HPR volume 18 issue 10: news (28 November and 2 December)
Updated 20 December 2024
Increasing levels of norovirus activity in England
Norovirus is the most common cause of infectious gastroenteritis worldwide and contributes significantly to winter pressures on the NHS and social care each winter. Also known as the ‘winter vomiting virus’ norovirus is transmitted through ingestion of viral particles and has a very low infectious dose, so is easily passed on by close contact with an infected person or a contaminated object as well as consumption of contaminated food or water. Symptoms including vomiting, diarrhoea, fever and muscle aches are usually short-lived, only lasting 2 to 3 days, and resolve without medical treatment. While norovirus infects people of all age groups, people in vulnerable groups such as the very young, elderly and immunocompromised people are at risk of more severe or prolonged illness which can lead to dehydration and may require treatment in hospital.
Outbreaks often occur in closed setting such as prisons, nurseries or schools, but the biggest impacts are seen in hospital and care homes settings where ward/home closures and staff sickness cause great disruption every year and contribute to winter pressures in the NHS. Previous studies have estimated norovirus outbreaks costs at £298 million per year to NHS inpatient services and results in around 30,000 bed days lost (1).
Since late 2023 norovirus laboratory reporting to national surveillance has been consistently higher than expected and norovirus activity has remained high into the start of the 2024/2025 season.The cumulative total of norovirus laboratory reports since the start of the season in week 27, 2024, is more than double the 5-season average (3,425 compared to 1,491) (see Figure 1) (2).
During weeks 45 and 46 reports were almost double (+98.6%) the 5-season average for the same reporting period. Outbreaks reported to UKHSA in hospital settings are also 19.4% higher than the 5-season average (75 outbreaks compared to 63).
Figure 1. Norovirus laboratory reports in England by week during the 2023/2024 and 2024/2025 seasons, compared with 5-season average*

*‘5-season average’ is calculated from the same period during the 5 prior seasons excluding the seasons which were impacted by the COVID-19 pandemic (2019/2020. 2020/2021, 2021/2022). The 2023/2024 5-season average is calculated from 2015/2016, 2016/2017, 2017/2018, 2018/2019 and 2022/2023; the 2024/2025 5-season average is calculated from 2016/2017, 2017/2018, 2018/2019, 2022/2023 and 2023/2024.
Activity is now increasing across all age groups, with the biggest increase in adults, particularly adults aged 65 years and over. Overall compared to the 5-season average the age-distribution has been more skewed towards adult groups so far this season, with 49.4% (+9.6% compared to the 5-season average) of reports from cases in the 65 years and over group, 29.6% (+4.2% compared to the 5-season average) in the 18 to 64 year group, but only 15.6% in children aged 0 to 4 years (-13.5% compared to the 5-season average) and a comparable percentage of children aged 5 to 17 years group at 4.8%.
While some of the increased reporting may be attributable to the increased use of PCR multiplex technology (capable of detecting multiple gastrointestinal pathogens in one test) at frontline diagnostic laboratories, it is likely that the emergence of an unusual norovirus genotype, GII.17 (Figure 2), as well as changes in the epidemiology following the COVID-19 pandemic and other factors, are contributing to the observed rise.
Figure 2. Trends of GII norovirus samples typed as genotype GII.17, GII.4 or another GII in England by season, 2017/18 to mid-November of 2024/2025*
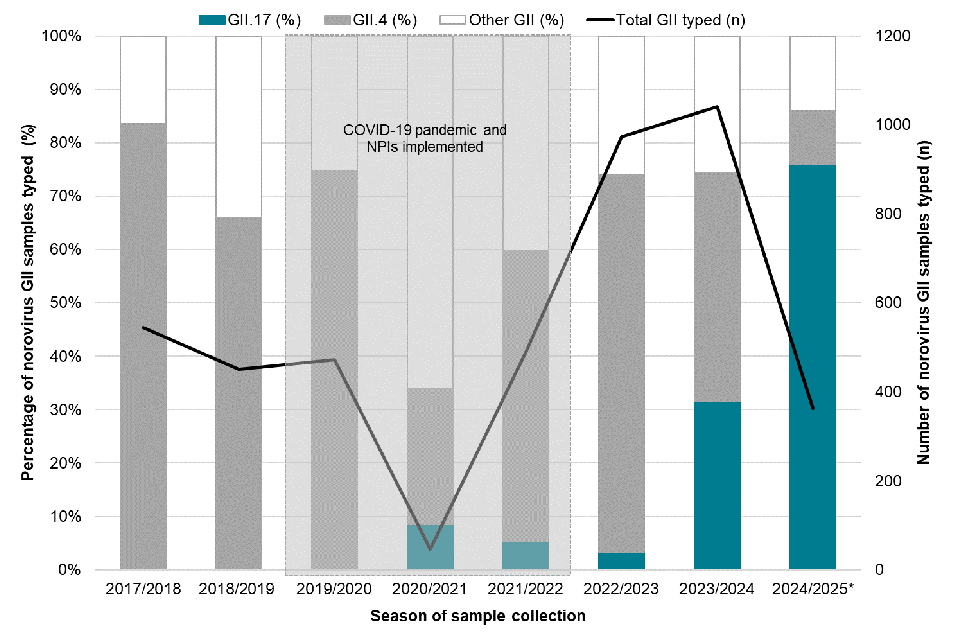
*Data for 2024/2025 season incomplete as only available up to week 45 (commencing 18 November 2024)
The usual escalation in reporting seen each autumn has started earlier than in previous seasons and, following a drop in reporting which coincided with the October half-term school holidays, reports are expected to continue to increase. A shift in the timing of the seasonal increase does not always result in a higher peak of norovirus activity; however, the ‘unexpected’ activity has potential to cause more significant impacts in health and social care settings.
The latest data on norovirus is published weekly during the winter months as Official Statistics and UKHSA guidance on how to prevent onward transmission is available at: Norovirus: What to do if you catch it and helping to stop the spread
Background
Norovirus transmission is influenced by many factors including, but not limited to, whether the person has been infected with norovirus recently, community contact patterns and the time of the year. Infections peak in the colder months and therefore norovirus is most prevalent during winter.
As most people recover quickly from norovirus infection, and do not need medical treatment, cases are rarely laboratory confirmed compared to other gastrointestinal infections such as salmonella. It has been estimated that for every case of norovirus reported to national surveillance in the UK there are about 288 in the community that go unreported, representing an annual burden of around 3 million cases (3). Norovirus is not a notifiable causative agent under Schedule 2 of the 2010 Health Protection (Notification) Regulations (4), which also contributes to the under-reporting to national surveillance.
Since the 2019/2020 season norovirus activity in England has been more variable compared to historical trends, likely due to multiple impacts of the COVID-19 pandemic. Throughout the 2019/2020 and 2020/2021 seasons a reduction in reporting to national surveillance was observed. Many of the non-pharmaceutical interventions (NPI’s) implemented to reduce COVID-19 transmission (enhanced environmental cleaning, isolation of symptomatic individuals, thorough hand washing etc) are also routinely used to control norovirus outbreaks (5). This resulted in a true drop in norovirus incidence while the measures were in place; however, following the staged relaxation of NPIs, unusual activity was observed in the 2021/2022 season, such as a greater proportion of norovirus outbreaks reported in educational settings than before the pandemic (6). In the 2022/2023 season, norovirus activity returned to pre-pandemic levels and in early 2023 norovirus reporting peaked at a level twice as high as that experienced in the decade prior to the emergence of COVID-19 (7), as predicted by modelling (8).
The most commonly detected norovirus genotype worldwide until 2023 was genogroup II, genotype 4 (GII.4). Historically, between 1995 and 2013 there have been five global GII.4 strain replacements events (9,10). Since the winter of the 2012/2013 season in England, the most frequently detected variants were Norovirus/GII.4/Sydney/2012 or GII.4/Sydney/2012-like variants (11). Following an unseasonal increase of norovirus laboratory reports in late spring 2024, further investigation determined the usual activity was associated with the emergence of genogroup 2, genotype 17 (GII.17) norovirus and a concurrent decrease in the GII.4/Sydney/2012 variants which had dominated since the 2012/13 season. This shift was also observed in the Unites States and several European countries including France, Germany and Austria (10,12). During the first 20 weeks of the 2024/2025 season, 66.3% of all norovirus-positive samples genotyped by the national reference laboratory (Enteric Virus Unit) were GII.17; of the total GII viruses, GII.17 now accounts for 76.0% and GII.4 only accounts for 10.0% (see Figure 2).
It is not possible to predict whether GII.17 has only transiently replaced GII.4 as the most commonly detected genotype and further work to understand this shift is underway. At present there is no indication that GII.17 causes more severe illness so the usual advice on how to prevent passing the infection on to others should be followed.
References
1. Sandmann FG, Shallcross L, Adams N, Allen DJ, Coen PG, Jeanes A and other (2018). Estimating the hospital burden of norovirus-associated gastroenteritis in England and its opportunity costs for non-admitted patients. Clinical Infectious Diseases: volume 67 number 5
2. UKHSA (2024). National norovirus and rotavirus surveillance reports: 2024 to 2025 season
3. Tam CC, Rodrigues LC, Viviani L, Dodds JP, Evans MR, Hunter PR and others (2012). Longitudinal study of infectious intestinal disease in the UK (IID2 study): incidence in the community and presenting to general practice.
4. The Health Protection (Notification) Regulations 2010.
5. Douglas A, Sandmann FG, Allen DJ, Celma CC, Beard S, Larkin L (2021). Impact of COVID-19 on national surveillance of norovirus in England and potential risk of increased disease activity in 2021.
6. UKHSA (July 2022). National norovirus and rotavirus bulletin 2020 to 2021: week 28 report.
7. UKHSA (March 2023). National norovirus and rotavirus bulletin 2022 to 2023: week 12 report.
8. O’Reilly KM and others (2021). Predicted norovirus resurgence in 2021-2022 due to the relaxation of non-pharmaceutical interventions associated with COVID-19 restrictions in England: a mathematical modelling study. BMC Medicine: volume 19 number 1, page 299.
9. Allen JA and others (2014). Emergence of the GII-4 Norovirus Sydney2012 strain in England, winter 2012-2013.
10. Zakikhany K, Allen DJ, Brown D (2012). Molecular evolution of GII-4 Norovirus strains.
11. Ruis C and others (2017). The emerging GII.P16-GII.4 Sydney 2012 norovirus lineage is circulating worldwide, arose by late-2014 and contains polymerase changes that may increase virus transmission.
12. Chhabra and others (2024). Increased circulation of GII.17 noroviruses, six European countries and the United States, 2023 to 2024.
Legionellosis in England and Wales: summary of 2023 annual report
A new report on legionellosis in residents of England and Wales reviews cases reported to the UKHSA’s National Enhanced Legionnaires’ Disease Surveillance Scheme (NELSS) from 2017 up to and including 2023, describing the epidemiological features of microbiologically-confirmed cases (1).
Of the nine UKHSA regions in 2023, the East and West Midlands regions recorded the joint-highest case rate of Legionnaires’ Disease (LD), with 1.2 cases per 100,000 population (95% CI: 0.9 to 1.5); the North East region recorded the lowest case rate of 0.6 cases per 100,000 population (95% CI: 0.4 to 1.0).
Following a decline in reported cases across all age groups during the COVID-19 pandemic period 2020 to 2021, incidence returned to pre-pandemic levels in 2023: a total of 604 confirmed cases were reported in that year (424 cases in males, 180 in females) compared with 338 cases in 2020, 352 in 2021, and 413 in 2022.
In 2023, 217 LD cases were reported in individuals aged 70 years and over, comprising 35.9% of reported cases; this was an increase of 99 cases compared with 2022 for this age group, and an increase compared with pre-pandemic levels.
Legionnaires’ Disease continues to be a significant contributor to preventable morbidity and mortality in England and Wales, with the majority of infections and deaths occurring among older adults. The age distribution of cases is markedly skewed toward individuals aged over 60, who remain the most affected demographic.
Despite the year-on-year increase in total cases in 2023, the report notes, a decrease in case fatality rate was observed; this is attributed to factors such as increased awareness of respiratory diseases following the pandemic and improvements in diagnostic testing. In contrast, a marked increase in CFR in 2020 is attributed to disruption to healthcare and diagnostic pathways during the pandemic.
The report highlights that the proportion of LD cases attributed to the three main exposure categories – community-acquired, foreign travel-related, and healthcare-associated – has been consistent in non-pandemic years. Unsurprisingly, incidence of travel-related cases fell dramatically during the pandemic period, as a result of travel restrictions, whereas community-acquired cases became more common during this period. This reflects changes in mobility and social behaviours rather that any inherent changes to disease or transmission patterns.
In 2023, of the total 604 confirmed cases reported, 379 (62.7%) were deemed to be community-acquired (a category which includes cases that may have been associated with travel within the UK) while 35 per cent of all cases (379) were associated with travel abroad. Thirteen cases (2.2%) were thought to have been healthcare-associated/nosocomial.
The most deprived areas of both England and Wales reported higher numbers of LD cases (according to the relevant indices of multiple deprivation). This deprivation-related divergence in incidence of cases was not explained by either tobacco smoking, diabetes or older age (the recognised risk factors), the report notes.
Reference
1. UKHSA (2024). Legionellosis in residents of England and Wales: 2017 to 2023 report
ESPAUR annual report in summary
The annual English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) report, published by the United Kingdom Health Security Agency (UKHSA) on 14 November (1), covers activity up to March 2024 and data on resistances and usage to the end of 2023. Key findings of the eleventh report as follows.
Antibiotic resistance
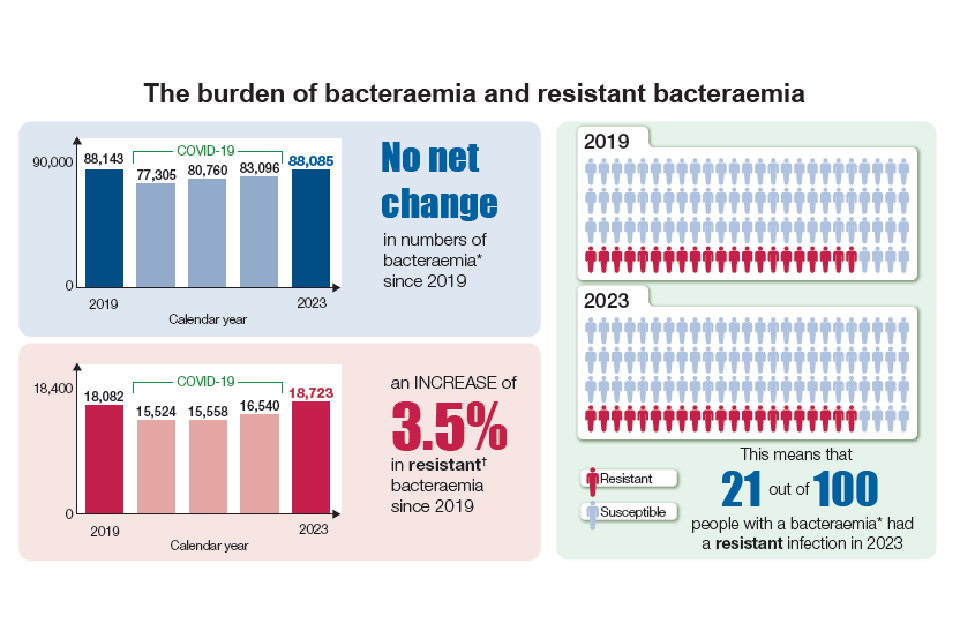
In 2023, antibiotic resistant bacteria identified from blood samples (bacteraemia) surpassed pre-pandemic levels in 2019.
The latest national surveillance data analysing pathogens of public health importance due to antimicrobial resistance show that an estimated 18,723 people in England had an antibiotic-resistant bacteraemia in 2023 – a rise of 3.5% since 2019 (18,082). An estimated 2,041 deaths occurred in people within 30 days of having an antibiotic-resistant bacteraemia in 2023. The proportion of bloodstream infections that are resistant to one or more antibiotics – 1 in 5 – has remained stable since 2019.
There is considerable regional and demographic variation in England. People living in the most deprived areas (measured by the Index of Multiple Deprivation) had a higher rate of resistant bacteraemia compared to the least deprived group, and the resistant bacteraemia rate was 42.6% higher for those living in the most deprived areas compared to the least deprived areas, which has increased compared 2019 (a 29.4% higher rate in the most deprived compared to the least deprived). Asian or British Asian people were more likely to acquire antibiotic-resistant bacteraemia than other ethnic groups.
Antibiotic usage
The UK’s National Action Plan (NAP) for AMR 2019 to 2024 set a UK-wide target to reduce antimicrobial consumption from 2014 baseline by 15% by 2024. There was a 2.4% increase in total antibiotic use in England between 2022 and 2023, although this did remain 1.9% below pre-pandemic levels in 2019. This highlights the need for continued efforts to reduce inappropriate antibiotic use.
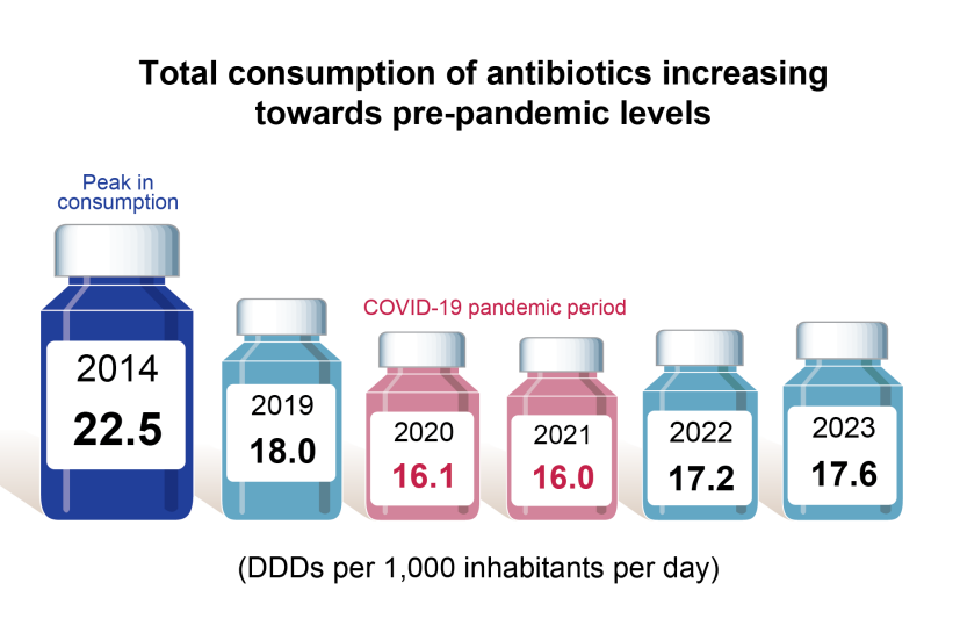
As seen over the past five years, primary care accounts for the majority of all antibiotics prescribed, at approximately 80%. In 2023, 79.7% of all antibiotics used were consumed in primary care. Despite a decreasing trend during the COVID-19 pandemic, there was an increase of 2.3% (from 1.66 to 1.70 items per 1,000 inhabitants per day) in primary care antibiotic usage between 2019 and 2023, emphasising the need for continued AMS efforts. Antibiotic prescribing continued to be greatest within the general practice setting (71.7%).
The sixth national point-prevalence survey (PPS) on healthcare-associated infection (HCAI) was carried out. Overall prevalence of HCAI was 7.6%, with the most common types of HCAI being pneumonia or lower respiratory infections (29.6%).
In financial year 2023/24, 20% (30/132) of NHS England acute trusts achieved the NHS Standard Contract target to reduce antibiotic prescribing from WHO ‘Watch’ and ‘Reserve’ categories adapted for England by 10% from their 2017 baseline.
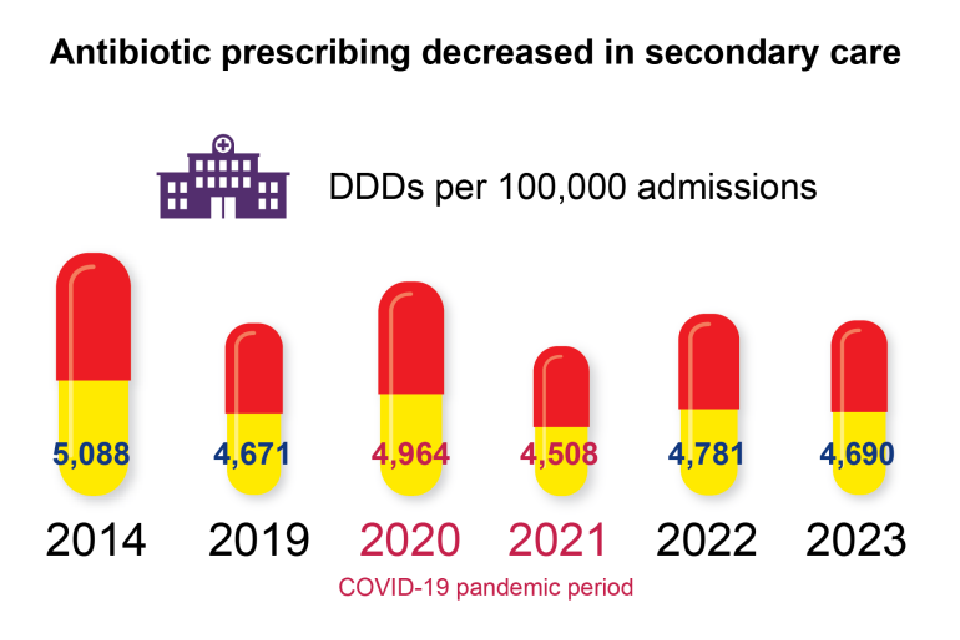
Secondary care consumption rates are measured using defined daily doses (DDDs) per 1,000 hospital admissions. Antibiotic use in secondary care surpassed 2019 levels in 2023 by 0.4% (from 4,671 to 4,690 DDDs). There was however a decrease of 1.9% in overall antibiotic use in secondary care between 2022 and 2023 (from 4,781 to 4,690 DDDs per 1,000 admissions).
Systemic antifungal use in 2023 was similar to that seen in 2019 (+0.06%) after having decreased significantly in 2020, the first year of the COVID-19 pandemic.
Antibiotic stewardship
The Treat Antibiotics Responsibly, Guidance, Education and Tools (TARGET) website saw the number of views almost double in November 2023 compared to the previous month, coinciding with the TARGET promotional campaign and World Antimicrobial Resistance Awareness Week. The significant increase in visits to the TARGET website post campaign highlights the importance of reminding and raising awareness of antimicrobial stewardship among heathcare professionals. An example of this would be raising awareness of stewardship tools and resources available to primary care clinicians on RTIs before the winter.
A systematic review evaluating IVOS criteria for paediatric patients and a 2-step modified-Delphi were undertaken. The new national criteria and sample decision aid were published in June 2024.
The UK-specific Access, Watch and Reserve antibiotic medicines classifications have also been updated to ensure they remain relevant for the needs of healthcare professionals in the UK. A 4-step modified Delphi process was used to gain consensus from a panel of experts. This led to 16 antibiotics differing in classification when compared to classifications based on the 2023 World Health Organization classifications and the proposed UK adapted indexes. Further discussions are underway to consider the policy implications from the proposed list.
Professional and Public Education, Engagement and Training
In 2024, the Antibiotic Guardian campaign is celebrating 10-years since its inception. The campaign surpassed 100,000 pledges in 2020 and received 177,681 pledges made via the main website page and >200,000 pledges from all the Antibiotic Guardian collaboration pages by the end of 2023.
Reference
1. UKHSA (2024). ‘English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) report’.
GRASP and MARS annual reports published
UKHSA has published its annual Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) report, presenting the latest data on antimicrobial resistance in Neisseria gonorrhoeae in England and Wales (1).
Between 2022 and 2023 Neisseria gonorrhoeae isolates collected through Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) showed:
- no cases of ceftriaxone resistance (minimum inhibitory concentration (MIC) >0.125 milligrams per litre (mg/L))
- an increase in reduced susceptibility (MIC >0.03 mg/L) to ceftriaxone, the current first-line therapy, from 0.21% (3 out of 1,460) in 2022 to 0.91% (16 out of 1,762) in 2023
- the modal MIC for ceftriaxone remained at 0.015 mg/L overall and across sexual orientation groups after the modal MIC for isolates from heterosexual men and women increased to equal that from gay, bisexual and other men who have sex with men (GBMSM) in 2022
- cefixime resistance (MIC >0.125 mg/L) is at 5.6% in 2023
- ciprofloxacin resistance (MIC >0.06 mg/L) remained unchanged at 58.6%
- tetracycline resistance (MIC >0.5 mg/L) remains high from 84.1% to 80.1%
- penicillin resistance (MIC >1.0 mg/L) remained stable from 13.6% to 14.3%
- as in previous years, no spectinomycin resistance was detected
- azithromycin MICs in 2023 have not been presented due to a laboratory technical issue
Whole genome sequencing of GRASP isolates showed:
- over three-quarters of the 2023 isolates belonged to only 13 multi-locus sequence types that also dominated in 2022
- resistance determinants associated with reduced susceptibility to cephalosporins and resistance to ciprofloxacin were mainly detected in isolates belonging to the 13 dominant multi-locus sequence types
- reduced susceptibility or resistance to cefixime (MIC 0.06 to 0.5 mg/L) and reduced susceptibility to ceftriaxone (MIC 0.015 to 0.06 mg/L) were associated with the expression of mosaic penA alleles, notably penA-34 and penA-93
- amino acid alterations in GyrA and ParC mediated resistance to ciprofloxacin were highly concordant with phenotypic testing
- high levels of resistance to tetracycline (MIC >8 mg/L) and penicillin (MIC >1 mg/L) were associated with the acquisition of the plasmid-mediated genes encoding Tet(M) and TEM b-lactamase, penicillinase, respectively
- only 1.6% of isolates had A2059G or C2611T mutations in the 23S ribosomal ribonucleic acid (rRNA) gene, associated with higher azithromycin MICs (2 to 256 mg/L)
No cases of ceftriaxone resistance were detected in GRASP. However, outside of the sentinel surveillance system, 23 cases of ceftriaxone resistance have been detected since the start of 2022, totalling 32 cases detected in England since the first case, detected in 2015. Six of these recent cases were also extensively drug-resistant (XDR), with high levels of resistance to the second line treatment (azithromycin) as well as other antimicrobials.
Prescribing data demonstrated excellent adherence to the UK guideline for managing infection with N. gonorrhoeae, with 97.9% of individuals receiving the recommended first-line of ceftriaxone 1g intramuscular (IM) monotherapy in 2023.
The effectiveness of first-line treatment for gonorrhoea continues to be threatened by antimicrobial resistance. While ceftriaxone-resistant cases continue to have travel links with the Asia-Pacific region, some cases appear to have acquired infection in the UK and, as not all partners could be contacted, undetected transmission within England is possible.
To note, a laboratory technical issue has been identified with susceptibility testing for cefixime and azithromycin affecting data as early as 2018. Please see technical notes for further details on cefixime and azithromycin.
Sexual health services should report cases of suspected treatment failure to UKHSA via the online HIV and STI Data Exchange.
The Mycoplasma genitalium Antimicrobial Resistance Surveillance (MARS) report has also been published (2). M. genitalium is a sexually transmitted pathogen that causes non-gonococcal urethritis (NGU) and is associated with cervicitis and pelvic inflammatory disease (PID). In 2023, the MARS programme included 928 M. genitalium specimens with linked demographic and clinical data. These showed:
- macrolide resistance of 62.2%
- fluoroquinolone resistance of 12.1%
- dual macrolide and fluroquinolone resistance of 10.1%
- most (89.6%) individuals were prescribed the recommended first or second-line treatments of azithromycin (a macrolide) or moxifloxacin (a fluoroquinolone)
- over three-quarters of individuals received doxycycline (a tetracycline) as a pre-treatment
- a high treatment success rate (95.4%) was observed with azithromycin in those with a macrolide susceptible M. genitalium infection
- a high treatment success rate (98.3%) was also seen with moxifloxacin in those with a fluoroquinolone susceptible M. genitalium infection
References
1. UKHSA (2024). ‘Gonococcal resistance to antimicrobials surveillance programme (GRASP) report’
2. UKHSA (2024). ‘Mycoplasma genitalium Antimicrobial Resistance Surveillance (MARS) report: 2023’
Update on lead exposure in children in England: 2023 cases
Lead is a persistent, heavy metal environmental contaminant that has an adverse effect on the body even at low blood lead concentration. There is no known safe threshold for lead exposure and children and the foetus (and, therefore, pregnant women) are particularly vulnerable to harmful effects. Since 2010 a surveillance system has been in place for formal notification to UKHSA from collaborating laboratories of children under 16 years and pregnant women with elevated blood lead.
The seventh annual report of data from the Lead Exposure Public Health Intervention and Surveillance (LEPHIS) group within UKHSA has now been published (1). The report summarises the cases reported to UKHSA, from 1 January to 31 December 2023, of children 0 to 15 years with an elevated blood lead concentration ≥0.24μmol/L (equivalent to ≥5μg/dl) who require public health intervention to identify and remove the exposure sources. For the first time, this report includes data collected from the Enhanced Surveillance Questionnaires (ESQ) that are used by HPTs as part of case management to gather information on potential risk factors and lead exposure sources.
A total of 226 cases met the case definition and were notified to UKHSA in 2023. The key findings are that:
- the majority of cases (78%) were directly notified through the surveillance system by participating laboratories; 22% were notified through other routes which is similar to previous years
- the average detection rate for England in 2023 was 21 cases per million children aged 0 to15 years, although there was significant regional variation
- the number of cases reported to LEICSS are significantly lower than the estimated incidence of lead exposure in children in England based on international population survey data
- cases are typically 1 to 4 years of age (67%), male (65%), and a significant proportion from the most deprived areas (48%)
- the most common associated reported exposures (236 completed ESQs out of 507) (2) from 2021 to 2023 were soil (67%,157 cases) and paint (44%, 103 cases) and majority of cases exhibited pica behaviour (194, 82%) and learning difficulties (162, 69%)
The main messages and recommendations include that:
- children exhibiting pica or other hand-to-mouth behaviour in environments with lead hazards are at the highest risk of exposure
- clinicians should be aware of: the risk of lead exposure for children, the main sources of lead exposure, children most at risk, presenting symptoms and signs of exposure
- cases who meet the case definition should be notified to UKHSA health protection teams for active public health case management
The LEPHIS group aims to increase prevention activities and raise awareness of the hazard with laboratories, clinicians and parents across England. For more information, details of LEPHIS group activities, please contact epht@ukhsa.gov.uk
Reference/note
1. Lead Exposure in Children Surveillance System (LEICSS) annual report, 2024.
2. Case management requires cases with a BLC ≥0.48 μmol/L (equivalent to ≥10 μg/dL) to complete an ESQ.
Vaccine coverage reports in this issue
RSV vaccine coverage report in older adults for catch-up cohorts in England: October 2024
Infection reports
Laboratory confirmed cases of invasive meningococcal infection in England: April to June 2024
Laboratory surveillance of paediatric BSI and antimicrobial resistance (England) 2018 to 2022
Laboratory surveillance of fungaemia due to yeasts in England: 2023
Chemical and environmental hazards report
Lead Exposure in Children Surveillance System (LEICSS) annual report, 2024
