Infectious disease surveillance and monitoring for animal and human health: summary July 2024
Updated 15 May 2025
1. Interpreting this report
The UK Health Security Agency’s (UKHSA) Emerging Infections and Zoonoses (EIZ) team uses an integrated horizon scanning approach, which combines information on both human and animal health, to identify and assess outbreaks and incidents of new and emerging infectious diseases globally. For further information about the EIZ team’s horizon scanning process, please see our Epidemic intelligence activities.
This summary provides an overview of incidents (new and updated) of public health significance, which are under close monitoring. The incidents are divided into 2 sections: Notable incidents of public health significance and Other incidents of interest. For each notable incident of public health significance, an incident assessment is provided, based on the EIZ team’s interpretation of the available information.
The report also includes a section that focuses on Novel pathogens and diseases and a final Publications of interest section, which contains new publications relevant to emerging infections.
Epidemiological updates for diseases classified as a high consequence infectious disease (HCID) are published in UKHSA’s HCID monthly summary, unless they are considered a notable incident of public health significance, in which case a more detailed summary will be provided in this report.
For more information, or to sign up to the distribution list to receive an email alert when new reports are published, please contact epiintel@ukhsa.gov.uk
2. Notable incidents of public health significance
2.1 Summary of incidents
| Disease or infection | Location | New or update since the last report |
|---|---|---|
| Mpox | African Region | New |
| Nipah virus infection | India | New |
| Oropouche fever | Brazil, Americas Region | Update |
2.2 Mpox - African Region
Event summary
Since the declaration of the nationwide mpox outbreak in the Democratic Republic of the Congo (DRC) on 16 December 2022 and up to July 2024, a continued increase in clade I mpox virus (MPXV) cases and increased geographical spread has been observed in the African Region.
In 2024, up to 28 July 2024, 13,791 cases of mpox (including 2,628 confirmed cases) and 450 deaths (case fatality rate (CFR) of 3.3%) have been reported in the DRC across 25 out of 26 provinces. This includes cases in vulnerable communities such as displacement camps in Goma, North Kivu. This is a 10% increase in the total case number compared to the equivalent period in 2023. Children aged under 15 years accounted for the majority of reported cases (68%) and deaths (85%). To date, only clades Ia and Ib MPXV has been reported in the DRC.
Countries which have previously reported clade I MPXV have also reported an increase in cases in 2024. As of 28 July 2024, clade Ia MPXV cases have been reported from the Republic of the Congo (146 cases and one death), and the Central African Republic with 213 cases (28 confirmed). On 25 July 2024, Burundi’s Ministry of Health reported 3 confirmed clade Ib MPXV cases in Bujumbura Mairie and Bujumbura Rural provinces. Since then and up to 31 July 2024, 22 cases (13 confirmed) have been reported in Burundi. Additionally, an unspecified number of clade Ib MPXV cases were also reported in Uganda during July 2024.
During July 2024, MPXV cases were also reported in Kenya and Rwanda for the first time. On 25 July 2024, 2 confirmed clade Ib MPXV cases were reported by the Rwandan Ministry of Health in individuals in Rwanda with travel history to the DRC. On 31 July 2024, the Kenyan Ministry of Health reported a confirmed clade Ib MPXV case on the Kenya-Tanzania border in an individual who had been travelling from Uganda to Rwanda.
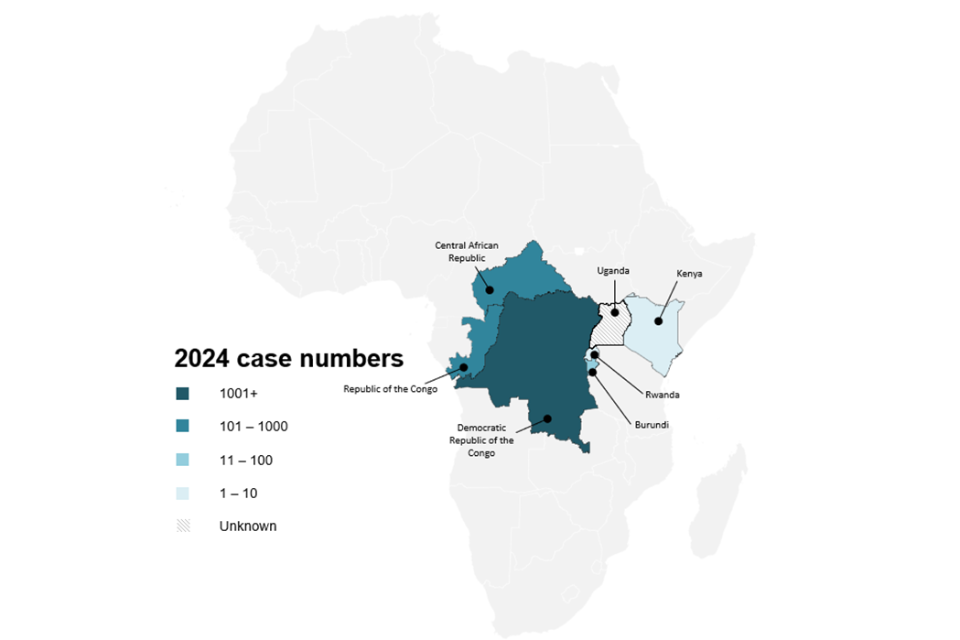
Figure 1. A map of clade I MPXV cases reported in 2024, as of 31 July 2024, in the African Region (see text above for data sources).
2.3 Incident assessment
The World Health Organization (WHO) has assessed the risk associated with mpox in the DRC to be high. This assessment is based on several factors. The majority of cases and deaths in endemic regions occur among children, resulting in a significant impact on this vulnerable group. Clade I MPXV is also being transmitted through sexual contact within populations such as sex workers in the mining industry. The spread of clade I MPXV to neighbouring countries of the DRC such as Rwanda, Kenya, Burundi, and Uganda with international travel connections, increases the risk of further geographical expansion.
The increase in newly detected cases as well as a high positivity rate may indicate underreported cases, and/or undetected transmission, particularly in the DRC. There are a lack of adequate resources to effectively respond to the outbreak in some areas, compounded by limited public awareness about the disease and its transmission. Insufficient information regarding animal reservoirs complicates understanding of transmission pathways and the implementation of responses.
As of 31 July 2024, there have been no cases of clade I MPXV reported in the UK, and this clade has not been implicated in the international clade II mpox outbreak in non-endemic countries that started in mid-2022. There are established processes for the isolation and contact management of high consequence infectious disease (HCID) cases in the UK, such as clade I mpox. There are a range of robust public health, clinical and infection prevention and control guidelines available for HCIDs in the UK.
2.4 Nipah virus infection - India
Event summary
On 21 July 2024, a fatal case of Nipah virus infection in a 14-year-old male was reported by India’s Ministry of Health and Family Welfare in Mallapuram, in the state of Kerala. The case developed acute encephalitis and was hospitalised, before being transferred in a critical condition to another hospital, where they died. The National Institute of Virology in Pune confirmed infection with Nipah virus. The fatal case had consumed fruit from their neighbourhood, which may have been contaminated by secretions from infected bats. Previous outbreaks in this area have been associated with the consumption of foods contaminated by bats secretions.
Public health teams and health care workers promptly established response measures to limit the outbreak’s spread, including active case finding in the local area, contact tracing with strict quarantine, and isolation of any suspected cases. A joint outbreak response team was deployed to assist with public health interventions, along with a mobile BSL-3 laboratory from the Indian Council of Medical Research. Malappuram District imposed community restrictions which included avoidance of public gatherings, social distancing, and the wearing of face masks in public and educational establishments. Restrictions on business operating hours was also implemented in two areas within the district. As of 24 July 2024, 472 people were listed as case contacts, of which 220 were considered high risk contacts. One contact from the list was hospitalised with mild symptoms, though these were not described in detail.
The last outbreak of Nipah virus in India was also in Kerala, in Kozhikode district in September 2023. This resulted in 6 confirmed cases and 2 deaths.
2.5 Incident assessment
Nipah virus infection is a zoonotic viral disease caused by Nipah virus, which circulates in fruit bats of the Pteropus genus. Humans can be infected through exposure to infected animals such as bats and pigs, via food contaminated by infected animals’ saliva, urine or excreta, or via human-to-human transmission.
The first outbreak of Nipah virus in India occurred in 2001 in West Bengal. Since then, 6 outbreaks have happened in the country, with outbreaks in 2018, 2019, 2021 and 2023 occurring in Kerala state on the south-western coast of India, where this most recent case was also reported.
To date, there have been no reported cases of Nipah virus in the UK. While severe disease in a case is possible, transmission within the wider UK population is highly unlikely as there are established processes for the isolation and contact management of high consequence infectious diseases (HCID) cases. There are a range of robust public health, clinical, infection prevention and control measures available for HCIDs, which can be adapted for use as necessary.
2.6 Oropouche fever - Brazil, Americas Region
Event summary
In 2024, the geographical spread of Oropouche fever has been observed across the Region of the Americas. During the past 10 years, Oropouche virus (OROV) has primarily been identified in the Amazon basin, however in 2024 detections have expanded within Brazil to non-Amazonian states and outside of Brazil, to Bolivia and Cuba. As of 30 July 2024, 8,078 confirmed cases of OROV have been reported in 5 countries across the Region of the Americas. Most cases have been reported in Brazil (7,284 cases), followed by Bolivia (356 cases), Peru (290 cases), Cuba (74 cases) and Colombia (74 cases). To compare, in 2023, Brazil reported 773 confirmed cases of OROV, while Peru reported 94 cases between 2016 and 2022.
On 25 July 2024, the Brazilian Ministry of Health confirmed the first fatal cases of OROV. The first fatal case was a 24 year old female from Bahia State who experienced symptom onset on 23 March 2024. The case reported symptoms of headache, fever, and vomiting, which later worsened resulting in death on 27 March 2024 following cardiorespiratory arrest. The second fatal case was a 21 year old female also from Bahia, with symptom onset on 5 June 2024. The case reported symptoms of bleeding and rashes and was hospitalised and later died on 9 June 2024. Both cases tested positive for OROV, and both cases reported no co-morbidities. These deaths represent the first fatal cases of OROV globally. As of 30 July 2024, 2 additional fatal cases were under investigation in Brazil. Additional details regarding the first 2 fatal cases of OROV have been reported in a recently published pre-print.
In addition to these fatal cases, the Brazilian Ministry of Health also reported the first potential cases of vertical transmission of OROV. As of 30 July 2024, 5 suspected cases have been reported among pregnant women in Brazil resulting in 4 cases of still birth and one case of spontaneous abortion. Additionally, 4 cases of microcephaly have been recorded amongst newborns.
2.7 Incident assessment
Oropouche fever is caused by OROV, which is known to circulate in the Caribbean and Central and South America. OROV is primarily transmitted to humans from the Culicoides paraensis midge but can also be transmitted by the Culex quinquefasciatus mosquito. Other than humans, vertebrate hosts include non-human primates, sloths and birds. Due to its mild, often self-limiting manifestation and similarity in clinical presentation to other arboviral infections circulating in the Americas Region (for example dengue, chikungunya and yellow fever), there is likely an underestimation of the true burden of OROV disease due to low case detection and/or misdiagnosis. There are currently no specific antiviral treatments or vaccines against OROV. Further details regarding the geographical spread of OROV can be found here.
Due to the recent fatal cases of OROV in Brazil, suspected cases of vertical transmission, and the geographical spread of OROV, the Pan American Health Organization (PAHO) have assessed the overall risk of OROV in the Region of the Americas as high.
In 2024, imported cases of OROV have been reported in the European Region for the first time. Between June and July 2024, 19 imported cases were reported from Spain (12 cases), Italy (5 cases), and Germany (2 cases) amongst individuals with travel history to Cuba (18 cases) and Brazil (one case). The European Centre for Disease Prevention and Control (ECDC) assess the risk of OROV infections amongst European Union and the European Economic Area travellers to OROV-epidemic countries in the Region of the Americas as moderate, while the risk of locally-acquired OROV in the EU/EEA is assessed as low. In the UK, whilst travel associated infections are possible in returnees to the UK from OROV affected areas, further transmission in the UK is unlikely due to the absence of established competent vectors required for OROV transmission. As of July 2024, the UK has not reported any cases of OROV infection.
2.8 Summary of other incidents
| Disease or infection | Location |
|---|---|
| Avian influenza A(H5) | United States |
| Chandipura virus | India |
| Cholera | African Region, Myanmar |
| Dengue | multi-country |
| Polio | multi-country |
| West Nile virus | Spain |
2.9 Avian influenza A(H5)
During July 2024, confirmed human cases of avian influenza A(H5) were reported in Colorado State, the United States (US) for the first time. The first case was reported on 3 July 2024 in a dairy worker who had been exposed to avian influenza A(H5N1) infected cattle while working on a dairy farm. The case developed symptoms of conjunctivitis and was treated with oseltamivir. Since then and as of 30 July 2024, 10 confirmed human cases of avian influenza A(H5) have been reported amongst dairy cattle and poultry workers across Colorado State. These cases bring the total number of human cases of avian influenza A(H5) reported across the US to 13 since April 2024, with cases reported from Colorado, Michigan (two cases), and Texas (one case) states. The US Centers for Disease Control and Prevention (CDC) continue to assess the current risk of avian influenza A(H5N1) to the general public as low.
Since the first detections of avian influenza A(H5N1) amongst in dairy cattle farms in Texas and Kansas during March 2024, the US Department of Agriculture (USDA) have reported 178 detections in livestock across 13 states in the US, up to 31 July 2024. Most cases have been reported in Colorado (n=52), Idaho (n=30), and Michigan (n=27).
2.10 Chandipura virus
In June 2024, India’s Ministry of Health and Family Welfare reported an increase in cases of acute encephalitis syndrome (AES) predominantly amongst children aged under 15 years old in Gujarat, India. As of 31 July 2024, 148 cases of AES and 59 deaths have been reported, of which 51 cases were confirmed positive for Chandipura virus (CHPV). Most cases have been reported in Gujarat (140 cases), followed by Madhya Pradesh (4 cases), Rajasthan (3 cases), and Maharashtra (one case). The number of new cases has declined since 19 July 2024 following the implementation of various public health measures. Sporadic cases of CHPV are reported in western, central, and southern India, particularly during the monsoon season. CHPV is presumed to be transmitted by sand fly and tick vectors.
2.11 Cholera
Between 1 January and 26 July 2024, 128,374 cholera cases (including 24,226 confirmed cases) and 1,943 deaths were reported across 16 African Union member states, according to the Africa Centres for Disease Control and Prevention (Africa CDC). Most cases have been reported in the DRC (21,764 cases and 307 deaths), Ethiopia (21,287 cases and 182 deaths), and Zambia (20,063 cases and 612 deaths). To compare, during 2023, a cumulative total of 241,317 cholera cases (including 93,475 confirmed cases) and 3,827 deaths (CFR of 1.6%) were reported across 19 African Union member states.
On 25 June 2024 an outbreak of acute watery diarrhoea was reported in the Yangon Region of Myanmar. The presence of cholera was later confirmed by the Ministry of Health. As of 22 July 2024, a total of 1,141 hospitalised cases of acute watery diarrhoea, 139 cases with severe diarrhoea and one death have been reported across townships in the Yangon Region. Prior to this, Myanmar last reported a high number of cholera cases in 2016 (782 cases).
2.12 Dengue
Between 1 January and 26 July 2024, the Africa CDC reported 50,370 dengue cases (10,535 confirmed cases) and 63 deaths across 12 African Union Member States. Most cases have been reported in Burkina Faso (30,865 cases, 47 deaths), Mauritius (9,166 cases, 8 deaths), and Mali (5,283 cases, 6 deaths). In 2023, 280,218 dengue cases and 808 deaths were reported in 18 African Union Member States, with Burkina Faso reporting the highest numbers (242,425 cases and 709 deaths). Data should be interpreted with caution due to differences in case definitions, laboratory capacities and reporting capabilities across African Region countries. The reported burden of disease within these countries is likely an underestimation.
In the Region of the Americas, the WHO has reported 10,893,547 suspected dengue cases and 5,940 deaths between 1 January and 13 July 2024. This is a 233% increase in cases compared to the same period in 2023, and a 418% increase compared to the average of the last 5 years. Most cases reported during week 28 of 2024 were reported in Brazil (35,193 cases), Mexico (10,299 cases) and Colombia (7,487 cases). All 4 serotypes are currently circulating in the Region of the Americas.
On 8 July 2024, Occitania’s Regional Health Agency reported its first locally acquired case of dengue in France and Europe for the 2024 season. The case was detected in the Herault department of Occitania region. During 2023, 45 locally acquired dengue cases were reported in France, including Herault department (3 cases). Vector control measures have been implemented in Montpellier and Perols, areas which had been frequented by the case.
According to media on 17 July 2024, Guatemala’s Ministry of Public Health and Social Assistance declared a National Health Emergency due to an early increase in dengue cases across Guatemala. The transmission of dengue in Guatemala usually peaks between May and December. As of 25 July 2024, 53,489 dengue cases have been reported in Guatemala. To compare, during 5,594 cases had been reported during the equivalent period in 2023.
On 14 June 2024, the Ministry of Health and Medical Education of Iran reported their first two cases of local transmission of dengue in Bandar-Lengheh City, Hormozgan Province, Iran. The establishment of the dengue vectors, Aedes aegypti and Aedes albopictus, in the province has resulted in further locally acquired cases. As of 17 July 2024, 12 locally acquired dengue cases were reported in Bandar-Lengheh City. Prior to this, Iran had only reported travel-associated dengue cases, with an average of 20 cases recorded annually. A notable increase in the number of travel-associated dengue cases in Iran has also been reported, with 137 cases reported in 2024, up to 10 July. The WHO have assessed the national risk of dengue for Iran as high due to the established presence of the vector and the movement of people from endemic countries and countries experiencing ongoing outbreaks, to Iran.
In 2024, up to 27 July, a cumulative total of 128,834 dengue cases and 337 deaths were reported in the Philippines. This is a 33% increase in cases compared to the equivalent period in 2023 (97,211 cases). The number of new cases continues to increase, particularly in the Western Visayas, Central Visayas, Cagayan Valley, and Calabarzon regions.
2.13 Polio
Wild poliovirus type 1 (WPV1)
From 1 January 2024 to 30 July 2024, the Global Polio Eradication Initiative (GPEI) reported 9 cases of WPV1 in Pakistan and 9 cases of WPV1 in Afghanistan. In 2023, 6 cases of WPV1 were reported from Pakistan and 6 cases were reported from Afghanistan.
On 29 July 2024, media reported that Gaza’s health ministry declared a polio epidemic. This follows 6 environmental detections of circulating variant poliovirus type 2 in sewage. Scarce supplies of drinking water in the densely populated Gaza Strip increase the risk of contamination by the virus.
Circulating vaccine derived polio virus (cVDPV)
During July 2024, the GPEI reported one case of cVDPV1 in the DRC and one case in Mozambique (this is the first case reported in Mozambique for 2024). In 2023, 134 cases were reported across 3 countries: the DRC (106 cases), Madagascar (24 cases), Mozambique (4 cases).
During July 2024, the GPEI reported cases of cVDPV2 from:
- Angola (2 cases)
- Benin (one case)
- Guinea (2 cases)
- Indonesia (4 cases)
- Niger (one case)
- Chad (one case)
- DRC (3 cases)
- Yemen (17 cases)
- Nigeria (one case)
- Ethiopia (5 cases)
- Somalia (one case)
A total of 395 cases were reported across 22 countries in 2023, with most cases reported from:
- the DRC (118 cases)
- Nigeria (87 cases)
- Guinea (47 cases)
2.14 West Nile virus
In July 2024, an increase in WNV cases was observed in Israel. As of 30 July 2024, the Israel Ministry of Health had reported 738 confirmed cases and 51 associated deaths. Cases are distributed throughout the country, with the majority of cases occurring in the north of the country, specifically Tel Aviv District. West Nile virus has been reported in Israel since the 1940s with peak transmission occurring in late summer and early autumn. This is the largest outbreak of WNV in Israel since 2000, when 425 cases were reported. Between 2001 and 2023, less than 150 cases were reported annually. It has been suggested that the large increase in case numbers earlier in the season may be due to the effects of climate change expanding the insect vector’s geographic range (June 2024 was the hottest June on record for Israel). Additionally, disruptions caused by conflict, such as that in Gaza, may impact vector control, waste management, and levels of standing water, conditions which are known to promote mosquito proliferation. A recent study has been published detailing the recent cases of WNV in Israel.
In 2024, and as of 31 July 2024, Europe has also experienced 69 locally acquired human WNV cases, with 8 countries in Europe reporting human cases:
- Austria
- France
- Greece
- Hungary
- Italy
- Romania
- Serbia
- Spain
8 deaths were reported, from Greece, Italy and Spain. A higher case fatality rate (13%) has been observed in 2024 compared to the previous decade (11%), though European case numbers for July 2024 are below the average seen for July in the years between 2014 and 2023. However, the number of reported cases in Spain and Greece exceeds the average for July in previous years.
3. Publications of interest
3.1 Chikungunya
On 28 June 2024, the European Union approved the registration of the Valneva Chikungunya vaccine, IXCHIQ, for use in individuals aged over 18 years. This is the first Chikungunya vaccine to be approved for use in Europe. Chikungunya is not endemic in Europe, and the majority of cases in the region are in travellers returning from regions of endemicity in the tropics and subtropics. However, there have been sporadic incidents of onward transmission by infected travellers after their return, mainly in Southern Europe where the Aedes albopictus mosquito is established. Spread of this vector due to climate change could lead to cases of Chikungunya in these currently non-endemic regions.
4. Further reading
4.1 Avian influenza A(H5N1)
4.2 Lyssavirus
Toward the Development of a Pan-Lyssavirus Vaccine
4.3 Poliovirus
4.4 Rift Valley fever
4.5 Severe fever with thrombocytopenia syndrome virus
4.6 Usutu virus
Ixodes ricinus as potential vector for Usutu virus
5. Related resources
1. High consequence infectious diseases monthly summaries
2. National flu and COVID-19 surveillance reports
3. Avian influenza (influenza A H5N1): technical briefings
4. Avian influenza (bird flu) in Europe, Russia and the UK reports
5. Bird flu (avian influenza): latest situation in England updates
6. Human Animal Infections and Risk Surveillance (HAIRS) group risk assessments and statements
7. Animal and Plant Health Agency (APHA) monitoring of disease in livestock and poultry monthly reports
6. Authors of this report
UKHSA’s Emerging Infections and Zoonoses team epiintel@ukhsa.gov.uk
