HPR volume 19 issue 3: news (27 and 31 March 2025)
Updated 31 March 2025
Increase in Candidozyma (Candida) auris reports in England, linked to hospital outbreaks
Candidozyma (Candida, C.) auris is a rapidly emerging fungal pathogen with a global distribution. First described in 2009, it has now been identified across six continents, and in over 60 countries worldwide (1). C. auris can result in colonisations (presence without signs and symptoms of infection) and infections (including invasive infections causing severe disease). It is a cause of outbreaks within healthcare settings. Resistance has developed to many available classes of antifungal treatments, including the first-line antifungal agent fluconazole. C. auris can also acquire resistance to other antifungal agents during therapy (1). Invasive infection has been associated with significant mortality in non-UK settings. The World Health Organization has categorised C. auris as a critical priority fungal pathogen (2).
The UK Health Security Agency (UKHSA) is working with NHS England and other partners to respond to increasing detections of C. auris in hospitals. C. auris, previously rarely detected in England, has been emerging over the last decade, particularly following the lifting of travel restrictions imposed during the COVID-19 pandemic period. C. auris is identified through clinical samples from patients (such as when infections are suspected) or surveillance swabs (such as screening of patients on admission to hospital or when screening is implemented relating to outbreaks). Antifungal susceptibility testing to inform patient management/treatment may be performed locally, or via specialist and reference laboratories.
Between January 2013 and December 2024 inclusive, a total of 637 C. auris cases (including both colonisations and infections) were reported across multiple regions of England (of which 178 were reported in 2024; see Figure 1). Since January 2023, most cases have been reported from the UKHSA London and South-East regions (199 and 46 cases respectively; see Figure 2). There is likely to be significant under-detection of cases due to incomplete reporting, coupled with a lack of routine screening and non-identification of Candida to species level in many settings. Most detections of C. auris represent colonisation rather than infection (though colonisations can lead to subsequent infections). C. auris can cause a wide variety of infections in adult, paediatric and neonatal populations; these range from superficial (mild) skin infections, to severe infections in normally sterile sites such as blood, bone, internal organs, and cerebrospinal fluid.
Figure 1. Number of patients with first detections of C. auris, England, January 2013 to December 2024 (and whether isolated from blood or other body site)
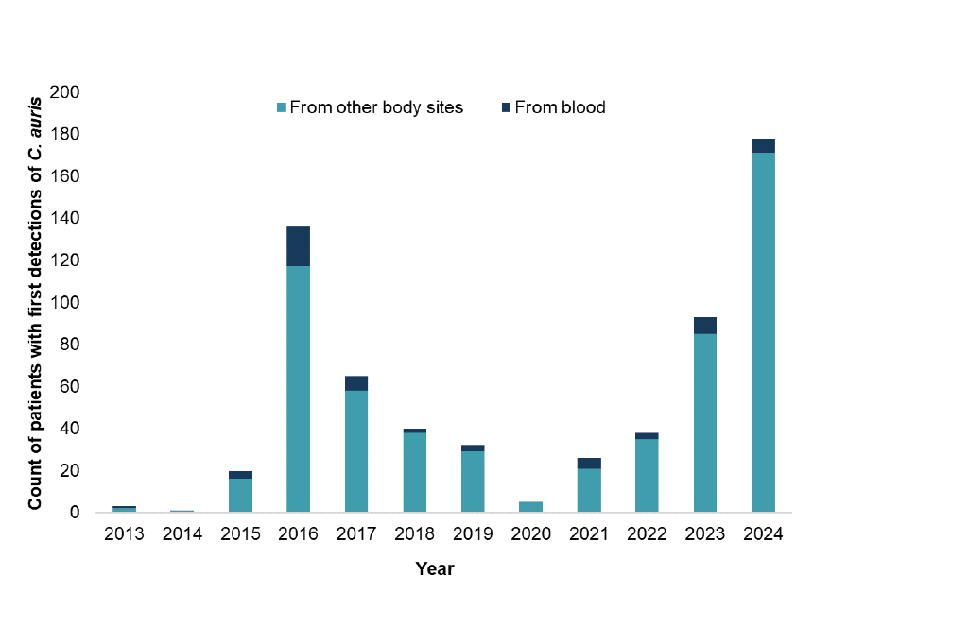
Several prolonged C. auris outbreaks have occurred in UK hospitals since 2015, requiring interventions to control them and prevent further spread. Peaks in detections over time have been largely attributed to these. There have been significant healthcare associated outbreaks affecting two NHS Trusts in London and the south of England respectively, from 2023 to date. Hospital outbreaks can be disruptive and costly due to the substantial service disruption resulting from measures put in place to reduce risk to patients and to control transmission.
Following public consultation, UKHSA published revised ‘Guidance for the laboratory investigation, management, and infection prevention and control of Candidozyma auris (formerly Candida auris)’. The guidance has been updated in line with the latest available evidence from published literature (1), international best practice, and expert consensus, alongside national surveillance.
From April 2025, C. auris will be considered a notifiable organism (causative agent) under Schedule 2 of the Health Protection (Notification) Regulations 2010. This means that laboratories that test human samples in England will be required to report C. auris cases to UKHSA. This change aims to strengthen surveillance and inform public health response to this organism. Reporting to date has been on a voluntary basis.
Figure 2. Number of patients with first detections of C. auris by UKHSA region in England, January 2023 to December 2024

UKHSA is requesting that laboratories include C. auris (all isolates, including colonisations and infections) as part of routine reporting, and that clinicians notify UKHSA Health Protection Teams promptly if they suspect an outbreak.
Healthcare professionals working in the acute NHS and independent healthcare sector settings in England, especially Infection Prevention and Control (IPC), microbiology, infection, and laboratory specialists, are asked to familiarise themselves with the revised C. auris guidance and develop local policies and guidance accordingly.
Organisations with C. auris cases or experiencing outbreaks are expected to share information proactively with their local UKHSA Health Protection Team, and relevant NHS and independent hospitals and organisations (including commissioners, providers, and regulatory bodies as appropriate) within their locality and referral networks. Prompt information sharing is important for risk assessment, coordination of public health response, and to enable hospitals to initiate measures such as screening to detect cases early and IPC interventions to prevent spread.
UKHSA will continue to work with the NHS and partners to closely monitor C. auris and put in place measures to reduce risks to patients and the public.
References
1. Jones CR, Neil C, Borman AM, Budd EL, Cummins M, Fry A, and others (2024). ‘The laboratory investigation, management, and infection prevention and control of Candida auris: a narrative review to inform the 2024 national guidance update in England’. Journal of Medical Microbiology: volume 73, number 5
2. WHO (2022). ‘Fungal priority pathogens list to guide research, development and public health action’
Infection reports in this issue
Laboratory confirmed cases of measles, mumps and rubella in England: October to December 2024
Laboratory-confirmed cases of invasive meningococcal infection in England: July to September 2024
Group A streptococcal infections: second update on seasonal activity in England, 2024 to 2025
Gastrointestinal infections in England: 2022 to 2024
Travel-associated infections in England, Wales and Northern Ireland: 2024
Vaccine coverage
RSV vaccine coverage report in older adults for catch-up cohorts in England: February 2025
RSV maternal vaccination coverage in England: November 2024
Pneumococcal polysaccharide vaccine (PPV): coverage report, England, April 2023 to March 2024
