age at screening. People under 46 years 10 months are automatically rejected from batches in BSS.
The age range for a failsafe batch is 52 years 11 months to 70 years 11 months, in accordance with failsafe guidance.
Optimal screening interval and justification
Services should re-invite people for screening at 36-month intervals. This means inviting people to have their next breast-screening appointment so that it occurs within 36 months of their previous screen. Maintaining round length helps achieve the desired mortality reduction by:
- detecting cancers as early as possible
- minimising interval cancers (cancers presenting between screening episodes)
- reducing negative consequences of inviting people too frequently
AgeX trial
The AgeX trial offers an earlier screen to people aged 46 years and 10 months to 49 years and <8 months (who will all be offered routine screening 3 years later), and an additional screen to people aged 71 years and 0 months to 73 years and 11 months (who will already have been offered routine screening previously). Half the eligible population is randomised to receive an invitation in the extended age ranges. Of the 78 breast screening services, 68 are taking part in the AgeX trial.
Ensuring completeness of screening episodes
NBSS uses codes to describe the outcome of various procedures carried out during screening. The screening office must ensure all invited individuals have the appropriate outcome code associated with their screening episode in a timely manner. It is good practice to ensure that all screening episodes are closed within 6 months of their DOFOA. On BSS this is technically 6 months from the episode open date. Definitions of NBSS outcome codes relating to round length are in Appendix 5.
3. Screening round-length planning
Before starting your round-length plan, it is essential you regularly update and register details of GP practices and the records of eligible people on NBSS. This information is provided by BSS, which allows this information to be transferred electronically. Check with local contacts to keep updated with upcoming changes to GP practices. Where mobile sites are in use by providers, having clearly documented agreements in place can help ensure that mobile locations are still available for use, or an agreed notice period can be given for any changes.
Update round-length plans if you identify changes that will impact on the current plan.
Plan to screen the eligible population within a period of less than 36 months to ensure screening round-length targets are achieved. Plan to invite people between 34 to 36 months of their last invitation. This will give time to accommodate unforeseen circumstances and reduce the risk of slippage.
3.1 Principles of screening round-length planning
To create a round length plan, population calculations are required to determine if the service has enough resources to screen the population it serves. Follow these steps.
- Use the BSS recall interval safety period (RISP) or NTDD population estimates (breast-screening population estimates – population count) to determine how many people will need to be screened in the next 36 months. The age range included in this report will depend on whether you are part of the AgeX trial (see Appendix 1).
- Calculate your operational capacity by looking at the numbers of mobile and static units available for screening and the number of days these will be operational (factoring in maintenance and bank holidays). Then calculate how many people need screening each day and week using your current resources (see Appendix 1).
- If the service’s screening population fits within the existing capacity (on these calculations), maintaining round length is achievable. If these calculations demonstrate insufficient capacity, you need to consider alternative service methods to resolve this. These may include using Smart clinics (see section 6.1 below), extended days and weekend working. Occasionally services may need to request additional resources in discussion with their trust and commissioners.
- Additional capacity will also be required for people who self refer, people who are selected into routine failsafe batches, and also for second timed appointments (see below).
3.2 Building a new screening round plan
Once you have determined that you have sufficient capacity, add more detail to the plan. This involves:
- generating GP practice lists, including when the practice was last screened
- preparing an overview of the screening plan in weeks, by screening facility
- preparing a detailed screening plan by GP practice/outcode area/date of birth/NTDD by screening facility, giving expected screening dates for each batch of people invited
You can also include other information such as population counts, previous uptake, and dates for batch specification.
Services must ensure that the referral patterns for patients diagnosed with cancer via screening are evenly distributed across different hospitals in the 3-year cycle.
Any redesign of the screening round plan could result in some people being screened before or after 36 months (under exceptional circumstances). Only do this with the approval of screening commissioners and the quality assurance team (SQAS). It is important that SRL targets are met.
4. Methods of invitation
There are different methods of inviting people in batches. How to specify a batch is covered in Appendix 3.
4.1 Standard screening batches
All batches must firstly have a batch ID generated within NBSS. Standard screening batches, also known as Recall Interval Safety Period (RISP) batches are created and selected within BSS. You can break the batches down by both GP practice and outcode.
When using RISP to estimate the number of people selected into a batch for a specific GP practice or outcode, consider the effect of the safety period used in the batch specification. A 24-month safety period is used to maximise the number of people included in the routine batch, and minimise the number of people who would need to be screened via the routine failsafe process. The batch will include all eligible people within the age band who are due for screening in the next 24 months. This will include all the people counted in this year’s estimate or next year’s estimate and also a proportion of the additional people counted in the third year’s estimate.
4.2 Calling by NTDD
Some services call people for screening by NTDD. You can determine population counts as detailed in Appendix 1. It is useful for services to understand when their population is due for screening, and this can be found using the BSS report ‘NTDD screening estimate’.
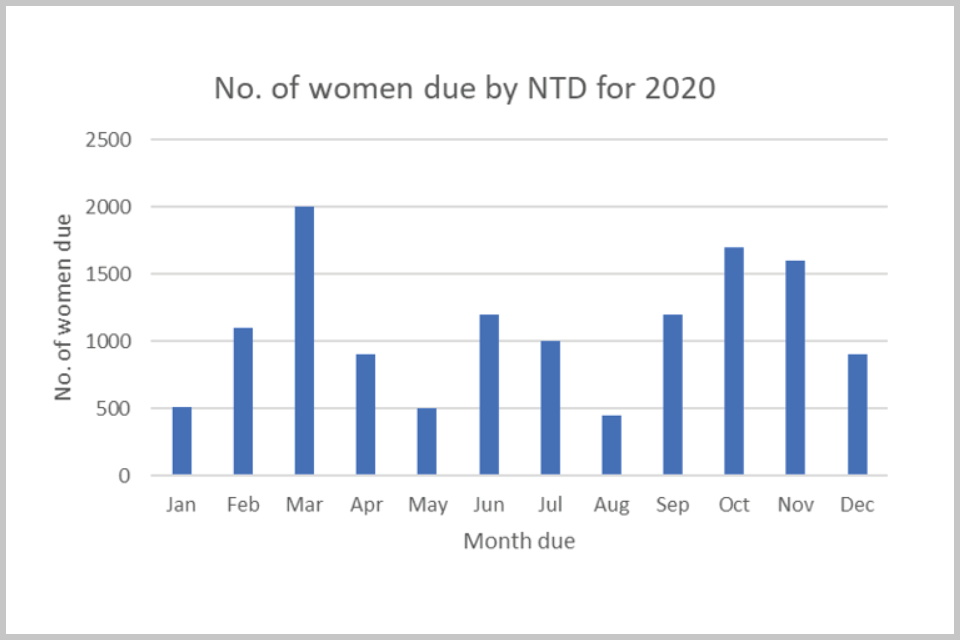
Figure 1: bar chart showing estimated numbers of eligible people for screening each month, based on next test due date (NTDD)
The NTDD screening estimate shows when people are due for screening within the specified dates. To be counted in the estimates a person must be eligible by date of birth and also NTDD, where they have one. Each person is only counted in one of the months of estimations.
4.3 GP practice
You may use the GP practice code in combination with RISP or NTDD. Using the GP practice code can help services map the location of suitable screening sites.
4.4 Date of birth
To specify people in a batch by date of birth, use a method of month selection. Services using this method may visit each GP practice annually. This can be used in combination with the above methods.
4.5 Outcode or area code
The outcode is defined as the first 2, 3 or 4 characters of the postcode. Using the outcode enables services to map the location of suitable screening sites. This can be used in combination with the above methods.
4.6 Obtaining numbers of people in a screening batch
The population estimate report from BSS counts the number of eligible people who are due for screening during a specified period. People who have never been screened are included in the call count, and people who have been previously screened (either in a batch episode or as a self referral) are included in the recall count.
A guide for RISP or NTD estimates is available within the BSS users manual.
4.7 Routine failsafe batches
It is possible for a person to become ‘out of sync’ with their screening cohort. This might be because they have recently moved into an area that has already been screened, or they have moved GP practice. You must invite such individuals at their NTDD. If a person has not been invited previously, you must invite them before they turn 53.
People in the AgeX trial who were historically randomised out of screening within the NBSS system in the lower age range have a NTDD on BSS which ensures they will be screened before the age of 53.
Routine failsafe ensures all people within the specified age range are invited within 36 months. Run routine failsafe batches at monthly intervals, specified and selected between day 13 and day 17 of each month. The number of people expected can vary depending on the size of the screening programme. The BSS routine failsafe report indicates the number of people due for screening in the next month and provides the batch specification parameters. If the number of people within a routine failsafe batch appear unusually high, you should investigate the reasons. This may be due to round-length slippage (where people who are overdue for screening are picked up in a routine failsafe batch rather than in their routine screening batch). You should exclude such people from the failsafe batch but include them in an appropriate standard screening batch, in accordance with failsafe guidance.
If large numbers of people from a single GP practice appear on the failsafe list, undertake checks to establish whether this GP has been overlooked on the round plan.
Routine failsafe batches may have lower uptake rates than normal batches, so it is worthwhile considering booking routine failsafe batches into routine Smart clinics to maximise capacity.
4.8 ZZZ registration
‘ZZZ GP code’ is included automatically in the routine failsafe batch when specifying the batch by ‘all’ as part of the batch selection process. However if you are deviating from the standard failsafe process, make sure that ‘ZZZ GP code’ is included.
5. Revising a screening round plan
Keep screening-round plans under constant revision because of changes in population and screening-service resource capacity. Several factors need to be considered, as outlined below.
5.1 Previous screening plans
It is important to have accurate records of who has been screened, when and by what method, to help plan the next screening round. This will identify when the GP practice is next due for invitation.
5.2 Batch reports
NBSS provides useful information about previous batches and how they were specified and when they were booked. Screening services may also have historical records which can provide useful information about previous screening batches.
5.3 Crystal reports
There are several Crystal reports (bespoke reports) to interrogate NBSS which can help in re-planning a screening round to achieve round length (see Batch round-length sorter MCO004 and the SR044 previous screen-date checker).
5.4 Population data
The population may have changed since the last round plan. Your will need to recalculate the screening population to check how this affects resource capacity.
5.5 Maximising uptake
For services which use mobile screening units, the location of the mobiles can have a considerable impact on screening uptake. There may be periods when previous sites are not available. This can impact on a service’s screening round plan.
A reduction in the number of locations can release additional screening days which would otherwise be lost in moving and re-calibrating mobile screening units. In rural areas, this needs to be balanced against the need to make the service accessible.
5.6 Screening to assessment waits
Insufficient assessment capacity can mean the number of people screened has to be reduced to ensure people do not wait longer than 3 weeks for an assessment appointment. This may have an impact on the ability of the service to achieve the 36-month round length.
6. Maintaining round length through intelligent appointment booking within NBSS
6.1 Booking methods
36-month round length can be maintained by the following NBSS appointment booking techniques:
Optimising (booking recalls before calls)
This is the most common method to ensure people with a previous screen date are appointed first. It is useful when you have SRL slippage and should be used in combination with selective booking or Smart clinics.
Randomising
This method is often used by services that have no SRL slippage. Call and recall people are randomly allocated to appointment slots. We recommend that this method is only used if all the clients in a batch can be invited before the date the batch started in the round previous. This will ensure all clients in the batch keep to their 36-month round length.
Selective booking
There are several options services can choose under the selective booking drop-down menu. They are based on a variety of characteristics, of which you can choose up to 2 at any one time including:
- age when episode opened
- attendance probability - based on % probability of attendance, for example 80% to 100%
- perpetual non-attender - selects clients who were 57 or more at the episode creation date, have episode character ‘F’ and Prevalent/Incident Status ‘XP’
- DNA last invite only - previous attender but failed to attend last time
- first ever invite at the office - first invitation issued by your office
- last invite - selects people who were aged 68 or more at the episode-creation date
- postcode - useful to allocate to nearest screening location, particularly failsafe batches
- call
- recall
- special appointment
Smart Clinics
Smart clinic functionality is a probability-based booking feature of NBSS to help screening services achieve and maintain round length.
If a screening clinic is a Smart clinic, NBSS fills its timeslots with a variable number of appointments according to the probability of each person attending. NBSS fills a timeslot with appointments until there is a good chance of at least one person attending the slot. This results in slots with a likely attender or many unlikely attenders. Smart clinics can contain a mixture of first and second appointments. When smart clinics are used across all sites, this removes the need for ‘DNA clinics’ dedicated to second timed appointments.
Smart clinics can increase the capacity of a screening clinic considerably, particularly if the uptake of the practices being screened is low. Smart clinics can also provide the capacity for second timed appointments without the need for additional clinics. In many cases, batches that could take up to 4 weeks to screen for example, can be reduced by up to a week. It is important to monitor the use of Smart clinics to ensure screening-round length is maintained. A service should monitor the performance of Smart clinics and adjust accordingly.
Increasing the number of appointments available per day
Offices may also extend the working day to increase the number of appointments they can offer. Offices may also utilise weekends and bank holidays. This will depend on staffing resources. Services can extend the working day using a shift system.
Figure 2 shows an example of a service that has developed 3 different lengths of working day. It operates between 8am and 8pm depending on which shift pattern is in operation.
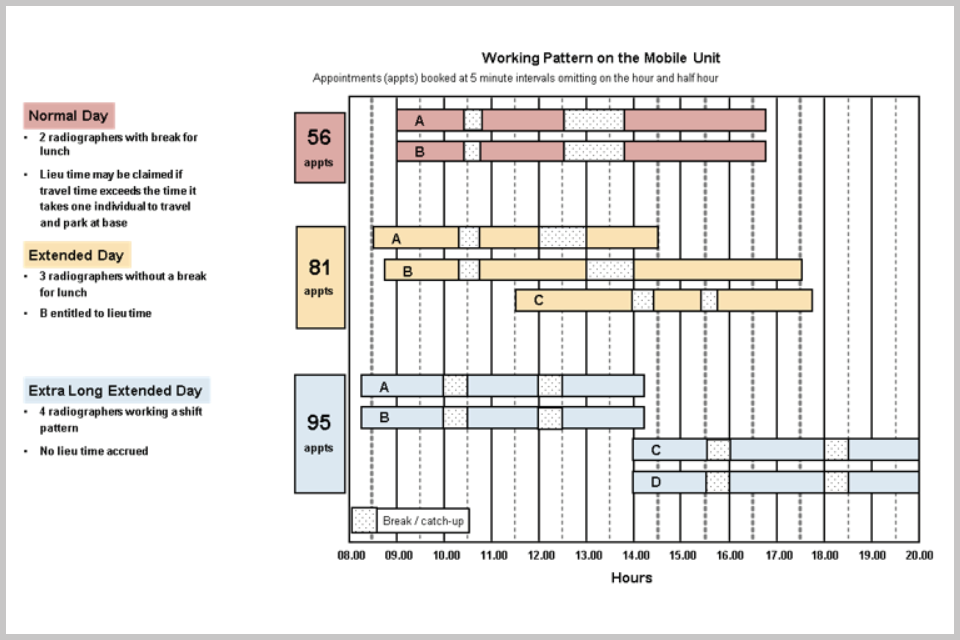
Figure 2: a chart giving an example of 3 different lengths of working day
Using DNA clinics
People who have previously DNA’d appointments are less likely to attend future appointments. You can use ‘DNA clinics’ to block book multiple people who have failed to attend in the past so that appointments are not wasted. This needs careful planning as it may cause delays to later appointments in the day if all invited people attend.
6.2 Factors for consideration
Second timed appointments
The service specification states that all people who DNA their first appointment are offered a second timed appointment. If a service is in round-length slippage you should approach the commissioning team and SQAS to approve the temporary suspension of offering second timed appointments until your service has caught up on its round length. Discuss and record this at a programme board meeting.
Uptake
You can use historical GP batch uptake to estimate uptake in new clinics. If uptake is expected to be low, services could choose to create extra screening timeslots which would allow them to invite more people each day, thereby using resources more effectively.
Confederated GP practices
This is where several practices have merged under one practice code (cancelling the other GP practice codes). This can often create a ‘super practice’ with a large population under just one screening service. It is necessary to check which cancelled codes were screened and date of screen, and then under the one code assess what this will mean in terms of numbers.
There are several things the service can do in these circumstances.
If the screening plan allows and the service has capacity to screen the total population created by the merger, then the practice can be selected and screened.This could result in people being screened on time, early or late.
If the numbers are too great and would put the rest of the plan at risk, the service can select the practice using an NTD date to prioritise those people who need screening sooner. This will omit those who have either been screened more recently or are not yet due. Using this method will only select ages 50 to 70 (49 years and 8 Months to 70 years and 11 months). Seek agreement from SQAS and commissioners to use NTDD methodology if the service is in the Agex trial. The service should be aware of how many additional people need to be screened at a later date and when they will appear in the screening cycle.
It is also possible that some people may appear in routine failsafe batches if the service was unaware or had not planned for the merger. This can create extra screening demand that the service was not prepared for. People from the younger age ranges from such practices, if not selected by using NTDD, will be picked up in routine failsafes so they will not be missed.
You should check that the population numbers the service receives are fairly comparable to the previous numbers from 3 years ago. Check the latest RISP/NTD estimate on BSS for practice counts before creating the batch.
You can use selective booking to send people to their nearest screening location when practices merge from a large geographical area. Services should create good communication links with SILs for advance notification of practice mergers. The BSP Programme Board should discuss any upcoming practice re-organisation.
Unanticipated short-term impacts on round length
Re-planning may be needed due to unexpected situations such as:
- a large number of self-referrals due to a national campaign or high profile breast cancer reports in the media
- consolidated or merged practices (particularly at short notice)
- prolonged equipment breakdown
- mobile site unavailability (particularly at short notice)
- a change in clinical practice that affects assessment clinic numbers
- IT issues
- reprocurement or closure of a screening service
- staffing issues
Reduced assessment capacity
A screening service may have to reduce the number of people invited to attend for screening (and consequently have a reduced round-length attainment) because of insufficient assessment capacity. In these circumstances, you should hold discussions with the commissioning team and SQAS, and record the outcome at a programme board meeting.
Using Crystal reports
There are several Crystal reports available on the NBSS website which can help achieve round length. These are particularly helpful where a service is very close to screening at 36 months, and a few days will make the difference between achieving the target and failure.
The batch round length sorter (MCO004) Crystal report allows services to manage round length at an individual-person level. Book the batch (or part-batch) of people into the clinic and then run the report against that batch of people (see Appendix 4 on how to run Crystal reports). The report identifies any people who have breached their 36-month round length. This then enables you to cancel and rebook these people using the ‘hospital’ cancellation function into any available earlier timeslots. The new appointment has to be within 36 months of the date of the previous screen.
The batch round-length sorter is not so useful if a service arrives late at a screening location. However, there is a report SR044 (previous screening date checker) that can identify such issues once the batch is on the NBSS system, to determine how much of the practice will be out of the screening round-length target.
7. Monitoring round length
The screening service should regularly monitor the round length to ensure that the round plan is working efficiently. The SQAS also monitors round length on a monthly and quarterly basis for ongoing monitoring and reporting to commissioners.
Screening services should run the SR050 (round length) report every month and submit the output to the regional SQAS team. The SR050 report measures the number of weeks overdue, which helps identify how far behind your service is in achieving the target 90% within 36 months (see Appendix 4).
An alternative report (SR002) is available which provides this information in months rather than weeks. This can provide a useful snapshot of a service’s performance.
-
Trans men and non-binary people assigned female at birth who are registered with a GP as female are invited for breast screening. Trans men and non-binary people assigned female at birth who are registered with a GP as male are not routinely invited for breast screening but can request screening. ↩
