NHS Diabetic Eye Screening Programme: grading definitions for referable disease
Updated 4 December 2025
Applies to England
Contains definitions for retinal screening images graded by the NHS Diabetic Eye Screening (DES) Programme. Images can be used for training purposes.
1. Classifying referable retinopathy
1.1 Feature based grading (FBG)
Graders identify individual features of diabetic retinopathy (DR) by selecting a given feature from the feature-based grading (FBG) form. This produces a grade which is determined by rules applied in the grading software.
1.2 Questionable features
Grading should be carried out in accordance with national guidance. Equipment should meet national specifications and used in line with recognised procedures for grading. This includes:
-
avoiding excessive enhancement of images (beyond scale of 1:1)
-
only recording lesions that are present
Microaneurysms should be differentiated from pigment spots by viewing in colour and red free and from artefacts by viewing on overlapping images where possible.
Intraretinal microvascular abnormality (IRMA) should not be recorded unless visible on colour images, without enlarging the image area, in addition to red free images.
1.3 Cotton wool spots
Isolated cotton wool spots (one or more) in the absence of any microaneurysm or haemorrhage should be counted as no DR (R0).
Any number of cotton wool spots (CWS) in the presence of other non‐referable features of DR should be graded as background DR (R1).
Where CWS are detected, graders should ensure they have checked for features of referable DR – in particular IRMA and early venous beading.
1.4 Venous loops
A venous loop should no longer be referred and should be regarded as a feature of R1.
1.5 Photocoagulation scars
Assign a P0 grade if no evidence of previous photocoagulation. Assign a P1 grade if evidence of previous photocoagulation (focal/grid to macula or peripheral scatter).
1.6 Definition of the macula
The macula is defined as the part of the retina which lies within a circle centred on the centre of the fovea. The radius is the distance between the centre of the fovea and the temporal margin of the disc.
2. Grading classification for pre‐proliferative DR (R2)
The R2 grade is sub divided into lower risk R2 (R2 L) and higher risk R2 (R2 H): The retina is divided into quadrants with a vertical and horizontal line through the middle of the disc.
Lower risk R2 L is defined as R2 not meeting the Higher Risk R2 definition. Higher risk R2 is defined in line with the International Classification 4-2-1 rule as set out below.
Lower risk R2 (R2 L), identified using the standard 2 field RDS photography, should be referred to Digital Surveillance initially so that additional images can be obtained to ensure there is no referable disease in the more peripheral retina. R2 L can then be monitored in Digital Surveillance unless there is progression to referrable disease, the images become un-assessable, or there is progression to higher risk R2.
Higher risk R2 (R2 H) identified in the standard 2 field RDS photographs should always be referred to Hospital Eye Services
The grading classification for R2 is the presence of any of the features below and they should be assessed to determine if they reflect R2 Lower risk or R2 Higher Risk:
Higher risk (R2 H) is defined the presence of ANY of the following features:
- More than 20 intraretinal haemorrhages or microaneurysms in EACH of the four quadrants of the retina, where the quadrants are centred on the centre of the optic disc with a line bisecting the disc vertically and horizontally.
- Venous beading in two or more quadrants
- Moderate IRMA equal to or worse than the Airlie House ETDRS Standard photograph 8a in one or more quadrants**
Lower risk R2 (R2 L) is defined as the presence of ANY of the following features:
- 8 or more blot haemorrhages (MBH)
- More than 20 intraretinal haemorrhages or microaneurysms located in 1,2 or 3 of the four quadrants of the retina where the quadrants are centred on the centre of the optic disc with a vertical line bisecting the disc vertically and horizontally.
- Venous beading in 1 quadrant
- Any quantity of IRMA less than ETDRS Standard photograph 8a
2.1 Haemorrhages and microaneurysms
These haemorrhages and microaneurysms (HMAs) are in the retina’s inner nuclear and outer plexiform layers. They are restricted in a particular location, and so take longer to clear than a superficial haemorrhage.
Flame haemorrhages are superficial haemorrhages in the nerve fibre layer. Any haemorrhage that is flame shaped or any MA should not be counted as a blot.
Refer people with more than 20 HMAs in each of the 4 quadrants of the retina, i.e. R2H.
A cluster of haemorrhages and microaneurysms in one or more quadrants can indicate a retinal vein occlusion (branch or hemi-retinal or central retinal vein occlusion) and this should be considered before grading as R2.

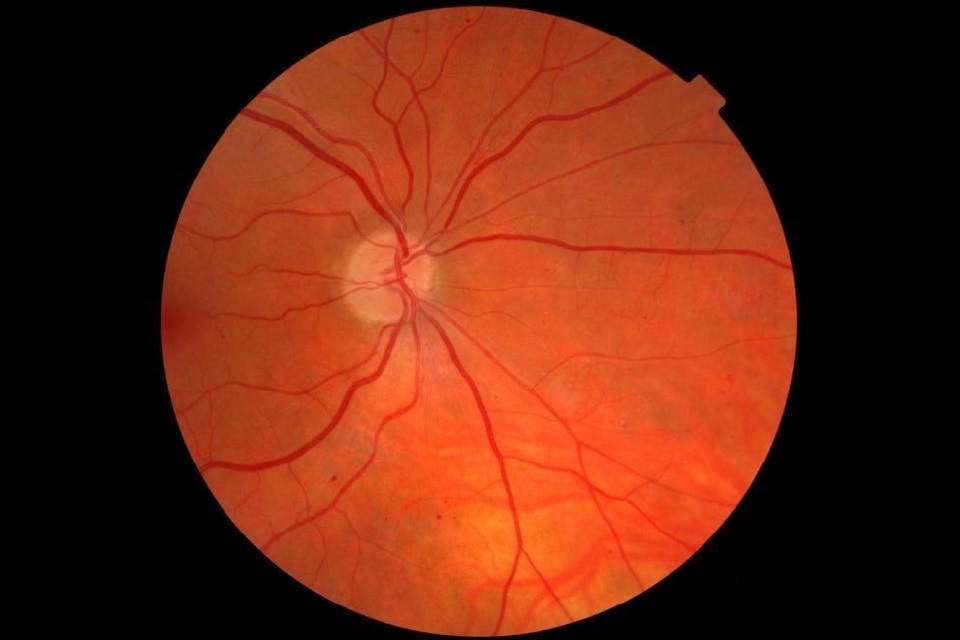
MBH macula

MBH macula red free

MBH nasal

MBH nasal red free
The images above show MBH, where you can identify more than 20 HMAs in 1, 2 or 3 quadrants that would give a classification of R2L. Images where you can identify more than 20 HMAs in all 4 quadrants would be classified as R2H and should be referred. (It can be helpful to assess the number of HMAs in the quadrant with the least number of haemorrhages first when considering if a set of images meets the R2H definition.)
2.2 Venous beading
Refer people with venous beading if involves 2 or more retinal quadrants as per R2 H definition. Venous beading from ischaemia in DR does not take place in isolation from MBH or IRMA.
2.3 Intraretinal microvascular abnormality (IRMA)
People with IRMA equal to or greater than ETDRS standard photograph 8a should be referred as they would classify as R2H.

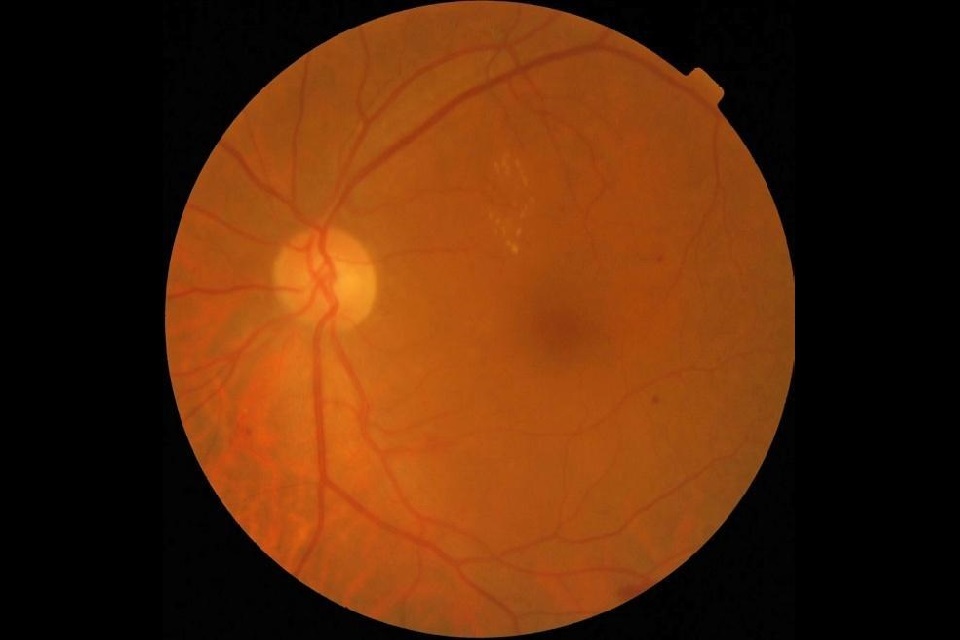
Standard Image 8A

Standard Image 8A Red Free
** ETDRS Standard photograph 8a standard photograph shows multiple patches of moderate IRMA and it is the severity and quantity of IRMA present within 1 quadrant which should be assessed to determine if there is equal to or greater levels of IRMA present within 1 quadrant.
Only IRMAs that are definitely seen should be classified as R2.
If an IRMA is found, the grader should return to the colour image. IRMA is considered present if the IRMA can still be seen on the colour image, that has not been enlarged, as well as on the red free.
If an IRMA can only be seen on a red free image and not on the colour image a referral should not be made and the images should be graded as no IRMA present and should be returned to annual screening.
The above assumes screen settings, colour balance, monitor, software and camera settings are optimal according to the recommendations of the NHS DES Programme.
Sometimes collaterals from vein occlusions can look like IRMAs. In cases where there is a localised patch of possible IRMA, the likelihood of a vein occlusion should be considered. If it is judged that small collaterals are present from an old vein occlusion rather than IRMA, this should not be given an R2 grade.
There are 3 examples of IRMA images below.

IRMA 1

IRMA Image 1 Red Free
IRMA 2

IRMA Image 2 Red Free
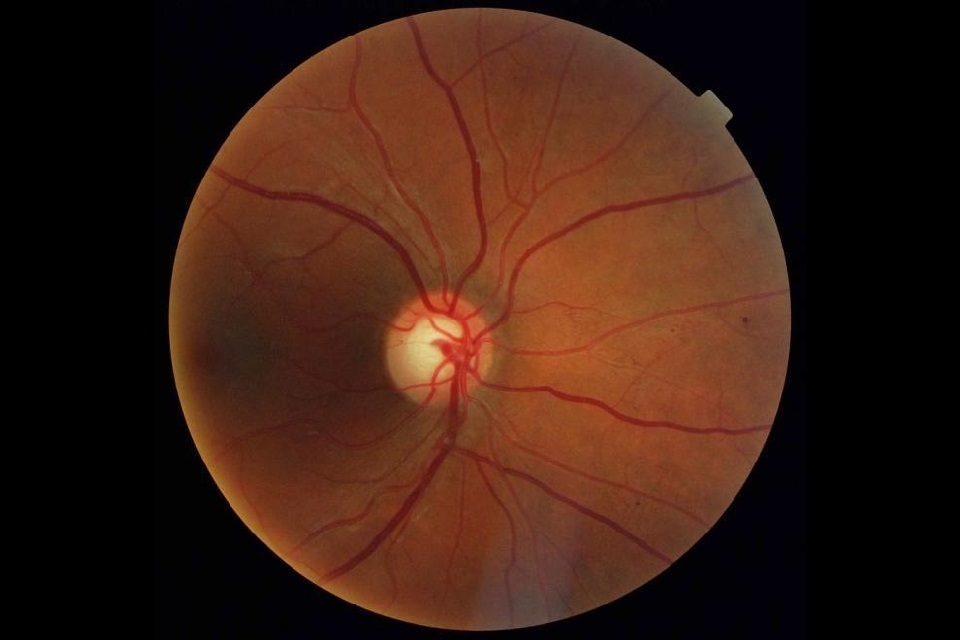
IRMA 3

IRMA Image 3 Red Free
3. Grading classification for proliferative DR (R3)
The new classification consists of 2 categories – R3A (active proliferative retinopathy) and R3S (stable treated proliferative retinopathy).
This allows for urgent attention where disease is active. It also helps maintain a high quality monitoring pathway outside the hospital eye service (HES) for discharged people once treatment has allowed the condition to stabilise.
3.1 R3A
People should be classified as R3A (active) when:
- they have newly presenting proliferative retinopathy
- previous treatment has not been deemed stable by the treating ophthalmologist
- new features indicating reactivation of proliferation or potentially sight threatening change from fibrous proliferation can be seen with respect to a previously obtained reference image set
3.2 R3S
R3S (stable) is when there is:
- evidence of peripheral retinal laser treatment
- a stable retina with respect to reference images taken at or shortly after discharge from HES
A referral outcome grader (ROG) will always be responsible for the decision as to whether the presentation can be considered stable. They may make that decision based on photography and patient history when encountering people who have moved from other screening services.
A referral should be made as R3A in any case where there is doubt.
3.3 Pathway
On discharge, the HES must either:
- place a benchmark set of images on the screening service software
- supply a benchmark set of images electronically for the service to import
- arrange for a set of benchmark images to be taken by the screening service within 3 months
These should be graded by the discharging clinician to make sure they represent a stable condition.
When the individual is screened again, their images must be compared with the benchmark images taken on discharge before deciding the grade.
People who are graded as R3S following discharge from the HES should be managed in the DS pathway.
People with stable treated retinopathy currently in routine annual screening should:
- be graded as R3S at their next routine annual screen
- have benchmark images taken
- be transferred to DS pathway for their next and subsequent routine appointments
The only R grades that will be allowed for such people are R3A and R3S
The grading would be R3S if there are no significant changes from the baseline discharge images.
If there are significant changes then the patient would revert to R3A and be urgently referred back to the HES. Not all changes will be clinically urgent but the grading committee decided it is better to keep things simple and not introduce the concept of routine referral of R3.
Significant changes requiring urgent re-referral would include:
- signs of active neovascularisation (including active new vessels)
- pre-retinal or vitreous haemorrhage
4. Grading classification for maculopathy – groups of exudates (M1)
A group of exudates is an area of exudates that is greater than or equal to half the disc area and all within the macular area.
4.1 How to work out the area
The outer points of the exudates are joined and compared to half the area of the optic disc.
4.2 Referable groups of exudates
In this section you’ll find examples of referable and non-referable groups of exudates.
The example below (GE1) would not be referred. This is an image showing an area of exudates that is less than half a disc.

GE 1
The example below (GE2) would not be referred. This is an example of an area of exudates that is less than half a disc area, borderline in size, but less than half a disc within the macular area.

GE 2
The example below (GE3) would be referred. This is an example of an area of exudates that is greater than half a disc.
GE 3
The example below (GE4) would also be referred. This is an example of an area of exudates that is greater than half a disc.
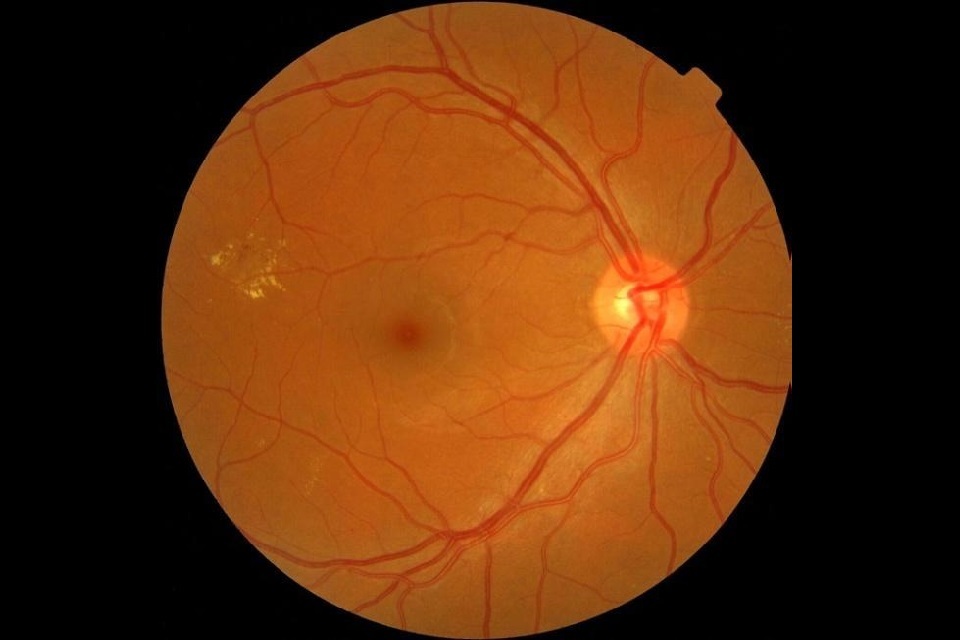
GE 4
5. Classifying the macula where amblyopia and age-related macular degeneration (AMD) are known
There will be cases when the VA is less than or equal to 6/12 and microaneursms or haemorrhages present within one-disc diameter of the centre of the fovea.
If screener has documented known amblyopia, or there is AMD which may also show exudates within the macula to account for the poor VA:
- the images should be graded by the ROG
- decide whether the reduced vision is due to the amblyopia, the AMD or diabetic maculopathy
If the ROG decides the reduced vision is due to the amblyopia or AMD, the maculopathy should be graded as M0. Follow local protocols for referral of non-DR lesions.
If the ROG decides that the reduced VA could be caused by diabetic maculopathy, grade the maculopathy as M1 and refer the person in accordance with the nationally recommended pathway.
6. Early treatment DR study (ETDRS) final retinopathy severity scale
6.1 No apparent retinopathy
ETDRS (final) grade: 10, 14 and 15
Lesions: DR absent DR questionable
Risk of progression to PDR in 1 year (ETDRS interim): N/A
ETDRS screening or clinic follow up intervals: N/A
English Screening Programme levels: R0 currently screen annually
Scottish Grading Classification: R0 currently screen annually
6.2 Mild NPDR (1)
ETDRS (final) grade: 20
Lesions: micro aneurysms only
Risk of progression to PDR in 1 year (ETDRS interim): N/A
ETDRS screening or clinic follow up intervals: 1 year
English Screening Programme levels: R1: screen annually. Background microaneurysms, retinal haemorrhages, any exudate
Scottish Grading Classification: R1: screen annually. Background dot haemorrhages microaneurysms, hard exudates cotton wool spots, blot haemorrhages superficial or flame shaped haemorrhages
6.3 Mild NPDR (2)
ETDRS (final) grade: 35a, 35b, 35c, 35d, 35e
Lesions: One or more of the following: venous loops > definite in 1 field SE, IRMA, or VB questionable. Retinal haemorrhages present HE > definite in 1 field SE > definite in 1 field
Risk of progression to PDR in 1 year (ETDRS interim): Level 30 = 6.2%
ETDRS screening or clinic follow up intervals: 4 to 6 months
English Screening Programme levels: R1: screen annually. Background microaneurysms, retinal haemorrhages, any exudate
Scottish Grading Classification: R1: screen annually. Background dot haemorrhages microaneurysms, hard exudates cotton wool spots, blot haemorrhages superficial or flame shaped haemorrhages.
6.4 Moderate NPDR
ETDRS (final) grade: 43a, 43b
Lesions: H/Ma moderate in 4 to 5 fields or severe in 1 field or IRMA definite in 1 to 3 fields (ETDRS: Grade 0 = no evidence of IRMA. Grade 1 = questionable IRMA. Grade 2 = IRMA present < standard photo 8A. Grade 3 = IRMA present > standard photo 8A but < standard photo 8B. Grade 4 = IRMA > standard photo 8B)
Risk of progression to PDR in 1 year (ETDRS interim): Level 41 = 11.3%
ETDRS screening or clinic follow up intervals: 3 to 6 months
English Screening Programme levels: R2: refer to ophthalmologist. Pre-proliferative MBH IRMA venous beading, venous reduplication. It is recommended that venous loop is removed
Scottish Grading Classification: R2 Background DR BDR – observable. Rescreen 6 months. 4 or more blot haemorrhages (in other words: AH standard photograph 2a – in one hemi-field only)
6.5 Moderately severe NPDR
ETDRS (final) grade: 47a, 47b, 47c, 47d
Lesions: Both level 43 characteristics – H/Ma moderate in 4 to 5 fields or severe in 1 field and IRMA definite in 1 to 3 fields or any one of the following: IRMA in 4-5 fields, HMA severe in 2-3 fields, VB definite in one field
Risk of progression to PDR in 1 year (ETDRS interim): Level 45 = 20.7%
ETDRS screening or clinic follow up intervals: 4 months
English Screening Programme levels: English DES Programme referral criteria.
Scottish Grading Classification: R3 Background diabetic retinopathy (BDR) – referable. Any of the following features: 4 or more blot haemorrhages (in other words, AH standard photograph 2a – in both inferior and superior hemi-fields, venous beading standard photograph)
