HPR volume 13 issue 41: news (20 December)
Updated 20 December 2019
Infections among people who inject drugs in the UK: annual report in summary
Shooting Up, the annual report on infections among people who inject drugs in the United Kingdom, has been published by Public Health England. The report has been produced in collaboration with Health Protection Scotland, Public Health Wales, and Public Health Agency Northern Ireland.
People who inject drugs (PWID) are vulnerable to a wide range of infections that can result in high levels of morbidity and mortality. The Shooting Up report provides an update on the extent of infections among PWID in the UK and of associated risk and protective behaviours. Key messages are presented below.
Bacterial infections
Preventable bacterial infections are increasing. The cause of the rise is not clear and there are likely to be several factors involved. Services that work with PWID should encourage people with skin lesions or other signs of infection to seek prompt medical attention, ensure easy access to needle and syringe programmes (NSPs) and emphasize safer and hygienic injection practices.
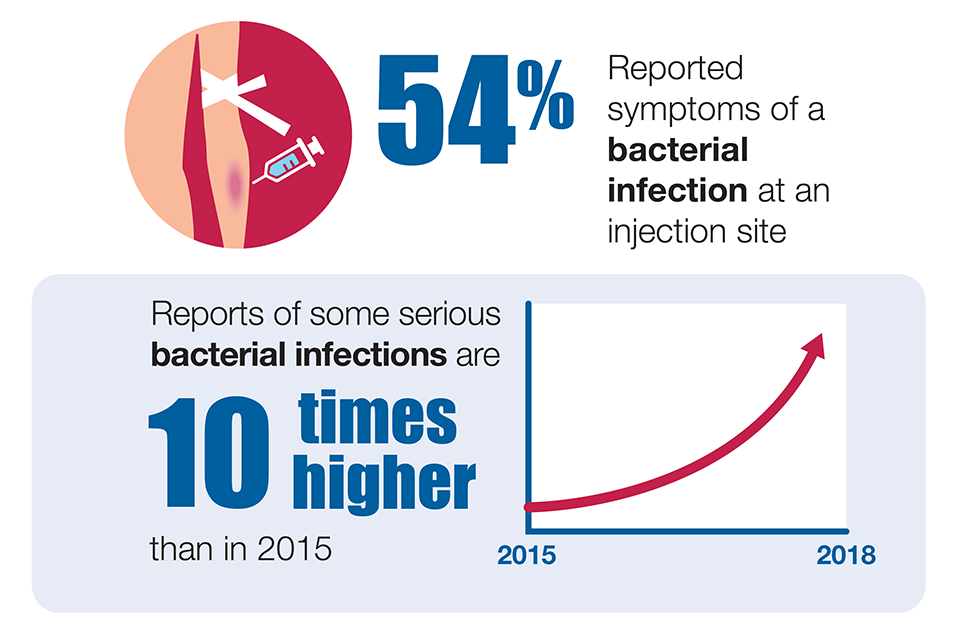
Bacterial infections infographic
Hepatitis C
Hepatitis C continues to be a major problem among people who inject drugs in the UK, with around 1 in every 4 currently infected. There is early evidence of a modest reduction in the prevalence of current hepatitis C infection and this is likely attributable to the increase in uptake of testing and treatment. However, there has been little change in transmission of new infections among PWID and improved coverage of harm reduction such as NSPs and opioid substitution treatment (OST) uptake are needed to reach elimination targets.

Hepatitis C infections infographic
HIV
The prevalence of HIV remains low, but outbreaks of HIV among PWID continue to occur. As HIV is often diagnosed at a late stage among PWID, regular testing should be encouraged.
Hepatitis B
Hepatitis B remains uncommon in PWID but vaccine uptake needs to be sustained, especially in younger age groups and recent initiates to injecting where the uptake of vaccination is particularly low.
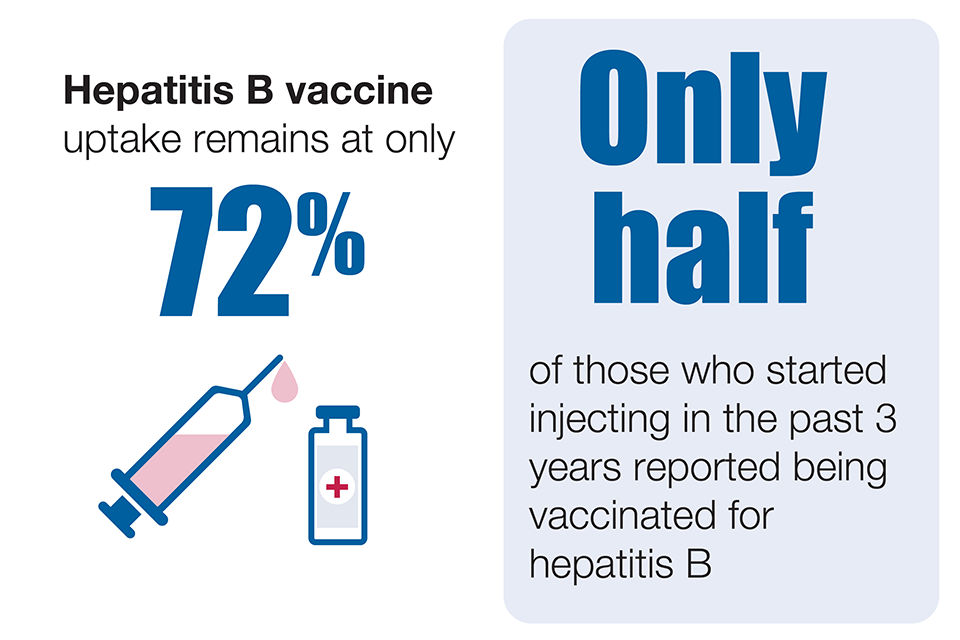
Hepatitis B infections infographic
Sharing and re-use of injecting equipment
Continued sharing and re-use of injecting equipment remains a concern. Adequate provision of new, sterile injecting equipment is vital to reduce sharing and re-use and the associated risks.
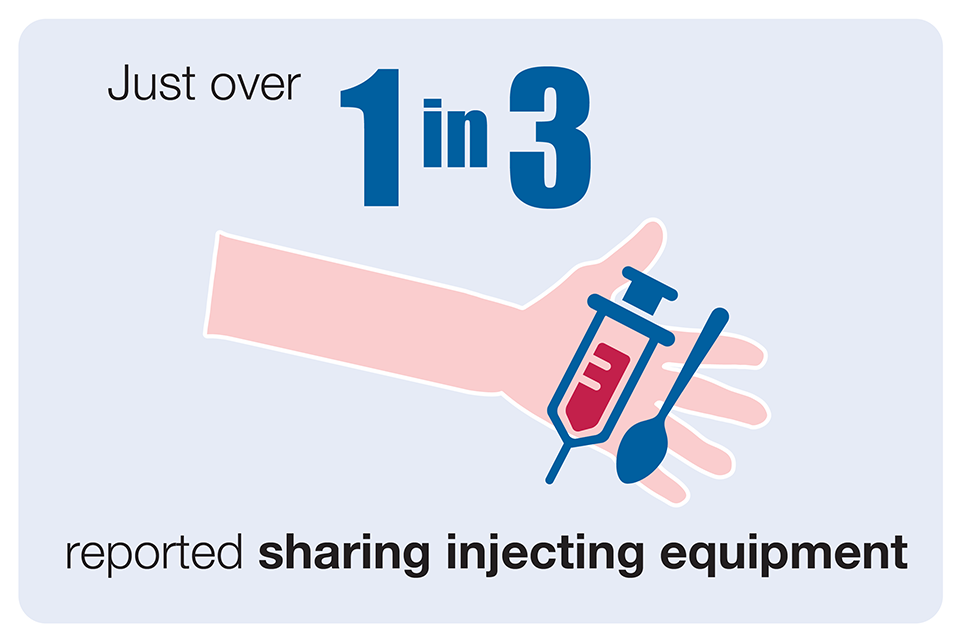
Sharing injection equipment infographic
Psychoactive drug trends
Changes in psychoactive drug preferences could lead to riskier injecting practices, particularly the observed increase in injection of crack cocaine in England and Wales, and increase in injection of powdered cocaine in Scotland.

Psychoactive drugs infographic
Effective interventions
Provision of effective interventions, including OST and NSPs, need to be maintained and optimised [1,2]. In addition, the appropriate provision of the following services needs to be maintained and optimised to prevent and treat infections [2]:
- diagnostic testing for blood-borne infections, including HIV, hepatitis C and hepatitis B
- access to care and treatment for those infected
- vaccinations, including for hepatitis B
- information on avoiding injection site infections and easy access to wound care services and treatment for injection site infections
Sufficient coverage of these interventions is vital to prevent infections and should be responsive to changes in the pattern and the nature of injecting drug use.
References
-
NICE (2014). Needle and syringe programmes: providing people who inject drugs with injecting equipment Public Health Guidance, PH52.
-
DH (2017). Drug Misuse and Dependence: UK guidelines on clinical management.
Influenza indicators increasing in the UK
Influenza activity in England, Wales, Scotland and Northern Ireland continued to increase across several surveillance indicators during the week-ending 15 December 2019, according to the PHE’s latest Weekly National Influenza Report.
The RCGP general practitioner consultation rate for influenza-like illness remains above the baseline threshold. Health service impact indicators of hospitalisation and intensive care admission rates were increasing and at moderate intensity levels.
There were 586 hospitalised influenza cases across the UK in the sentinel scheme (a rate of 6.85 per 100,000 population compared with 5.13 in the previous week). There were 174 admissions to intensive care reported from the mandatoryscheme. Indicators suggested that RSV activity was starting to plateau but continuing to circulate among the under-fives in England.
Flu vaccine uptake registered by reporting GP practices in England indicated that the proportion of people who had received the 2019/20 influenza vaccine in targeted groups in 79.4% of GP practices reporting for the main collection was: 38.5% in under 65-year-olds in a clinical risk group, 39.5% in pregnant women and 69.3% in the over-65s. In 78.4% of GP practices reporting for the childhood collection, the proportion vaccinated was: 32.5% in 2 year olds and 31.7% in 3 year olds.
Data from the second monthly collection of influenza vaccine uptake by frontline healthcare workers showed 61.5% were vaccinated by 30 November 2019, compared to 61.0% vaccinated in the previous season.
The second monthly collection of influenza vaccine uptake data for primary school children indicated: 46.4% uptake among reception age children, 45.8% in the school year 1 cohort, 45.0% in school year 2, 43.7% in school year 3, 43.2% in school year 4, 41.3% in school year 5 and 39.7% in school year 6 (as at 30 November 2019).
RSM conference: Spotlight on Falling Vaccination Rates, February 2020
In 2019, the UK lost its measles-free status from the World Health Organization, as childhood vaccination rates in the country fell across the board. This event, designed specifically for healthcare professionals, will focus on the factors contributing to the decline and what can be done to address falling vaccination rates.
Topics to be covered include:
- why vaccination rates are falling, looking at the data, trends and factors involved
- understanding the extent to which vaccine hesitancy and misinformation around vaccines is affecting vaccination rates, with a particular focus on the impact of social media
- direct experiences from frontline staff who talk daily with patients, parents, and children
- appropriate responses to questions and concerns raised
Venue: Royal Society of Medicine, London W1G 0AE.
Conference website: Spotlight on falling vaccination rates.
Infection and vaccine coverage reports in this issue
This issue includes:
Infection reports
- Laboratory-confirmed measles, mumps and rubella (England): July to Sept 2019
- Laboratory confirmed cases of pertussis (England): July to September 2019
- Laboratory confirmed cases of invasive meningococcal infection (England): July to September 2019
- Laboratory reports of hepatitis C in England and Wales, January to March 2019
- Laboratory reports of hepatitis C in England and Wales, April to June 2019
- Laboratory surveillance of pyogenic and non-pyogenic streptococcal bacteraemia in England, Wales and Northern Ireland: 2018
Vaccine coverage reports
Pertussis vaccination programme for pregnant women update: vaccine coverage in England, April to September 2019.
