Delivering the Five Year Forward View
Published 25 June 2015
The Five Year Forward View set out a clear direction for the NHS – showing why change is needed and what it should look like.
1. Personalised Health and Care 2020
1.1 Introduction
The Five Year Forward View set out a clear direction for the NHS – showing why change is needed and what it should look like.
Since the Five Year Forward View’s publication the National Information Board (NIB) has been examining how the NHS can harness the power of data and technology to transform citizens’ experiences of health and care services and deliver greater quality and efficiency.
In November 2014, the NIB published its framework for action - Personalised Health and Care 2020: Using data and technology to transform outcomes for patients and citizens. The framework for action considered the progress the health and care system has already made and set out proposals for the delivery of modern and efficient services. The framework has been adopted as Government policy.
Over the course of the last 6 months, NIB members have been working together to develop more detailed plans for delivery of the transformation of health and care described in Personalised Health and Care 2020. Stakeholders from across the health and social care system, including members of the voluntary sector, local government, clinical leaders and others have worked in partnership with NIB members in developing these plans.
Supporting the Government’s priorities for health and care and contributing to the Five Year Forward View’s vision of high quality health and care services that are sustainable and prevent people from falling into ill-health has been at the heart of this work.
1.2 Implementing personalised health and care 2020
The NIB translated the proposals set out in Personalised Health and Care 2020 into a series of work streams, broadly covering the following areas:
- enable me to make the right health and care choices
- give care professionals and carers access to all the data they need
- make the quality of care transparent
- build and sustain public trust
- bring forward life-saving treatments and support innovation and growth
- support care professionals to make the best use of data and technology
- assure best value for taxpayers and open up existing infrastructure
NIB work streams have developed roadmaps, setting out detailed evidence based plans for how the proposals for transformation through data and technology will be delivered and the benefits they will bring.
When assessing these plans to consider how they can make most difference to patients, citizens and professionals and also best contribute to meeting the quality and efficiency challenge in health and care, they fall into 6 clear priority domains for delivery.
These 6 domains are:
- enable me to make the right health and care choices: supporting digital services for patients and citizens
- transforming general practice
- out of hospital care and integration with social care
- acute and hospital services
- paper-free healthcare and system transactions
- data for outcomes and research
These 6 core priority domains for delivery are intended to become programmes that will help transform health and care services through data and technology. Over the course of the summer, the Department of Health working with NIB and other system partners will be leading work to define how much needs to be invested into which technology programmes to achieve this and to also better understand how these programmes will contribute to efficiency savings across health and social care.
The domains and examples of the programmes that will be delivered through them are described in the section below. This paints a picture of how data and technology will help transform health and care services over the next 5 years.
2. DOMAIN ONE: enable me to make the right health and care choices: supporting digital services for patients and citizens
The NIB vision is to transform health and care services to help citizens and patients make the right health and care choices. This domain is therefore a priority for the NIB as it both contributes to the efficiency and productivity challenge and also transforms the patient’s digital experience of and access to health and care services and transactions. Programmes will include:
- nhs.uk, including access to personal health records
- digital primary care services
- digital 111
- digital applications library
- support for self-care
- support for digital inclusion
At the heart of the domain, will be the development of nhs.uk into a new integrated health and care digital platform that will be a source of access to information, directorate, national services and locally accredited applications.
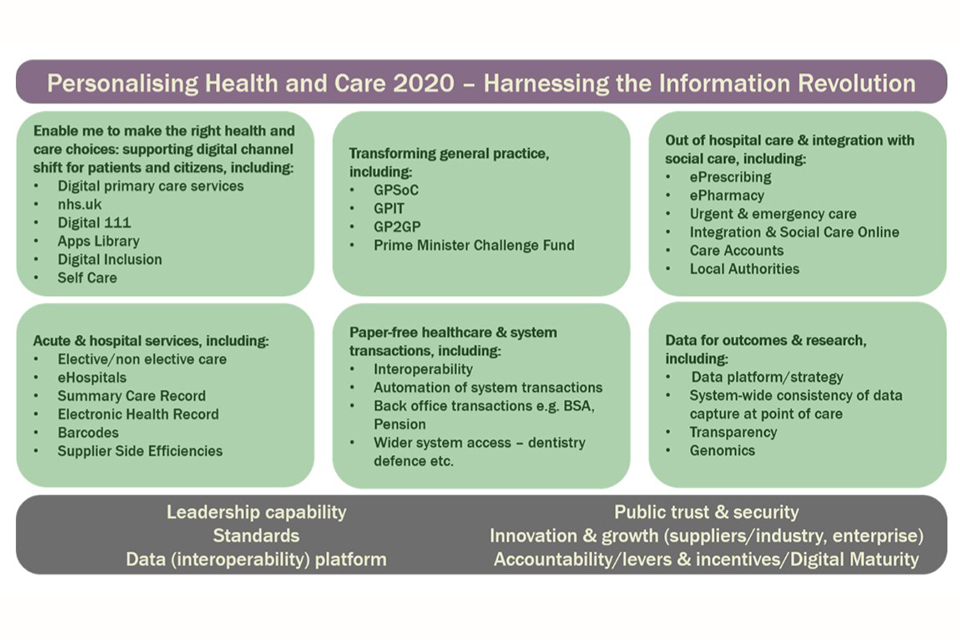
Personalising Health and Care 2020: show the six domains that make up the delivery strategy
Convenient digital transactions will be offered like ordering and paying for prescriptions, registering with GPs, claiming funds for treatment abroad, registering as an organ and blood donor and reporting the side effects of drugs. This new transactional focus will complement nhs.uk’s existing role as the authoritative source of condition and treatment information, NHS services and health and care quality information.
NHS.UK will also become the citizen’s gateway to the creation of their own personal health record, drawing on information from the electronic health records in primary and secondary care. This will enable citizens to communicate with clinicians and practices via email, secure video links and fill out pre-consultation questionnaires. They will also be able to include data from their personal applications and wearable devices in their personal record. Personal health records will be able to be linked with care accounts to help people manage their personal budgets.
The MyNHS data service on nhs.uk will be expanded to include new scorecards, expanded coverage of patient experience and regular themed reports. This will help people to make informed choices about where they get their health care from.
Through nhs.uk citizens will have access to a set of health and care digital applications which have been assessed by the health and care system to enable them to make the right health and care choices and support them looking after themselves better. This will be supported by a four-stage assessment process being launched later this year to make sure that the NHS is promoting only the best and most useful applications.
3. DOMAIN TWO: transforming general practice
The Five Year Forward View sets out the need for a new deal for GPs. The NIB aims to support this through transforming general practices’ experience of technology and digital services. Programmes in this domain will take forward:
- General Practice Systems of Choice (GPSoC)
- GP IT
- GP2GP
- Prime Minister’s Challenge Fund (PMCF)
Further procurement under the GPSoC will be used to stimulate the supply of new and innovative systems. In addition, new forms of ‘software-as-a-service’ clinical systems to support new providers of primary care services will be encouraged and the GPSoC framework will be reviewed as vehicle for change before it ends in April 2018.
Technology and digital services will support modern seven-day primary care. Citizens will be able to communicate with their general practitioner at their convenience via online communications. They will be able to register securely with a general practitioner and be able to change their primary care provider online.
4. DOMAIN THREE: out of hospital care and integration with social care
The changes through digital services and data that are outlined in the NIB plans will stimulate new models of patient-focused care, supporting a shift to more care being provided out of hospital. In this way, domain three will support NHS England’s New Models of Care Vanguard sites. It will also support the test bed initiative. Programmes in this domain will cover:
- ePrescribing
- ePharmacy
- urgent and emergency care
- integration with social care online
- care accounts
- local Authorities
Patients and carers will be given convenient ways to manage and better understand their medicines through digital services. They will be able to choose how and where they get their prescriptions, without the need for paper and be able to check information about their medicines, through simple barcodes. Connecting data to other digital applications will help remind people when to take their medicines.
111 and 111 digital will deliver a safe and effective online triage and consultation service for patients with urgent needs. This will be fully integrated with local services so that patients only have to tell their story once. Digital 111 will be part of the nhs.uk platform, allowing transactions to be conducted seamlessly by the citizen based on their clinically assessed need. In addition, people will be encouraged to use digital applications to record their health and care preferences, values and goals in advance of them needing urgent and emergency care.
There will be a programme to support those with social care needs to self-care, to plan and manage their care and finances and to connect to carers and peers. The programme will support the work of local government, and also involve the independent and voluntary sectors, and carers, who deliver the majority of care within England. This will explore the use of telehealth between care homes, primary and acute settings. It will also consider how digital personal care assessment, budgets, planning and commissioning can provide people with more choice and control about how their support needs are met, helping to improve their experience of social care.
5. DOMAIN FOUR: acute and hospital services
For secondary care, digital innovation offers considerable benefits in terms of driving efficiencies in day-to-day working and continued progress in key patient safety areas. Programmes in this domain will cover:
- elective/non elective care
- eHospitals
- summary Care Record
- electronic Health Record
- barcodes
- supplier side efficiencies
Better management of access to secondary care is essential to making best use of NHS resources. Providing citizens with the ability to choose where they go for treatment at a time convenient for them is an established commitment of the government. The redevelopment and design of the e-Referrals system will create a partnership between patients and professionals by helping patients compare services, complete referrals and book appointments online.
Digital initiatives like: providing a single source of information on referrals and bookings; providing a standard tool to support the management of health and social care referrals; simplifying the referral process and supporting national standards of integration and interoperability; issuing digital appointment reminders to citizens for their convenience and to minimise non-attendance and exploring the use of digital channels for pre and post-operative assessments, will all contribute to driving greater efficiency in hospital settings.
Asset tracking is increasingly regarded as an effective way of addressing inefficiencies. This type of solution enables a hospital’s wireless infrastructure to actively track assets through the use of Radio Frequency Identification (RFID) tags. This technology is enabling hospitals to reduce the financial impact of inefficiencies in three key areas – equipment utilisation; patient care and safety, and staff productivity.
Adoption of common digital and information standards is essential to effective digital service delivery and the NIB is proposing a set of common requirements – including use of the NHS Number as primary identifier of patients, adoption of the GS1 barcoding standard and SNOMED-CT among others – for implementation by all care providers.
6. DOMAIN FIVE: paper-free healthcare and system transactions
In a paper-free NHS and social care system, professionals will obtain information from across the health and care system to help make effective, efficient high quality decisions. Professionals will be able to find and use digital health and care information in a secure, timely and reliable manner. Domain five will include programmes that will support this joining up of the system (i.e. interoperability) around common digital and information standards including:
- interoperability
- automation of system transactions
- electronic Health Record
- Summary Care Record
- electronic medicines supply chain
- digital diagnostics
- back office transactions, e.g. BSA, pensions
- wider system access – dentistry, defence etc
The NIB plans to support interoperability though technology and data are underpinned by 2 overarching aims:
-
by 2018 clinicians in primary, urgent and emergency care will be operating without needing to use paper records
-
by 2020 all patient and care records will be digital, real time and interoperable
Local health and care economies will create joined up plans demonstrating how they will make viable progress towards the paper-free targets for 2018 and 2020. These digital roadmaps will be published by April 2016. Detailed guidance to CCGs, local authorities and providers regarding the core content of their local digital roadmaps will be published at the end of June 2015.
To ensure transparency on progress towards being paper-free in 2018 and 2020 a Digital Maturity Index is being co-produced with the health and care sector. This will enable individual providers and health and care economies to baseline and benchmark their current position and mark progress. It will assist local organisations and economies identify solutions to address the gap between their current reality and what making best use of digital technology delivers. The first data collection for the Digital Maturity Index, focusing on acute and mental health and aspects of information sharing, will begin this summer. The first Digital Maturity Index will be published in the autumn of 2015.
The Summary Care Record (SCR) provides information, extracted from the GP system, nationally for access across care settings. The core set of information includes details of medications, allergies and adverse reactions. An extended data set that is currently being introduced includes items such as of end of life preferences.
By March 2016, it will be a core requirement for all providers to have enabled access to SCRs. Work will also begin on the commitment to have 100% of pharmacies with access to the summary care record by March 2017.
By March 2016 the information available to clinicians in the SCR will be extended to include whether a patient has learning disabilities or suffers from dementia. This will improve the experience for these patients and prevent them or their carers having to repeat important information each time they interact with the NHS. Domain five will support system-wide priorities, for example, an end-to-end medicines supply chain and digital diagnostic services, with an initial focus on pathology.
7. DOMAIN SIX: data for outcomes and research
At present, health and care data is often fragmented, incomplete and inaccessible. Its full potential to inform what the system needs to do to deliver the government’s priorities for health and care and meet the challenges in the Five Year Forward View cannot be realised. Neither is it fully available to researchers to help them develop new medicines and treatments to benefit citizens and patients. The programmes in domain 6 will seek to address this and will include:
- data platform/strategy
- system-wide consistency of data capture at point of care
- transparency
- genomics
Subject to patient consent, high quality standardised data will be extracted from all parts of the NHS and care services. A standardised record will be generated at the end of every episode of care. Each of these records will follow the patient as they move through the NHS or social care, for example, from ambulance to A&E or from inpatient care to nursing home, with a copy being made available to a patient’s GP. These changes will lead to the capture of data which may spark further innovation and potential for efficiency and growth.
Considerable work is underway on major national genomics projects such as the 100,000 genomes programme, laboratory reconfiguration and wider National Institute for Health Research (NIHR) and research council activities.
A National Genome Informatics Network will be created to align work plans over the next 6 months and create a detailed assessment of how NHS genomic and pathology services can share genome or molecular data for the benefit of patients and research.
8. Enablers for digital healthcare
Common themes – for example, the development of standards for digital services; accountability; security - run through all 6 domains and will continue to be developed and led through the NIB where appropriate, working with the Department of Health and system partners.
Core to success across all 6 domains is making sure that leaders in health and social care fully understand how data and technology can enable efficient, high quality services, help people manage their own care and prevent them falling into ill-health. The NIB is developing programmes that will support health and care leaders in this.
Another key priority is the development of standards to ensure public trust is strengthened in the secure management of personal data. The National Data Guardian will support work by the NIB to develop proposals.
9. Contribution towards efficiency savings
The last 20 years have seen other industries use technology and digital channels to reduce costs whilst maintaining or improving customer experience. So far the health and care system has not taken full advantage of these opportunities. Personalised Health and Care 2020 set out transformational changes though data and technology that enable the health and care system to begin to do so.
Initial modelling indicates that technology could contribute to potential savings opportunities of between £8.3bn and £13.7bn a year by 2020 to 2021, between £1.8bn and £3.4bn of this could be achieved through enabling patients to make the right health and care choices.
Over the course of the summer the Department of Health will lead work with system partners to define the investment required to develop and deliver priority programmes and will continue to further examine the efficiency savings that can be delivered to be confident that data and technology are fully contributing to efficient and sustainable health and care services.
10. What happens next?
The NIB will seek wider views on plans to deliver the transformation of health and care described in Personalised Health and Care 2020 during July and August this year. This will be through a combination of working with and through the NIB member organisations and other partners in the health and care system, and also through holding a series of regional listening events. Plans will be refined to reflect these views. The plans will be subject to a greater level of scrutiny to ensure that their contribution to releasing efficiencies and resources into the system is robust and evidence based.
The NIB will publish its final roadmap and more details about the programmes that will deliver this in September 2015.
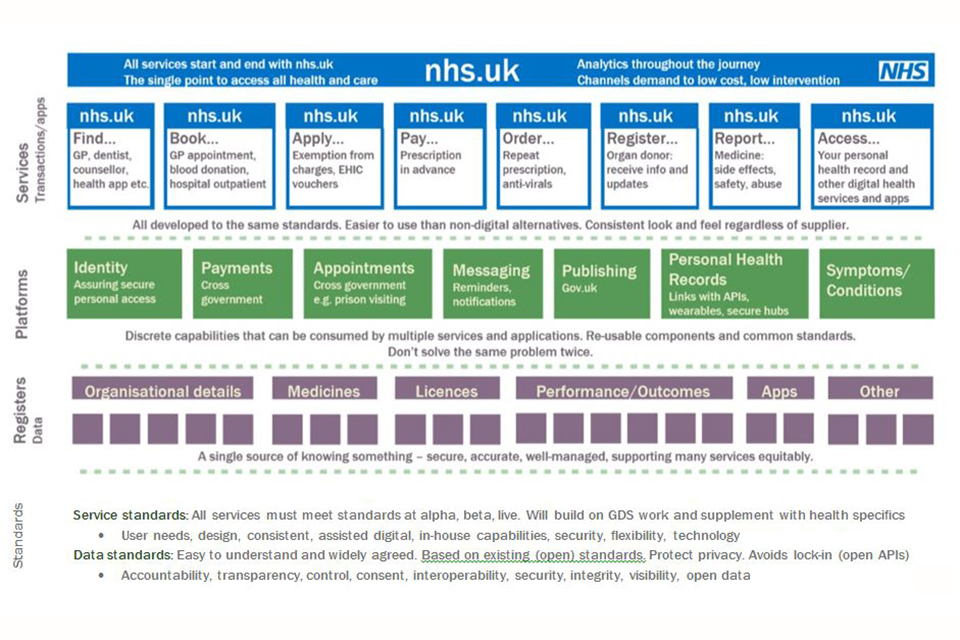
An outline of the nhs.uk vision
