Health matters: Prevention - a life course approach
Published 23 May 2019
Summary
This resource for NHS and public health professionals focuses on taking a life course approach to the prevention of ill health and explores the evidence base for this approach. The resource signposts to evidence-based interventions and tools, as well as to evaluation and monitoring techniques.
A life course approach
A person’s physical and mental health and wellbeing are influenced throughout life by the wider determinants of health. These are a diverse range of social, economic and environmental factors, alongside behavioural risk factors which often cluster in the population, reflecting real lives. All these factors can be categorised as protective factors or risk factors.
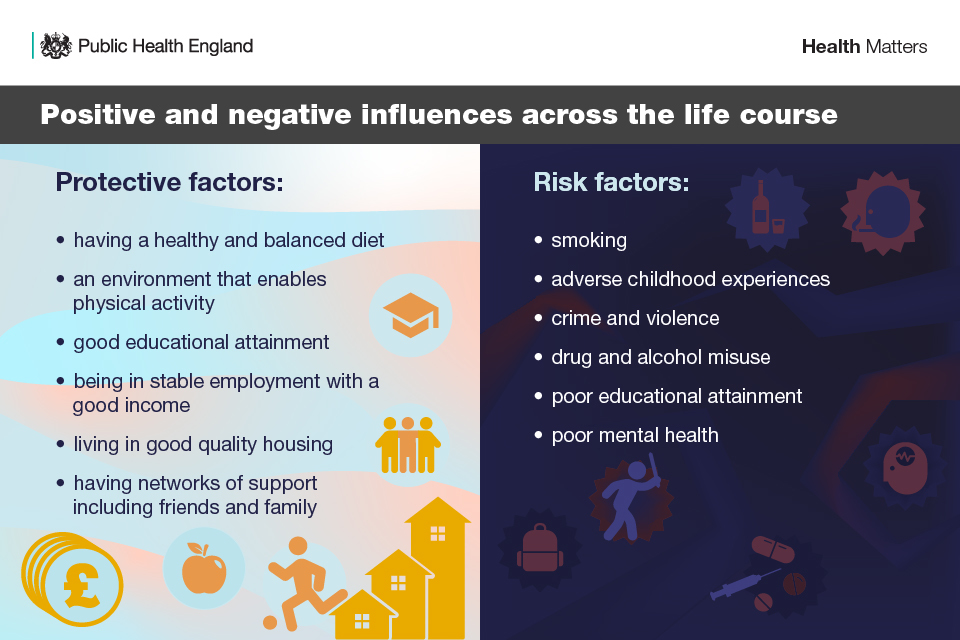
Infographic listing positive and negative influences across the lifecourse
Addressing the wider determinants of health will help improve overall health by helping to improve the conditions into which people are born, live and work.
Unlike a disease-oriented approach, which focuses on interventions for a single condition often at a single life stage, a life course approach considers the critical stages, transitions, and settings where large differences can be made in promoting or restoring health and wellbeing.
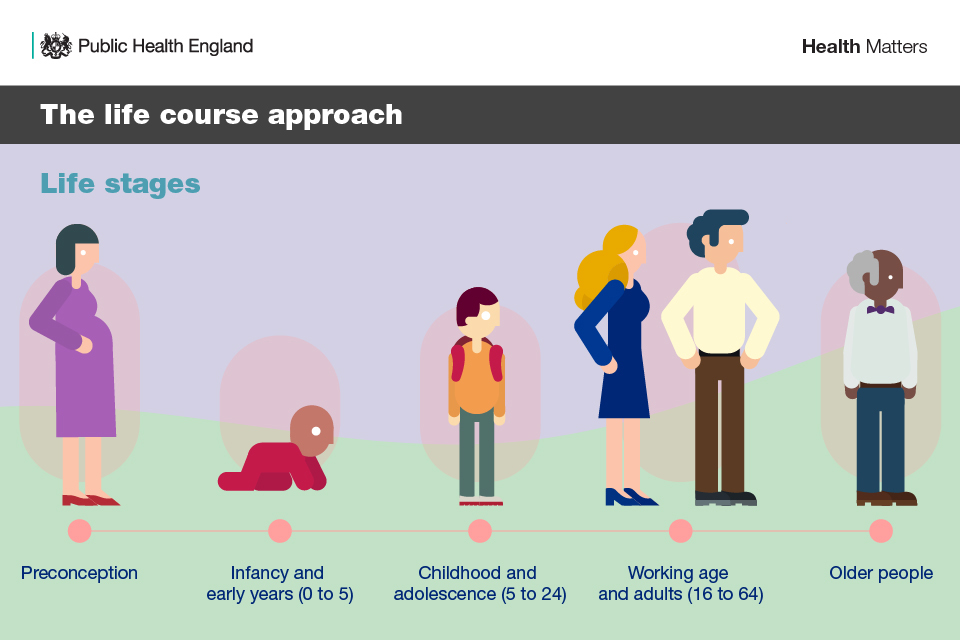
Infographic showing the life stages of the life course: preconception; early years; childhood and adolescence;working age; older people;
A life course approach values the health and wellbeing of both current and future generations. It recognises that:
- there are a wide range of protective and risk factors that interplay in health and wellbeing over the life span
- maintaining good functional ability is the main outcome of the life course approach to health
- functional ability can be enhanced throughout life by a supportive environment
- by altering policies, environments, and societal norms, inequalities affecting the life course trajectory can be reduced, which could benefit the whole population across the lifespan, as well as future generations
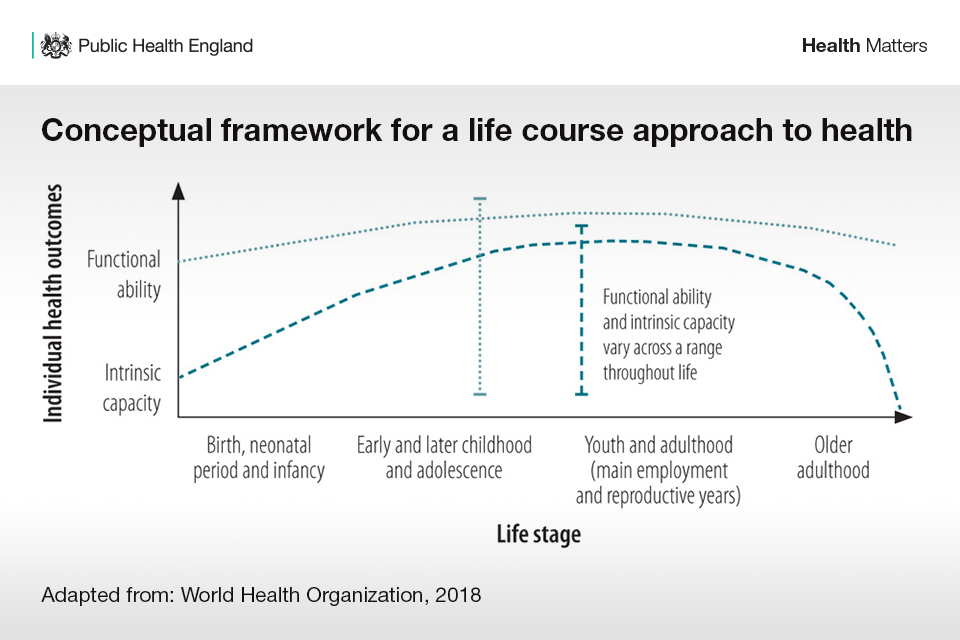
Graph showing conceptual framework for a life course approach. Illustrates how functional ability and intrinsic capacity vary overt he stages of life
The conceptual framework of the life course has been defined by the World Health Organization (WHO). In the chart above, ‘functional ability’ and ‘intrinsic capacity’ are shown diagrammatically as idealised curves across the life course.
Intrinsic capacity refers to the internal attributes that we are born with, such as our physical and mental health. These can be boosted by supportive environmental and social factors throughout our lives, therefore contributing to our functional ability. These could include glasses to correct poor vision, dropped pavements to enable easy access for pushchair and wheelchair users or availability of affordable healthy food.
If our attributes are still developing (as in the case of children) or reduced (as in the case of poor health or disability), then the environment takes on an even more critical role in maintaining or improving functional ability, enabling people to be or do what they have reason to value.
There are also supportive environmental factors that can enhance functional ability throughout life. For example, a young child’s functional ability can be demonstrated by the ability to play well. In older age, environmental factors such as safe streets and appropriate housing can impact positively on mobility which, in turn, supports functional ability.
Adopting the life course approach means identifying opportunities for minimising risk factors and enhancing protective factors through evidence-based interventions at important life stages, from the perinatal period through early childhood to adolescence, working age, pre-conception and the family-building years, and into older age. It also capitalises on the potential to deliver an inter-generational approach to health improvement and reduce health inequalities from generation to generation and improve conditions of daily life.
It is important that these interventions fit the life course framework. This means taking action:
- early and appropriately across the life course to protect and promote health during important transition periods
- together as a society to create healthy environments and improve conditions of daily life
- to reduce health inequalities throughout the life course
WHO states that ensuring that the life course perspective is integrated more fully into our work will help us identify appropriate settings for health promotion, design more effective interventions proportionate to need, and ultimately, save lives.
Health inequalities in the life course approach
Systematic variation in the protective and risk factors that make up the wider determinants of health are social inequalities. These are strong and persistent drivers of health inequalities, leading to differing trajectories and outcomes over the course of a person’s life, and influencing life expectancy and healthy life expectancy. Some people are impacted more by the negative influences on health, leading to shorter life expectancy and more years living with disability.
In England, the gap in life expectancy at birth between the least and most deprived areas was 9.4 years for males and 7.4 years for females in 2015 to 2017. For healthy life expectancy (years lived in good health) it was 19.1 years and 18.8 years respectively.
The least deprived men and women at 65 years of age could expect to live 5.2 and 4.8 years longer respectively than their most deprived counterparts in 2015 to 2017.
Looking through the life course lens enables action on social determinants of health, both to address negative risk factors and build empowered and resilient individuals and communities.
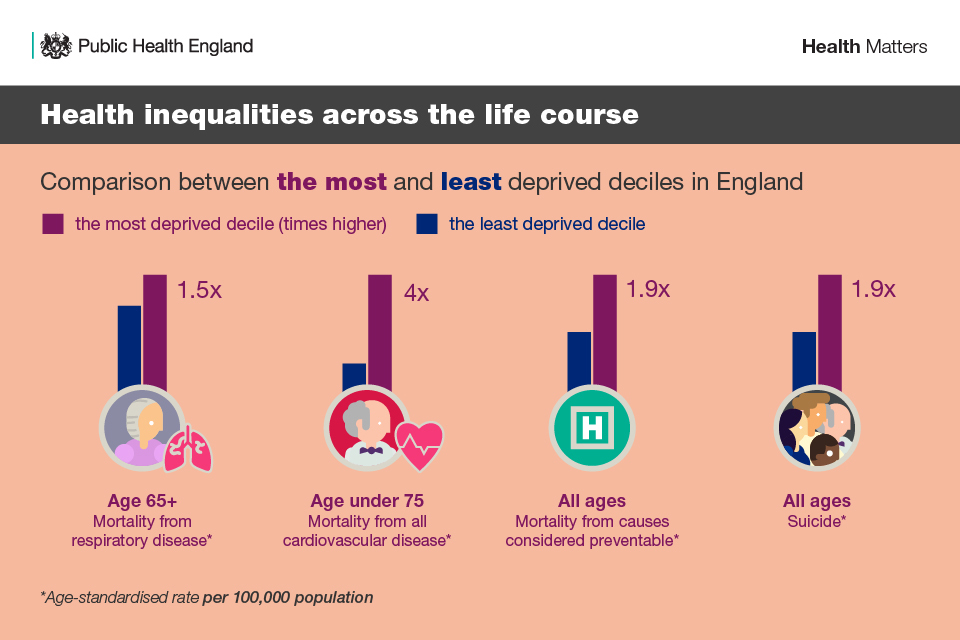
Infographic showing inequalities across the lifecourse between the most and least deprived deciles in England
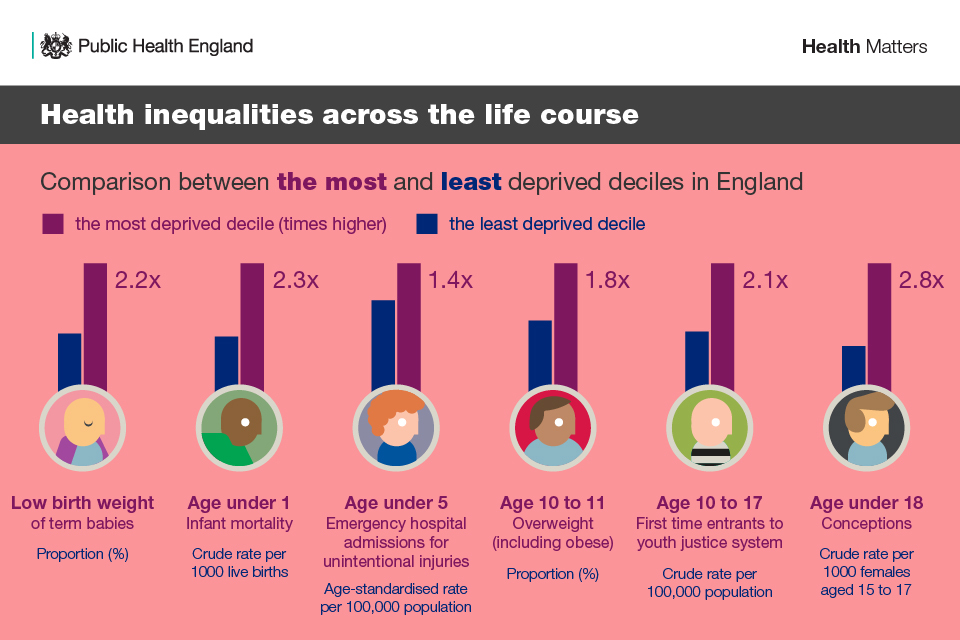
Infographics showing health inequalities at different life stages of the life course
Reducing health inequalities through the life course requires a whole-of-society approach dealing comprehensively with all health determinants, such as Health in All Policies. This approach recognises the importance of action needed at every stage of life, including at working and older ages, to improve equity within and between generations.
PHE and partners’ Health Equity Collection comprises comprehensive evidence, resources and guidance to help support national, regional and local areas to reduce health inequalities. PHE is developing resources and tools to support place-based approaches to tackle health inequalities (forthcoming summer 2019).
Investing in the life course approach
Long-term investment in a life course approach can limit ill health and the accumulation of risk throughout life. Therefore, it can provide high returns for health and contribute to social and economic development.
To put into practice the life course approach to health, a more holistic approach to investment is required. This will, in turn, allow more focus on preventing health risks and reducing their cumulative effect throughout life and across generations, and mitigate the economic burden of health care costs.
1. Childhood and adolescence
Investment in early childhood, child and adolescent health and development, and preconception, pregnancy and childbirth care can yield a 10-to-1 benefit to cost ratio in health, social and economic benefits. It can also reduce rates of mental health disorders and noncommunicable diseases in later life.
2. Working age adults
PHE’s movement into employment tool shows that among adults, entry or re-entry to sustainable employment leads to financial outcomes per person, as follows:
- financial benefits to the individual(s): £3,530
- financial benefit to society: £23,070
- financial benefits to the exchequer: £12,030 (of which to central government: £11,410, to local authority: £535 and to NHS: £85)
3. Older people
Older people contribute significantly to the economy through work: by providing care to younger generations, therefore enabling younger family members to pursue their careers; caring for older family members who need support; and by volunteering (estimated at £6 billion by Age UK).
However, the opportunities available to each of us as we age will be dependent on our health. As such, investing in the health of people from earlier on in the life span is important, as it will help them to stay well in older age and continue contributing to the UK economy.
PHE health economics tools: Health Economics Evidence Resource updated 2019 Health economics: a guide for public health teams 2018 (includes extensive range of return on Investment (ROI) tools.)
The life course approach and local action
To achieve the desired outcomes of the life course approach, national policies should be translated into local actions. At the same time, these local actions can be seen as examples of innovation for how national policy might develop.
With local government services facing increasing demand and a challenging financial situation, it is important to note that the life course approach does not demand new or extra actions that incur additional costs. Rather, it is based on the current responsibilities and working practices of local authorities, and public health responsibilities.
Local authorities are already taking practical action on prevention across the life span, for example, in:
- early years work
- productive healthy ageing
- healthy places
- improved incomes for the low-waged
- good quality work opportunities
Some local authority-led integrated health and wellbeing services (IHWS) are now attempting to address multiple risk factors in a more comprehensive way, delivering coordinated support for different risk factor-related behaviours, targeting more deprived communities, and reflecting the real-life context of people’s lives.
The ongoing challenge is to break the generational cycle of disadvantage that drives health inequalities. Taking a life course approach reinforces local authority efforts to tackle this challenge.
Alongside local government, the NHS also plays a vital role in the life course approach, particularly through service provision and their role in prevention. The NHS Long Term Plan sets out NHS England’s commitment to stronger action on prevention and health inequalities, which is important for improving the health and health equity of both current and future generations.
Watch the stakeholder video discussion
Interventions across the life course
This section covers several recommended interventions across the life course selected by PHE for local government, the NHS and commissioners. It is not intended to highlight all the available interventions. An expanded interventions table is available to download.
Preconception and becoming a parent
The preconception period and pregnancy, which occur during the reproductive years, are important times during the life course. They can affect the next generation, as reflected in intrinsic capacity at birth.
What happens during pregnancy and the first few years of life influences physical, cognitive and emotional development in childhood and may influence health and wellbeing outcomes in later life. In addition to the critical events that shape an individual’s health trajectory, the number and sequence of exposures to risk and periods of increased susceptibility, some of which occur before birth or are genetically inherited, are also crucial.
Primary interventions
The preconception period presents an opportunity for health professionals to encourage women and men to adopt healthier behaviours in preparation for a successful pregnancy and positive health outcomes for both themselves and their child. This includes:
- being aware of screening before or during pregnancy
- being up to date with all vaccinations before and during pregnancy
- taking folic acid supplements
- eating a healthy diet
- being physically active
- giving up smoking
- reducing alcohol consumption
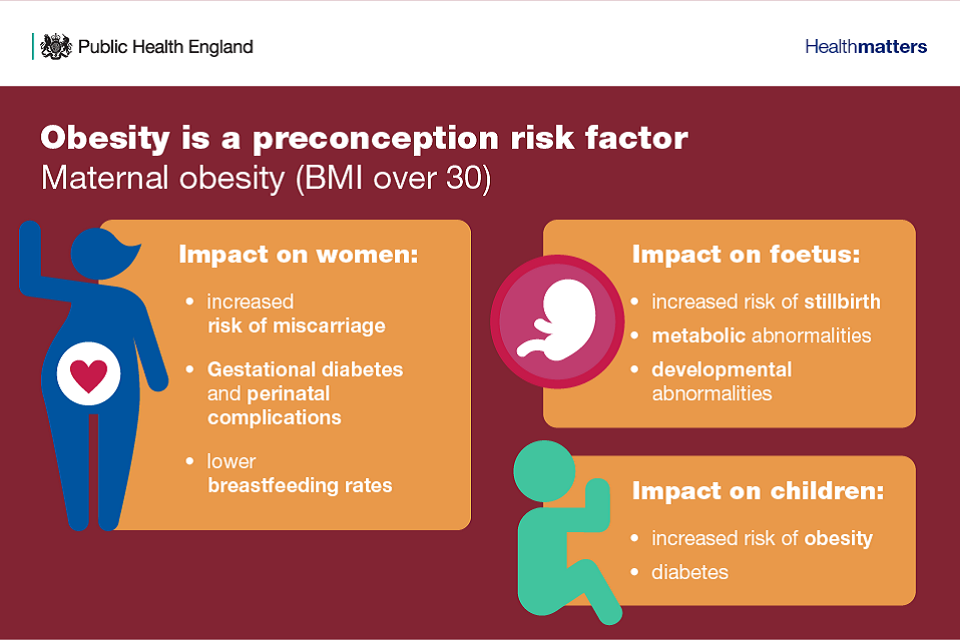
Infographic showing that maternal obesity is a risk factor with impacts on women, foetus and child
Read more in the Health Matters edition on reproductive health and pregnancy planning and the PHE Making the Case for preconception care resource.
Establishing vaccination status pre-pregnancy, such as MMR, and assessment of genetic conditions including sickle cell and thalassaemia, afford valuable protection to the woman, her unborn child and wider family. It also supports reproductive choices and early intervention to optimise health.
Antenatal screening provides an opportunity to detect conditions in the mother or baby as early as possible, which enables women and their partners to make personal informed decisions about their own health and their pregnancy. Some of the antenatal screening tests, such as blood tests for infectious diseases, eye screening for diabetes and the newborn hearing, infant physical examination and blood spot screening, are recommended as timely interventions can significantly impact on vertical transmission and neonatal morbidity and mortality.
Vaccinations in pregnancy help protect in 3 ways: firstly, they prevent illness and death in the pregnant women themselves, secondly, they reduce the risk of pregnancy loss, and thirdly, they help protect the newborn for the first few months of life.
Find out more about the NHS population screening programmes for newborns.
Infancy and early years (0 to 5)
The earliest years of life set the tone for the whole of the lifespan, according to the Marmot Review.
There is growing evidence that intervening in the first 1,000 days of a child’s life can make a difference over their whole lifetime. During this period the brain displays a remarkable capacity to absorb information and adapt to its surroundings.
Positive early experience is therefore vital to ensure children are ready to learn, ready for school and have good life chances. It is shaped by several factors such as:
- sensitive attuned parenting
- effects of socio-economic status
- the impact of high-quality early education and care
Improving children and young peoples’ mental wellbeing will have a positive effect on their cognitive development, learning, physical health, and their mental health, social and economic prospects in adulthood. It is known that poor social and emotional well-being in young children can lead to behaviour and developmental problems and, later in childhood, severe depression, anxiety, self-harm and other poor mental health outcomes.

Infographic about giving every child the best start in life: secure and reliable relationship, emotional wellbeing, brain and language development, capacity to form relationships with others
Primary interventions
Speech, language and communication skills
Early language impacts on many areas of child development; it contributes to children’s ability to:
- manage emotions and communicate feelings
- establish and maintain relationships
- think symbolically
- learn to read and write
Almost all children learn to communicate through language, yet there are strong and persistent differences in their ability to do so, with a pronounced social gradient in early language acquisition. The link between language and other social, emotional and learning outcomes makes early language a primary indicator of child wellbeing.
Speech and language development data forms part of school readiness evaluation.
Read the case study: Stoke Speaks Out: supporting speech, language and communication
Better development at this early age improves a child’s ability to make the most of his or her learning opportunities, achieving higher grades and better employment prospects. These are then associated with economic prosperity and better health outcomes in the longer term. (Health Profile for England 2018).
The Healthy Child Programme is at the heart of public health services for children and families. It brings together the evidence on delivering good health, wellbeing and resilience for every child through to the age of 5. This is delivered as a universal service with additional services for families needing extra support, whether short-term intervention or ongoing help for complex longer-term problems.
Early intervention programmes
Early intervention programmes and strategies are designed to prevent poor outcomes later in life; they may be implemented at any time from conception to the onset of adulthood.
PHE has set out the evidence on 2 areas of early intervention in childhood:
- increasing access to parenting programmes
- easing children’s transition between home and school, with a particular focus on interventions to reduce inequalities in health
Vaccination
After clean water, vaccination is the most effective public health intervention in the world for saving lives and promoting good health. The UK has one of the best immunisation programmes in the world and recently introduced the world’s first infant meningitis B vaccination programme.
Childhood immunisations are part of the Healthy Child Programme. There is a full checklist of vaccines provided on the NHS in the UK, including additional vaccines that may be required for certain at risk groups.
Childhood and adolescence (5 to 19)
Children and young people face many new challenges and experiences as they grow and develop; part of growing up includes experimenting and trying new things. Risky behaviours are those that potentially expose young people to harm, or significant risk of harm, which will prevent them reaching their full potential.
Some risky behaviour is normal and part of growing up and may be influenced by peer pressure, social media, friends and family and the wider community (Cabinet Office and Department of Health and Social Care, 2015).
Children and young people exposed to adverse childhood experiences have an increased risk of poor health outcomes and health-harming behaviours across the life course. Poor health outcomes include death or injury in childhood, increased risk of disease and poor mental health.
Health-harming behaviours increased by adverse childhood experiences include:
- binge drinking
- poor diet
- smoking
- violence perpetration
- substance misuse
- unintended teenage pregnancy
- increased risk of interface with criminal justice
Adolescence, defined as the transitional phase between childhood and adulthood, is a time when young people begin developing habits that will carry over into adulthood. Healthy behaviours initiated in childhood, such as physical activity and healthy nutrition, should be maintained during adolescence.
PHE’s report on School aged years 5 to 19 high impact area 2: reducing risky behaviours highlights the important role that school nurses can play in building trusting and enduring professional relationships with children and young people throughout their time in education, to enable them to become confident and healthy adults.
Primary interventions
Tackling vulnerabilities and adverse childhood events (ACEs) and safeguarding children
Whilst it is parents and carers who have primary care for their children, local authorities, working with partner organisations and agencies, have specific duties to safeguard and promote the welfare of all children in their area, defined as:
- protecting children from maltreatment
- preventing impairment of children’s health or development
- ensuring that children grow up in circumstances consistent with the provision of safe and effective care
- taking action to enable all children to have the best outcomes
The government has set out that a child centred approach is fundamental to safeguarding and promoting the welfare of every child. A child centred approach means keeping the child in focus when making decisions about their lives and working in partnership with them and their families.
Children may be vulnerable to neglect and abuse or exploitation from within their family and from individuals they come across in their day-to-day lives. These threats can take a variety of different forms, including:
- physical and emotional abuse
- neglect
- loss through bereavement
- exploitation by criminal gangs and organised crime groups
- trafficking
- online abuse
- sexual exploitation
- the influences of extremism leading to radicalisation
Whatever the form of abuse or neglect, practitioners should put the needs of children first when determining what action to take.
Supporting young people’s mental health and emotional wellbeing
Children and young people’s mental and emotional wellbeing is a significant public health priority. The most recent data suggests that 1 in 10 children and young people have some form of clinically diagnosable mental health problem. Three in 4 mental illnesses start before a child reaches the age of 18, while 50% of mental health problems in adult life (excluding dementia) take root before the age of 15 (Chief Medical Officer, 2012).
Building resilience, the ability to be able to bounce back from adversity, in young people can support better outcomes for them whatever challenges they face.
Adolescence is a critical period of development, and a window of opportunity. What happens at this age will have a long-lasting impact. It is worth investing in resilience at this age because human brains develop and change more during the teenage years than at any other time apart from the first 3 years of life. This means that this is a time when there is huge potential for the development of new skills and capabilities.
The environment has a principal role to play for teenage brain development. Enriching environments can enhance development while restrictive ones do the opposite. Young people who are not resilient will be more likely to respond to stress by developing anxiety and depression.
The components for promoting resilience combine:
- development of individual skills
- access to the right information at the right time
- availability of suitable or relevant or expert services and resources when they are needed
- tackling the wider determinants of unequal health outcome
Find out more in PHE’s report on a public health approach to promoting young people’s resilience.
Improving educational attainment
At this stage of the life course, schools and colleges should be promoting the health and wellbeing of pupils and students to improve their educational outcomes and their health and wellbeing outcomes. PHE has developed a briefing on the link between pupil health and attainment and the evidence shows that pupils with better health and wellbeing are likely to achieve better academically and the culture, ethos and environment of a school influences the health and wellbeing of pupils and their readiness to learn.
Tackling tobacco, alcohol and drug use
Reviews into the scale of smoking, drinking and drug use prevalence among young people suggest these behaviours have declined since the late 1990s. However, there are signs that drug use in particular is starting to become more common again. PHE has found that among more disadvantaged groups (including children and young people who are young offenders, not in education, employment or training (NEET), truants, care leavers, homeless or living in socio-economically disadvantaged areas) the prevalence of smoking and drug use is much higher than in the general population. While there is a decline in the number of young people drinking, a number of young people still report drinking over the CMO’s low risk guidelines and young people are more vulnerable to alcohol-related harm.
Most smokers start as teenagers, two-thirds before the age of 18. The reasons they start are complex, ranging from peer pressure to behavioural problems. Children are more likely to take up smoking if they live with people who smoke. The best way to reduce smoking among young people is to reduce it in the world around them.
The impact of having a parent with an alcohol problem on the lives of children can be devastating. It is estimated that there are 200,000 children in England living with 120,000 parents who have alcohol problems. An analysis of serious case reviews (where a child was seriously hurt or killed) found that 37% recorded alcohol as a contributing factor.
Read the case study: Family safeguarding in Hertfordshire
PHE has produced a toolkit for commissioners of alcohol and drug services and children and family services to help understand the extent of parental alcohol and drug use in your local area and how this can impact upon children within the same household.
Reducing the number of teenage pregnancies and improving outcomes for young parents and their children
The under 18 conception rate has fallen by 62% since 1998 with the rate at its lowest level since 1969. However, there remain significant differences in rates between local authorities and inequalities remain between wards. England’s teenage birth rate remains high in comparison with other western European countries and more needs to be done to sustain and accelerate progress.
PHE’s Teenage Pregnancy Prevention Framework, including a self-assessment tool, is designed to help local areas assess their local programmes to see what’s working well, identify any gaps, and maximise the assets of all services to strengthen the prevention pathway for all young people.
Support for young parents is also integral to addressing inequity. Many young mothers and fathers enter parenthood with pre-existing vulnerabilities which contribute to disproportionately poor outcomes and intergenerational inequity for them and their children. These include higher rates of infant mortality, low birth weight and developmental delays.
Teenage mothers have higher rates of poor mental health for up to 3 years after the birth of their child; poor mental health also affects young mothers up to the age of 25. PHE’s Framework to support teenage mothers and young fathers highlights the need for dedicated support for young parents with a coordinated, multi-agency care pathway.
Addressing teenage pregnancy can bring savings, with £4 saved in welfare costs for every £1 spent. Furthermore, every young mother who returns to education, employment and training saves agencies £4,500 a year and for every child prevented from going into care, social services would save on average £65,000 a year.
Return on investment for contraception alone shows for every £1 spent, £9 is saved over a 10 year period. This applies to women of all ages but is particularly relevant for teenagers who are at highest risk of unplanned pregnancy.
PHE’s Teenage Pregnancy Prevention Framework is designed to help local areas assess their local programmes to see what’s working well, identify any gaps, and maximise the assets of all services to strengthen the prevention pathway for all young people.
Vaccination
The following vaccinations are relevant for this stage of the life course:
- HPV vaccine (12 to 13 years)
- 3-in-1 teenage booster (14 years)
- MenACWY vaccine (14 years)
Later in 2019 the HPV vaccination programme offered to all school girls aged 12 and 13 to protect against cervical cancer, will be extended to boys of the same age. The vaccine protects boys from HPV-related diseases, such as oral, throat and anal cancer, but also helps reduce the overall number of cervical cancers in women, though herd immunity.
Working age (16 to 64)
Emphasis on a good start in life does not mean that actions at later stages of the life course are not important. Adulthood is an important time for building assets, reducing risks and intervening early. In England, alcohol misuse is the biggest risk factor attributable to early mortality, ill health and disability for those aged 15 to 49 years.
This stage is crucial as it is a time of significant opportunity to build resilience for later life, to reinforce the improvement in skills and individual empowerment provided by a good start but also to achieve greater health equity among the existing adult population. In particular, it is essential to reduce stress at work, reduce long-term unemployment through active labour-market programmes and address the causes of social isolation.
Primary transition points during adulthood include, for example, starting work, becoming a parent or becoming a carer. At these times, a person may adopt healthy lifestyles and build supportive social networks. Sometimes the life course trajectory is ‘interrupted’ and is less positive, for example through ill health, unhealthy lifestyles or coming into contact with the criminal justice system.
Throughout this period, health professionals can ensure that they make every contact count and use everyday interactions with people to support them in making positive changes to their physical and mental health and wellbeing, as well as promoting services such as the NHS Health Check.
The NHS Health Check offers an opportunity to assess the top 7 risk factors driving premature death and disability in England among 15 million people in midlife. This includes pulse rhythm, BP and cholesterol. They are also supported to understand their risk of CVD and make positive behavioural changes that can prevent and delay the onset of CVD.
For example, everyone having an NHS Health Check should benefit from personalised support and where appropriate access to local services, such as:
- stop smoking services
- weight management services
- physical activity services
- alcohol support services
- NHS diabetes prevention programme
Read the Health Matters edition on using the NHS Health Check programme to prevent cardiovascular disease.
Interventions
Employment opportunities and workplace health
As adults in employment spend a large proportion of their time in work, our jobs and our workplaces can have a big impact on our health and wellbeing. In fact, employment can impact both directly and indirectly on the individual, their families and communities. Therefore, work and health-related worklessness are important public health issues, both at local and national level.
There is clear evidence that good work improves health and wellbeing across people’s lives, not only from an economic standpoint but also in terms of quality of life. ‘Good work’ means having not only a work environment that is safe, but also having a sense of security, autonomy, good line management and communication within an organisation.
Read the Health Matters edition on health and work for actions that employers in general, local authorities, and the NHS workforce can take with regards to health and work.
Improving wellbeing and mental health
More people than ever are working on zero-hours contracts in the UK. Research carried out by the UCL Institute of Education’s Centre for Longitudinal Studies found that people on zero-hours contracts and those who were unemployed were less likely to report feeling healthy, compared to those in more secure employment. They are also at higher risk of poor mental health than workers with stable jobs.
Mental health promotion and mental ill-health prevention: the following prevention activities provide a ROI between £1.26 and £39.11 per £1 spent. Where it is possible to estimate impacts on quality of life, all the interventions seem to be cost-effective, with a cost per quality-adjusted life year (QALY) gained below £20,000. This is the same threshold as used by the National Institute for Health and Care Excellence (NICE):
- workplace programmes to help adults at risk of stress, anxiety and depression
- mental health support for people with long term physical health problems eg diabetes and heart disease
- group based social activities, including volunteering, to address loneliness
- financial advice services for people with debt problems located in primary care
- initiatives to identify and support people who have self-harmed and are potentially suicidal
PHE provides comprehensive guidance for commissioners and health professionals to make decisions about mental health services and interventions based on data and analysis.
Musculoskeletal health (MSK)
MSK conditions are problems of the bones, joints, muscles and spine, and are a common cause of severe long-term pain and physical disability. In 2017, MSK problems were the second most common cause of sickness absence in England after coughs and colds, accounting for 28.2 million days lost in work (17.7% of total sickness absences).
PHE has produced a range of MSK tools including:
- PHE’s Musculoskeletal Diseases profile to help understand the health needs of your local populations, the number of people accessing services and the outcomes services deliver
- PHE’s ROI tool to assess interventions designed to prevent and treat individuals with MSK conditions
You can read more about MSK in the productive healthy ageing and MSK health edition of Health matters.
Screening
Screening saves lives and improves health. Many of the conditions for which we offer screening and treatment disproportionately affect individuals from socio-economically deprived backgrounds or those with the 9 protected characteristics as described in the 2010 Equality Act. National screening programmes therefore have an important role to play in reducing health inequalities.
Every year:
- 5,000 deaths are prevented by cervical screening
- 2,400 bowel cancer deaths are avoided by screening
- breast screening prevents 1,300 women dying of breast cancer every year
- 7,000 people with sight threatening diabetic retinopathy are referred to hospital eye services for urgent treatment
Ageing well
There has been a steady increase in average life expectancy in recent decades, albeit increases have slowed considerably since 2011.
There are now half a million people in their 90s in the UK according to the Office for National Statistics (ONS). This is more than two and a half times the number in 1985. By 2041 in the UK, the ONS estimates that there will be 3.2 million people aged 85 years and older.
This is a public health success story. Longer lives are a benefit to society in many ways, including financially, socially and culturally, because older people have skills, knowledge and experience that benefit the wider population. There is an opportunity to utilise this increased longevity as a resource, whilst challenging ageism and the view that retirement is about ‘sitting more and moving less’.
The older a person is, the more likely they are to experience chronic diseases and disabilities of both the body and brain. As life expectancy rises, we must promote the concept of productive healthy ageing, which involves:
- improved health and wellbeing
- increased independence and resilience to adversity
- the ability to be financially secure through work and build resources
- engagement in social activities
- being socially connected with enhanced friendships and support
- enjoying life in good health
Primary interventions
Access to good employment
Being in good quality work supports health and wellbeing because work generally provides the income needed to live a healthy life, is a source of social status, and offers opportunities to participate fully in society. You can read more about how work benefits health and wellbeing in the Health and Work edition of Health Matters.
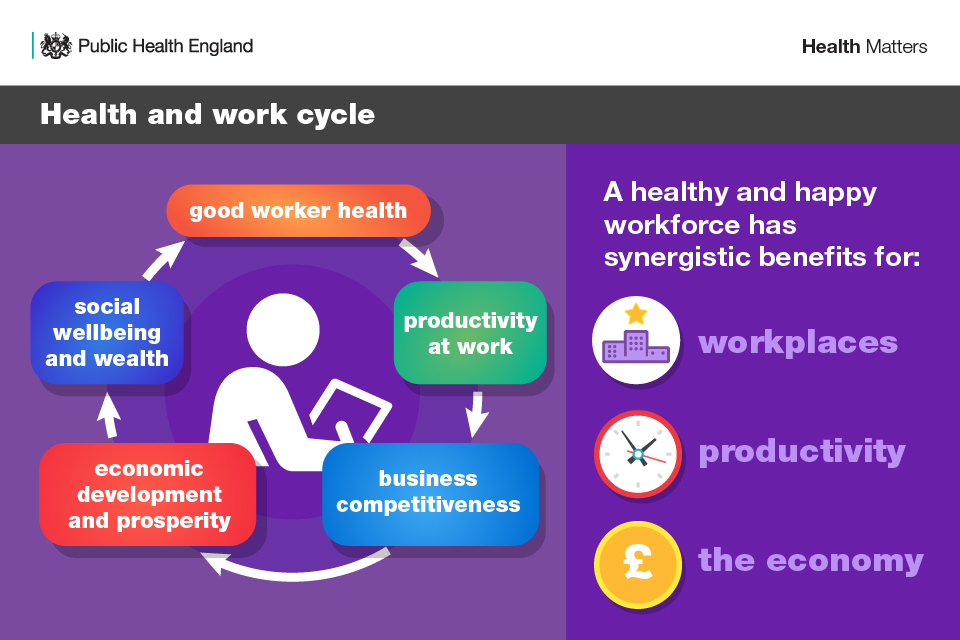
Infographic showing that a healthy and happy workforce has benefits for workplaces, productivity and the economy
With an ageing population that is facing the prospect of working to older ages, good quality employment opportunities for older people are essential and can bring additional benefits for health and wellbeing.
PHE and the UCL Institute of Health Equity’s Local action on health inequalities: Increasing employment opportunities and retention for older people report outlines what works to increase employment opportunities and retention for older people, including:
- improvements to the physical and psychosocial work environment
- fair recruitment practices that encourage applications from older people
- encouraging training opportunities and making them accessible for workers of all ages
- flexible working
- phasing retirement and flexible retirement options
Local authorities have a role as employers and as local leaders in improving employment opportunities and job retention for older people. Effective action to address the barriers that may prevent older people from finding and staying in work should help to improve health and wellbeing within this group.
Housing and the built environment
The built environment and well-designed outdoor spaces are important wider determinants of health. They can enhance the long-term health and wellbeing of those who use them regularly, reduce the risk of falls, promote physical activity, and reduce social isolation.
Providers of housing and housing with care have an important role in enabling active ageing within the home environment. Important actions to promote active ageing within the home or housing with care include:
- recognising the need to plan and build housing that is appropriate and adaptable to the needs of older people
- supporting the development of extra care housing with its emphasis on inclusive design and independent living
- encouraging care homes to provide all residents with access to gardens and assistance to enjoy them
- ensuring that regeneration programmes consider the impact on older people in terms of active ageing
- landscaping and ongoing maintenance of external space to encourage outdoor activities
- developing partnerships with other local stakeholders to promote active ageing in the community
Supported by PHE, Housing LIN have a report on Active Ageing and the Built Environment, which includes more interventions and case studies. It also outlines the role of local authorities in ensuring their housing and built environment allow healthy and active ageing.
Vaccination
Vaccination brings benefits across the life course. In England, patients aged 65 and over are eligible to receive vaccination against flu and pneumococcal infection.
Patients are eligible for the shingles vaccine as soon as they turn 70 or 78 years of age. Anyone who was eligible in previous years but who has not yet had the vaccine remains eligible until they turn 80 (this includes anyone in their 70s who was born on or after 2 September 1942, and anyone who is 79 years old).
Maintaining functional ability: brain and body health
The World Health Organization’s Global Healthy Ageing Strategy talks not of age, but rather ‘functional ability’, which as described earlier is a combination of intrinsic capacity (physical and mental abilities) and environmental factors (transport, housing, relationships).
1. Dementia
The mortality rate from dementia and Alzheimer’s disease in males and females has increased steadily since 2006 (note that some of the recent increase is likely to be due to deaths being classified as dementia that would not have been in the past) and these rates are expected to continue to increase for both males and females. Dementia is already the number one cause of death among women and could overtake heart disease to become the number one cause of death in men by 2020.
NICE’s guidance on mid-life approaches to delay or prevent onset of dementia, disability and frailty in later life recommends reducing the risk of these health conditions by helping people to:
- stop smoking
- be more active
- reduce their alcohol consumption
- improve their diet
As outlined in the Menu of Interventions for Productive Healthy Ageing, there are several interventions that can be actioned to make a dementia friendly pharmacy, where the environment and communication with people diagnosed with dementia and their carers is adapted. There are also lifestyle interventions for dementia risk reduction.
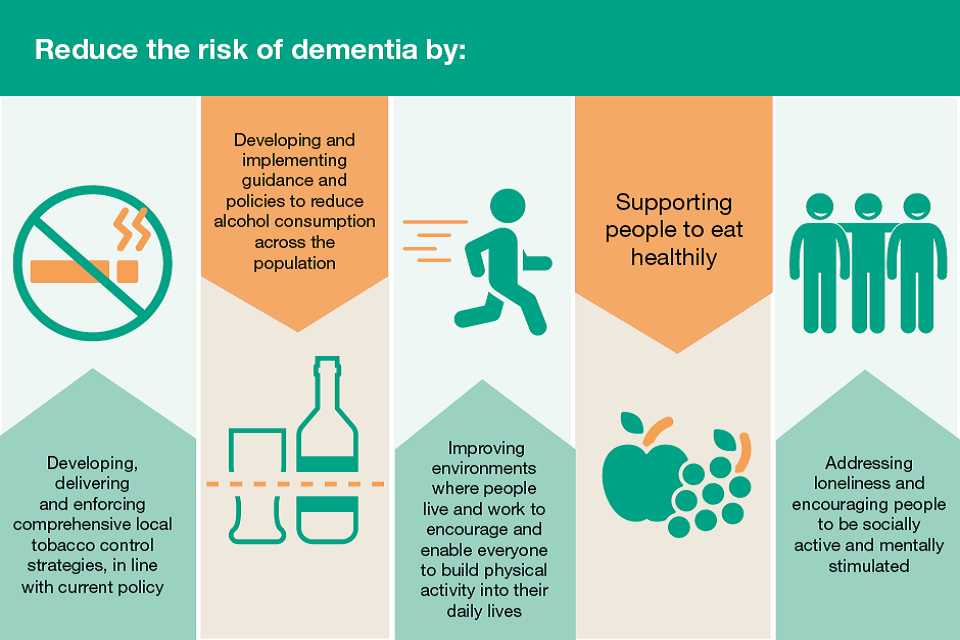
Infographic showing how to reduce the risk of dementia: stopping smoking reduce alcohol intake, physical activity, eating healthily, socially active and mentally stimulated
2. Depression
Depression can affect anyone, but more older people are affected than any other age group as they are more vulnerable to factors that lead to depression, including:
- being widowed or divorced
- being retired or unemployed
- physical disability or illness
- loneliness and isolation
- neurobiological changes associated with ageing
- prescribed medication for other conditions
Depression affects around 22% of men and 28% of women aged 65 years and over. However, it is estimated that 85% of older people with depression do not receive help.
PHE’s Older People’s Mental Health Data Catalogue provides a platform of data and resources relevant to depression in older people, and signposts to information which will increase awareness and understanding of the mental health needs of older people at both a national and local level.
Preventing falls
Falls are very common, with around a third of people aged 65 and over experiencing a fall each year, increasing to half of those aged 80 and over. In around 5% of cases, a fall leads to fracture, one of the most serious MSK problems seen in the older population, and hospitalisation. There are around 255,000 falls-related emergency hospital admissions in England among patients aged 65 years and over each year, and an audit by the Royal College of Physicians found that fractures and falls in people aged 65 and over account for over 4 million hospital beds each year in England. Therefore, preventing falls is important for helping to maintain the independence and wellbeing of older people and their carers, as well as our health and social care services.
PHE’s falls prevention tool, Return on Investment of Fall Prevention Programmes in Older People in the Community, has been designed for healthcare commissioners and providers in England who wish to assess the ROI for community-based falls prevention programmes for older people. The tool aids decision-making and helps increase the uptake of cost-effective programmes.
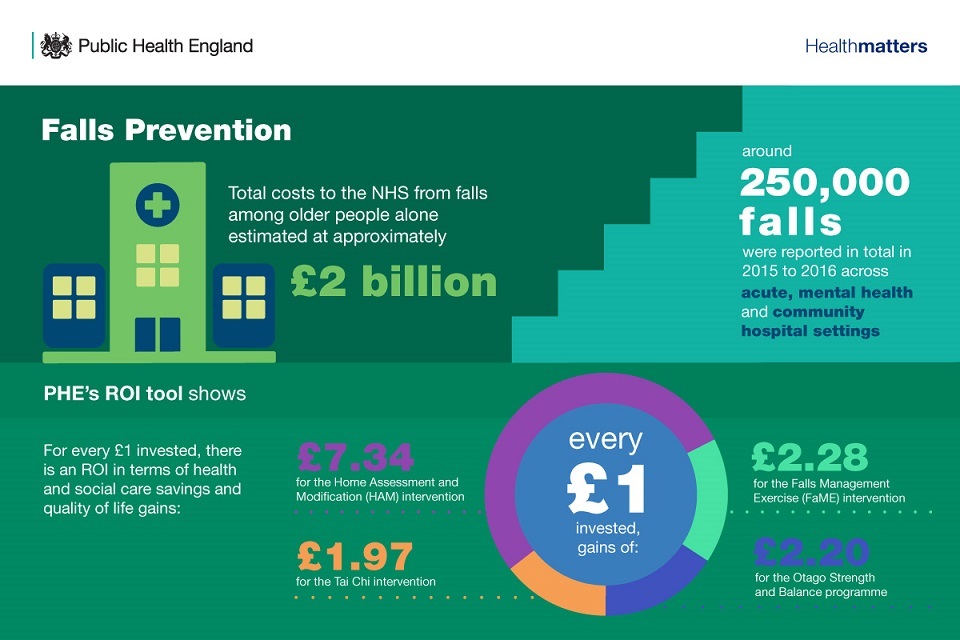
Infographic showing the return on investment from falls prevention
The Menu of Interventions for Productive Healthy Ageing also outlines the interventions that pharmacy teams can carry out to support falls prevention.
Preventing loneliness and social isolation
Anyone can experience social isolation and loneliness, but it is more commonly considered in later life. As our population ages, the number of older people grows, and we are therefore seeing an increase in the absolute number of people experiencing chronic and severe loneliness. In fact, 1 million older people in the UK can go for a whole month without speaking to a friend, neighbour or family.
Retirement can be a time of increased wellbeing as the burden of work pressures is reduced and individuals have time to take up a different range of activities. However, some retired and older people are at risk of social isolation, which, when experienced at older ages, increases the risk of premature mortality by up to 26%.
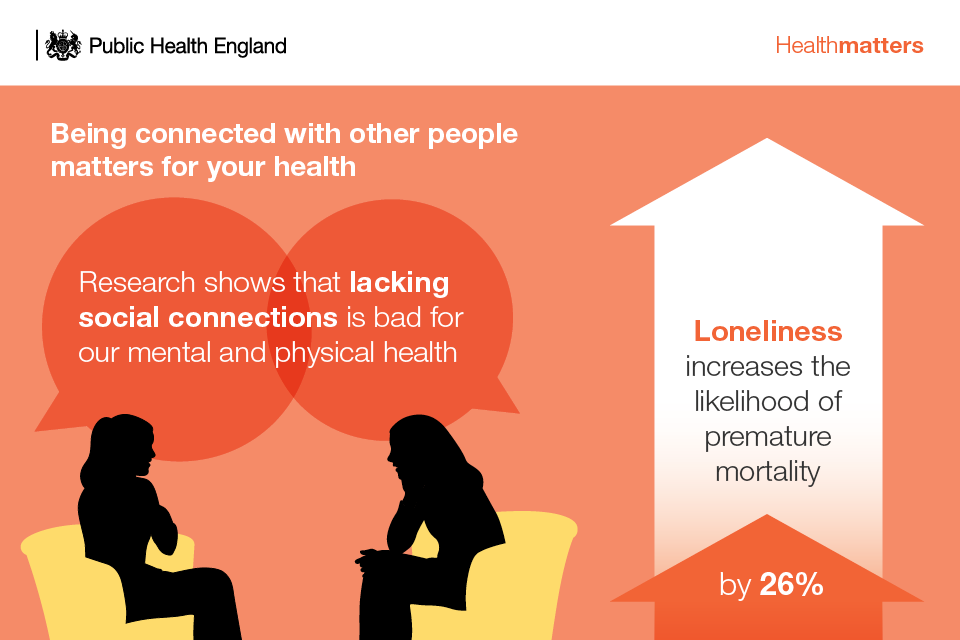
Infographic illustrating that being connected with other people matters for your health
Three life events in particular are associated with social isolation among older people:
- retirement and losing connection with colleagues
- falling ill and becoming less mobile
- a spouse dying or going into care
PHE and the UCL Institute of Health Equity’s Reducing social isolation across the lifecourse report is a practical resource that outlines interventions to reduce social isolation at different stages of the life course, including retirement and later life.
Actions across the life course
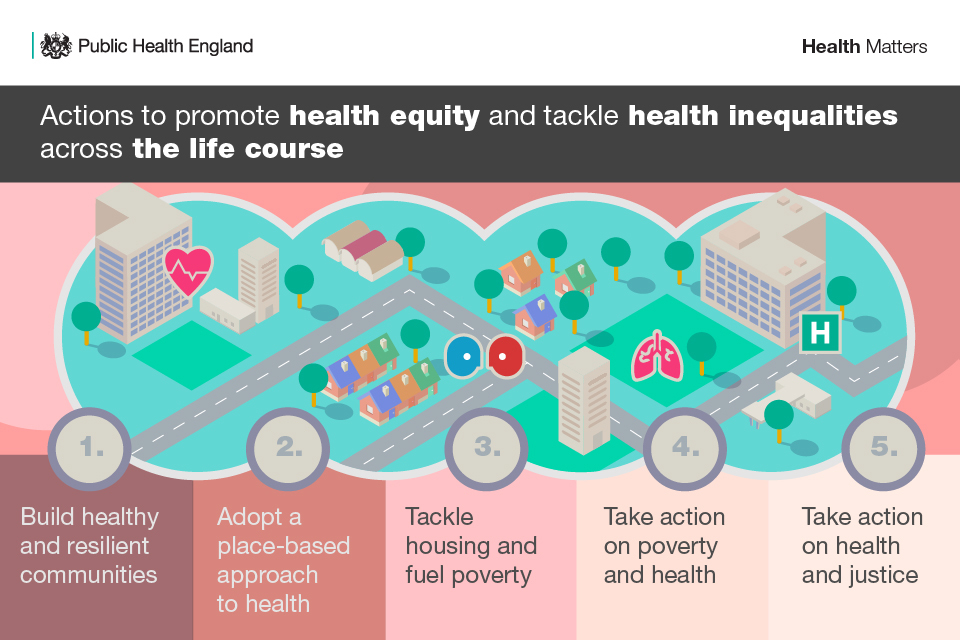
Infographic showing actions to promote health equity and tackle health inequalities across the life course
Actions to promote health equity and tackle health inequalities across the life course and from generation to generation:
- Build healthy and resilient communities
- Adopt a place-based approach to health
- Tackle housing and fuel poverty
- Take action on poverty and health
- Take action on health and justice
Prioritising prevention of ill health
Now is the time to prioritise prevention of ill health. Action is needed by the NHS, by national government and by local government, all working in partnership with the voluntary, community and private sector. Together we can ensure that our children have the best start in life and are ready to start school, that our young people are supported so they enter adulthood ready to start work, that adults are able to secure and maintain a job and a home and that older adults have fulfilling, productive and connected lives.
When using a life course approach:
- ensure your intervention fits the life course framework of taking action early, appropriately and together
- take the long view - consider the intra and intergenerational aspects of the issue you are trying to tackle
- consider how your intervention minimises risk factors and enhances protective factors
- ensure your intervention strives to achieve health equity and tackle health inequalities, working together with partners
- undertake evaluation and monitoring of your approach to add to the evidence base
PHE has produced several tools to help monitor and evaluate your approach to prevention across the life course. These include PHE resources on evaluation in health and wellbeing as well as a range of monitoring tools:
- Public Health Outcomes Framework (PHOF)
- Health Inequalities Dashboard
- Wider Determinants of Health Profile
- Early years foundation stage profile (EYFSP)
- Mental Health Profiling Tools including: Mental health and wellbeing JSNA Profile, JSNA toolkit and Children and Young People’s mental health and wellbeing profiling tool
Resources
These resources can be used in presentations of your own or to share with colleagues:
- expanded interventions table
- supporting references
- Health matters infographics
- read the Health matters blog
- Health inequalities chart
Health matters case studies highlight projects and approaches that have been put in place to improve public health:
