HPR volume 13 issue 19: news (7 and 10 June)
Updated 20 December 2019
PHE publishes full annual STIs data for 2018
Public Health England (PHE) has released its annual data on sexually transmitted infections and screening for chlamydia in England, together with a detailed commentary on the data in a report entitled, Sexually Transmitted Infections and Screening for Chlamydia in England, 2018 [1].
The review report provides an overview of trends for the sexually transmitted infections (STIs) of most concern in England: gonorrhoea, syphilis, chlamydia, genital herpes and genital warts [1].
The latest data show that the overall number of new STI diagnoses increased by 5% in 2018, compared with 2017 (from 424,724 to 447,694). The increase in the total number of new STIs was due to a large increase in gonorrhoea (26%; from 44,812 to 56,259) and more moderate increases in chlamydia (6%; from 205,365 to 218,095), syphilis (primary, secondary and early latent stages: 5%; from 7,149 to 7,541), and first episode genital herpes (3%; from 32,828 to 33,867) diagnoses. The increase in gonorrhoea (see figure) was observed in both heterosexuals and gay, bisexual and other men who have sex with men (herein referred to as MSM) and is of particular concern given the recent emergence of extensively drug resistant Neisseria gonorrhoeae [2].
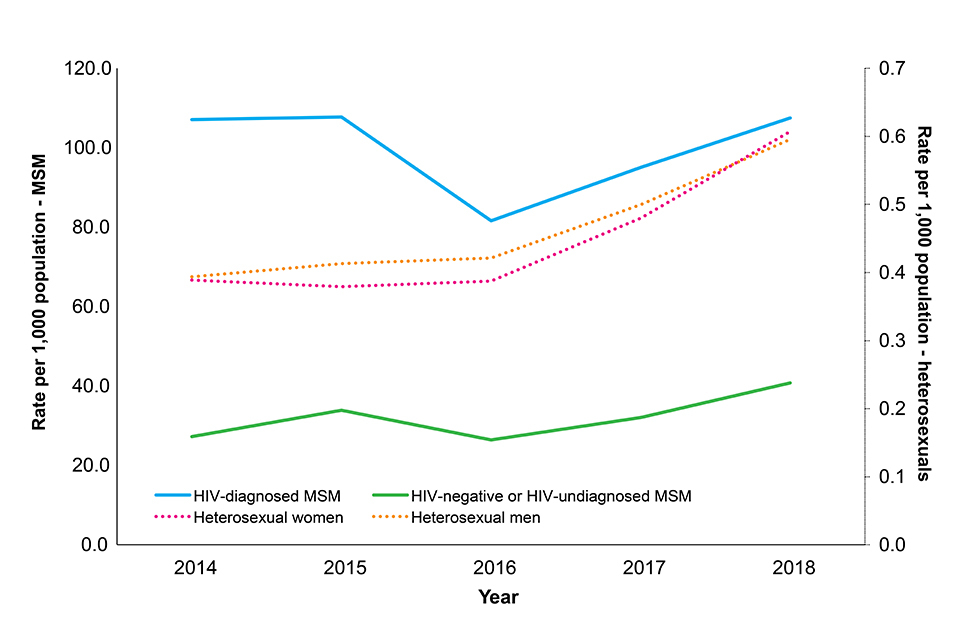
Population diagnosis rates of gonorrhoea, by sexual orientation and among gay, bisexual and other men who have sex with men (MSM), HIV status, 2014 to 2018, England. [See main report for data sources and notes]
However, there were continued falls in genital warts diagnoses. In 2018, the rate of genital warts diagnoses among girls aged 15 to 17 years attending sexual health services (SHSs) – most of whom would have been offered the quadrivalent human papillomavirus (HPV) vaccine (protecting against HPV types 16,18, 6 and 11) when aged 12 to 13 years old – was 92% lower compared to 2014 (20.2 vs 257.9 per 100,000 population). A decline of 82% (10.6 vs 59.2 per 100,000 population) was seen in same-aged heterosexual boys over this time period, suggesting substantial herd protection.
Chlamydia was the most commonly diagnosed STI in 2018, accounting for 49% (218,095 cases) of all diagnoses. In 2018, over 1.3 million chlamydia tests were carried out among England residents aged 15 to 24 years – the target age group for the National Chlamydia Screening Programme (NCSP). There was a 1% decline in the number of chlamydia tests conducted in 15 to 24 year olds between 2017 and 2018, however, due to an increase in the proportion testing positive, this resulted in a 2% increase in the number of chlamydia diagnoses (to 131,269) over this period. Chlamydia screening activity for 15 to 24 year olds continued to decline in non-specialist SHSs, with the exception of online sexual health services, which increased by 54% and now account for 17% of tests and 14% of chlamydia diagnoses in this age group.
The annual STI/NCSP report [1,3] concludes by highlighting PHE’s initiatives to address the higher rates of STIs in MSM, black ethnic minority populations and young people.
The full range of data and commentary published this week is provided on PHE’s annual STI and NCSP data pages in the form of data tables and slide sets. An infographic is also available, and refreshed data for HIV/STI indicators have been published to PHE’s Sexual and Reproductive Health Profiles.
References
- PHE (4 June 2019). Sexually transmitted infections and screening for chlamydia in England, 2018, HPR 13(19) Advance Access report.
- GOV.UK (9 January 2019). Two cases of resistant gonorrhoea diagnosed in the UK.
- People urged to practise safer sex after rise in STIs in England, PHE press release, 4 June 2019.
Syphilis Action Plan for England
The number of diagnoses of infectious syphilis seen in England has increased substantially in recent years. Following a gradual increase in diagnoses between 2000 and 2012, an increase of 126% was seen between 2013 (3,344) and 2018 (7,541), including a 5.5% increase between 2017 and 2018. In 2018, most diagnoses (75%) were made in gay, bisexual and other men who have sex with men (MSM) and the diagnosis rate was highest in MSM who were aware that they were living with HIV at the time of syphilis acquisition (see figure).
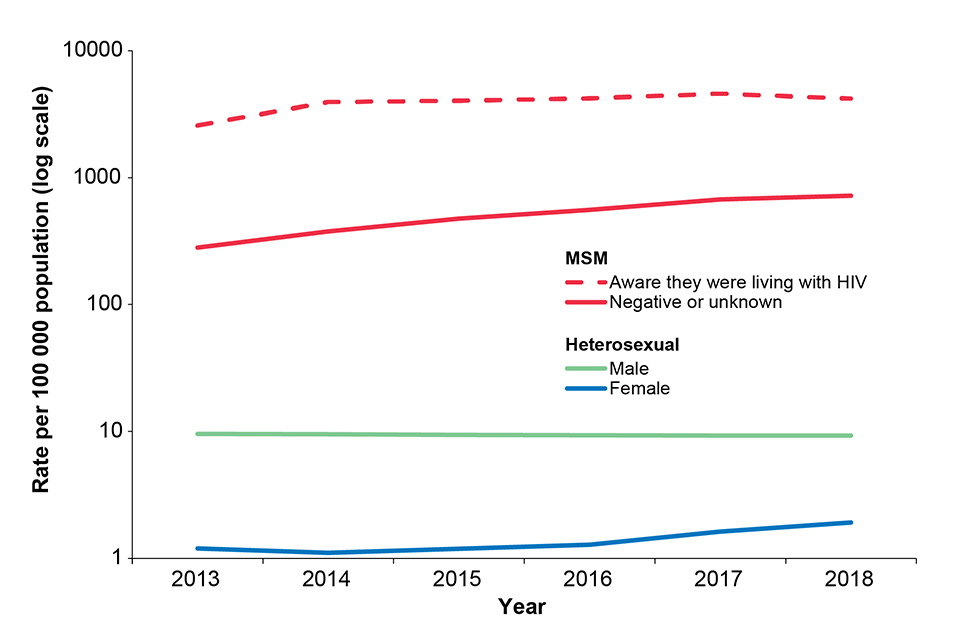
Population diagnosis rates of infectious syphilis by sexual orientation and among gay, bisexual and other men who have sex with men (MSM), awareness of HIV status when syphilis acquired, England: 2013 to 2018. [See Action Plan for data sources and notes]
To address the continued increase in syphilis in England, PHE published a Syphilis Action Plan alongside the annual STI data release on 4 June 2019 [1,2]. The Action Plan summarises existing national guidelines and best practice guidance into four prevention pillars fundamental to syphilis control and prevention:
- increasing testing frequency of high-risk MSM and re-testing of syphilis cases after treatment
- delivering partner notification to BASHH standards
- maintaining high antenatal screening coverage and vigilance for syphilis throughout antenatal care
- sustaining targeted health promotion
References
- PHE (4 June 2019). PHE Syphilis Action Plan.
- PHE (4 June 2019). Sexually transmitted infections and screening for chlamydia in England, 2018
EVD outbreak in eastern DRC: tenth update
The outbreak of Ebola virus disease in eastern Democratic Republic of the Congo continues. As of 3 June 2019, 1,926 confirmed and 94 probable cases had been reported in North Kivu and Ituri provinces [1]. Of these, 459 were newly confirmed cases reported between 1 and 31 May, the largest monthly total to date in this outbreak. There have been 1,354 deaths, 370 since the last update.
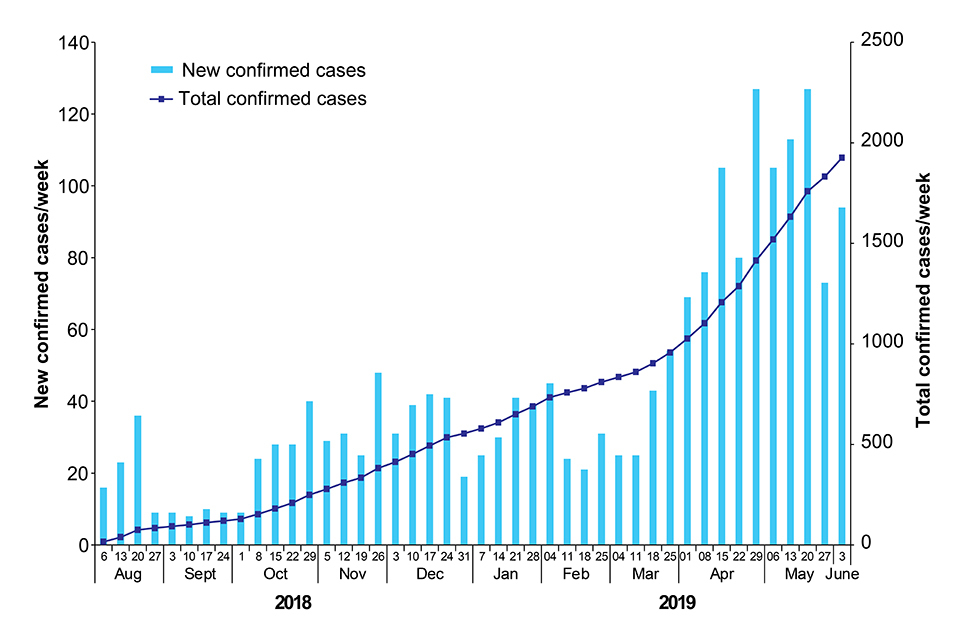
Figure: New and total confirmed cases by week. Data provided by DRC MoH [2]
Over 2,000 confirmed and probable cases have now been reported. Comparison of the period over which the first thousand cases were reported (1 August 2018 to 23 March 2019, 233 days), with that for the second thousand (24 March to 2 June, 71 days), provides stark evidence of the recent marked escalation in case reporting [2].
During May, 4 zones reported more than 67% of the cases: 98 (21%) in Mabalako, and 210 (46%) from Katwa, Butembo, and Beni combined. A new health zone in North Kivu, Alimbongo, reported its first confirmed case, bringing the total number of affected health zones to 22. Further healthcare workers were confirmed as cases during May, bringing the total to 110. An additional 28 probable cases were retrospectively identified across 7 health zones – all community deaths which had occurred between 30 January and mid-May.
Over the 21 days to 30 May, 14 health zones reported new cases demonstrating that transmission is still widespread.
While there has been some improvement in the security situation over the last month, outbreak response activities continue to be hampered and there is ongoing uncertainty regarding the completeness of surveillance and detection of all new cases. The outbreak does, however, remain confined to the same two provinces in DRC, and no spread within the country or internationally has been detected to date [3].
Despite the critical situation in DRC, the risk to the UK public remains very low to negligible. The situation is being monitored closely and the risk assessment regularly reviewed.
Further information sources
- GOV.UK website collection Ebola virus disease: clinical management and guidance
- NaTHNaC website travel advice Travel Health Pro website
- WHO website EVD homepage Ebola virus disease
- FCO travel advice DRC advice
References
- DRC Ministry of Health update, 4 June 2019 (in French).
- DRC Ministry of Health daily updates (in French).
- WHO Disease Outbreak News update, 30 May 2019.
Infection reports in this issue
This issue includes:
Sexually transmitted infections and screening for chlamydia in England, 2018
