Abdominal wall defects: gastroschisis information for parents
Updated 3 February 2025
Applies to England
1. Overview
This information will help you if your baby is suspected of having gastroschisis (often pronounced ‘ga-stros-ki-sis’) following your 20-week scan (sometimes referred to as the mid-pregnancy scan).
We hope it helps you and your health professionals to talk through the next stages of your and your baby’s care. This information should support, but not replace, discussions you have with health professionals. Finding out there may be a problem with your baby’s development can be worrying. It is important to remember you are not alone.
We will refer you to a specialist team who will do their best to:
- provide more accurate information about your baby’s condition and treatment
- answer your questions
- help you plan the next steps
2. About gastroschisis
Gastroschisis is an abdominal wall (tummy wall) defect. It happens when a baby’s abdominal wall does not develop fully while in the womb.
Early in all pregnancies, the baby’s intestine develops inside the umbilical cord. It usually moves inside the abdomen a few weeks later.
In gastroschisis, the baby’s ‘belly button’ does not develop properly, meaning that the intestines develop outside the body and are open to the air when the baby is born.
The baby’s intestines outside the abdomen float in the amniotic fluid, which can cause irritation and make them swollen and thick.
2.1 Causes
We do not know exactly what causes gastroschisis, but we do know it is becoming more common, especially in mothers under the age of 20.
Gastroschisis happens in about 5 babies out of every 10,000 (0.05%).
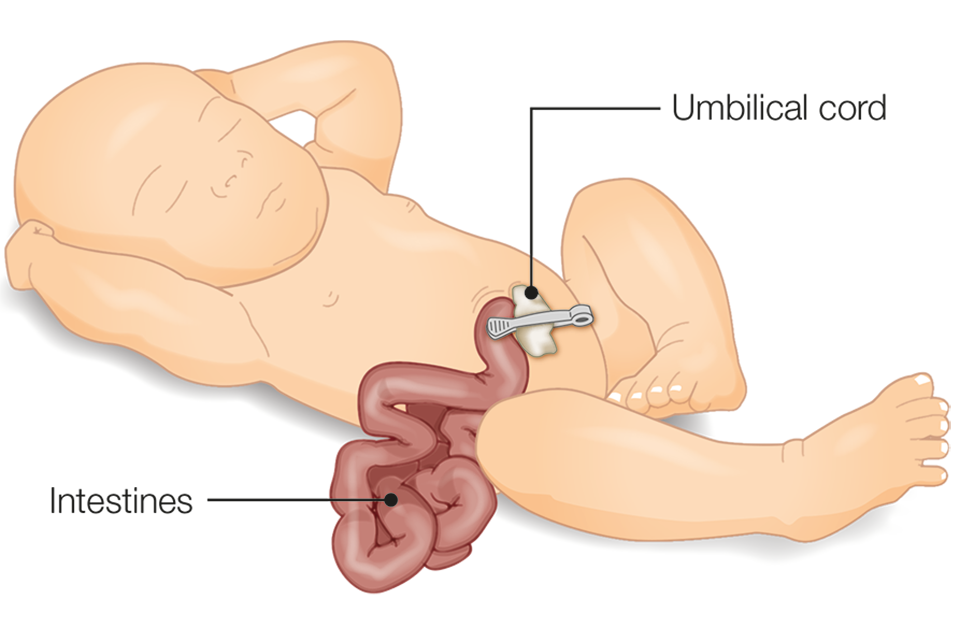
Illustration of a baby with gastroschisis showing intestine developed outside the body
3. How we find gastroschisis
We screen for gastroschisis at the 20-week scan (between 18+0 and 20+6 weeks of pregnancy). Sometimes we notice it during an earlier scan at around 12 weeks of pregnancy.
4. Follow-up tests and appointments
As the result of the scan suggests your baby has gastroshisis, we are referring you to a team of experts in caring for pregnant mothers and their babies before they are born. They may be based at the hospital where you are currently receiving antenatal care, or in a different hospital. You will need a second scan to find out for sure if your baby has the condition. The specialist team will be able to confirm if your baby has gastroschisis, and what this might mean.
It may be useful to write down any questions you want to ask before you see the specialist team.
If your baby has gastroschisis, the specialist team will offer you extra ultrasound scans to monitor your baby. They may also offer you more detailed monitoring of your baby’s well-being before they are born.
Mothers of babies with gastroschisis usually have a normal birth, but the specialist team may discuss a caesarean section with you if the gastroschisis is very large.
5. Treatment
The team looking after you and your baby will involve specialists such as neonatologists and paediatric surgeons, who will care for your baby. They will talk to you about the condition, possible complications, treatment and how you can prepare for the birth of your baby.
Babies with gastroschisis need an operation after they are born.
Most cases of gastroschisis are classed as ‘simple’, which means that the treatment and recovery tend to be quite straightforward.
In some cases, the gastroschisis is classed as ‘complex’, and there is often a blockage in the baby’s bowel. This means treatment and recovery can be more complicated. The team looking after you will discuss this with you in detail.
Most babies with gastroschisis:
- cannot feed in the same way babies usually feed after birth
- will need to be fed using a special tube to begin with
If you wish to breast-feed, you can store expressed milk to give to your baby when they are ready to feed.
Gastroschisis is often linked with the baby being small. It is usual to plan induction of labour between 36 and 40 weeks of pregnancy. Sometimes, babies may need to be born before 36 weeks.
The length of time your baby needs to spend in hospital depends on the baby, and varies from weeks to months. This depends on things like the kind of operation your baby needs, the recovery time, if there are any complications and how your baby is feeding. The specialist team will be able to give you more information depending on your individual circumstances.
6. Longer term health
Some babies with ‘complex’ gastroschisis will have more serious health problems. The possible outlook for you and your baby will depend on your individual circumstances.
Most babies can go home when they have recovered from their operation and are feeding on their own. A small number of babies still have difficulty feeding or absorbing food after 4 weeks. This is not usually a serious problem, and it usually sorts itself out in time.
The specialist team looking after your baby will do their best to:
- answer your questions
- help you plan the next steps
About 9 in 10 (90%) babies born with gastroschisis make a full recovery. There is an increased chance that they are born early and are smaller than other babies.
7. Next steps and choices
You can talk to the team caring for you during your pregnancy about your baby’s gastroschisis and your options. These will include continuing with your pregnancy or ending your pregnancy. You might want to learn more about gastroschisis. It can be helpful to speak to a support organisation with experience of helping parents in this situation.
If you decide to continue your pregnancy, the specialist team will help you:
- plan your care and the birth of your baby
- prepare to take your baby home
If you decide to end your pregnancy, you will be given information about what this involves and how you will be supported. You should be offered a choice of where and how to end your pregnancy and be given support that is individual to you and your family.
Only you know what the best decision for you and your family is. Whatever decision you make, your healthcare professionals will support you.
8. Future pregnancies
If you decide to have another baby, they are unlikely to have gastroschisis.
9. More information
Antenatal Results and Choices (ARC) is a national charity that supports people making decisions about screening and diagnosis, and whether or not to continue a pregnancy.
Gastroschisis Exomphalos Extrophies Parental Support Group (GEEPS) is a support group run by parents for parents. It is based in the UK, but welcomes parents from anywhere in the world.
Find out how NHS England uses and protects your screening information.
Find out how to opt out of screening.
