HIV Action Plan monitoring and evaluation framework 2022 report
Updated 17 February 2025
Applies to England
Report summarising progress from 2019 to 2021 .
Foreword
It is exactly one year since the HIV Action Plan for England 2022 to 2025 was published. The goals set were ambitious: to reduce HIV transmission by 80% and AIDS diagnoses and HIV-related, preventable deaths by 50% between 2019 and 2025.
In 2020, the coronavirus (COVID-19) pandemic impacted on the delivery and the public health progress to tackle the HIV epidemic. Numbers having an HIV test fell and the number of people living with diagnosed HIV but not in contact with HIV services doubled.
The 2021 data has shown positive signs of recovery, but that recovery is uneven. The number of all people with diagnosed HIV infection and in care who were treated and virally suppressed remained extremely high between 2019 and 2021. Among gay, bisexual and other men who have sex with men (GBMSM), transmission continues to fall and these individuals are getting more HIV tests than ever and the estimated numbers of undiagnosed HIV infection continue to fall. However, the number of heterosexuals having an HIV test remains below pre-COVID-19 levels, the estimated number of undiagnosed HIV infection has not fallen and late HIV diagnoses are rising.
This first Monitoring and Evaluation Framework report tracks the progress towards the HIV Action Plan ambitions. This framework sets out 5 key themes with accompanying indicators to measure the HIV Action Plan’s success across the continuum of care. These indicators will allow us to not only track progress across HIV activities, but also to identify where intensive efforts are needed to work with specific populations and geographic regions. If we are to meet the 2025 ambitions, we need to reduce the number of individuals diagnosed with HIV in England by 360, diagnosed with AIDS by 16 and HIV-related preventable deaths by 44, each year, from 2022 onwards.
The ambition to end HIV transmission remains feasible and we have the tools and knowledge to achieve this goal. As we continue to recover from the impact of COVID-19 on the HIV epidemic, it is vital that we exceed pre-pandemic levels of HIV testing, partner notification, pre-exposure prophylaxis (PrEP) and retention in care. Equally important is our work to ensure public health interventions are culturally competent and accessible across the diverse population living with HIV and people at risk of acquiring HIV.
I commend this work to present indicators to improve the end-to-end delivery of care and look forward to monitoring the excellent progress over the coming years.
Susan Hopkins
Chief Medical Adviser
Results at a glance
This first edition of the monitoring and evaluation framework measures progress towards achieving England’s long-term commitment to zero new HIV transmissions by 2030. It specifically focuses on the interim ambitions of England HIV Action Plan 2022 to 2025 to reduce HIV transmission (by 80%), AIDS diagnoses (by 50%) and HIV related preventable deaths (by 50%) between 2019 and 2025. This report provides a public health commentary around progress towards these interim targets, the results of which are presented in Table 1.
Table 1. Summary table of progress towards interim ambitions in 2025
| HIV Action Plan indicators | 2019 baseline | 2020 | 2021 | Percentage change (2019 to 2021) |
|---|---|---|---|---|
| Number of new HIV diagnoses first made in England | 2,986 | 1,987 | 2,023 | -32% |
| Number of people diagnosed with AIDS | 216 | 169 | 171 | -21% |
| Estimated number of HIV-preventable deaths | 233.6 | 325.6 | 289.2 | +24% |
| UNAIDS 95 95 95 targets | 94%-98%-97% | 95%-99%-98% | 95%-99%-98% | Not applicable |
This report also provides an overview of progress in relation to 5 key HIV themes. These themes and key indicators are briefly summarised in Table 2.
Table 2. Summary of 5 HIV themes and selected indicators
| Theme 1: maintain people’s HIV negative status | 2019 | 2020 | 2021 |
|---|---|---|---|
| Number of people attending sexual health services (SHSs) due to HIV partner notification | 1,558 | 850 | 820 |
| Number of people attending through HIV partner notification who tested | 1,397 | 702 | 620 |
| Ratio of HIV partner notification contacts tested per diagnosis – a ratio of 1 suggests each HIV diagnosis results in at least one partner having a test | 1.007 | 0.846 | 0.76 |
| Proportion of all HIV negative individuals accessing specialist SHSs categorised as having a pre-exposure prophylaxis (PrEP) need | Not applicable | Not applicable | 7% |
| Proportion of all HIV negative individuals with estimated PrEP need who had this need identified | Not applicable | Not applicable | 79% |
| Proportion of all HIV negative individuals with estimated PrEP need who started or continued PrEP | Not applicable | Not applicable | 70% |
| Theme 2: reduce the number of people living with HIV who are undiagnosed | 2019 | 2020 | 2021 |
|---|---|---|---|
| Estimated number of people living with undiagnosed HIV | 5,600 (95% CrI 4,100 to 7,900) | 4,700 (95% CrI 3,600 to 6,500) | 4,400 (95% CrI 3,500 to 6,100) |
| Number of people HIV tested in all SHSs | 1,319,915 | 913,383 | 1,053,169 |
| Number of people HIV tested in specialist SHSs | 1,000,598 | 465,781 | 478,203 |
| Number of eligible people offered a test in specialist SHS | 1,296,276 | 635,301 | 648,923 |
| Number of people declining a test in specialist SHS | 295,678 | 169,520 | 170,720 |
| Number of people who had tested at least once in the year before their most recent test in specialist SHS – GBMSM | 56,054 | 38,685 | 36,094 |
| Late diagnosis in those first diagnosed in England | 857 | 667 | 754 |
| Number of people tested in emergency departments (ED) in higher HIV prevalence areas | 115,349 | 90,677 | 98,919 |
| Reactive tests (rates) in ED in higher HIV prevalence areas | 630 (0.5%) | 543 (0.6%) | 602 (0.6%) |
| Theme 3: reduce the number of people with transmissible levels of virus | 2019 | 2020 | 2021 |
|---|---|---|---|
| Estimated number of people living with transmissible levels of virus in England | 12,932 | 12,184 | 11,985 |
| Number of people not linked to care within calendar year of diagnosis | 342 | 259 | 147 |
| Number of people on treatment and no evidence of viral suppression | 3,608 | 1,222 | 2,762 |
| Number of people not linked to care within 15 days of HIV diagnosis | 1,910 | 1,357 | 1,525 |
| Number and proportion of people starting treatment within 90 days of diagnosis | 2,279 | 1,446 | 1,538 |
| Number of people seen for HIV care and not on treatment | 1,627 | 1,119 | 1,195 |
| Number (%) of people treated who are not virally suppressed (viral load over 200 copies) | 2,096 (2.4%) | 1,874 (2.2%) | 1,799 (2.0%) |
| Number (%) of people not attending care for at least 15 months (“not retained in care”) | 2,519 | 4,980 | 4,444 |
| Theme 4: manage and prevent co-morbidities and HIV-related conditions in people living with HIV |
|---|
| Under development |
| Theme 5: improve quality of life and reduce HIV stigma |
|---|
| Under development |
Main messages
England has a long-term commitment to zero HIV transmissions by 2030. This first report of the monitoring and evaluation framework measures progress towards the interim ambitions set by England’s HIV Action Plan 2022 to 2025 to reduce HIV transmission (by 80%), AIDS diagnoses (by 50%) and HIV-related, preventable deaths (by 50%) between 2019 and 2025. It also sets out 5 key themes with accompanying indicators to measure the progress that must be achieved if the ambitions of the HIV Action Plan are to be realised. Each theme covers a specific aspect of HIV prevention and care. These indicators are previously published and have been taken from existing data sources. Future indicators will be developed with the HIV Action Plan Steering Group and other stakeholders. This report presents progress at the national level. Future reports will focus on inequalities between population groups and regions of residence for each indicator. An interactive tool will be developed to allow local experts to track progress and inequalities.
The baseline for the HIV Action Plan was 2019; however, during 2020 and 2021, the COVID-19 pandemic impacted the HIV epidemic in several ways. Public health measures to control COVID-19 altered patterns of sexual behaviour and reduced the number of people accessing HIV testing services during the first year of the COVID-19 pandemic. Among people living with diagnosed HIV, the proportion of consultations that were virtual rose and fewer people had CD4 and viral load counts reported.
Progress towards reducing HIV transmission, AIDS and HIV-related, preventable deaths by 2025
New HIV diagnoses first made in England fell by 32% from 2,986 in 2019 to 1,987 in 2020, but numbers plateaued in 2021 (2,023). The number of HIV diagnoses first made in England among GBMSM reduced among GBMSM living in London from 550 in 2019 to 247 in 2020 to 204 in 2021; equivalent figures outside London were 712 in 2019, 452 in 2020 and 517 in 2021, respectively. The fall in new HIV diagnoses first made in England in GBMSM, which occurred in the context of high numbers testing for HIV, suggests a fall in incidence. A CD4 back calculation model supported an 80% probability of a decline in incidence between 2019 to 2021 in this population.
Among women exposed by heterosexual contact, new HIV diagnoses first made in England decreased by 32% from 576 in 2019 to 392 in 2020 but rose by 9% to 429 in 2021. New HIV diagnoses first made in England among men exposed by heterosexual contact decreased by 31% from 533 in 2019 to 367 in 2020 and remained stable at 369 in 2021. Among heterosexual adults, in whom HIV testing has not recovered to pre-COVID-19 levels, this indicates no evidence of a fall in HIV incidence. To achieve the 2025 ambition of 600 new HIV diagnoses, a decrease of approximately 360 diagnoses per year is required from 2022 onwards.
The number of AIDS cases within 3 months of diagnosis in 2021 has fallen by 21% (to 171) compared with 2019. The number of AIDS cases within 3 months of diagnosis would need to reduce by 16 cases per year from 2022 onwards if the 2025 ambition (under 110) is to be achieved.
There were 723 deaths in people with HIV in 2021, a 24% rise compared with 584 in 2019. It is likely that the rise in deaths was partly driven by improved ascertainment of deaths resulting from the National HIV Mortality Review together with additional deaths due to COVID-19. The number of deaths in 2020 and 2021 were most pronounced in the months with the highest numbers of COVID-19 deaths, indicating the rise in deaths unlikely to be HIV related. Assuming 40% of deaths are HIV related and preventable, corresponding to 289 for 2021, a reduction of 44 HIV-related deaths per year from 2022 onwards is needed to meet the 2025 ambition. Application of a pan-European definition of HIV-related, preventable mortality to replace the estimate of 40% all-cause deaths will allow evaluation of progress towards the target.
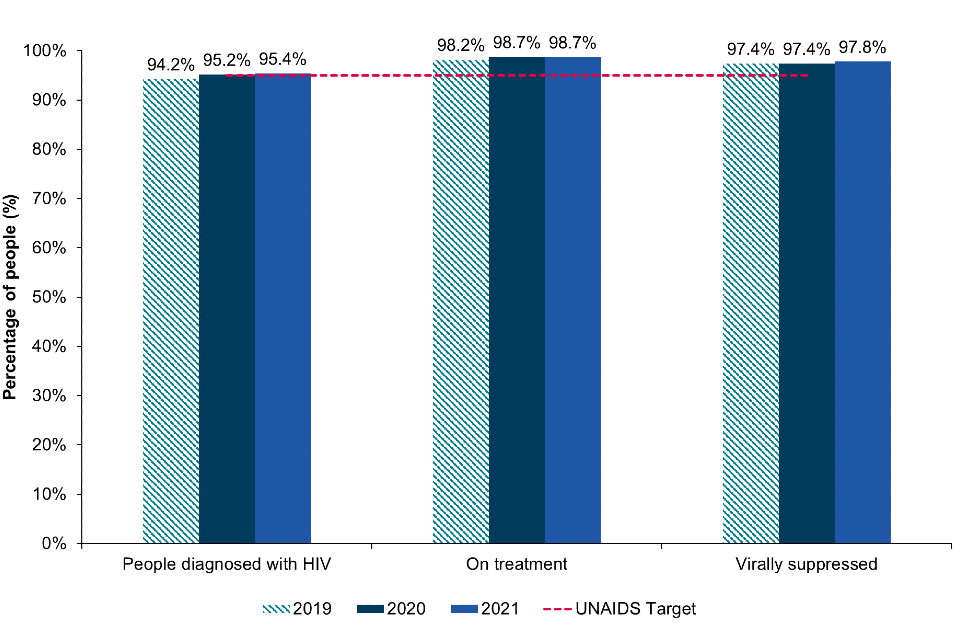
In 2021, England has met the UNAIDS 2025 targets for the second time with 95% of all people with HIV being diagnosed, 99% of those diagnosed on treatment and 98% of those on treatment being virally suppressed and unable to pass on the virus.
Theme 1: maintain people’s negative HIV status
Partner notification, pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) maintains the status of people who are HIV negative (HIV testing is detailed in Theme 2). Between 2019 and 2021 the number of people attending Sexual Health Services (SHSs) due to partner notification decreased from 1,558 to 820, among whom the proportion testing positive was 3.8% in 2019, and 2.6% in 2021. Despite a decrease in service provision in response to COVID-19, HIV partner notification remains an effective way to reduce the number of people with undiagnosed HIV and to stop HIV-negative people acquiring HIV.
In 2021, 7% (87,828 of 1,180,923) of HIV-negative people accessing specialist SHSs in England were defined as having PrEP need, of whom, 70% (61,092) initiated or continued PrEP. However, substantial variation exists in relation to need and uptake by population group. London residents, GBMSM and people over 35 years old were more likely to have PrEP need, have PrEP need identified, and initiate or continue PrEP compared to the rest of England, and other exposure groups and younger populations. In 2021, 8,115 people received PEP for HIV, a 33% decrease compared with 2019 (12,038).
Theme 2: reduce the number of people living with HIV who are undiagnosed
Reducing undiagnosed HIV infection through HIV testing not only provides access to treatment that saves lives but means people who obtain undetectable levels of virus cannot pass on HIV. Of the estimated 95,900 (credible interval (CrI) 94,700 to 97,700) people living with HIV in 2021, an estimated 4,400 (95% CrI 3,500 to 6,100) were undiagnosed in 2021, compared with 4,700 (95% CrI 3,600 to 6,500) in 2020 and 5,600 (95% CrI 4,100 to 7,900) in 2019. In 2021, the number of people living with undiagnosed HIV infection was 1,300 (95% CrI 1,000 to 1,900) in London, compared to 3,000 (95% CrI 2,300 to 4,400) elsewhere in England (numbers do not add up due to rounding).
In 2021, across all SHSs, 1,053,169 people received an HIV test, a 20% reduction compared to 2019 (1,319,915). However, the number of GBMSM testing increased 14% since 2019, from 156,631 to 178,466 in 2021. Conversely, among heterosexual men and heterosexual and bisexual women, a 41% (419,501 to 248,355) and 22% (628,607 to 471,831) reduction in numbers testing was seen respectively, in the same period.
The proportion of people declining an HIV test remained stable at 19% in 2019, to 16% in 2021. GBMSM were least likely to decline a test (3%) compared with heterosexual men (12%) and women (22%).
Theme 3: reduce the number of people with transmissible levels of virus
For people diagnosed with HIV, rapid linkage to care and treatment, and subsequent retention in care (and re-engagement in care where necessary) will reduce the number of people living with a detectable viral load, thereby improving health and reducing onward transmission.
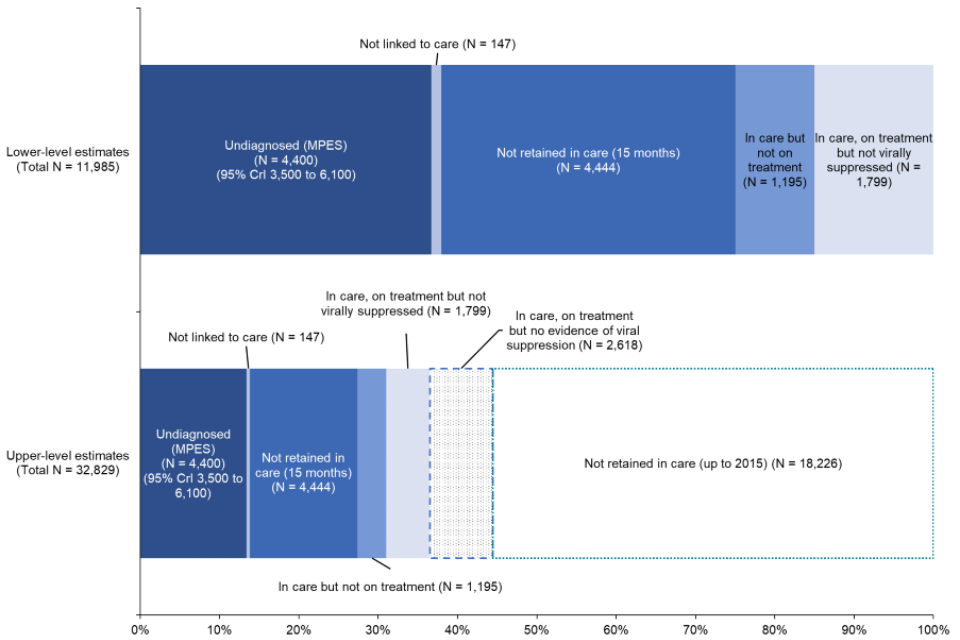
In 2021, a lower-level estimate of 11,985 people living with HIV had transmissible levels of virus in 2021, equivalent to 12% to 14% of the 95,900 (CrI 94,700 to 97,700) people living with HIV.
Among the 11,985, 37% (4,400) were undiagnosed, 1% (147) were diagnosed but not linked to care, 37% (4,444) were not retained in care (more than 15 months since last appointment between October 2019 and September 2020), 1,195 (10%) attended care in 2021 but not on antiretroviral therapy (ART), 15% (1,799) were on treatment but not yet virally suppressed (viral load under 200 copies per mL).
A higher-level estimate for the number of people living with transmissible levels could reach up to 32,829 in 2021 when including 2,618 people on treatment with no evidence of viral suppression and an additional 18,226 people not retained in care (more than 15 months since last appointment between January 2015 and October 2019).
Theme 4: manage and prevent HIV related conditions and co-morbidities
HIV-associated stigma remains a significant factor in people’s experience of living with HIV and reduces access to testing and healthcare. Improving the quality of life for people with long-term conditions is a long-standing goal for the NHS and wider health and care system. The most recent UNAIDS targets has set an ambition for under 10% of people with HIV to experience stigma. Future work with key stakeholders and the HIV community will develop indicators to monitor quality of life and stigma.
Conclusion
There is much to celebrate in the progress made to end HIV transmission with under 4,500 people living with undiagnosed HIV infection and extremely high levels of antiretroviral therapy coverage and viral suppression. However, progress made towards the interim ambitions as set out in the HIV Action Plan has been adversely impacted by COVID-19. If we are to meet the interim ambitions, the following areas must be prioritised: PrEP access for all groups, partner notification scaled up, and HIV testing numbers exceeding levels seen in 2019 among heterosexual men and women; further efforts to make sure those not retained in care are re-integrated and supported; understanding and measuring stigma, in all its forms to improve the quality of life of people living with HIV and ensure good health outcomes; and, monitoring inequalities in HIV prevention and care to inform accessible and culturally-competent interventions.
Introduction
On 1 December 2021, England’s government published an HIV Action Plan, an initiative which sets out the activities that need to be undertaken to meet England’s long-term commitment to zero new HIV transmission by 2030 (1). England is well placed to achieve this. New HIV diagnoses first made in England have decreased since 2015, particularly in GBMSM, due to high sustained levels of HIV testing (including frequent repeat testing), the availability and effectiveness of PrEP, the effectiveness of treatment as prevention (TasP) and excellent care provision by the NHS. In addition, since 2020 (2), England has met the UNAIDS 2025 targets (3) of 95% of all people with HIV being diagnosed, 95% of those diagnosed on treatment and 95% of those on treatment being virally suppressed and so unable to pass on the virus.
The interim ambitions of the England’s HIV Action Plan 2022 to 2025 (1) aimed to reduce the following between 2019 (baseline data for the HIV Action Plan) and 2025:
- number of people first diagnosed with HIV in England by 80%
- number of people diagnosed with AIDS within 3 months of an HIV diagnosis by 50%
- HIV preventable deaths in England by 50%
- HIV-related stigma
Achieving these interim ambitions is crucial if England is to achieve its commitment of zero new HIV transmission by 2030. This first report for the monitoring and evaluation framework measures progress towards achieving these interim ambitions and collates key HIV indicators.
This monitoring and evaluation framework focusses on the national picture. Future reports will provide regular updates as well as data stratified by key populations and geographical regions. This will allow any inequalities between populations and regions to be identified and addressed. Tracking inequalities is essential to end HIV transmission since the accessibility of healthcare services differs by population, and progress overall may mask broadening inequalities for specific groups. An interactive care pathway tool will be developed to allow local experts to track progress and inequalities. Working with and supporting populations for whom health inequalities exist and services are inaccessible will be central to ensuring progress to meeting the interim ambitions to end HIV transmission, AIDS diagnoses and HIV-related, preventable deaths.
Most of the information included in this report was included in the official statistics published in October 2022 (4). However, this report interprets information in relation to HIV Action Plan, sets out indicators that can be used to identify and address inequalities, and includes additional information including modelled estimates for the number of people living with HIV (diagnosed and undiagnosed) and HIV incidence.
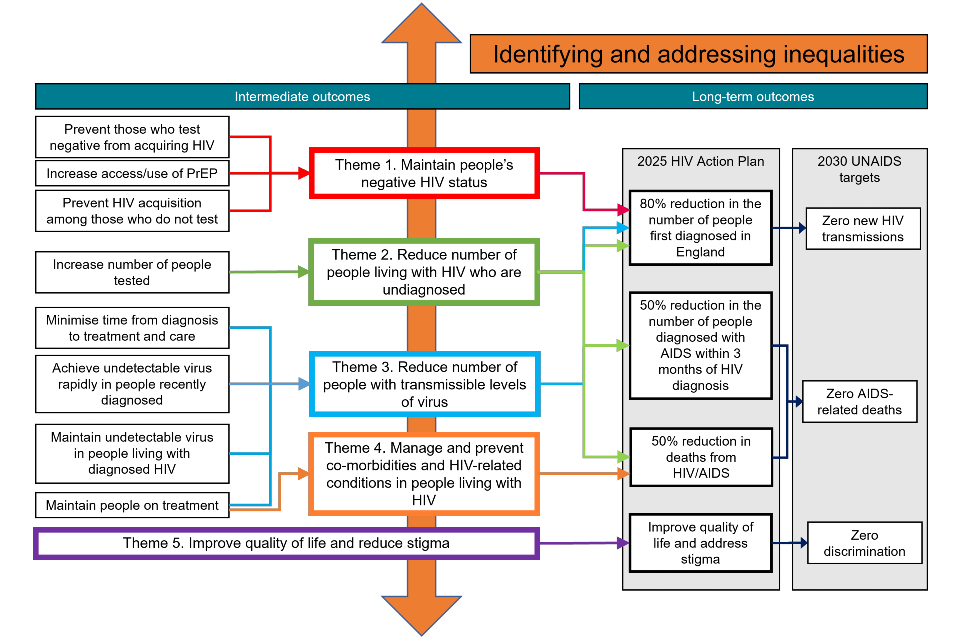
Our approach
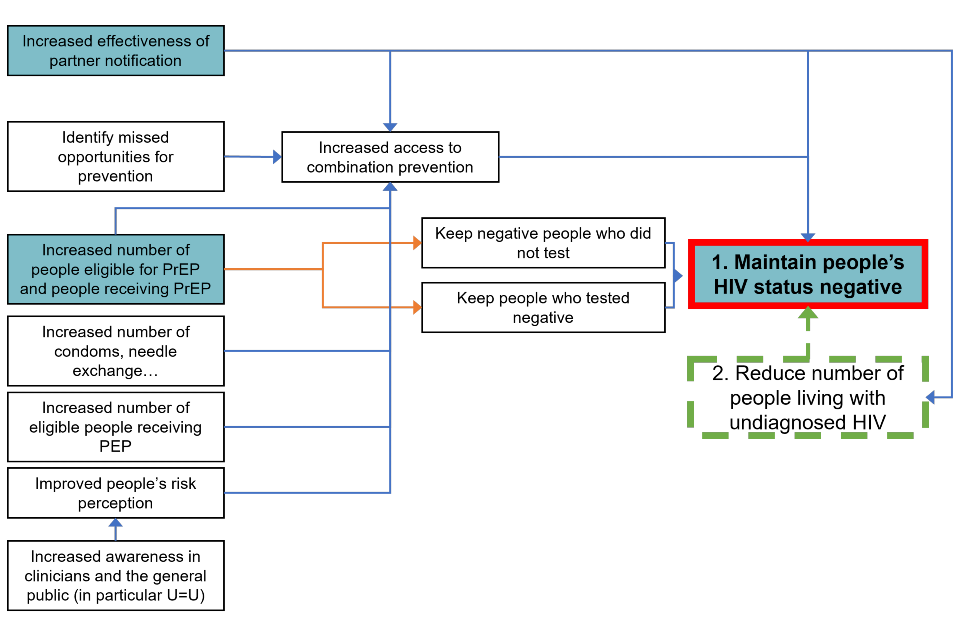
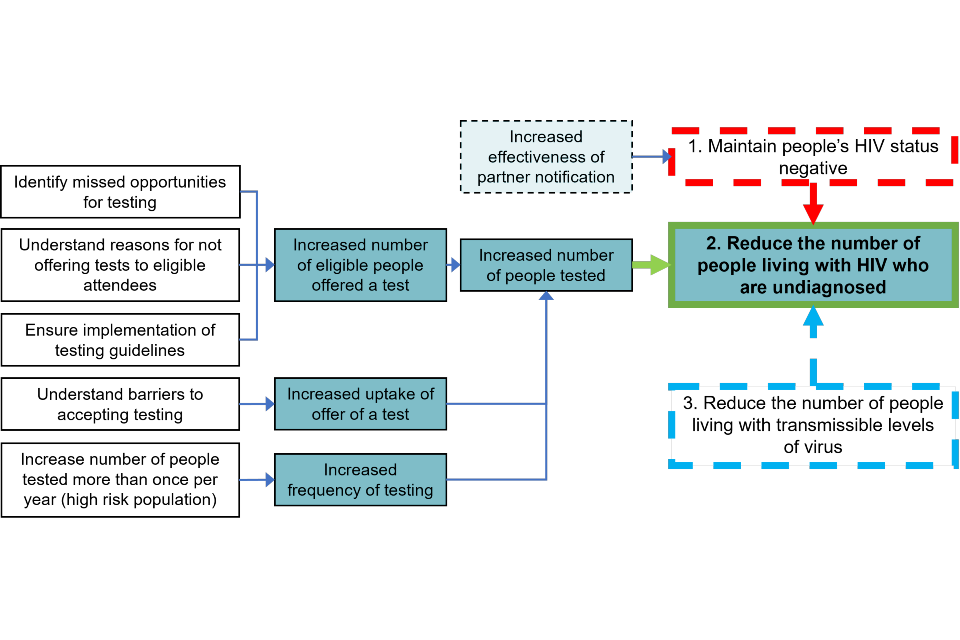
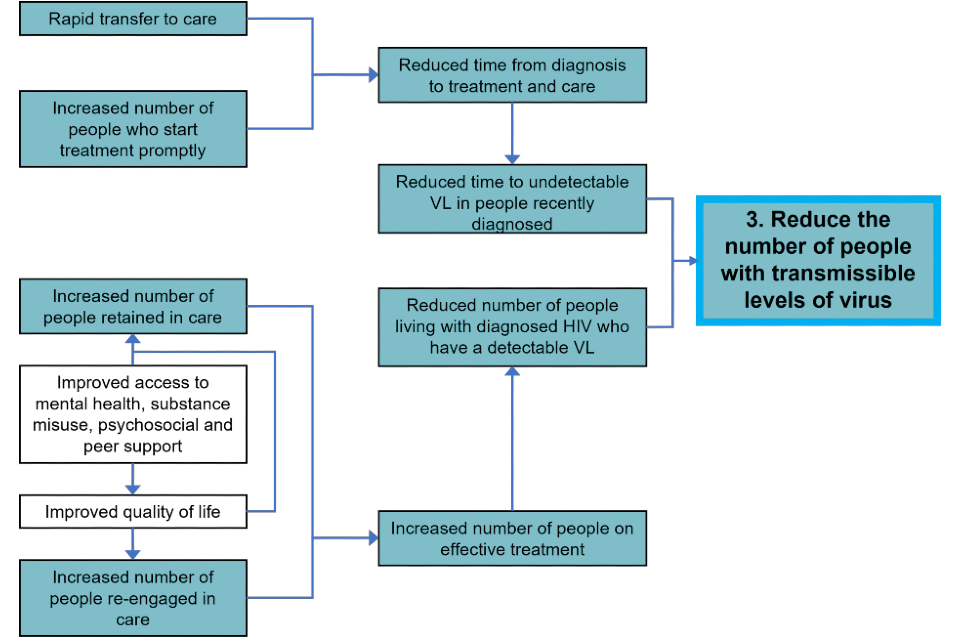
A logic model was developed in order to consider all aspects of HIV prevention, testing, diagnosis and care and how these link to the aims of the HIV Action Plan. From this, 5 themes were developed, each covering a specific aspect of prevention across the continuum of care (Figure 1):
- Maintaining people’s negative HIV status.
- Reducing the number of people living with HIV who are undiagnosed.
- Reducing the number of people with transmissible levels of virus.
- Managing and preventing co-morbidities and HIV-related conditions in people living with HIV.
- Improving quality of life and reducing stigma for people living with HIV.
Each theme is accompanied by a provisional set of indicators. These have been drawn, where available, from existing published metrics and developed using existing data sources. Sources include the Sexual and Reproductive Health profiles (5), the NHS England Specialised Services Quality Dashboards (6), the PrEP monitoring and evaluation framework (7), the 2025 UNAIDS targets (8) and the British HIV Association (BHIVA) standards of care (9). The definitions for indicators and targets for the HIV Action Plan are presented in Appendix 1.
These indicators are provisional and the UK Health Security Agency (UKHSA) will continue to work with key stakeholders to refine them in future reports for the HIV Action Plan monitoring and evaluation framework.
Figure 1 provides an overview of how the HIV themes relate to the ambitions of the HIV Action Plan and the UNAIDS targets as well as to each other.
Figure 1. Overview of the HIV themes and how they relate to long-term ambitions and UNAIDS targets
An accessible text version of this flowchart is also available.
Progress against HIV Action Plan ambitions
This report presents data between 2019 and 2021, which predates the HIV Action Plan (published in 2021). The HIV Action Plan uses 2019 as the baseline year against which the ambitions are set. In this report, the figures for the baseline year, 2019 (4), differ from those published in the HIV Action Plan (1) as further HIV clinic reports have been received since and integrated into the HIV database retrospectively. The estimates of population living with HIV (including undiagnosed) were rounded to the nearest 100.
Towards zero new HIV transmissions
New HIV diagnoses first made in England
New HIV diagnoses first made in England fell by 32% from 2,986 in 2019 to 1,987 in 2020, but numbers plateaued in 2021 (2,023) (Figure 2 and Table 3). This plateau is likely due to the COVID-19 pandemic affecting HIV testing access and health-seeking behaviours (10) with a proportion of people deferring their HIV test in 2020 and subsequently testing in 2021. To achieve the 2025 target of 600 new HIV diagnoses by 2025, a decrease of approximately 360 diagnoses first made in England, annually, from 2022 onwards, would need to be achieved. This plateau is likely due to the COVID-19 pandemic affecting HIV testing access and health-seeking behaviours with a proportion of people deferring their HIV test in 2020 and subsequently testing in 2021 (10). To achieve the 2025 target of 600 new HIV diagnoses by 2025, a decrease of approximately 360 diagnoses first made in England, annually, from 2022 onwards, would need to be achieved.
Table 3. Summary of indicators for progress towards the HIV Action Plan ambitions and UNAIDS targets, England, 2019 to 2021
| HIV Action Plan indicators | 2019 baseline | 2020 | 2021 | Percentage change (2019 to 2021) | 2025 ambition | Annual decrease from 2022 to achieve ambition |
|---|---|---|---|---|---|---|
| Number of new HIV diagnoses first made in England | 2,986 | 1,987 | 2,023 | -32% | 600 | 360 |
| Number of people diagnosed with AIDS | 216 | 169 | 171 | -21% | 110 | 16 |
| Estimated number of HIV-preventable deaths | 233.6 | 325.6 | 289.2 | +24% | 115 | 44 |
| UNAIDS 95 95 95 targets | 94%-98%-97% | 95%-99%-98% | 95%-99%-98% | Not applicable | Not applicable | Not applicable |
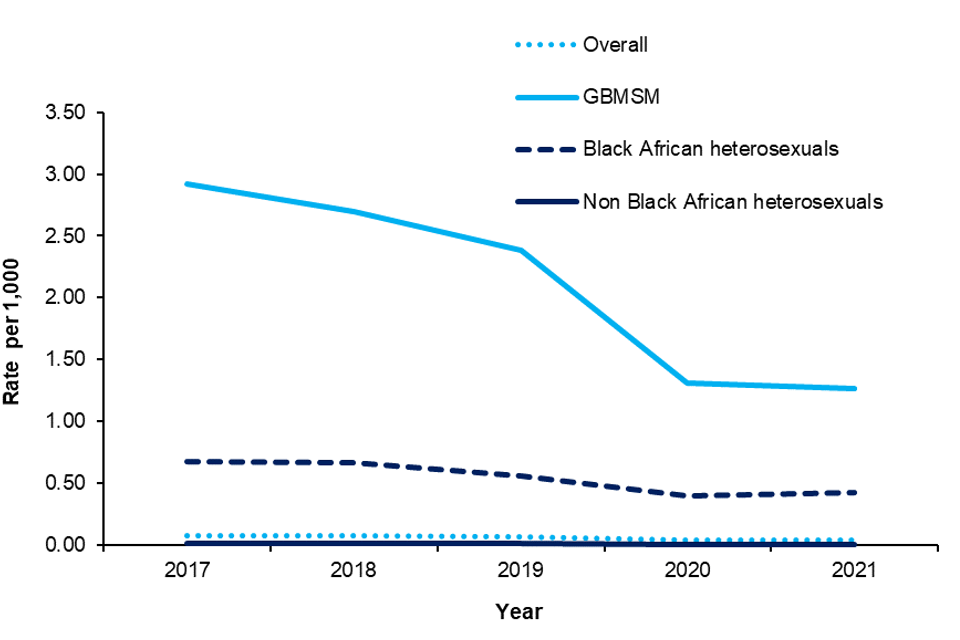
The fall in the number of people first diagnosed with HIV in England was not equal between groups. Among GBMSM first diagnosed in England, there was a 45% fall in new diagnoses between 2019 and 2020 from 1,262 to 699. Subsequently, among GBMSM living in London, new HIV diagnoses first made in England continued to decrease from 247 in 2020 to 204 in 2021. However, among GBMSM living outside London, numbers rose from 452 in 2020 to 517 in 2021. The sustained fall in GBMSM in London, which occurred in the context of high numbers of HIV testing, reflects a fall in incidence.
Among heterosexual men in London, new diagnoses first made in England reduced from 156 in 2019 to 134 in 2020 and to 108 in 2021. Outside London, new diagnoses first made in England fell from 377 in 2019 to 233 in 2020 but rose to 261 in 2021. Among heterosexual women in London, new diagnoses first made in England fell from 176 in 2019 to 117 in 2020 and rose to 140 in 2021. Outside London, new diagnoses first made in England reduced from 400 in 2019 to 275 in 2020 and rose to 289 in 2021. Among heterosexual adults, in whom HIV testing has not recovered to pre-COVID-19 levels, this suggested incidence has not fallen in this group.
Further work is needed to ensure the fall in new HIV diagnoses in London observed in GBMSM can also occur in GBMSM outside London, and among heterosexual men and women.
New HIV diagnosis rates were calculated using population denominators derived from the Multi Parameter Evidence Synthesis (MPES) model, a complex statistical model fitted to census, surveillance and survey-type prevalence data (11, 12). Although new HIV diagnoses rates (among people first diagnosed in England) have decreased across all groups over time, they remain disproportionately higher among GBMSM and Black African heterosexuals in comparison to the overall population and non-Black African heterosexuals (Figure 3).
Figure 2. Progress towards ending HIV transmission, AIDS and HIV-related, preventable deaths by 2025, England, 2010 to 2021
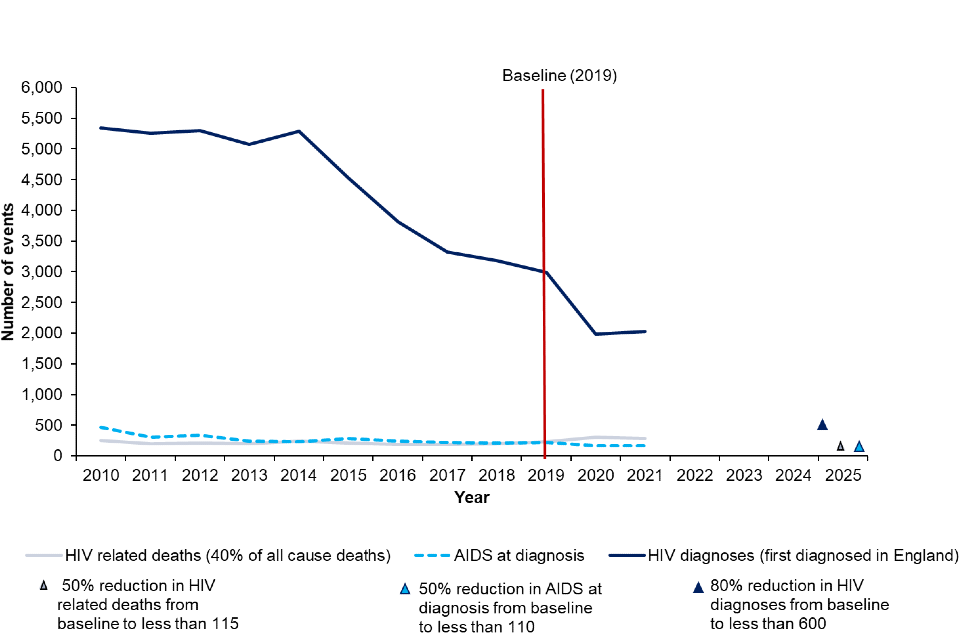
Figure 3. New HIV diagnoses rate (per 1,000) among people first diagnosed in England, by specific population groups, ages 15 to 74, 2017 to 2021
Estimating HIV transmission in gay, bisexual and other men who have sex with men
An age-dependent CD4 back-calculation model which estimates newly acquired HIV infections and probability of HIV diagnosis according to the number of new HIV diagnoses and the distribution of CD4 counts at or soon after diagnosis (13, 14) was used to generate point estimates and 95% credible intervals (CrIs) of HIV incidence among GBMSM. The number of new HIV infections in GBMSM in England was estimated to have declined from 750 (95% CrI 610 to 910) in 2019, to 660 (95% CrI 470 to 880) in 2020, and to 620 (95% CrI 390 to 910) in 2021. These estimates indicate that the trend of decreasing incidence seen in previous years has been maintained, with an 80% probability of a decline between 2019 to 2021. The extent of the decline varied between age groups, with incidence of HIV among GBMSM aged 15 to 24 declining from an estimated 170 (95% CrI 130 to 210) infections in 2019 to 90 (95% CrI 50 to 150) in 2021 (probability for decline 99.5%) (Figure 4). In comparison, incidence in GBMSM aged 35 to 44 was estimated to be stable, at 170 (95% CrI 130 to 210) in 2019, and 180 (95% CrI 100 to 290) in 2021 (probability for decline 34%).
Figure 4. Estimated HIV incidence in GBMSM in England by age group, using a CD4 back-calculation method, England, 2016 to 2021

Towards zero AIDS diagnoses
There were 171 AIDS diagnoses within 3 months of HIV diagnosis in 2021 compared to 216 in 2019. If we are to meet the HIV Action Plan ambition of fewer than 110 in 2025, we would need to reduce the number of AIDS diagnoses within 3 months of an HIV diagnosis by 16 each year from 2022 onwards.
Towards zero preventable, HIV-related deaths
In 2021, there were 723 deaths occurring in people with HIV, a 24% rise from 584 in 2019. An estimated 40% of all deaths in 2021 in people with HIV related, preventable deaths (15), this equates to 289 deaths. If the target of fewer than 115 preventable HIV-related deaths in 2025 is to be met, the number of deaths would need to reduce by 44 each year from 2022 onwards.
Compared with 2019, there were 170 and 139 more all-cause deaths in 2020 and 2021, respectively. Spikes in mortality in people living with HIV coincided with peak COVID-19 mortality (4). This suggests excess mortality in 2020 and 2021 was partially due to direct impact of COVID-19 infection, as well as its indirect impact through disruption to healthcare services. However, people living with diagnosed HIV who were on treatment and virally suppressed did not have a higher risk of COVID-19 death compared to the general population prior to the start of the widescale COVID-19 vaccination programme in December 2020 (16). In addition to the impact of COVID-19 on mortality in 2020 and 2021, the national HIV mortality review (4) which was implemented in 2019 has also led to improved ascertainment of deaths reported in this period.
Further work is underway to implement the pan-European definition of HIV-related and preventable mortality (17), which will replace the current 40% estimate of all-cause deaths occurring in people with HIV. This definition will be implemented in England in due course.
Those first diagnosed late (CD4 count under 350 cells within 91 days of diagnosis) in England in 2020 were 13 times more likely to die within a year of their diagnosis, compared to those who were diagnosed earlier (with higher CD4 counts) (4). This figure is higher than the equivalent measure for 2019 (8 times) and may reflect again the direct and indirect impact of the COVID-19 pandemic (4).
Towards zero stigma
Measuring HIV stigma is challenging, and work is ongoing to develop consensus definitions and measures. Previous publications indicate that in 2015, 30% of respondents to the Stigma Survey UK (18) and in 2017, 19% of the participants in the 2017 Positive Voices survey (19) reported having ever been treated differently from other patients in healthcare settings (enacted stigma). The UNAIDS 2025 targets set an ambition for stigma to be experienced by under 10% of people living with HIV by 2025 (8).
UNAIDS 95-95-95 progress
In 2021, England again achieved the UNAIDS 95-95-95 target nationally, with 95% of people living with HIV being diagnosed, 99% of those diagnosed being on treatment and 98% of those on treatment having an undetectable viral load (Figure 5). In London, the equivalent figures were 96%, 98% and 98% compared to 95%, 99% and 98% outside of London.
Figure 5. Progress towards the UNAIDS 95-95-95 targets by population group, England, 2019 to 2021
Theme 1: maintain people’s negative HIV status
Increased access to HIV combination prevention (including health prevention and promotion interventions, partner notification, frequent HIV testing, PrEP and PEP) will help maintain the HIV status of those who are HIV negative (Figure 6).
Partner notification is a highly effective HIV prevention strategy which is not only an extremely efficient way to find people with an undiagnosed HIV infection, but also provides the opportunity to maintain the HIV status of those partners who test negative. PrEP prevents people who are HIV negative from acquiring HIV, where appropriate, and those who test negative should be offered and maintained on PrEP while indicated, thereby preventing transmission.
Figure 6. Flowchart for theme 1: maintain people’s HIV status negative
An accessible text version of this flowchart is also available.
A summary of current and provisional indicators for theme 1 can be found in Table 4.
Table 4. Provisional indicators for theme 1: maintain people’s negative HIV status
| Code | Description | 2019 | 2020 | 2021 |
|---|---|---|---|---|
| PT1A | Number of people attending SHS due to partner notification | 1,558 | 850 | 820 |
| PT1B | Proportion of people attending SHS due to partner notification among new HIV diagnosis | Provisional indicator | Provisional indicator | Provisional indicator |
| PT1C | Number of people attending though partner notification who tested | 1,397 | 702 | 620 |
| PT1D | Ratio of partner notification contacts tested per diagnosis - a ratio of 1 suggests each HIV diagnosis results in at least one partner having a test | 1.01 | 0.85 | 0.76 |
| PT1E | Number of people attending through partner notification who tested positive | 59 | 42 | 28 |
| PT1F | Proportion of all HIV negative individuals accessing specialist SHSs categorised as having a PrEP need | Not applicable | Not applicable | 7% |
| PT1G | Proportion of all HIV negative individuals with estimated PrEP need who had this need identified | Not applicable | Not applicable | 79% |
| PT1H | Proportion of all HIV negative individuals with estimated PrEP need who started or continued PrEP | Not applicable | Not applicable | 70% |
| PT1I | Number of individuals accessing specialist SHSs who are receiving PrEP | Not applicable | Not applicable | Provisional indicator |
| PT1J | Number of individuals accessing specialist SHSs stopping PrEP | Not applicable | Not applicable | Provisional indicator |
| PT1K | HIV seroconversions among people receiving PrEP | Not applicable | Not applicable | Provisional indicator |
Partner notification (PT1A, PT1C, PT1D, PT1E)
Between 2019 and 2021 the number of people attending SHSs due to HIV partner notification decreased from 1,558 to 820. The resulting ratio of new HIV diagnoses in SHS settings to attendees due to HIV partner notification was 1.01 in 2019 and 0.76 in 2021 nationally. This means for every 100 HIV diagnoses in 2021, 76 people attended SHS as a result of HIV partner notification. Overall, 3.8% (59 people) of those attending due to HIV partner notification tested positive for HIV in 2019 compared to 4.2% in 2020 (42 people) in 2020 and 2.6% (28 people) in 2021. This data indicates that when implemented, HIV partner notification is an effective strategy to find people with undiagnosed HIV. The declining number attending SHS due to HIV partner notification is likely due to the impact of the COVID-19 pandemic in terms of health-seeking behaviours, access to services and also a decrease in sexual mixing during the national lockdowns to control COVID-19 (10, 20 to 23). While most HIV partner notification attendees were GBMSM, the highest ratios of new HIV diagnoses to HIV partner notification attendees were observed in heterosexual adults across all 3 years (Figure 7).
Figure 7: Number of people who attended SHSs due to HIV partner notification, and who had an HIV test or not, and ratio of new HIV diagnoses over number of HIV partner notification attendees, England, 2019 to 2021

Pre-exposure prophylaxis (PT1F, PT1G, PT1H)
Between October 2017 and July 2020, the Impact Trial in England recruited 24,268 patients PrEP (24). Participants received PrEP in England during and after the trial period and until the rollout of a routine PrEP service in specialist SHSs in the autumn of 2020, as part of a combination approach to HIV prevention. The PrEP monitoring and evaluation framework (7) was published in March 2022 and consists of a series of indicators to inform service improvement in PrEP commissioning and delivery.
In 2021, 7% (87,828 of 1,180,923) of HIV negative people accessing specialist SHSs in England (excluding people accessing reproductive health services only) were categorised as having PrEP need. This proportion represents people who were at substantial HIV risk and therefore could benefit from receiving PrEP (Figure 8). Among this group 79% (69,507 of 87,828) had their need identified during clinical consultation. Of those with a PrEP need identified, 70% (61,092 of 87,828) initiated or continued PrEP. However, there were differences between groups in relation to PrEP need, PrEP need identified and those initiating or continuing PrEP.
GBMSM were the group most likely to be categorised as having PrEP need (65%; 70,076 of 108,605), compared to heterosexual men (1%; 3,119 of 229,926) and heterosexual women (0.5%; 3,009 of 624,856) respectively.
While a smaller proportion of those aged under 35 years (6% (52,044 of 843,816)) were identified as having PrEP need in 2021 compared to those aged 35 years or older (11% (35,754 of 332,129)) a higher number of younger people were categorised as having PrEP need as they constitute 72% of the SHS population. PrEP need was categorised as highest among the following ethnic groups: White British (7%), Any other Asian (15%) and people of other ethnicity (12%) but lower among Black Africans (4%), Black Caribbeans (5%) and Black other groups (5%). A higher proportion of attendees were categorised as having PrEP need in London at 14% (42,774 of 301,764) compared to 5% (43,309 of 855,859) elsewhere in England.
Among those accessing specialist SHS with PrEP need, the proportion who had their need identified was 81% (56,793 of 70,076) in GBMSM compared to 49% (1,542 of 3,119) among heterosexual men and 33% (994 of 3,009) in heterosexual women respectively. Among those aged under 35 years, 77% (40,175 of 52,044) had PrEP need identified compared to 82% (29,326 of 35,754) among those aged 35 years and over. The ethnic groups with highest proportion of PrEP need identified were Any other Asian (85%), White other (84%) and people of other ethnicity (80%), with lower levels of need identified observed among a Black Caribbean (70%), Black other (69%) and Black African (62%) groups. PrEP need was more likely to be identified in London 84% (35,940 of 42,774) compared to 74% (32,223 of 43,309) in areas out outside of London.
The proportion of people accessing specialist SHSs with PrEP need identified who initiated or continued PrEP was 72% (50,152 of 70,076), 34% (1,068 of 3,119) and 23% (700 of 3,009) in GBMSM, heterosexual men and heterosexual women respectively. The proportion of people aged under 35 years with PrEP need identified who started or continued PrEP was 66% (34,557 of 52,044) compared to 74% (26,532 of 35,754) in those aged 35 years and over.
The proportion of people accessing specialist SHSs who started or continued PrEP was 79% (33,944 of 42,774) in London residents, and ranged from 65% (6,410 of 9,856) among people residing in the South East to 47% (1,785 of 3,834) among people residing in the West Midlands.
Figure 8. Proportion of HIV negative people accessing specialist SHSs with PrEP need who had their need identified, and who initiated or continued PrEP by demographics, England, 2021

Post-exposure prophylaxis
In 2021, 8,115 people received PEP for HIV. This is a 13% increase in PEP activity relative to 2020, but a 33% decrease compared with 2019 (12,038). GBMSM constituted 57% (4,664 of 8,115) of all those receiving PEP, with heterosexual and bisexual women and heterosexual men representing 14% (1,137 of 8,115) and 11% (865 of 8,115), respectively. Among the 494 people receiving more than one course of PEP in 2021, 76% (373 of 494) were GBMSM.
Theme 2: reduce the number of people living with undiagnosed HIV
Scaling up HIV testing aims to reduce the number of people living with undiagnosed HIV infection and decrease the number of people diagnosed late, thereby reducing morbidity, mortality and onward transmission (Figure 9).
Most people access HIV tests (including tests provided via the internet) through SHSs, but there are many people for whom these services are not accessible. This report provides an overview of testing activity in other settings including community settings.
Figure 9. Flowchart for theme 2: reduce the number of people living with undiagnosed HIV
An accessible text version of this flowchart is also available.
A summary of current and provisional indicators for theme 2 can be found in Table 5.
Table 5. Provisional indicators for theme 2: reduce the number of people living with undiagnosed HIV
| Code | Description | 2019 | 2020 | 2021 |
|---|---|---|---|---|
| PT2A | Estimated number of people living with undiagnosed HIV | 5,600 (95% CrI 4,100-7,900) | 4,700 (95% CrI 3,600-6,500) | 4,400 (95% CrI 3,500-6,100) |
| PT2B(i) | Number of people HIV tested in all SHSs | 1,319,915 | 913,383 | 1,053,169 |
| PT2B(ii) | Number of people HIV tested in specialist SHSs | 1,000,598 | 465,781 | 478,203 |
| PT2C | Number of eligible people offered a test in specialist SHS | 1,296,276 | 635,301 | 648,923 |
| PT2D | Number of people declining a test in specialist SHS | 295,678 | 169,520 | 170,720 |
| PT2E | Number of people who had tested least once in the year before their most recent test in specialist SHS – GBMSM | 56,054 | 38,685 | 36,094 |
| PT2F | Late diagnosis in those first diagnosed in England | 857 | 667 | 754 |
| PT2G | Late HIV diagnosis among all people newly diagnosed with HIV in England | 1,017 | 773 | 866 |
| PT2H | HIV testing coverage for universal antenatal screening | 99.7% | 99.8% | 99.8% |
| PT2I | Number of people tested in other settings | Provisional indicator | Provisional indicator | Provisional indicator |
| PT2J | Number of people tested in ED in higher prevalence areas | 115,349 | 90,677 | 98,919 |
| PT2K | Coverage in ED in higher prevalence areas | Provisional indicator | Provisional indicator | Provisional indicator |
| PT2L | Reactive tests and rates in ED in higher prevalence areas | 630 (0.5%) | 543 (0.6%) | 602 (0.6%) |
| PT2M | New HIV positives in ED in higher prevalence areas (excluding people already known to be HIV positive both in care and not engaged in care) | Provisional indicator | Provisional indicator | Provisional indicator |
| PT2N | Positive tests in ED in higher prevalence areas in people previously diagnosed and not in care | Provisional indicator | Provisional indicator | Provisional indicator |
Estimated number of people living with undiagnosed HIV infection (PT2A)
National estimates of the number of people living with HIV in England, including those undiagnosed, are obtained from a multi-parameter evidence synthesis (MPES) model, which is fitted to census, surveillance and survey-type prevalence data (11, 12).
In 2021, there were an estimated 4,400 (95% CrI 3,500 to 6,100) people unaware of their infection, equivalent to 5% (95% CrI 4% to 6%) of all people estimated to be living with HIV in England (95,900 (CrI 94,700 to 97,700)). An estimated 1,500 (95% CrI 1,000 to 2,600) GBMSM were living with an undiagnosed HIV infection compared with 1,100 (95% CrI 700 to 2,400) heterosexual men and 1,500 (95% CrI 1,200 to 2,000) heterosexual women. Overall, there were 1,300 (95% CrI 1,000 to 1,900) people estimated to be living with an undiagnosed HIV infection in London compared with 3,000 (95% CrI 2,300 to 4,400) outside of London.
The relative contribution of different age groups to undiagnosed HIV infection varies between different exposure groups. In GBMSM, those aged 15 to 34 years old have dropped from accounting for 58% (95% CrI 34% to 78%) of those undiagnosed in 2019, to 49% (95% CrI 27% to 70%) in 2021. As a result, most GBMSM living with undiagnosed HIV are now estimated to be over the age of 34 years (51%, 95% CrI 30% to 73%). In contrast, among heterosexual men living with undiagnosed HIV, the largest age group was those aged between 35 and 44 years between 2019 (36% of those undiagnosed, 95% CrI 23% to 47%) and 2021 (37% of those undiagnosed, 95% CrI 26% to 47%). During this period, the estimated proportion of undiagnosed heterosexual men in the 15 to 34 age group slightly reduced (26% in 2019, 95% CrI 11% to 47%, and 23% in 2021, 95% CrI 10% to 42%; probability of decline 59%). Finally, in heterosexual women, the largest age category in 2019 was women aged 15 to 34 (43% of those undiagnosed, 95% CrI 33% to 53%), whereas proportions in those aged 15 to 34 and 35 to 44 years in 2021 were similar (32% of those undiagnosed age 15 to 34, 95% CrI 24% to 42%; 33% age 35 to 44, 95% CrI 26% to 39%). The probability of a decline from 2019 to 2021 in the proportion of undiagnosed heterosexual women who were aged 15 to 34 was 94%. Overall, these estimates reflect a shift in the population living with undiagnosed HIV from younger to older age groups between 2019 and 2021, though one which shows considerable heterogeneity between different populations, and considerable uncertainty.
Trends in the estimated number of people living with undiagnosed HIV from 2019 to 2021 for different exposure groups and different regions vary considerably (Figure 10). Estimates for GBMSM living in London have consistently declined between 2019 and 2021 (probability of decline 94%), in contrast to those for Black African and non-Black African heterosexuals, which have remained relatively stable over this period (probabilities of decline 71% and 55%, respectively). Outside London, the estimated number of GBMSM living with undiagnosed HIV declined between 2019 and 2020 (probability of decline 84%) but has remained stable between 2020 and 2021 (probability of decline 50%; probability of decline 2019 to 2021 83%). For Black African and non-Black African heterosexuals, estimates have remained largely stable between 2019 and 2021 (probabilities of decline 31% and 61%, respectively).
Figure 10. Estimated number of people with undiagnosed HIV infection by region and exposure group, 2019 to 2021, England

HIV testing
Number of people tested at all SHSs (PT2B(i)) and in specialist SHSs (PT2B(ii))
The number of people having an HIV test at all SHSs reduced by 31% between 2019 and 2020 (1,319,915 to 913,383). However, the number of people tested in 2021 showed a partial recovery with a 15% rise to 1,053,169. Despite this rise, there were still 266,746 (20%) fewer people tested in 2021 than in 2019.
The recovery in testing between 2020 and 2021 is not seen equally across different demographic groups. The number of GBMSM having an HIV test in an SHS increased by 23% from 144,800 in 2020 to 178,466 in 2021, 14% higher than the 156,631 people tested in 2019. Notably, online testing played a central role in this increase in GBMSM, comprising 21% of tests in 2019, but 56% in 2021, and thus has become a substantially larger component of all testing in this time this time. In heterosexual and bisexual women, a smaller 11% increase was seen between 2020 and 2021 (441,017 to 489,727), placing levels of testing at 78% of 2019 testing levels (628,607). Despite a substantial fall between 2019 and 2020 (42%, 419,501 to 242,813), testing in heterosexual men increased by just 2% between 2020 and 2021 to 248,355; 59% of 2019 testing levels. In each of these groups, online testing has increased between 2019 and 2021; 199% in GBMSM, 151% in heterosexual and bisexual women and 125% in heterosexual men.
When restricted to specialist SHS, similar patterns were observed, though displayed a less substantial recovery as online testing continued to play a far greater role in both 2020 and 2021 than in previous years. Between 2019 and 2021 testing in specialist SHS declined: 52%, from 1,000,598 to 478,203. Unlike for testing in all SHSs, the number of GBMSM testing in specialist SHS in 2021 remained below what was seen in 2019, at 66% of 2019 level. Meanwhile, testing in groups such as heterosexual men and heterosexual and bisexual women in 2021 remained substantially below what was seen in 2019, at 33% and 40% of 2019 levels, respectively.
Number of people offered (PT2C) and declining a test (PT2D) in specialist SHSs
Between 2019 and 2021, the number of specialist SHS attendees who were eligible for an HIV test declined from 1,542,038 in 2019 to 1,044,998 in 2021, reflecting a sharp reduction in attendances between 2019 and 2021. In this period, the proportion of these attendees offered an HIV test decreased from 84% in 2019 to 62% in 2021, while the proportion declining an HIV test decreased from 19% in 2019 to 16% in 2021. These corresponded to a reduction in the number offered an HIV test from 1,296,276 in 2019 to 635,301 in 2021, and in the number declining an HIV test from 295,678 to 170,720 in 2021.
The number of GBMSM offered an HIV test in specialist SHS increased by 6% from 78,609 in 2020 to 83,024 in 2021, only 66% of the 126,289 offered in 2019 (Figure 11). In the same period, the proportion of GBMSM offered an HIV test declined from 91% in 2019 to 81% in 2021. Between 2020 and 2021, the number of GBMSM declining an HIV test decreased by 13% from 3,937 to 3,425, while the proportion declining an HIV test remained stable (4% to 3%).
In specialist SHS, 140,067 heterosexual men were offered a test in 2021 compared with 167,006 in 2020, a decrease of 19%. The number of heterosexual men declining a test decreased by 19% from 30,469 in 2020 to 24,752 in 2021. The proportion of heterosexual men who declined an HIV test fell slightly from 13% in 2020 to 12% in 2021.
In heterosexual and bisexual women, the number offered an HIV test decreased by 7% from 335,483 to 312,060 between 2020 and 2021. This coincided with a small increase in the proportion of eligible heterosexual women declining an HIV test, from 21% in 2020 to 22% in 2021. However, among women, the number attending for reproductive purposes may not have been fully excluded.
Figure 11. HIV testing offer and uptake among people tested at specialist SHS, by ethnicity, sexual orientation and gender: England, 2021

Frequency of HIV testing among GBMSM (PT2E)
Testing guidance (25) recommends that GBMSM should be tested for HIV at least once a year and every 3 months if they are having sex without condoms with new or casual partners. Frequent HIV testing facilitates prompt diagnosis of HIV, enabling prompt treatment initiation to avoid serious illness in the future, and reduces onward transmission.
The proportion of GBMSM attendees who had at least one HIV test in the year before their most recent test remained broadly consistent over the last 3 years (47% in 2019, 52% in 2020, 45% in 2021). In this time, the proportion of tested attendees who had tested 4 or more times in the year before their most recent test declined (3.9% in 2019, 2.9% in 2020, 1.8% in 2021).
Late HIV diagnosis among those first diagnosed in England (PT2F) and among all people newly diagnosed with HIV in England (PT2G)
A late HIV diagnosis is defined as having a CD4 count below 350 cells per mm3 within 91 days of diagnosis and excludes those with evidence of recent HIV infection (26). People diagnosed late include both those first diagnosed in England, and those previously diagnosed abroad.
The total number of individuals diagnosed late first was 1,017 in 2019, declining to 866 in 2021. Over the same period, the proportion of people diagnosed who were diagnosed at late stage of infection rose from 35% in 2019 to 40% in 2021.
Excluding those previously diagnosed abroad, the total number of persons diagnosed late among those first diagnosed in England fell from 857 in 2019 to 754 in 2021. This corresponds to an increase in the overall rate of late diagnosis from 41% in 2019 to 46% in 2021.
The proportion of late HIV diagnoses first made in England increased across all groups between 2019 and 2021: 55% to 64% among heterosexual men, 48% to 50% in heterosexual and bisexual women, and 29% to 37% in GBMSM. The decrease in the number of late diagnoses combined with a rise in rates is likely to reflect several aspects of disruption caused by the COVID-19 pandemic, particularly among heterosexuals. Reduced testing in SHS during 2020 and 2021 means more people remaining undiagnosed, including those at a late stage of infection. Disruption to non-SHS health services will also have reduced opportunities for testing, with many late diagnoses being made in these settings. Finally, given reduced testing opportunity, diagnosis may have skewed towards those at a late stage of infection accessing health services with illness directly related to HIV, and so are more likely to be diagnosed despite the disruptions caused by the COVID-19 pandemic (29).
Universal antenatal screening (PT2H)
HIV testing coverage for pregnant women in antenatal care remained high at 99.8% with 642,434 women tested (643,856 eligible women) in England during the 2020 to 2021 financial year (30). The proportion of women who tested positive for HIV during pregnancy remained low at 0.96 per 1,000 eligible pregnant women. The proportion of newly diagnosed women remained at 0.11 per 1,000 eligible women. This has met the UNAIDS 2025 target of 95% coverage of antenatal services testing to end vertical HIV transmission (8).
HIV testing in other settings (PT2I)
1. Home and community
In 2021,38,027 tests were delivered via the national HIV and syphilis self-sampling framework co-ordinated by the Office for Health Improvement and Disparities (OHID), UKHSA and local authorities, and delivered by SH:24 (27). This is an increase of 45% compared with 21,060 in 2020, with a test reactivity rate of 0.7% in 2021 (27).
Another 13,857 tests were reported through the UKHSA Survey of HIV Testing in Community Settings (28) in 2021, compared with 10,780 tests reported in 2020. The overall reactivity rate was 0.4%.
2. Blood donation services
In 2021, over 1.7 million blood donations were screened across the UK, with 9 donors confirmed positive for HIV (0.5 per 100,000 donations): 7 were new donors (4.7 per 100,000 donations) and 2 were repeat donors (0.1 per 100,000 donations).
From June 2021, a major change in blood donor selection policy was introduced across the UK following recommendations from the For Assessment of Individualised Risk (FAIR) steering group (31). The changes allow GBMSM in established relationships and people with partners from HIV endemic areas to donate if no other donor selection criteria apply. A 6-month review has showed no impact on the safety of the supply. Close monitoring remains in place with a further review of the impact 12-months post-implementation (32).
3. Tuberculosis (TB) testing
In 2021, testing information was available for 96% (4,028 of 4,217) of notified TB cases in England, with previously unknown HIV status and excluding those who were diagnosed with TB post-mortem. Of these, the uptake rate was 97%, with 3,908 tested in this setting.
4. People who inject drugs
The Unlinked Anonymous Monitoring (UAM) Survey of People Who Inject Drugs (PWID) is an annual cross-sectional biobehavioural survey that recruits people who have ever injected psychoactive drugs who attend specialist drug and alcohol services across England, Wales, and Northern Ireland (33). During 2020 and 2021, the COVID-19 pandemic impacted recruitment to the UAM Survey, with changes to the number, characteristics and geographical distribution of the participants recruited during these years (34). In England the proportion of PWID ever having had an HIV test was 81% (95% confidence interval (CI) 79% to 83%) in 2021, with 32% (95% CI 30% to 35%) reporting having had a test in the past 12 months. Among PWID who started injecting in the past 3 years, during 2020 and 2021 (years were combined due to small numbers), 58% (95% CI 49% to 67%) reported ever having had a diagnostic HIV test, with 52% (95% CI 40% to 65%) of these reporting a test in the past 12 months.
5. Prisons
In March 2018, opt-out testing of blood-borne viruses, including HIV, was implemented in all adult prisons in England (35). New arrivals and people transferring between prisons should now be offered HIV tests, unless they have been tested within the last year and are not at risk, or they have a known HIV positive status. Between April 2021 and March 2022, 92% of new receptions and transfers not already confirmed as HIV positive were offered HIV testing within 7 days of reception (125,284 of 136,219). Where a test was not declined and was considered appropriate, 67% were tested within 2 weeks of reception date (67,346 of 101,142).
6. General practice, emergency departments and in and out-patient secondary care
In 2021, 20 laboratories reported HIV testing data from general practice and hospitals to the Sentinel Surveillance of Blood Borne Viruses (SSBBV) (36). A total of 94,340 people tested at a general practice in 2021 (50,100 in 2020); 221,124 in secondary care (144,190 in 2020) and 105,343 in emergency departments (68,560 in 2020) were reported through SSBBV, with 0.2%, 0.4%, and 0.6%, testing positive, respectively. The number of individuals tested are comparable to pre-COVID-19 pandemic levels.
7. Opt-out testing in ED setting (PT2J-N)
As part of the HIV Action Plan (1), NHS England (NHSE) are expanding opt-out testing in emergency departments in the 21 local authority areas across the country with the highest prevalence of HIV, in line with HIV testing guidance (2016) from the National Institute for Health and Care Excellence (NICE) (25). It is hoped this will address health inequalities experienced by groups of people living with HIV who may not routinely attend SHSs (37). This intervention was expanded to include Hepatitis B and C, and the rollout of blood-borne viruses opt-out ED testing began in April 2022. NHSE published a report on numbers tested and diagnosed through the first 100 days of this intervention being implemented (38).
Future UKHSA analyses will present information on testing coverage, number testing positive for blood-borne viruses, positivity, the number of positive tests that were new HIV diagnoses and the number that occurred in people previously diagnosed, including those not retained in care, as well as identifying and monitoring health inequalities. An assessment will also be undertaken on the extent to which those previously diagnosed and not retained in care subsequently re-engage with treatment and care.
Theme 3: reduce the number of people with transmissible levels of virus
For those who test positive, minimising time from diagnosis to initiation of treatment will reduce the time people are living with a detectable viral load (Figure 12).
Enabling individuals to remain on treatment with an undetectable viral load reduces overall transmissible levels of virus and the opportunity for onwards transmission to sexual partners. This includes ensuring that individuals already diagnosed with HIV are linked to, engaged in, and where relevant, re-engaged in care so that they can access effective treatment and achieve viral suppression.
Figure 12. Flowchart for theme 3: reduce the number of people with transmissible levels of virus
An accessible text version of this flowchart is also available.
A summary of current and provisional indicators for theme 3 can be found in Table 6.
Table 6. Provisional indicators for theme 3: reduce the number of people living with transmissible levels of virus
| Code | Theme 3: indicator | 2019 | 2020 | 2021 |
|---|---|---|---|---|
| PT3A | Estimated number of people living with transmissible levels of virus in England | 12,932 | 12,184 | 11,985 |
| PT3A(i) | Number of people not linked to care within calendar year of diagnosis | 342 | 259 | 147 |
| PT3A(ii) | Number of people on treatment and no evidence of viral suppression | 3,608 | 1,222 | 2,762 |
| PT3B | Number of people not linked to care within 15 days of HIV diagnosis | 1,910 | 1,357 | 1,525 |
| PT3C | Number of people not linked to care within 28 days of HIV diagnosis | 2,244 | 1,578 | 1,742 |
| PT3D | Number and proportion of people starting treatment within 90 days of diagnosis | 2,279 | 1,446 | 1,538 |
| PT3E | Number of people seen for HIV care and not on treatment | 1,627 | 1,119 | 1,195 |
| PT3F | Number (and proportion) of people treated who are not virally suppressed (viral load over 200 copies) | 2,096 (2.4%) | 1,874 (2.2%) | 1,799 (2.0%) |
| PT3G | Number of people not attending care for at least 15 months (‘not retained in care’) | 2,519 | 4,980 | 4,444 |
| PT3H | Number of people who had not attended care for at least 15 months and have attended a new appointment | 5,259 | 3,626 | 4,939 |
| PT3I | Number of people effectively re-engaged in care – people who had not attended care for at least 15 months, reattended and who have undetectable viral load within 6 months | 4,094 | 2,301 | Not available |
| PT3J | Number of late HIV presentations among those previously diagnosed abroad | 160 | 106 | 112 |
| PT3K | Number of people who had not attended care for >15 months and have attended a new appointment following opt-out testing in ED | Provisional | Provisional | Provisional |
Estimated number of people with transmissible levels of virus in England (PT3A)
In 2021, a lower-level estimate of 11,985 people living with HIV had transmissible levels of virus, equivalent to 13% of people living with HIV. The equivalent numbers for 2019 and 2020 were 12,184 and 12,932 respectively.
Of the 11,985 people (lower level estimate) with transmissible levels of virus, an estimated 4,400 (37%) (95% CrI 3,500 to 6,100) remained undiagnosed in 2021 while 7,585 were living with diagnosed HIV, of which: 147 (1.2%) were first diagnosed in 2021 and not linked to care by end of the year, 4,444 (37%) were not retained in care (not seen in care for at least 15 months since last HIV care appointment between October 2019 and September 2020), 1,195 (10%) attended care in 2021 but were not receiving treatment, and 1,799 (15%) were on treatment in 2021 but were not virally suppressed (viral load below 200 copies per mL) (Figure 13).
In a higher-level estimate, the number of people living with transmissible levels could reach up to 32,829, if we include the 2,618 people who were on treatment in 2021 but had no evidence of viral suppression (95% of whom had missing viral load data for 2 consecutive years) and the additional 18,226 people who had been seen once from January 2015 to September 2019 but not seen for at least 15 months by end of 2021. For 2019 and 2020, the higher-level estimates were 23,613 and 25,239, respectively.
Figure 13. Lower-level estimates for the number of people living with HIV with transmissible levels of virus, England, 2021
Linkage to HIV care (PT3B and PT3C)
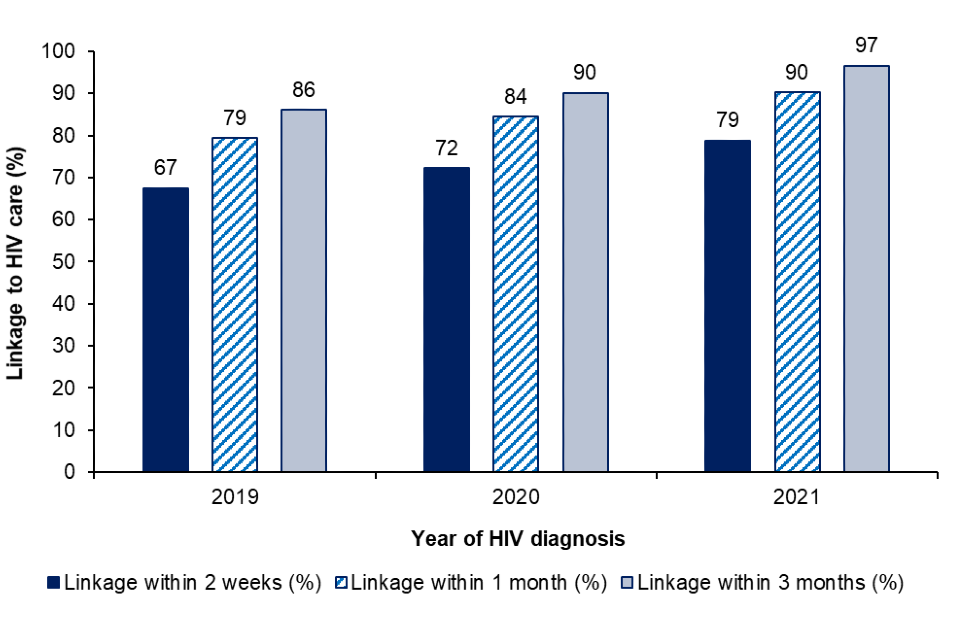
Linkage to HIV care is defined as having a first CD4 count result, viral load result or HIV clinic attendance within a specific number of weeks or months of the HIV diagnosis date. In 2021, 79% (1,525 of 1,935) of adults first diagnosed with HIV in England were linked to HIV care within 2 weeks, 90% (1,742 of 1,930) within 1 month and 97% (1,857 of 1,923) within 3 months. This compared to 67% (1,910 of 2,831), 79% (2,244 of 2,826) and 86% (2,426 of 2,820) within 3 months respectively, in 2019 (Figure 14).
Figure 14. Linkage to HIV care within 2 weeks, one month and 3 months among adults first diagnosed with HIV in England: 2019 to 2021
Prompt HIV treatment (PT3D)
Among those diagnosed with HIV in England in 2021, 78% (1,583 of 2,023) started HIV treatment within 90 days of diagnosis, compared to 73% (1,446 of 1,987) in 2020 and 76% (2,279 of 2,986) in 2019.
Treatment coverage (PT3E)
The proportion of people receiving anti-retroviral therapy (ART) amongst people in HIV care remains high, at 98% (88,352 of 89,982) in 2019 and 98% (89,583 of 91,083) in 2021. In 2021, there were 1,195 people living with HIV and attending care who were not receiving ART and 305 people with a missing ART status recorded.
Viral suppression (PT3F)
ART not only prevents illness and death in people living with HIV but achieving viral suppression also prevents transmission of HIV. This is referred to as TasP and also promoted as undetectable=untransmissible or U=U (39).
In England, 98% of people on treatment and with viral load results available were virally suppressed (79,951 of 81,750) in 2021.
In 2021, 1,799 people on ART had a reported detectable viral load, compared with 1,874 in 2020 and 2,096 in 2019. In addition, 2,618 people on treatment did not have any viral load recorded in 2021 and either no viral load reported or a detectable (over 200 copies per mL) viral load reported in 2020. This is an increase compared with 1,071 in 2020 but lower than 2019 (3,500).
Retention in care (PT3G, PT3H)
During the COVID-19 pandemic, fewer people were seen in HIV care compared to previous years due to the impact of the public health measures to control COVID-19 on HIV care access and delivery (2). People not retained in care are not receiving the treatment and support needed to remain healthy and virally suppressed.
Current BHIVA guidelines recommend that people living with HIV should attend care on a yearly basis (40). Though most people are seen within 12 months, some delays may occur. Therefore, people not retained in care are those not seen within 15 months of their last attendance for the below measures.
Among the 94,695 people seen for HIV care between 1 October 2019 and 30 September 2020, 4,444 people were not retained in care that is were not seen for care again for at least 15 months, and up until the end of 2021. Similar measures for 2019 and 2020 were 2,519 and 4,980, respectively.
It is worth noting that of the 91,083 people seen for HIV care in 2021, 4,939 people had returned after a care gap of over 15 months since January 2015. Future analyses will include as a proxy for reintegration into care, an assessment of the extent to which people with a history of over 15 months’ absence from care attain an undetectable viral load.
Late HIV presentations among those diagnosed abroad (PT3J)
Amongst those diagnosed at a late stage of infection in England are individuals who were previously diagnosed outside the UK, and who present at a late stage of infection. Overall, those previously diagnosed abroad constitute approximately one quarter of new HIV diagnoses made each year in England (25%, 669 of 2,692 in 2021), but only 13% (112 of 866 in 2021) of all diagnoses made at a late stage of infection.
From 2019 to 2021, the proportion of those previously diagnosed abroad who presented at a late stage of infection remained stable, at 20% (160 of 788 in 2019, 106 of 525 in 2020, and 112 of 547 in 2021). Meanwhile the proportion of those who were diagnosed late increased (41%, 857 of 2,101 in 2019; 44%, 667 of 1,520 in 2020; 46%, 754 of 1,630 in 2021).
Theme 4: manage and prevent co-morbidities and HIV related conditions
Delivering high quality care in line with national standards and guidelines (40, 41) will improve quality of life, and reduce morbidity, AIDS diagnoses and HIV-related mortality. Using data sources including Positive Voices, UKHSA’s HIV surveillance systems and in collaboration with BHIVA and the British Association for Sexual Health and HIV (BASHH), we plan to provide an overview of progress to ensure those living with HIV experience holistic person-centred care. This will include developing indicators that relate to BHIVA standards of care (9) and UNAIDS 2025 targets (such as 90% of people with HIV being linked to people-centred and context-specific integrated services and 95% of women having access to sexual and reproductive health services) (8).
Table 7. Provisional indicators for theme 4: manage and prevent co-morbidities and HIV-related conditions in people living with HIV
| Code | Definition or description | 2019 | 2020 | 2021 |
|---|---|---|---|---|
| PT4A | Successful linkage from paediatric to adult HIV care | Provisional indicator | Provisional indicator | Provisional indicator |
| PT4B | Drug resistance (to PI, NRTI, NNRTI and INSTI) | Provisional indicator | Provisional indicator | Provisional indicator |
| PT4C | Hepatitis B co-infection | Provisional indicator | Provisional indicator | Provisional indicator |
| PT4D | Hepatitis C co-infection (diagnoses, treatment and cure) | Provisional indicator | Provisional indicator | Provisional indicator |
| PT4E | Patient satisfaction with services such as patient-reported experience measures (PREMs) | Provisional indicator | Provisional indicator | Provisional indicator |
| PT4F | Number and proportion of people whose GP is aware of HIV status | Provisional indicator | Provisional indicator | Provisional indicator |
These indicators (Table 7) and the corresponding flowchart (Figure 15) have not been fully developed. Through consulting with the HIV Action Plan Implementation Steering group and others, including professional groups, HIV community, and academic partners, we aim to develop a suite of indicators to measure the extent of co-morbidities and HIV related conditions.
Figure 15. Flowchart for theme 4: manage and prevent co-morbidities and HIV related conditions in people living with HIV
An accessible text version of this flowchart is also available.
Theme 5: improve quality of life and reduce stigma
Reducing stigma is central to achieving the UNAIDS 2030 goals (42). This is because HIV-associated stigma remains a significant factor in people’s experience of living with HIV and negatively impacts on access to testing and effective prevention interventions (43). Furthermore, for some people with diagnosed HIV, it can be challenging to prioritise their HIV care and adherence to treatment if they are experiencing personal, financial, housing, immigration, or mental health difficulties (44). Increasing retention in, and adherence to treatment and support in achieving good health outcomes in turn reduces HIV transmission. Improving the quality of life for people with long-term conditions is a well-established goal for the NHS and wider health and care system (45).
However, previously published data from 2 UK-based surveys (Stigma Index 2015 (18) and Positive Voices 2017 (19)) can provide some context. Table 8 summarises potential indicators that could be taken from these 2 sources. However, further work with the HIV Action Plan Implementation Steering group and with professional groups, HIV community, and academic partners will focus on further developing key indicators and the corresponding flowchart (Figure 16) to monitor quality of life and stigma for people living with HIV. It is likely these will be aligned to UNAIDS 2025 targets, which include an assessment of punitive laws and policies, less than 10% of people living with HIV experiencing stigma and discrimination and less than 10% experiencing gender inequality and violence (8).
Table 8. Potential indicators for theme 5: improve quality of life and reduce stigma in people living with HIV
| Code | Provisional indicator description | Stigma Index Survey (2015) | Positive Voices Survey (2017) |
|---|---|---|---|
| PT5A | Quality of life (Positive Voices life satisfaction) | Not available | 7.4 |
| PT5B | Patients living with HIV reported to have been treated differently from other patients (enacted stigma) | 26% | 19% |
| PT5C | Patients living with HIV felt that they were being refused healthcare or delayed a treatment or medical procedure (perceived stigma) | 15% | 11% |
| PT5D | Patients living with HIV were worried that they would be treated differently than other patients (anticipated stigma) | 46% | 35% |
| PT5E | Patients avoided seeking healthcare when they needed it (anticipated stigma) | 18% | 24% |
| PT5F | Experience of HIV stigma in other settings among people living with HIV | Not available | Not available |
| PT5G | Disclosure of HIV status outside of healthcare settings – people with HIV who never told anyone | 15% | 13% |
Figure 16. Flowchart for theme 5: improve quality of life and reduce stigma
An accessible text version of this flowchart is also available.
Quality of life and life satisfaction
In 2017, respondents to the Positive Voices survey (19) rated their life satisfaction at a score of 7.4 (compared with 7.7 in general population). In the same survey, people living with HIV reported more issues with mobility, self-care, usual activities, pain or discomfort, and anxiety or depression, the 5 EQ-5D-5L domains (46) than the general population: for instance, 49% of respondents reported anxiety and depression compared with 30% in the general population.
Recent work funded by BHIVA developed the Positive Outcomes questionnaire, an HIV-specific PROMs (47) that can be used in clinical settings to ascertain patient quality of life and healthcare needs.
Stigma, discrimination and disclosure
In 2017, 19% of Positive Voices survey respondents reported having been treated differently from other patients (19). In 2015, 26% of respondents to the Stigma Index survey reported this (18). Among Positive Voices survey respondents in 2017, 11% reported that they felt that they were being refused healthcare or delayed a treatment or medical procedure (19). In 2015, 15% of respondents to the Stigma Index survey reported this (18). Overall, 35% of patients surveyed in Positive Voices in 2017 were worried that they would be treated differently than other patients in healthcare settings due to their HIV status (19). This measure was 46% among respondents to the Stigma Index survey in 2015 (18). In 2017, 18% of patients surveyed in Positive Voices reported that they avoided seeking healthcare when they needed it (19). This measure was 24% among respondents to the Stigma Index survey in 2015 (18). A total of 13% of the 2017 Positive Voices survey (19) respondents had not disclosed their positive HIV status to anyone outside of healthcare settings. This measure was 15% among respondents to the Stigma Index survey (2015).
Concluding remarks
This first report for the monitoring and evaluation framework provides an overview of progress towards meeting England’s HIV Action Plan ambitions of reducing HIV transmission by 80% and HIV related and preventable deaths and AIDS diagnoses by 50% from 2019 to 2025. This report also sets out key indicators to identify where more work needs to be done in order to meet these ambitions.
The COVID-19 pandemic has impacted progress to meeting the Action Plan’s ambitions in several ways. Among GBMSM, after a fall in HIV testing in 2020, the numbers tested in 2021 exceeded pre-COVID-19 levels. The fall in HIV diagnoses in this population plateaued in 2021 and the CD4 back calculation model indicates an underlying fall in HIV incidence, but that rate of decline may be slowing. Among heterosexuals, HIV testing coverage remains substantially lower in 2021 than in 2019 and heterosexual women remain the group most likely to decline a test at specialist SHSs. This, combined with a slight increase in HIV diagnoses, suggests no fall in incidence and a rise in the number of people with undiagnosed HIV infection. This is supported by the MPES model which shows undiagnosed HIV infection in heterosexuals has not declined over 3 years, compared to a halving of the same estimate among GBMSM over the same period. The rise in deaths in people with HIV between 2019 to 2021 is partially due to improved ascertainment as part of the National HIV Mortality Review and to the impact of COVID-19 in 2020 prior to the start of the National COVID-19 Vaccination Programme.
Five key themes have been set out with accompanying indicators. HIV partner notification remains highly effective, but activity slowed down during 2020 and 2021. In 2021 over 60,000 initiated or continued PrEP but stark inequalities remain in relation to sexual orientation, ethnicity, region and age group with uptake highest in white, older GBMSM. An estimated 12,000 people are living with transmissible levels of virus, of whom 37% are diagnosed but not retained in care. This indicates that alongside HIV testing, identifying and re-engaging people not attending care is crucial for the health of the individual but also in reducing onward HIV transmission. Further work needs to be undertaken with people living with HIV and key stakeholders to map out what is needed to prevent and manage co-morbidities in people living with HIV in addition to developing accurate and meaningful measures of stigma.
There is much to celebrate in the progress made to end HIV transmission with under 4,500 people living with undiagnosed HIV infection and extremely high levels of antiretroviral therapy coverage and viral suppression. However, progress made towards the interim ambitions as set out in the HIV Action Plan has been adversely impacted by COVID-19. If we are to meet the interim ambitions, the following areas must remain a priority:
- improving access to PrEP for all groups in need, in particular heterosexual men and women
- expanding HIV partner notification and HIV testing numbers to exceed 2019 levels, especially among heterosexual men and women
- prioritising re-engagement in care and support for those people not retained in care
- continuing efforts to understand and measure stigma, in all its forms, to improve the quality of life of people with HIV and ensure good health outcomes
- continued monitoring, reporting and tackling of inequalities in HIV prevention and care to inform accessible and culturally-competent interventions
While this edition provides a national overview, future reports will focus on identifying further inequalities by population group and regions so that they can be addressed. It will also include the development of further indicators, aligned to the 2025 UNAIDS indicators, particularly in relation to themes 4 and 5. An interactive care pathway tool will be developed to allow local experts to track progress and inequalities. Working with and supporting populations for whom health inequalities exist, and for whom services are inaccessible, will be central to ensuring progress to meeting ambitions to end HIV transmission, AIDS diagnoses, and deaths.
Acknowledgements
Contributors: Addow A, Aghaizu A, Brown AE, Buitendam E, Chau C, Connor N, Cooper N, De Angelis D, Ekajeh J, Everall I, Folkard K, Harris R, Kelly C, Kirwan PD, Lester J, McCall M, Mackay N, Martin V, Mandal S, Mitchell H, Mohammed H, Morgan J, Mou D, Murphy G, Parmar S, Peters H, Presanis A, Rafeeq S, Ratna N, Saunders J, Shah A, Simmons R, Sinka K, Sullivan A, Toswill J, Wilkinson G.
Suggested citation
Martin V, Lester J, Adamson L, Shah A, Mackay N, Chau C, Sullivan A, Brown AE, and contributors. HIV Action Plan Monitoring and Evaluation Framework: Report summarising progress from 2019 to 2021. December 2022, UK Health Security Agency, London
References
1. Department of Health and Social Care. ‘Towards Zero - An action plan towards ending HIV transmission, AIDS and HIV-related deaths in England - 2022 to 2025’. 2021
2. UK Health Security Agency. ‘Official Statistics - HIV testing, new HIV diagnoses, outcomes and quality of care for people accessing HIV services: 2021 report’. 2021
3. UNAIDS. ‘Fast-Track - Ending the AIDS epidemic by 2030’. 2014
4. UK Health Security Agency. ‘Official Statistics - HIV testing, PrEP, new HIV diagnoses, and care outcomes for people accessing HIV services: 2022 report’. 2022
5. Office for Health Improvement and Disparities (OHID). ‘Sexual and Reproductive Health Profiles’. 2022
6. NHS England. ‘NHS Commissioning: HIV’. 2020
7. Mitchell, H and others. ‘Routine commissioning of HIV Pre-Exposure Prophylaxis (PrEP) in England: Monitoring and evaluation framework’. 2022
8. UNAIDS. ‘2025 AIDS targets: Putting people living with HIV and communities at risk at the centre’. 2020
9. British HIV Association. ‘Standards of care for people living with HIV’. 2018
10. Mercer, C and others. ‘Initial impacts of COVID-19 on sexual behaviour in Britain: Findings from a large, quasi-representative survey (Natsal-COVID)’. 2021. Preprint
11. De Angelis, D and others. ‘Estimation of HIV burden through Bayesian evidence synthesis’. Statistical Science. 2014; volume 29 issue 1: pages 9 to 17
12. Presanis, AM and others. ‘Trends in undiagnosed HIV prevalence in England and implications for eliminating HIV transmission by 2030: an evidence synthesis model’. The Lancet Public Health. 2021; volume 6 issue 10: pages 739 to 751
13. Brizzi, F and others. ‘Extending Bayesian back-calculation to estimate age and time specific HIV incidence’. Lifetime Data Analysis. 2019; volume 25 issue 4: pages 757 to 780
14. Brizzi, F and others. ‘Tracking elimination of HIV transmission in men who have sex with men in England: a modelling study’. Lancet HIV. 2021; volume 8 issue 7: pages 440 to 448
15. Croxford, SE and others. ‘Mortality among people with HIV in the UK in 2020: findings from the National HIV Mortality Review’. HIV Medicine. 2022; volume 23 issue S2: page 9
16. Brown, AE and others. ‘COVID-19 mortality among people with diagnosed HIV compared to those without during the first wave of the COVID-19 pandemic in England’. HIV Medicine. 2021; volume 23 issue 1: pages 1 to 13
17. Croxford, S and others. ‘Recommendations for defining preventable HIV-related mortality for public health monitoring in the era of “Getting to zero”: an expert consensus’. Lancet HIV. 2022. Accepted
18. Hibbert, M and others. ‘Experiences of stigma and discrimination in social and healthcare settings among trans people living with HIV in the UK’. AIDS Care. 2018; volume 30 issue 7: pages 836 to 843
19. Public Health England. ‘Positive Voices: The National Survey of People Living with HIV’. 2020
20. Hyndman, I and others. ‘COVID-19 restrictions and changing sexual behaviours in HIV-negative MSM at high risk of HIV infection in London, UK’. Sexually Transmitted Infections. 2021; volume 97 issue 7: pages 521 to 524
21. Public Health England. ‘The impact of the COVID-19 pandemic on prevention, testing, diagnosis and care for sexually transmitted infections, HIV and viral hepatitis in England’. 2020
22. Shah, A and others. ‘Impact of the COVID-19 pandemic measures on HIV consultations in England’. HIV Medicine. 2022; volume 23 issue S2: page 18, TP03
23. Wang, D and others. ‘Changes in sexual behaviours and access to sexual health services, of Londoners, during first COVID-19 lockdown‘. HIV Medicine. 2021 volume 22 issue S2: pages 43 to 44, P072
24. Sullivan, A and others. ‘The HIV Pre-exposure prophylaxis (PrEP) Impact Trial: Baseline demographics, coverage and first regimen choice’. HIV Medicine. 2021; volume 22 issue S2: page 10, O013
25. National Institute for Care and Excellence. ‘Recommendations. HIV testing: increasing uptake among people who may have undiagnosed HIV’. 2016
26. Kirwan, PD and others. ‘Re-assessing the late HIV diagnosis surveillance definition in the era of increased and frequent testing’. HIV Medicine. 2022
27. Public Health England. ‘National HIV self-sampling service, November 2018 to October 2019’. 2020
28. Nash, S and others. ‘How well are the NICE recommendations for community HIV testing being implemented in England?’. HIV Medicine. 2018; volume 19 issue S2: page s135, P347
29. Brown, JR and others. ‘Changes in STI and HIV testing and testing need among men who have sex with men during the UK’s COVID-19 pandemic response’. Sexually Transmitted Infections. 2022
30. NHS England. ‘Official Statistics - Antenatal screening standards: data report 1 April 2020 to 31 March 2021’. 2022
31. NHS Blood and Transplant. ‘Blood donor selection policy: More people now able to give blood - FAIR Steering Group’. 2021
32. NHS Blood and Transplant ‘Safe supplies 2021:FAIRer donor selection - annual report’. 2022
33. UK Health Security Agency. ‘Shooting Up: infections among people who inject drugs in the UK’. 2022
34. UK Health Security Agency. ‘Unlinked anonymous monitoring (UAM) survey of HIV and viral hepatitis among people who inject drugs (PWID) 2022 report’. 2022
35. Keeley, E. ‘NCDR Health and Justice Dashboard - Health and Justice Information System (HJIS), Strategic Reporting Unit (SRU). NECS Direct Commissioning Business Intelligence’. 2022
36. Public Health England. ‘Sentinel surveillance of blood borne virus testing in England: 2020’. 2021
37. Simmons, R and others. ‘Blood-borne virus testing in emergency departments – a systematic review of seroprevalence, feasibility, acceptability and linkage to care’. HIV Medicine. 2022
38. British HIV Association. ‘COVID-19 and shielding: advice for HIV clinicians, GPs and people living with HIV’. 2020
39. British HIV Association. ‘BHIVA encourages universal promotion of Undetectable=Untransmittable (U=U)’. 2018
40. British HIV Association. ‘Current Guidelines’. 2022
41. British HIV Association. ‘BHIVA guidelines on antiretroviral treatment for adults living with HIV-1 2022: non-technical summary’. 2022
42. National AIDS Trust. ‘HIV: Public knowledge and attitudes’. 2021
43. Iott, BE and others. ‘The impact of stigma on HIV testing decisions for gay, bisexual, queer and other men who have sex with men: a qualitative study’. BMC Public Health. 2022; volume 22 issue 1: page 471
44. Dhaliwal, JS and others. ‘Mental health and implications for antiretroviral adherence in a multiethnic Asian cohort’. Sexually Transmitted Infections. 2022; volume 98 issue 7: pages 497 to 502
45. NHS Digital. ‘NHS Outcomes Framework (NHS OF)’. 2021
46. EuroQol Group. ‘EQ-5D-5L’. 2021
47. Harding, R and others. ‘Positive Outcomes: Validity, reliability and responsiveness of a novel person-centred outcome measure for people with HIV’. HIV Medicine. 2022; volume 23 issue 6: pages 673 to 683
