Biological evaluation methods to assist in assessing the age of unaccompanied asylum-seeking children (accessible)
Published 10 January 2023
Interim Age Estimation Science Advisory Committee
October 2022
1. Executive summary
1.1. The interim Age Estimation Science Advisory Committee (AESAC) was commissioned to provide advice to the Home Office Chief Scientific Adviser on scientifically based methodologies that might assist with assessing the age of unaccompanied asylum-seeking children (UASC) whose claimed age is disputed and supplement the existing, Merton-compliant method of age assessment.
1.2. UASC require a date of birth (and therefore a known, or assigned, age) to access services for minors (under the age of 18 years), including health, education and identity documents. However, most UASC are unable to provide documentary evidence of their date of birth on their arrival in the UK, and some may not know their exact chronological age (time elapsed since birth).
1.3. Since January 2022, more than 500 children and young people have sought asylum in the UK, requesting access to, and protection within, the children’s social care system. This is a small proportion of the children and young people who will seek protection and care in 2022. Care standards require children to have age-appropriate provision in terms of their placement and education, and to meet their health needs.
1.4. There is a duty to protect children in care and the wider community, particularly in schools, from individuals who claim to be younger than they really are and who seek to gain inappropriate access to the care and care leavers system. There is a major safeguarding issue when adults are housed with children as was evidenced in the case of Ahmad Otak (R v Ahmad Otak [2012], BBC News, 2012). There is an equally important safeguarding issue when minors are incorrectly aged as adults and so inappropriately placed in adult facilities where they may be at risk. Therefore, it is imperative that the methods used to assess the claimed age are as robust, repeatable and accurate as possible.
1.5. Assessment of age for UASC in the UK, where a local authority doubts the age claimed, currently relies exclusively on the Merton-compliant process and there are four important considerations regarding this:
-
The Merton-compliant process has not been baseline tested to evidence either for accuracy or repeatability and the process is not uniformly applied.
-
The Merton-compliant process can be lengthy and stressful for the claimant, and places a significant resource burden on local authorities.
-
A large number of age assessments are challenged, resulting in significant impact on local authorities’ time and resources and causing a delay in processing.
-
Incorrect decisions have been made, sometimes with catastrophic consequences, when vulnerable children are inadvertently placed at risk of harm either from adults who are incorrectly assessed as children or when children are incorrectly placed into adult facilities.
Biological methods
1.6. The interim committee was asked to advise on methods that could be implemented within 12 to 18 months as a means to support the existing Merton-compliant process. As a result, this report focusses on biological methods utilising dental and skeletal development that have already been widely tested for the assessment of age in the UK and internationally in both the immigration system and the criminal justice system.
1.7. Assessment of biological age using teeth and bones is based on the analysis of maturational stages of development. Images taken of teeth and bones show the maturational stage that an individual has achieved and can be compared to reference images of individuals whose chronological age is known.
1.8. While all maturational changes happen in an essentially uniform way for most individuals, it is the timing of these changes that are important for age assessment. The difference in timing of maturation between males and females has been well documented, but there are many factors that can exert an impact on timing, such as socioeconomic factors.
1.9. While every effort should be made to use reference images that are representative of the group from which the individual being age assessed originates, it is not possible to match the background of every individual. As a result, an age range is usually presented taking into account differences influenced by many factors including ethnicity and socioeconomic impact. The committee propose assessing whether that range of ages encompasses the UASC claimed age and so reporting whether the claimed age was possible rather than assigning a specific age or age range. Of note, once development is complete, when the teeth or bones are fully mature, biological age assessment will give a minimum age only, set by the youngest age at which that maturational stage has been observed.
1.10. Any methodology used for the assessment of age should respect and prioritise the health and wellbeing of the individual, upholding their dignity and right to choose, and minimising any health risk, whether physical or psychological, to the individual being assessed. Experience within the committee identified that there may be many reasons why a UASC may choose not to give consent for biological age assessment that is not linked to concealment of chronological age.
1.11. The dental and skeletal methods proposed in this report are:
-
Radiography (x-ray) of the third molar (wisdom teeth)
-
Radiography (x-ray) of the bones of the hand and wrist
-
Magnetic Resonance Imaging (MRI) of the knee bones
-
MRI of the clavicle (collar bone)
1.12. There are strong views on the use of ionising radiation in the age assessment process and the interim committee has listened to and debated these arguments at length. However, the risk is recognised to be small and the benefits of a reliable age assessment are considerable for the ongoing health and wellbeing of the individual while minimising safeguarding risks.
1.13. The interim committee advocates the use of MRI for age assessment where possible and there is a growing body of peer reviewed research that provides confidence in the future use of MRI for assessment of the hand/wrist and third molar, although this will require further research.
Combining biological methods
1.14. It is key that methods used for age assessment have a low chance of misclassification, that is a low chance of a minor (age under 18) being assessed as an adult, or an adult (over 18) being assessed as a minor. Combining assessment of dental and skeletal development is important as it increases the accuracy of the approach, compared to assessment of these areas in isolation.
1.15. A triage approach is proposed in this report with the methods to be combined dependent on the sex and claimed age of the person being assessed. Development of the third molar is useful for assessing the age of males and females up to around 18 years of age. Development of the hand/wrist or knee can be used to assess the age of females up to around 16 years of age and males up to around 18 years of age. The clavicle displays the longest period of growth-related activity in the human body, and is therefore of particular value for assessing age of males and females from around 15 years up to around 25 years of age.
1.16. There is no method, biological or social worker-led, that can predict age with precision therefore, biological assessment of age should consider whether the age claimed by the UASC is ‘possible’ rather than be used to answer the specific question of how old that person is or whether they are under or over 18 years of age.
1.17. If the existing Merton-compliant process and biological assessments are carried out independently it would be possible to use a likelihood ratio approach based on the known development timeframe of teeth and bones. This approach could compare the likelihood of the age assigned following the Merton-compliant process being possible against the likelihood that the claimed age is possible and show which carries stronger support.
1.18. The committee advocate a likelihood ratio approach. The committee acknowledge that there is uncertainty in the data used to predict the maturation points of the teeth and bones particularly as there is limited data on UASC population groups. However the likelihood ratio method offers a logical and consistent summary of the evidence and permits greater confidence in the assessment of whether the claimed age is possible.
1.19. Taken together with the existing Merton-compliant age assessment process, utilising a combination of biological age assessment methods would enhance confidence in the Merton process when determining whether the claimed age for a UASC is possible.
Recommendations
1.20. The interim committee make the following recommendations regarding the use of biological methods to assist with the assessment of the age of unaccompanied asylum-seeking children.
Recommendation 1: If biological age assessment is implemented it should be used to assess whether the age claimed by UASC is possible.
Recommendation 2: Research into the accuracy and reliability of the Merton-compliant process should be undertaken as a piece of urgent baseline research.
Recommendation 3: Any methodology used for the assessment of age must respect and prioritise the dignity of the individual being assessed and should minimise physical or psychological harm.
Recommendation 4: Biological age assessment can be carried out using an appropriate combination of dental and skeletal methods; assessment of development of the third molar using radiography, radiography of the hand/wrist or MRI of the knee, and MRI of the clavicle.
Recommendation 5: The use of ionising radiation must be limited, with the ultimate aim of eradicating its use. Continuing research into the use of non-ionising imaging, such as MRI, should be supported.
Recommendation 6: Where possible, the radiation dose should be limited through the use of recent pre-existing images, providing consent for the use of these images for age assessment had been freely obtained.
Recommendation 7: Further research into the impact of socioeconomic factors and their effect on growth and maturational timing, particularly those factors likely to be experienced by UASC, should be supported.
Recommendation 8: Dental and bone images should be acquired by those with the relevant training and expertise and reported by those with expertise in interpreting images for age estimation.
Recommendation 9: A guide should be developed on how to deal with those situations where there is a discrepancy between the claimed/suspected age and the biological or social worker-led evaluation outputs which makes clear what weight should be placed on different sources of information.
Recommendation 10: Consider adopting a likelihood ratio approach, using biological evidence of age, to compare the weight of evidence or ‘support’ for the Merton assigned age versus the claimed age.
Recommendation 11: UASC should be provided with clear information explaining the risks and benefits of biological evaluation in a format that allows the person undergoing the process to give informed consent and no automatic assumptions or consequences should result from refusal to consent.
Recommendation 12: Further research to gauge the differential impact of the proposed age assessment processes on UASC with respect to the protected characteristics in the Equality Act 2010 should be undertaken.
Recommendation 13: Research into biological age assessment methods based on a wide range of ethnic or geographical sub-groups to confirm and improve accuracy and applicability of these methods should be supported.
Recommendation 14: A watching brief should be maintained over the development of emerging age estimation methods including, but not restricted to, facial images and DNA methylation.
2. Introduction
2.1. The interim Age Estimation Science Advisory Committee has produced this report in response to a commission from the Home Office Chief Scientific Adviser to provide advice on scientific methodologies that might assist the existing Merton-compliant method of assessing the age of unaccompanied asylum-seeking children (UASC) whose age is contested.
2.2. Specifically, the committee was asked to focus on methods that could be implemented within the next 12 to 18 months and would assist with estimating whether a person was likely to be under or over 16 or 18 years of age.
2.3. The advice in this report focuses on:
a) guidance on the ethical use of medical imaging techniques
b) consideration of the accuracy, reliability and the likely range of estimated ages
c) consideration of any medical or ethical risks to the person being assessed and whether these risks would apply equally to all groups who may be assessed
d) consideration of any benefits, when compared to the existing method, and whether those benefits would apply equally to all groups who may be assessed
e) whether methods should be used in combination or sequentially
f) consideration of requirements for implementing these techniques.
2.4. This report first outlines the current position in the UK regarding age assessment and sets out the need for change. The report then introduces methods for biological assessment of age that could be implemented in the timeframe requested and are supported by evidence. In addition, the report recommends a probabilistic approach for assessing whether the Merton assigned age or the disputed claimed age is more likely.
2.5. Throughout this report the committee has assumed that Merton-compliant assessments will continue and that biological assessment methods will be supplementary and distinct. While the findings from the existing Merton-compliant process may be combined with the findings from the biological assessment to form a holistic assessment of age, the likelihood ratio approach proposed in this report requires the existing Merton-compliant process to be completed at least to the point of considering the age to assign before factoring in the biological assessment results.
2.6. The interim committee recommends, and has assumed, that UASC entering the UK would remain in the UK until their age is assessed and asylum application processed accordingly.
3. Background
The current position
3.1. UASC require a date of birth (and therefore a known, or assigned, age) to access services for minors (under the age of 18 years), including health, education and identity documents. However, most UASC are unable to provide documentary evidence of their date of birth on their arrival in the UK, and some may not know their exact chronological age (time elapsed since birth).
3.2. Many UASC without documentation are obviously children even if they incorrectly present as adults, and some are very clearly adults claiming to be children, and these cases are handled by either Immigration Officers at the point of entry or social workers once the individual is placed with a local authority. However, in some cases there remains doubt over whether they are an adult or a child (or they are thought to be a child, but potentially a different age than claimed), and in these circumstances an age assessment is required, to establish whether they could be the age that they claim to be or are likely to be older or indeed younger. Until an age assessment can be performed, the person is treated as a child (Home Office guidance on assessing age, 2022) and a swift resolution is imperative as there are important safeguarding issues to be addressed.
3.3. All asylum claimants being treated as UASC are referred to the relevant local authority who will undertake an age assessment if they have reason to believe that the claimed age may be incorrect based primarily on the physical appearance and demeanour of the young person.
3.4. A local authority age assessment is currently undertaken by two suitably trained social workers, and typically involves a series of interviews with the young person. The local authority may also consider other relevant information, such as views from a foster carer, teacher, psychologist, police officer, paediatrician or other relevant practitioners to assist them in their deliberations. The age assessment process can take weeks or months to reach completion depending on availability of resources, interviewers, interpreters and the co-operation of the age-disputed person. There is no uniform approach to a ‘social-worker-led’ age assessment, however the courts have provided guidance and minimum standards that must be applied. Much of the guidance was set out in B v London Borough of Merton [2003] EWHC 1689 (Admin) and so the assessments are commonly referred to as being ‘Merton-compliant’.
3.5. Following a Merton-compliant age assessment and review of all relevant and available information, a ‘minded to’ meeting is held with the young person in which the social workers explain the age they are ‘minded to’ assign to the young person, who is given the opportunity to provide further evidence to challenge the assigned age if they so wish. If the claimed age is accepted the young person is given a specific date of birth, based on their given day and month of birth if known or 1 January if not, and a year of birth to match the claimed age.
3.6. Where an individual disagrees with the outcome of a Merton assessment, the existing mechanism to challenge that finding is to request a judicial review of the decision. This process is set out in Figure 1.
Figure 1: Simplified outline of existing steps where claimed age can be accepted or disputed.
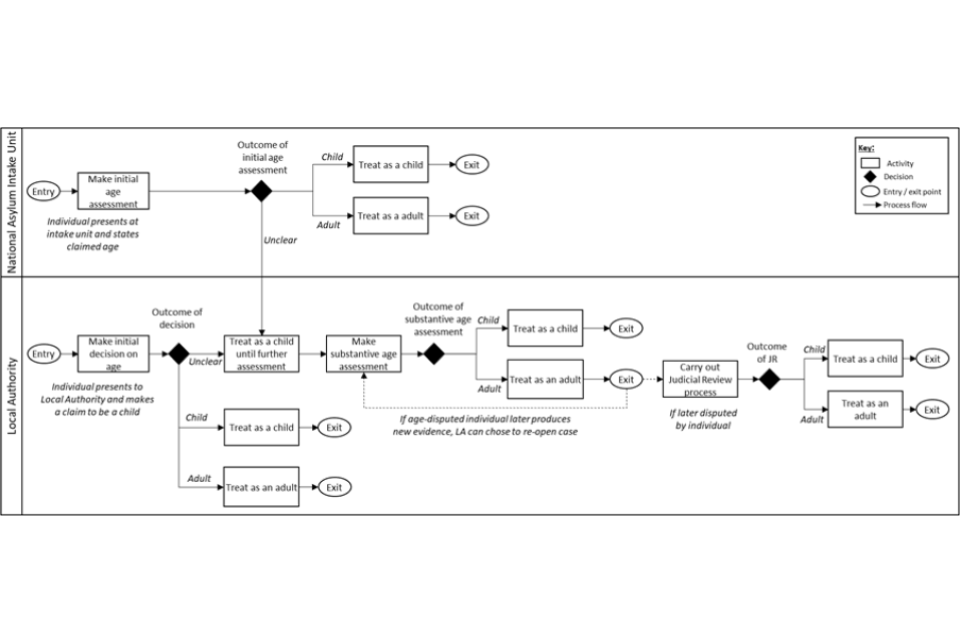
Flowchart showing the process described above.
3.7. In age assessment judicial review proceedings, there is no burden of proof on either party and the court’s task is to decide the issue on the ‘balance of probabilities’ in light of all the evidence. This means that the evidence for one position (for example, an alternative age to the one claimed) must be greater than the evidence in support of the opposing position (the claimed age being correct) for it to be accepted by the court.
3.8. Outside of the UK a number of countries have adopted scientific methods to assist with assessing age; methods such as radiography of the teeth, clavicle and wrist are already in use across a number of EU nations. The Second Edition of the European Asylum Support Office Practical Guide on age assessment (2018) provides an overview of the methods in use in the EU+ states. While the methods in use are known, the detail of how they are used in age assessment and how they are combined and weighted compared to other evidence, is less clear.
The scale of the issue
3.9. Since January 2022, more than 500 children and young people have sought asylum in the UK, requesting access to, and protection within, the children’s social care system. This is a small proportion of the children and young people who will seek protection and care in 2022.
3.10. Children and young people require care and protection to be provided in a timely way. The mandate of the National Transfer Scheme (2021) increased the number of offers from local authorities to take new arrivals, but the scheme has not been able to meet immediate demands in terms either of placements or timeliness. In a minority of cases unaccompanied asylum-seeking children will be temporarily accommodated in one of the hotels set up for the care of minors until a suitable placement at a local authority can be found.
3.11. Taking young people into care when age is unknown or uncertain is one of the main areas of concern for local authorities. Care standards require children to have age-appropriate provision in terms of their placement and education, and to meet their health needs. The appropriateness of the choice of placement is heavily age dependent, and for those whose age is disputed, this can, and does, build in delay. This is despite the legal requirement to treat all individuals who claim to be minors as such, until their age can be determined. The reality for local authorities is that their safeguarding duties are significantly tested when they may have adults claiming to be children in their care, and undertaking Merton-compliant age assessments is time consuming, challenging, costly and in many cases leaves a degree of uncertainty for all concerned.
3.12. Establishing a National Age Assessment Board (NAAB) is welcomed but simply progressing with a sole source of assessment – the existing Merton-compliant process – will not address all the current challenges.
The need for change
3.13. The relationship between chronological age (time elapsed since birth) and biological age (changes to body tissues with age), psychological age (maturation of the mind) or behavioural age is not, and likely never will be, a perfect correlation. The reasons for this are well documented and include general health, genetics, nutrition and life experiences. Therefore, it must be accepted that there is no infallible method for either biological or social-worker-led age assessment that will provide a perfect match to chronological age.
3.14. Therefore, one must question the veracity of assigning a specific age when, based on the ‘balance of probabilities’ and inherent limitations, it is arguably more relevant to ask the initial question of whether the claimed age is ‘possible’ rather than ‘how old is the person?’. This also supports the premise of ‘benefit of the doubt’.
Recommendation 1: If biological age assessment is implemented it should be used to assess whether the age claimed by an age-disputed person is possible.
3.15. There is an urgent practical need to undertake age assessment that will give the greatest confidence in supporting or contesting the claimed age, within the limits of current capabilities. This is essential to provide mandated support and critical safeguarding for those who legitimately seek asylum and who claim to be children, but who do not have documentary evidence of their birth date.
3.16. Furthermore, there is a duty to protect children in care and the wider community, particularly in schools, from individuals who claim to be younger than they really are and who seek to gain inappropriate access to the care and care leavers system. There is a major safeguarding issue when adults are housed with children as was evidenced in the case of Ahmad Otak (R v Ahmad Otak [2012], BBC News, 2012). There is an equally important safeguarding issue when minors are incorrectly aged as adults and so inappropriately placed in adult facilities where they may be at risk. Therefore it is imperative that the methods used to assess the claimed age are as robust, repeatable and accurate as possible within current capabilities.
3.17. It is important that an individual who claims to be a child and whose age is not contested is given swift access to the support they need. However, Home Office data show that 71% of asylum applications from UASC were from applicants who claimed their age to be 16 or 17 years, where a reliable evaluation is more challenging. This causes concern and raises the question of whether biological assessment methods could assist with assessment of this challenging age range by providing additional information to support decision makers.
3.18. The current process for age assessment for UASC, where a local authority doubts the age claimed, has relied almost exclusively on the expertise and subjective opinions of social workers following the Merton-compliant process. There are four important issues that impact on reliance on this as a standalone method for age assessment in UASC cases:
1. The Merton-compliant process has not been baseline tested to evidence either its repeatability or its accuracy, and the process is not uniformly applied.
2. The Merton-compliant process can be lengthy, stressful for the claimant, and places a significant resource burden on local authorities.
3. A large number of age assessments are challenged, resulting in a significant impact on local authorities’ time and resources and causing a delay in processing.
4. Cases have shown that incorrect decisions have been made, sometimes with catastrophic consequences, when vulnerable children are inadvertently placed at risk of harm either from adults who are incorrectly assessed as children or when children are incorrectly placed into adult facilities.
3.19. Baseline testing of the Merton-compliant process would allow assessment of its accuracy and repeatability and allow the impact of introducing biological age assessment to be judged.
Recommendation 2: Research into the accuracy and reliability of the Merton-compliant process should be undertaken as a piece of urgent baseline research.
3.20. Biological assessment methods have been tested repeatedly in the adversarial environment of the criminal courts; the committee expect that the introduction of biological approaches would enhance confidence in the Merton process when determining whether the claimed age for a UASC is possible.
3.21. It should be remembered that confirmation or otherwise of the claimed age has long-term implications for the individual, and it is essential that such a process is undertaken in an optimal fashion given the limitations of current technologies and approaches. Reliable age assessment ensures that claimants will have lifelong access to appropriate services at the right time in their life, including medical screening programmes and state pensions.
4. Biological age assessment methods
4.1. The interim Age Estimation Science Advisory Committee considered approaches based on appropriate scientific methodologies that could be implemented within 12 to 18 months as a means to support the existing Merton-compliant interview process. The methods that could be implemented in this timeframe are those that use imaging to assess dental and skeletal development.
4.2. Alternative and emerging methods such as facial age estimation (Yoti, 2021), and DNA methylation (Wu et al., 2019), were considered but as more extensive evaluation would be required, these methods were not deemed suitable for short-term implementation. Such potential future methods, improvements to existing methods and baseline testing of the Merton-compliant process should be a matter for the full committee to consider once it is established.
Use of physical development to assess age
4.3. While there are many areas of the body that can be utilised for age assessment, the interim committee proposes the following areas (teeth, clavicle, and hand/wrist or knee) that separate into two well-defined categories – dental age (teeth) and skeletal age (bone). These areas have been shown to have a significant research and publication credibility and provide a consistent age range over which changes occur.
4.4. Although there is research into other areas of the body for age estimation, including the iliac crest (pelvis), examination of this area requires radiography which was deemed too invasive due to the close proximity of radio-sensitive tissues (gonads). Further, the level of available data for magnetic resonance imaging (MRI) for this body region is currently insufficient and therefore this was discounted along with other areas of the body. The committee has relied on areas and methods that have been repeatedly tried and tested and shown to have consistency.
4.5. Maturational changes in the dentition include the development, eruption, subsequent loss and replacement of deciduous (baby) teeth with the development, eruption and maturation of permanent teeth. These changes occur within recognised age ranges and in a well-documented pattern.
4.6. Maturational changes in the skeleton include changes to the shape, relative size and extent of fusion of different components of growing bones (Cunningham et al., 2016). These changes occur in a well-documented pattern and within well-established time frames.
4.7. Age assessment methods compare dental and skeletal maturation markers in a young person to those recorded in reference datasets of children and adults of known age and ancestry.
4.8. Older datasets were often presented as ‘atlases’ and were frequently sourced from historical longitudinal studies of child growth based on radiographic images. More recent datasets are created from images taken from individuals of known age and populations on a cross-sectional basis and tend to use existing medical images or be MRI sourced (Black, et al., 2016).
4.9. Biological age is based on the analysis of maturational stages, each of which can be imaged and linked to a range of chronological ages rather than a single definitive age. The one exception is the final stage of maturation, which represents the fully mature adult state. In this final stage the lower limit for an individual’s chronological age is set by the youngest age at which that stage has been observed, but there is no upper limit as the stage applies to all individuals who have reached maturity. The chance of an individual having reached the mature stage increases with age in a way that can be visualised as a probability plot and estimated using binomial regression.
4.10. In determining the methods for inclusion in this report the committee considered the reliability of the methods available, the chance of a minor (age under 18) being incorrectly assessed as an adult, and the chance of an adult (aged 18 and over) being incorrectly assessed as a minor.
Imaging modalities
4.11. Based on a substantial body of research published in the peer reviewed scientific literature, age assessment based on both dental and skeletal development is generally considered via four recognised imaging modalities: radiography (x-ray), computed tomography (CT), magnetic resonance imaging (MRI) and ultrasound (US).
4.12. The interim committee advocates that any methodology used for the assessment of age should respect and prioritise the dignity of the individual being assessed and should minimise physical or psychological harm.
Recommendation 3: Any methodology used for the assessment of age should respect and prioritise the dignity of the individual being assessed and must minimise physical or psychological harm.
4.13. The use of US is not included in this report as the volume of peer reviewed literature for age assessment is insufficient to have confidence in its use. There are also practical issues with the reproducibility of the methodology, heavy reliance on the experience of a small number of experts, inconsistency of assessments, variation in interpretation of images, and poor results from those with higher body mass.
4.14. In line with the committee’s priority of minimising harm, the use of CT is also not advocated because of the levels of radiation involved (see Table 1).
4.15. Therefore, for the purposes of this report, only radiography and MRI were considered as possible imaging methods.
4.16. MRI is the preferred imaging method due to its safety through the absence of ionising radiation and there is sufficient evidence to support the use of MRI for assessment of age using the knee and clavicle. However, it should be acknowledged that MRI is not suitable for all individuals, for example if they have significant metal or dental implants or in cases where the process of MRI is found to be distressing through claustrophobia or an aversion to noise.
4.17. Radiography is the most common means of imaging dental development and there is a long history of age assessment using radiography of the hand/wrist. As a result, most data on age assessment using teeth or the hand/wrist are based on radiographic images (x-rays).
4.18. There has been some promising research undertaken using MRI to visualise the third molars (De Tobel et al., 2017a, 2017b; Guo et al., 2015; Widek et al., 2019). However, it is the view of the committee that there is as yet insufficient research undertaken to demonstrate the validity of MRI to allow this method to be used with confidence within the next 12 to 18 months. In addition, a head and neck MRI would be required if dental analysis was to be undertaken in this way, which could cause distress in some individuals, as it can be a claustrophobic experience.
4.19. In terms of the hand/wrist, the maturation of the distal radius in the wrist is visualised in much greater detail using MRI, and a suitable staging system has been developed by Krämer et al., (2014), merging the systems of Kellinghouse (2010) and Schmeling (2004). Research continues to be undertaken in this area and MRI may provide an alternative method for assessing age using the hand/wrist in the future.
4.20. Given the importance of combining methods of age assessment to improve accuracy and the need for further research into the use of MRI of the third molars and hand/wrist to assess age, radiography should be considered to image the third molars and hand/wrist at this time.
Recommendation 4: Biological age assessment can be carried out using an appropriate combination of dental and skeletal methods; assessment of development of the third molar using radiography, radiography of the hand/wrist or MRI of the knee, and MRI of the clavicle.
4.21. It should be noted that the hand/wrist can be held away from the body when exposed to radiation for imaging purposes and that the radiation exposure required for a radiograph of the hand/wrist is very low (see table 1).
4.22. MRI of the knee can also be used as an alternative for radiography of the hand/wrist as the range of ages assessed by the hand/wrist and the knee are similar.
4.23. The radiation dose for visualisation of the third molars has been shown to be reduced by up to a third by the use of sectional orthopantomograms (OPG) compared to full OPGs (Benchimol et al., 2018). The radiation dose can be reduced further by the use of the extra-oral bitewing setting on an OPG machine (Little et al, 2020).
4.24. The risk of harm from radiography of the teeth or hand/wrist is minimal when compared to the lifelong benefits that could result from a swifter and more accurate age assessment in terms of both safeguarding and wellbeing. However, the interim committee urges a move away from the use of radiography as soon as the research evidence makes it feasible to do so.
| Source of exposure | Average radiation dose (mSv) |
|---|---|
| Extremity x-ray (such as wrist or limb) [1] | Less than 0.001 |
| Dental x-ray (intra oral) | 0.005 |
| Panoramic dental x-ray (full orthopantomogram, OPG)[2] | 0.018 |
| Transatlantic flight | 0.08 |
| UK average annual background radiation dose | 2.7 |
| Computed tomography (CT) chest scan | 6.6 |
| Annual exposure limit for nuclear industry employees | 20 |
| Acute radiation effects, including nausea and reduced white blood cell count | 1,000 |
Table 1: Radiation dose in millisieverts (mSv) information from Public Health England, 2011, except; Radiologyinfo.org, 2021[1] and Benchimol et al., 2018[2].
4.25. Steps should be taken to ensure that the use of radiography is kept to a minimum, with the ultimate aim being to eradicate its use.
Recommendation 5: The use of ionising radiation in age assessment must be limited, with the ultimate aim of eradicating its use. Continued research into the use of non-ionising radiation imaging, such as MRI, should be supported.
4.26. During routine medical/dental assessment of UASC dental radiographs may already have been taken. Where recent images, most likely dental, already exist that would be appropriate for age assessment, these could be used, removing the need for additional images to be taken. Consent for this use would be required and the issue of consent is addressed in section 9.
Recommendation 6: Where possible, the radiation dose should be limited through the use of recent pre-existing images, provided consent for the use of these images for age assessment had been freely obtained.
4.27. It is recognised that MR imaging is more costly than radiography, and as NHS MRI equipment is in heavy clinical demand, use of commercial suppliers should be considered.
Dental age assessment
4.28. Dental development is a reasonably reliable means of age assessment throughout childhood but by the late teens, assessment of age relies almost exclusively on the maturation of the third molars (wisdom teeth). It is possible to assess an age range from third molar development in adolescence and young adults with a standard deviation of around two years for both males and females (Liversidge and Marsden, 2010). It is of value to note that dental maturation is reported to be less affected by disadvantageous environmental, social and health conditions than skeletal age and so the two approaches are frequently used together to capitalise on the semi-independent combinatorial benefits (Elamin and Liversidge, 2013).
4.29. Maturation of the roots of the third molars is reported to occur earlier in males than females, in contrast to the rest of the dentition where maturation occurs earlier in females than males (Liversidge, 2008; Thevissen et al., 2010; Thompson, Anderson and Popovich, 1975).
4.30. Assessment of the maturity of the third molars is usually performed using the mandibular (lower jaw) third molars because of the larger volume of research data available for these teeth compared to the maxillary teeth (upper jaw). Only one mandibular third molar is needed for assessment as development is generally comparable on the left and right sides. However, both sides are imaged because if a difference is noted, the tooth on the less developed side is assessed to give the benefit of the doubt. In addition, if the root apices of the third molar on one side are curved and therefore unclear, the opposite side third molar can be assessed.
4.31. Once the third molar has reached maturity, age can no longer be assigned as it is the presence of active maturation that is an indicator of chronological age. While the earliest that maturity has been observed is around 14 years for both males and females, it is accepted in the peer reviewed scientific literature that this method is useful for assessing age up to 18 years.
4.32. Development of the third molar is visible by examination of radiographs taken either as intra-oral images or extra-oral images via an orthopantomogram (OPG) which provides a swift panoramic scan of the dentition (taken in less than 30 seconds).
4.33. Extra oral radiographs are a more comfortable alternative to intra-oral radiographs. Where dental radiographs are not already available for an individual, sectional OPGs or extra-oral bitewing radiographs taken using an OPG machine would reduce the radiation dose compared to a full panoramic OPG (Benchimol et al., 2018 and Little et al., 2020).
4.34. Maturity of the third molar is illustrated by Demirjian stage H when the apical end of the root canal is completely closed and the periodontal membrane has a uniform width around the root and the root apex (Demirjian et al., 1973) – see Figure 2.
Figure 2: Two orthopantomograms with the individual’s left mandibular third molar circled. The upper image, taken from a female aged 13, shows an immature third molar with roots not fully developed. The lower image, taken from a male aged 18, shows a mature third molar where root growth has ceased (Demirjian stage H).
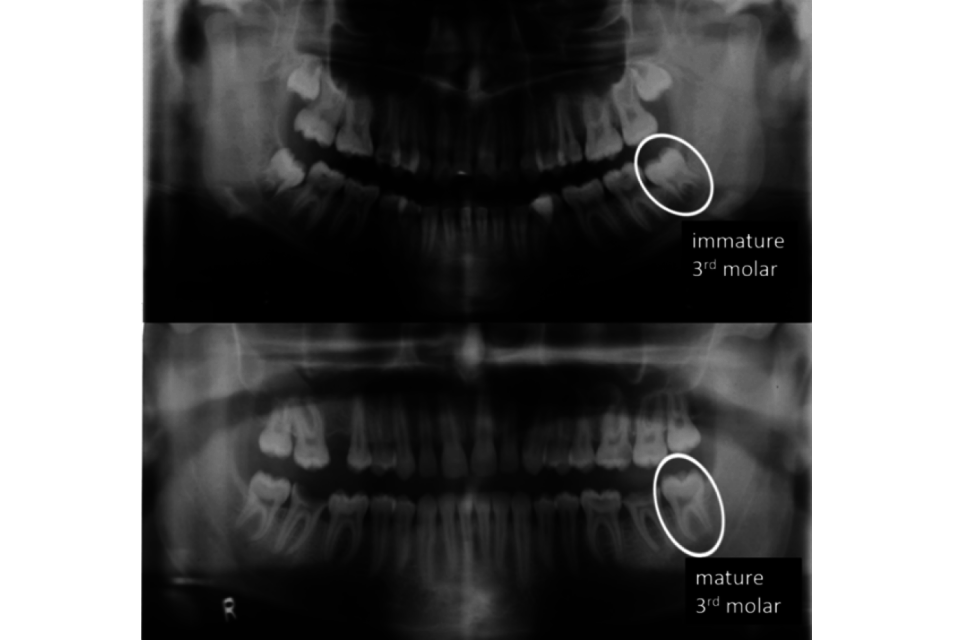
Orthopantomograms as described above.
Accuracy and repeatability
4.35. The specific standards recommended to assess age using the third molars are those with an appropriate sample size (particularly those including individuals aged between 15 and 21 years), that tabulates the proportion of individuals with the mandibular third molar in Demirjian stage H per year of age (Duangto et al., 2017; Johan et al. 2012; Kasper et al., 2009; Lee et al., 2009; Pinares Toledo et al., 2021; Uys et al., 2018).
4.36. There is variation in the timing of the maturation of the third molars and the graph in Figure 3 shows the distribution of the ages at which maturation is achieved in the mandibular third molar in males from seven different population groups. The figure shows how the percentage of mature individuals in each group increases with age, rising from 0% in late puberty to 100% in the third decade of life. There is considerable variability between groups – the youngest individuals reaching maturity are aged under 17 in American Hispanics whereas in Thailand they are over 17. At age 18 the proportions with mature third molars vary ten-fold from 3% to 30%. The point where 50% of individuals have reached maturity, the median age at which maturity is reached, ranges from 18.7 years in Chile to 20.8 years in Thailand, fully two years later (see raw data in Appendix 2).
Figure 3: Seven studies showing the proportion of males at different ages where their mandibular third molars have reached Demirjian stage H. The median age of reaching stage H is between 18.7 and 20.8 years, and the proportions of individuals who mature by age 18 vary from 2% to 31%. The curves were estimated by probit regression, where each curve corresponds to an underlying regression line defined by its intercept and slope. The values of intercept and slope by study, for this and other figures, are in Appendix 2.
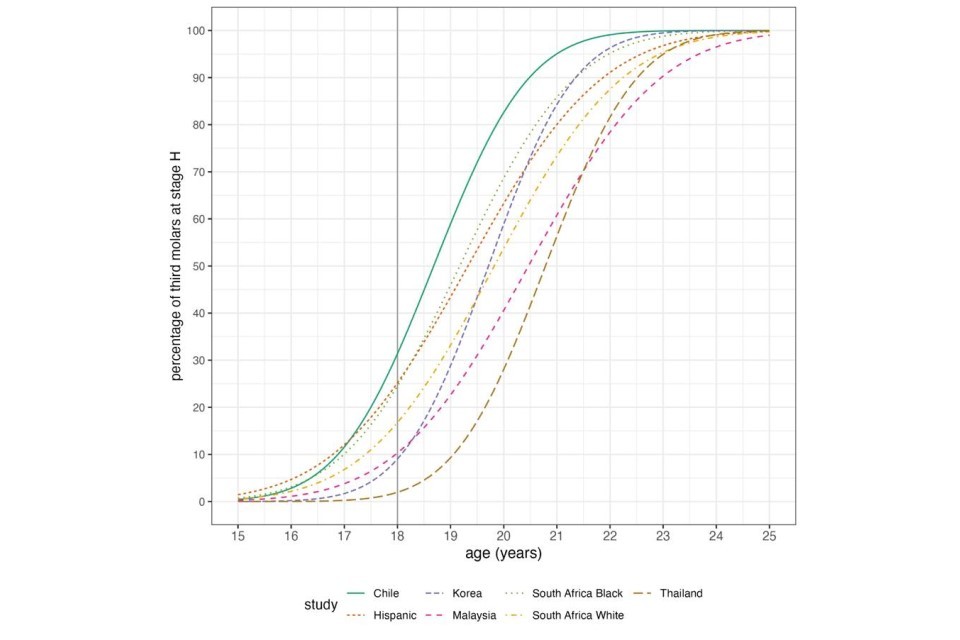
Graph showing data described above.
4.37. It is possible to assess age throughout the adolescent period with a standard deviation of 1.5 to 2 years for both females and males (Levesque et al., 1981).
Assessment of the hand/wrist
4.38. Skeletal or bone age assessment relies on the maturation of bones, before, during and after puberty. Different parts of the skeleton mature at different rates and times, and differ between males and females, with females maturing some two years earlier than males on average. This means that any methodology utilised for skeletal age estimation must take account of biological sex.
4.39. When assessing children’s development, paediatricians and radiologists may use software such as BoneXpert (BoneXpert.com, 2019) to give an automated bone age estimation based on development of the bones in the left hand and wrist. This software was developed specifically for assessing childhood development and not for age assessment. Caution is advocated in the use of a methodology that is not designed for the purpose to which it is applied and against which it has not been tested adequately. Therefore, further validation of the approach is advocated before it could be considered for age assessment in UASC.
4.40. Use of a radiograph of the hand/wrist to assess age is based primarily on maturation of the small bones in the wrist (carpals), the long bones in the palm (metacarpals) and fingers (phalanges), and the wrist end of the two long bones of the forearm – the radius and ulna (see Figure 4). While convention states that the left hand/wrist should be used, research has shown that either side of the body can be used interchangeably (Hackman and Black, 2012).
4.41. Maturation takes the form of changes to the shape and relative size of the bones, and the degree of fusion between the epiphysis (at the end of the bone) and the diaphysis (the bone shaft). The epiphysis and the diaphysis generally develop separately before fusing once maturity is reached (see Figure 4 which shows separate epiphyses in the image of the immature hand and wrist (A) but which are fused to the diaphysis in the image of the mature hand (B)).
4.42. These visible changes occur over a well-documented age range and can be correlated with chronological age using a reference dataset which allows comparison between the appearance of the bones seen in the radiograph and the appearance that would be expected at known ages.
4.43. The last bone to mature is the distal radius where fusion is complete by around 16 years in females and 17 to 18 years in males.
Figure 4: Radiographs of the hand and wrist of a female aged 10 years (A) and a female aged 17 years female (B) showing the bones and the epiphyses, the ends of long bones that initially grow separately from the shaft.
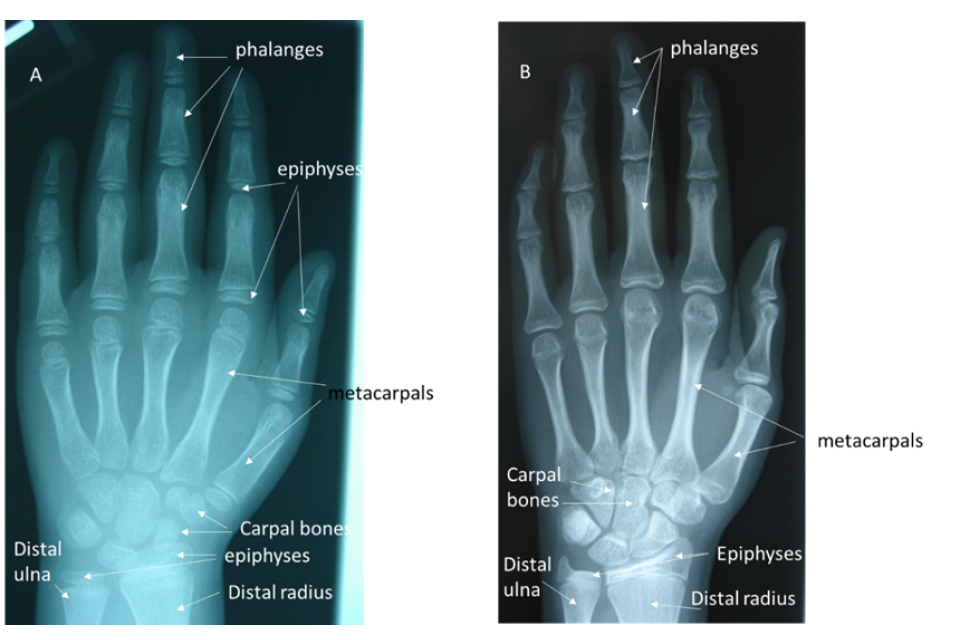
Radiographs described above.
4.44. The reference dataset that has been most widely used for age estimation of individuals from a hand/wrist radiograph is the Greulich and Pyle atlas (1959) since it includes comparison images of those who have reached maturity, where the radiographic appearance of the distal radius matched age 19 of the atlas (stage GP 19). It is an atlas that has been tested repeatedly and has continued to demonstrate reliability and accuracy in different populations across the last six decades and has been shown to still be applicable to modern populations (Groell et al., 1999; Hackman and Black, 2013; Jimenez-Castellanos et al., 1996; Tisè et al., 2011; Van Rijn et al., 2001).
4.45. The timing of the final maturational stage of the distal radius means that this approach has limited value in assessing a male who is aged 18 years or over and a female who is aged 16 years or older, since it is around this age that maturity is reached. A radiograph of a mature hand and wrist would only permit an expert to say that the individual was skeletally mature in this region but not how much time had elapsed since maturity was reached. Therefore, it is the presence of immaturity that is of discriminatory value and something that would be most likely seen if the male was younger than 18 years or the female was younger than 16 years. However, the presence of a mature distal radius does not rule out a claimed age of 17 years in a male.
Accuracy and repeatability
4.46. Studies have shown that final maturation of the distal radius occurs at around age 18 in males. A study by Thodberg and Martin (2016) used data from 119 boys from the First Zurich Longitudinal Study, who had a hand-wrist radiograph taken each year on their birthday from 3 to 19 years. This showed that 28% were mature by age 18 (matching stage GP 19 of the Greulich-Pyle atlas), around 50% by age 18.7, 62% by age 19 and 89% by age 20 (see Figure 5).
4.47. It is possible to assess age from hand/wrist images throughout the adolescent period with a standard deviation of between 0.3 and 1.4 years for females and 0.2 and 2 years for males (Hackman and Black, 2013; Chiang et al., 2005; and Tisè et al., 2011).
Figure 5: First Zurich Longitudinal Study (Thodberg and Martin, 2016). The percentage of 119 males whose hand-wrist x-rays at ages 18.0 and 19.0 had reached GP 19 – curve fitted by probit regression.
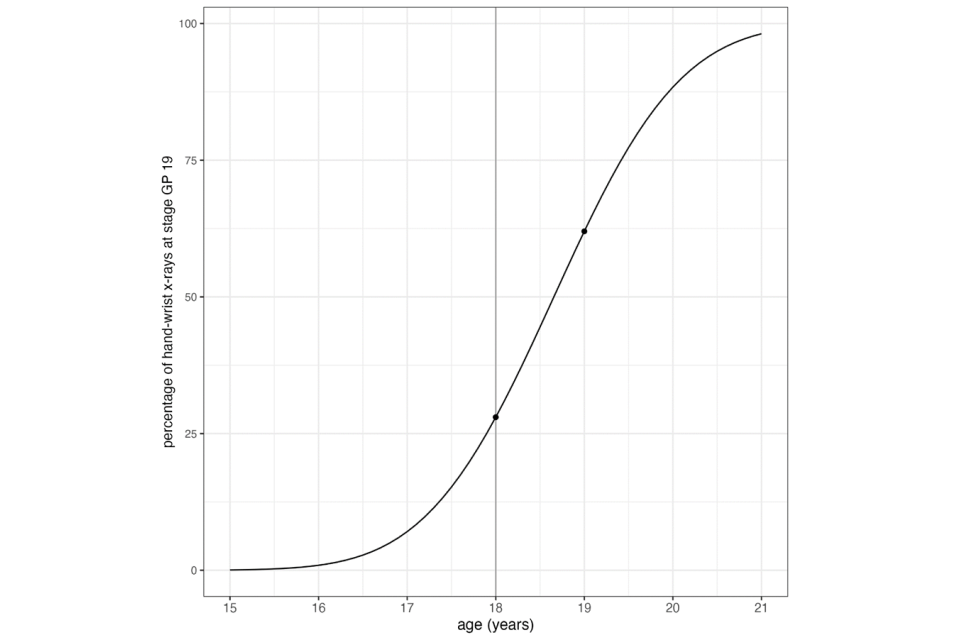
Graph described above
Assessment of the knee
4.48. Assessment of age using MR imaging of the knee has a more recent supporting bibliography than the use of radiography of the hand/wrist, and there is a growing body of international research to support its use. The assessment of age using the knee relies on changes to the appearance of the bones – changes to shape and fusion between the epiphysis and the diaphysis at both the distal end of the femur and the proximal end of the tibia. When this fusion starts to occur, an epiphyseal fusion line is visible by MRI (see Figure 6) and can persist for some time after fusion is complete.
Figure 6: Magnetic Resonance images of the knee of a male aged 15 years (A) and a male aged 17 -years (B)
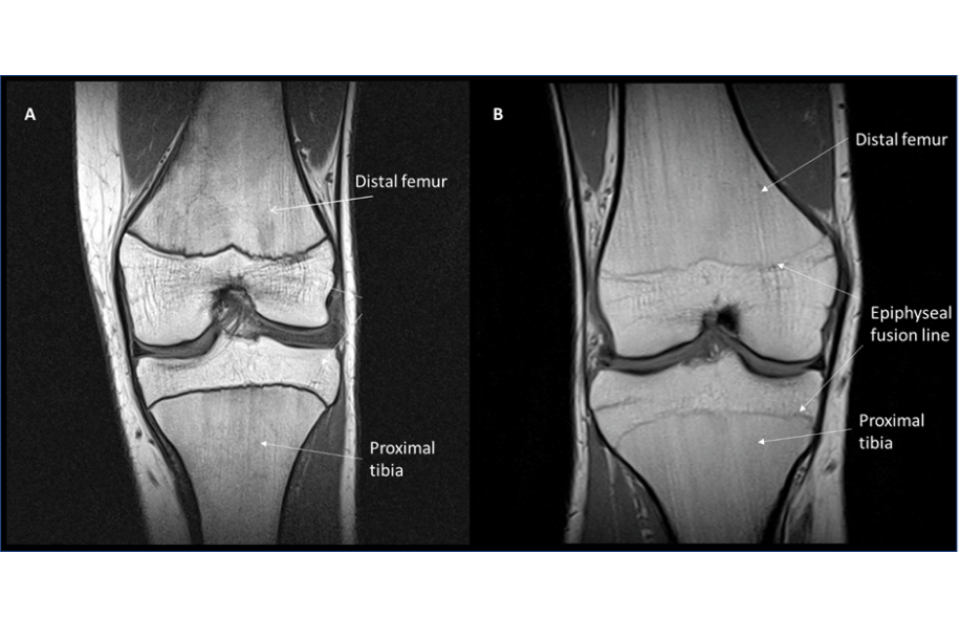
MRI described above
4.49. Although not part of the knee joint, the proximal fibula, which sits to the outer side of the tibia in the lower leg, can also be seen in an MRI of the knee. However, the relationship between maturation of the fibula and chronological age using MR images has not been researched sufficiently to be considered further in this report.
Accuracy and repeatability
4.50. Several studies have assessed the age of transition to the adult stage of the knee based on MRI, most recently reviewed by Heldring et al., (2022). Their probability plots for the distal femur in males and females summarise five studies published since 2014 (Figure 7).
Figure 7: The probability of females (solid line) and males (dotted line) reaching maturation stage 4 of the distal femur as measured by MRI (Heldring et al., 2022). (Logistic regression coefficients kindly provided by Dr Nina Heldring).
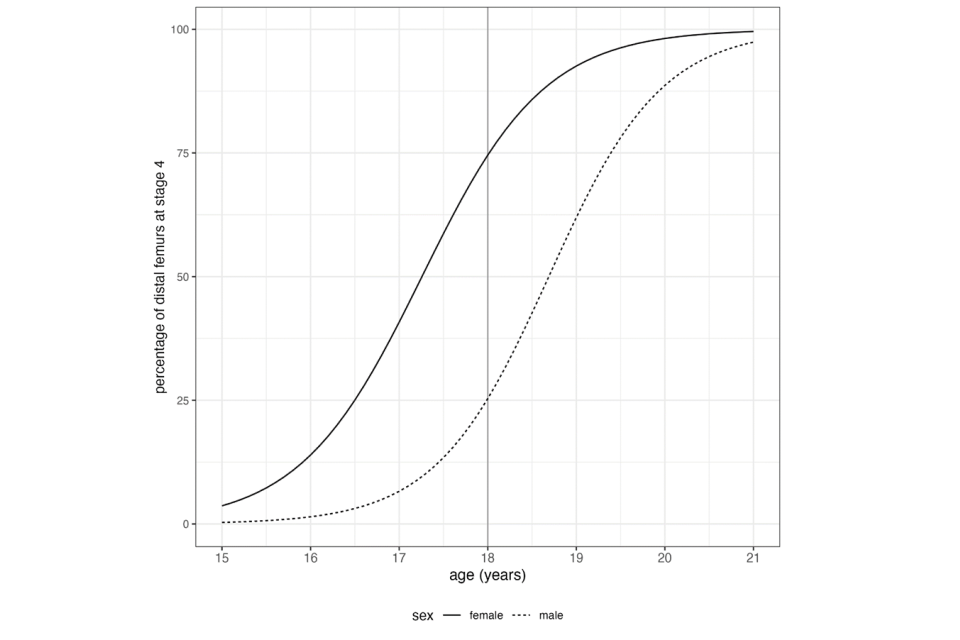
Graph described above
4.51. The median age for reaching stage 4 is 18.7 years in males, very similar to that for the distal radius visualised by radiography (Figure 5). For females the transition to a mature stage occurs earlier at 17.3 years (Heldring et al., 2022).
4.52. It is possible to assess age throughout the adolescent period for both females and males with a standard deviation of between 0.6 to 2.5 years for females and 1.5 to 3 years for males (Auf der Mauer et al., 2019; Dedouit et al., 2012; Kramer et al., 2014; Vieth et al., 2018). The earliest age that maturation of the distal femur is seen is 16 years in females and 18 years in males (Kramer et al., 2014; Saint-Martin et al., 2015).
4.53. Like all the methods proposed, MRI of the knee for age assessment continues to be tested and the interim committee would support ongoing testing so that the level of confidence given to age assessment using the Greulich and Pyle atlas for the hand/wrist radiograph might be achieved for MRI of the knee.
Assessment of the clavicle
4.54. Once an individual has completed puberty, most of the bones stop growing and so reach maturity, meaning that they cannot subsequently be used for age assessment. While puberty and age are closely correlated, it is important to recognise that puberty occurs across a wide range of ages and there are individuals who can experience either early or delayed puberty which will affect the appearance of their bones in relation to their expected age. The maturation of the clavicle continues after puberty and can therefore assist with assessing age particularly when other bones have reached maturity, especially around the important ages of 16 to 17 years.
4.55. The clavicle (collar bone) displays the longest period of growth-related activity in the human body. The medial end of the clavicle (at the base of the neck towards the midline) tends not to complete maturation until the early to mid-20s. This means that age assessment using the clavicle is of value for those who may claim to be minors but whose chronological age is over 18 years.
4.56. Age assessment using the clavicle focuses on the appearance and fusion of a thin flake of bone – the epiphysis, at the medial end of the shaft – to the remainder of the bone. The epiphysis appears and then fuses with the shaft of the bone throughout the late teenage period and into the early 20s (figure 8). The earliest that full maturity has been observed is at age 21 years for both females and males but for most individuals, fusion remains incomplete until age 25 (Ekizoglu et al., 2021; Hillewig et al., 2013; Schmidt et al., 2007, 2016, 2017; Vieth et al., 2014).
Figure 8: Two Magnetic Resonance images showing unfused epiphyses of the clavicle in a female aged 14.9 years (A) and fully fused medial ends of the clavicle in a male aged 36.3 years (B). (Images courtesy of Schmidt et al., 2007.)
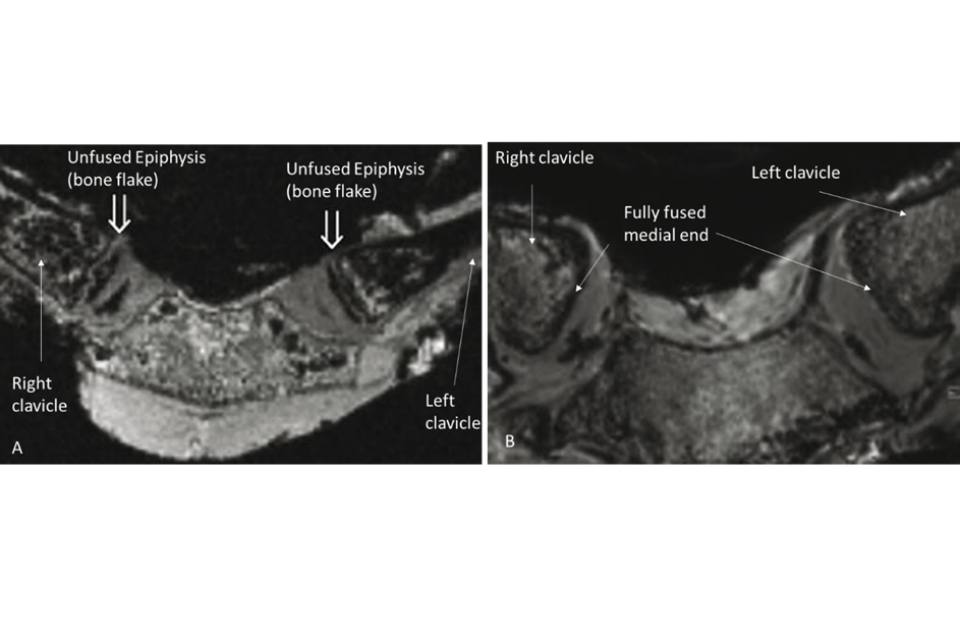
MRI described above
4.57. Due to its anatomical location, the medial end of the clavicle is difficult to visualise by standard radiography and the committee has excluded the use of CT due to higher levels of radiation exposure. There is a growing body of research that supports MR imaging of the clavicle (Ekizoglu et al., 2021; Hillewig et al., 2011; Hillewig et al., 2013; Schmidt et al., 2007, 2016, 2017; Vieth et al., 2014; De Tobel, 2020). Imaging of the clavicle using MRI requires the person to lie face down inside the MRI tunnel to lessen issues with movement from breathing and it is recognised that this could be challenging for some individuals.
Accuracy and repeatability
4.58. Age assessment from the medial clavicle is based on assigning a stage of development to assess maturational status. Schmidt et al., (2017) tabulate summary statistics of age by stage of the medial clavicular epiphysis up to Schmeling stage IV, in 669 males and females, aged 12 to 25 years, though there were only 15 males and 16 females represented in stage IV. In addition, they were unable to stage 99 (15%) of the subjects, which supports the observation of De Tobel et al., (2020) who, while testing only 18 participants, found movement during imaging to impede visualisation of the site.
4.59. Figure 9 is constructed using data taken from the summary statistics in Table 4 of Schmidt et al., (2017) and shows a median age of transition to the mature state of around 23.5 years in both sexes, substantially later than that seen for either the distal radius or distal femur.
4.60. Assessment of age from the medial end of the clavicle is useful in females between the ages of 15 and 25 years and in males between 17 and 25 years with a standard deviation of 1.3 to 3 years for females and 2 to 3 years for males (Ekizoglu et al., 2021; Hillewig et al., 2013; Schmidt et al., 2007, 2016, 2017; Vieth et al., 2014).
Figure 9: The probability by age of females and males reaching maturation stage IV of the medial clavicle as measured by MRI (calculated by logistic regression from Schmidt et al., 2017).
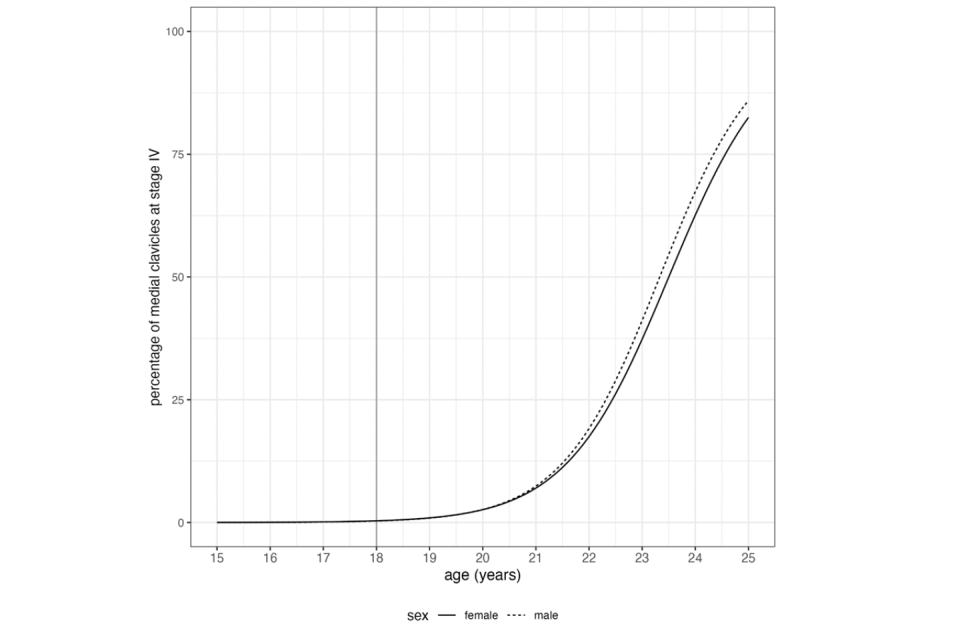
Graph described above
5. Data sets
5.1. All age assessments are undertaken by comparing the maturational stage that an individual has achieved with a reference dataset of images that comprises individuals of known chronological age. This allows an age range to be given within which those maturational changes would be expected to be observed. The individuals of known age, therefore, form the reference of information that informs the evaluation of the maturational changes observed.
5.2. While all maturational changes happen in essentially the same order in each individual, it is the timings and age range over which these changes occur that are of value in age assessment.
5.3. The difference in timing of skeletal maturation between males and females has been well documented, but other factors can also exert an impact on timing. Research initially suggested that there were differences in timings in skeletal development between different ethnic groups, however more recent research has shown that while these group differences do exist, there is no discernible pattern, as would be expected if the differences were due to ethnicity alone, suggesting that socioeconomic factors – including nutrition, disease and social status – may have more influence on maturational timings than ethnic origin (Schmeling et al., 2000). These socioeconomic factors can have a negative or positive impact on growth and maturation, and due to areas of deprivation and advantage within any population, can impact individuals within the same ethnic group in different ways (Bogin, 1988; Eveleth and Tanner, 1990; Garn, 1980). Further research into the impact of these factors and their effect on growth and maturational timing would be beneficial.
Recommendation 7: Further research into the impact of socioeconomic factors and their effect on growth and maturational timing, particularly those factors likely to be experienced by UASC, should be supported.
5.4. While every effort should be made to use a reference dataset that is representative of the group from which the individual being age assessed originates, it is not possible to match the background of every individual, simply because there are so many independent and co-dependent variables that can both positively and negatively impact growth throughout life (Bogin, 1988; Eveleth and Tanner, 1990). Any reference dataset would also have to reflect changes within any given society since socioeconomic changes can both negatively and positively impact throughout the growth period (Eveleth and Tanner, 1990).
5.5. Since it is not possible for reference datasets to be this flexible, it is one of the reasons why any age assessment is given as an age range, allowing for differences influenced by ethnicity and socioeconomic impact to be considered. It is also why the more appropriate question to be asked in relation to UASC is ‘is the claimed age possible?’ rather than the more definitive ‘how old is the individual?’.
5.6. The second consideration when using a reference dataset is how it was formed. The accepted gold standard for age estimation is one created from a longitudinal study of males and females as they progress from birth to adulthood. In the past these have been undertaken using radiography; however, for ethical reasons related to the repeated exposure of children to ionising radiation, these would not be permitted today. It is still possible to undertake longitudinal studies using imaging modalities which do not use ionising radiation, such as MR imaging, however they are expensive and would take a long time to complete (approximately 25 years) and so, understandably, are rare.
5.7. A number of longitudinal studies were undertaken in the first half of the 20th century and the two that have been most studied are the Greulich-Pyle atlas (Greulich and Pyle, 1959) and the Tanner-Whitehouse II atlas (Tanner et al., 1975). Of these the most widely studied and the one that has demonstrated the greatest consistency in accuracy and repeatability for age assessment is the Greulich and Pyle atlas (Chiang et al., 2005; Hackman and Black, 2013; Koc et al., 2001; Van Rijn et al., 2001; Varkkola et al., 2011; Zafar et al., 2010).
5.8. As a result of ethical considerations but also time and financial constraints, most modern imaging databases are cross-sectional in nature. Any reference dataset used should be developed from as large a number of individuals as possible to ensure that the information it provides is statistically robust and can be applied with confidence to the age assessment being undertaken. It should also include a wide range of known age individuals to identify the youngest age at which maturation first occurs. Cross-sectional databases are a snapshot in time of a number of individuals rather than several snapshots in time of a single individual. Therefore, inference drawn from the two different approaches should take this into consideration. Whilst Tanner advocated that his atlas should not be used for age estimation as it was not the original purpose for which the dataset was derived, there has been a significant volume of research undertaken since that time to show the validity of using the approach for the purposes of age estimation.
Combining assessments across body regions
5.9. The mean age of transition from a stage of immaturity to maturity varies by the body region under consideration. Maturity occurs earlier in the wrist and knee than it does for the third molars or the medial clavicle. There is proven value in combining information from two or more sites, to exploit these differences in age of transition.
5.10. Heldring et al., (2022) illustrated this by combining results from radiography of the third molars with MRI appearance of the distal femur. Their meta-analysis combined results from seven third molar studies and five distal femur studies. They presented probability plots similar to those seen in Figures 3, 5, 7, and 9, combining data from dentition and the knee by multiplying the two probabilities at each age — this gave a joint probability of maturity on the assumption that the two sources of evidence were conditionally independent.
5.11. Figure 10 compares the probability plots in males for third molar maturity and knee maturity separately, and then for combined molar and knee maturity. The figure shows that by age 18, 25% of males are already mature for the distal femur (green) and 11% for third molars (blue), and so they could be misclassified as adults. However, only 3% (that is, 25% of 11%) of males are mature for both distal femur and third molar (red) at age 18. This supports the accepted practice that combining markers can reduce misclassification error. Note that multiplying probabilities together in this way requires the two markers to be conditionally independent, which is generally the case for wrist and third molar maturation.
Figure 10: The probability of males reaching maturation stage 4 of the distal femur and/or stage H of the third molar (calculated from Heldring et al., 2022 with permission).
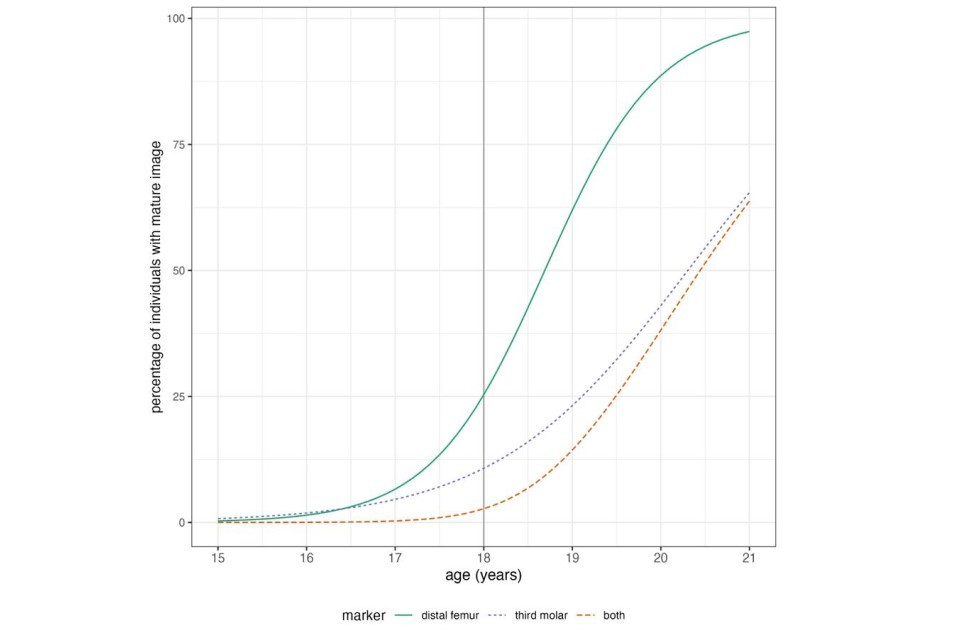
Graph described above
6. Implementation of methods proposed
6.1. The committee presents two options by which the current Merton-compliant assessments could be supported by biological age assessment. Either biological age assessment could be carried out in secondary support of the Merton-compliant assessment, if needed, or both assessment methods could be initiated at the beginning of the assessment process.
6.2. Where biological age assessment is used in secondary support of the existing Merton-compliant process, a local authority would complete the Merton-compliant interview process and, if doubts remained about the claimed age at the ‘minded to’ stage of the proceedings, biological evaluation could be introduced. In this situation, the outcome of the biological approach might support the Merton assessment, or it might not.
6.3. This process retains a heavy reliance on the untested Merton-compliant process if biological assessment is not routinely utilised. However, the option of biological assessment offers supporting evidence which may be considered together with the outcome from the Merton assessment to assist with a decision on whether the claimed age is possible. The claimant may still reject the findings and legally challenge the age assigned. Figure 11 summarises this approach.
6.4. The advantage of this approach is that it allows the Merton-compliant assessment to act as a filter such that biological age assessment is only performed in cases where the claimed age remains in doubt or there is conflicting or insufficient evidence to allow the social worker to assess the young person’s age with confidence. To avoid further delay in completion of the age assessment process the delivery timeframes for the results of biological age assessment could be defined to ensure that results were provided swiftly between the ‘minded to’ interview and the final decision to assign an age. The time between the young person arriving in the UK and their biological assessment should be kept to a minimum because maturational changes will continue to occur in the time between arrival and assessment.
Figure 11: Summary of approach applying Merton first and then biological evaluation if needed.
Applicant gives age (claimed age)
Immigration officers refer to a local authority (LA)
LA has signifcant doubts over claimed age
Merton-compliant process ‘minded to’ interview held
If minded to support claimed age > No biological evalutation needed (End)
If claimed age not supported/ insufficient evidence > Biological evaluation requested > Assessment of Merton and biological findings > Final age assignment (End)
6.5. An alternative approach could be to carry out biological and the existing Merton-compliant process in tandem, both started at the beginning of the age assessment process (see Figure 12). Assignment of age would therefore always take biological assessment into account. The claimant may still reject the findings and legally challenge the age assigned.
6.6. The tandem approach would allow for both methods to be used to provide more evidence and might provide more rapid and reliable results.
6.7. It is important that if both processes are to be used, then the assessments are undertaken independently to minimise the possibility of bias.
Figure 12: Summary of approach where either Merton or biological evaluation can be carried out first.
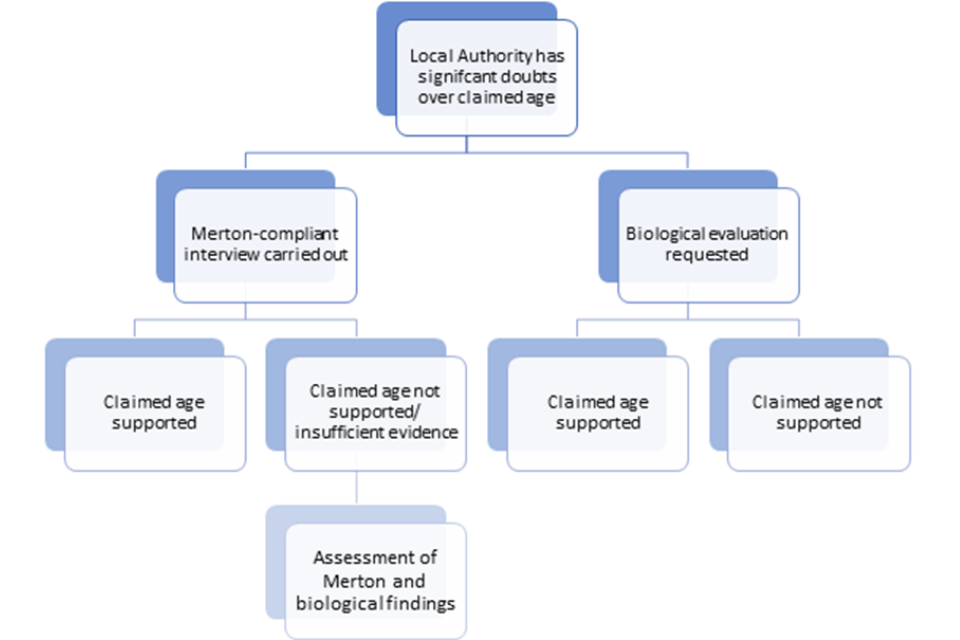
Flowchart of the process described above
Assessment environment
6.8. If biological age assessments are to proceed, consideration should be given to the environment within which any imaging or assessment would take place.
6.9. In line with the Department of Health quality criteria for young people friendly health services (2011) young people need to be seen and assessed in an environment that is appropriate to their age and development. Ideally, young people who claim to be under the age of 18 should be provided with a waiting area separate from adults and staffed by professionals who are skilled in communicating with young people. The area should be welcoming and designed to put young people at ease. Young people should be allowed to wear their own clothes wherever possible rather than be expected to change into ‘hospital’ wear. A young person should be able to bring a friend or supporter with them to their appointment as this will help to put them at ease and not feel alone.
6.10. To minimise the time in an assessment environment, facilities should be set up in such a way that all the necessary images can be captured at one appointment.
Image capture and analysis
6.11. Dental and bone images should be acquired by those with the relevant expertise, such as radiographers, interpreted and reported by those with the relevant expertise and training, such as clinical radiologists and reporting radiographers, paediatricians, odontologists and anthropologists.
6.12. If private sector suppliers are to be used for radiography and MRI, they should demonstrate expertise in acquiring images for age estimation.
Recommendation 8: Dental and bone images should be acquired by those with the relevant training and expertise, and interpreted by those with expertise in interpreting images for age estimation.
6.13. It would be beneficial to explore the development of a UK-based proficiency test in age estimation. The only proficiency test the committee is aware of is provided by the Study Group on Forensic Age Diagnostics of the German Association of Forensic Medicine.
6.14. Advice should be sought on the best practice for safely storing and sharing image and analysis data.
7. Interpretation of biological age assessment results
Misclassifications
7.1. There are two scenarios that could arise in the early stages of decision making prior to a Merton or biological assessment that should be acknowledged with regard to safeguarding. An individual may appear to Immigration Officers to be older than their claimed age and may be incorrectly judged to be adult when they are in fact a minor and so will not be age assessed unless they are able to make a representation to a local authority. Such individuals are false positives, minors rated as adults who, if not recognised by an Immigrations Officer, may be incorrectly placed in detention with adults. If the minor is wrongly assessed to be an adult their application for asylum may be deemed inadmissible on safe third country grounds, a decision that cannot apply to children.
7.2. There is also the opposite risk of misclassification where an individual is an adult but they look or behave younger than their years. These individuals would be unlikely to be recognised as an adult and so would not be age assessed. These are false negatives, adults rated as minors, and this group also raises significant safeguarding issues.
7.3. Neither of these categories might be recognised by Immigration Officers or the local authority and this needs further discussion, beyond the scope of the interim committee, on how to minimise such inaccuracies. To be clear, the committee is not advocating age assessment for all cases but raising awareness of the potential for false negatives and false positives which could raise major safeguarding issues either for the claimant or for those with whom the claimant is housed.
Triaging
7.4. The four biological regions proposed; third molar, hand/wrist, knee, and clavicle are suitable for assessing the age range of interest – around 16 to 18 years – but it is not necessary, or indeed desirable, to employ all approaches for every person being assessed. Rather, triaging is advocated to ensure that the most appropriate imaging methods and body regions are selected and that unnecessary imaging is avoided.
7.5. For example, the age assessment of a female claiming to be aged 17 but believed to be older would be unlikely to benefit from radiography of the hand/wrist, or MRI of the knee, since maturity is usually reached in these areas by that age in females. Evaluation of the third molars and clavicle would be of more value in this case and therefore these would both be advocated, and they have the added advantage of not being directly co-dependent.
7.6. The selection of appropriate regions for assessing biological age will depend on the sex, claimed age and whether there is an indication that the person may be older or younger than they claim. Selection of appropriate methods should be carried out on a case-by-case basis. In addition, since assessment of the hand/wrist and the knee provides information covering a similar range of ages, either radiography of the hand/wrist or MRI of the knee could be performed depending on availability of equipment or choice expressed by the person being assessed. The committee advocates using an MRI of the knee, but if not possible, then a single radiograph of the hand/wrist carries only a very small risk of harm.
7.7. There may be situations where a particular method is unsuitable because it would not provide useful information for assessing age. For example, there are certain skeletal dysplasias where the appearance of the bones would make the images difficult to interpret.
7.8. In addition, around 10% of individuals do not develop third molars (agenesis); however, agenesis will not be apparent until after the image has been taken. In these cases, biological estimation of age would rely on skeletal assessment alone and the weight of evidence should be adjusted appropriately.
7.9. Unexpected significant differences can occur between the ages generated by a biological evaluation, the Merton assigned age and the claimed age. Such cases should be investigated to establish if there are any underlying medical conditions that could have affected development, such as precocious puberty or under production of sex steroids.
7.10. Precocious puberty, where a child starts puberty early because of excessive production of the sex steroids (oestrogen or testosterone), can result in early skeletal maturation. Conversely, if a young person is unable to produce any, or low volumes of, pubertal hormones because of a clinical condition, then puberty will be delayed and their skeletal age will appear to be younger than their actual age (Dattani and Brook eds., 2020).
7.11. The interim committee recommends development of a guide on how to deal with those situations where there is a discrepancy between the claimed/suspected age and the biological evaluation outputs that considers United Nations High Commissioner for Refugees’ guidelines on international protection (UNHCR, 2009, para. 75) and makes clear what weight should be placed on different sources of information when making a decision on age.
Recommendation 9: A guide should be developed on how to deal with those situations where there is a discrepancy between the claimed/suspected age and the biological or social worker-led evaluation outputs which makes clear what weight should be placed on different sources of information.
Exploring the use of the likelihood ratio to minimise misclassification
7.12. Under the existing process, where a local authority has doubt about the age claimed by an unaccompanied asylum-seeking child, a Merton-compliant assessment is carried out and if this assessment does not support the claimed age a new date of birth is assigned – the Merton assigned age.
7.13. The committee proposes using a combination of biological age assessment methods to also assess whether the age claimed by a UASC is possible.
7.14. Unlike claimed age and Merton assigned age, biological age in this context is not a specific age in years – it is an assessment of radiographs or MRIs that reflect physical maturity based on the appearance of one or more body regions. In the simplest case, for a single area assessed, biological age status is either immature or mature, and the chance of being mature depends on the individual’s chronological age (which at this point is unknown).
7.15. The plots in Figures 3, 5, 7 and 9 show how the chance of being mature varies by age for the four regions: third molars, hand/wrist, knee, and clavicle, respectively. For these plots, maturity is defined using the following stages; Demirjian stage H (third molar), Greulich-Pyle GP 19/GP 18 (hand/wrist, male and female respectively), Krämer stage 4 (knee, Krämer et al., 2014) and Schmeling stage IV (clavicle, Schmeling et al., 2004; Schmidt et al., 2017). Other final stages could be used to indicate the point at which maturity is reached.
7.16. The plots in figures 3, 5, 7 and 9 are read as follows: choose a particular age, then read off from the plot the chance (i.e. the probability) of an individual of that age being mature.
7.17. The plots can be used to compare the probabilities for two different ages, e.g. the UASC’s claimed age and assigned age. This is best done by calculating the ratio between them, i.e. the probability for the Merton assigned age divided by the probability for the claimed age. This ratio is known as the likelihood ratio, and it is widely recognised as the appropriate way to summarise evidence in favour of two alternative hypotheses (Royal Society, 2020)— in this case the hypothesis that the assigned age is correct versus the hypothesis that the claimed age is correct.
7.18. Taken on their own, these plots provide only limited information, but they are more informative when the results are considered in combination. Heldring et al. (2022) has already shown how combining information on the distal femur and third molar can reduce misclassification error to around 3% (see figure 10).
7.19. Plots can also be created that combine the four regions proposed in this report, which can be assessed in three groups: hand/wrist or knee (henceforth called ‘limb’), tooth (third molar) and clavicle. Maturation of the bones of the hand/wrist and knee occurs at similar ages and the maturation is intrinsically linked to puberty; therefore these areas are grouped together and are not considered to be conditionally independent of each other. However, maturation of the clavicle occurs later in time and after puberty. Despite being part of skeletal development this difference allows the maturation timing of the limb (hand/wrist/knee) and the clavicle to be considered conditionally independent. In addition, the development of the teeth is distinct from the development of the skeleton (Garn et al., 1965, Lewis, 1991) allowing the maturation of the third molars to be considered conditionally independent.
7.20. The three results for limb (either hand/wrist or knee), tooth and clavicle can be either immature or mature, so this provides 2 x 2 x 2 (or eight) possible alternative outcomes from the assessment. All three markers may be immature, or just one of them mature and the other two immature, or two mature/one immature, or all three mature. In addition, each marker may optionally be omitted from the assessment. This provides a third alternative, making three possible outcomes: not done, immature and mature. With three possible areas assessed (limb, tooth, clavicle) and three possible outcomes (not done, mature, immature) this provides a total of 27 possible alternatives (3 x 3 x 3).
7.21. Multiplying together the probabilities for each of these alternative outcomes at each age gives a product of probabilities, or a likelihood. So the plot is more appropriately called a likelihood plot, with the y-axis labelled as relative support. Where a marker is immature the corresponding probability is 100% minus the probability of being mature.
7.22. When no biological age assessments are performed there is equal support for all ages, since the lack of information means that all ages are equally likely. In this case the likelihood plot is a flat line.
7.23. Figures 13 and 14 show the likelihood plots by sex for each of these 27 possible combinations. They are complicated at first glance, but they represent all the information to be gained from a biological age assessment in the two sexes.
7.24. Each panel is a likelihood plot for one particular outcome of the three biological assessments. The panel labels indicate for limb, tooth and clavicle respectively that an assessment is either not done (1), the marker assessed is immature (2), or it is mature (3), the three levels together defining the panel number (for example, 132 means - limb not done, tooth mature, clavicle immature). Limb, tooth and clavicle are ranked in this order to reflect their median ages of transition.
7.25. It should be noted that there is uncertainty about the data used to build the plots as they are based on a small number of studies. However, with further work, this uncertainty could be quantified and represented as a confidence interval for the likelihood ratio. Its effect would be to shrink the likelihood ratio towards one.
7.26. Each plot indicates the ‘relative support’ for different ages given the particular set of assessment outcomes. The upper set of panels (clavicle not done) corresponds to just limb and tooth, where panel 111 (no biological assessments done) contains no information, so each age is equally supported and the curve is flat. The other three corners of the upper set of panels (in figures 13 and 14) correspond to Figure 10: mature limb (311), mature tooth (131) and mature limb and tooth (331), where there is greater support for ages over 18.
7.27. Conversely when neither limb nor tooth is mature, ages under 18 are supported more strongly.
7.28. The false negative rate is high when relying on tooth alone, since immature teeth are relatively common over age 18 (the white region under the curve in panel 121). However, they are less common (the white region is smaller) in combination with immature limb indicators (panel 221), particularly in females. This is another benefit of working with tooth and bone in combination.
7.29. Looking at all the panels (except panel 111 where no assessments have been done) there are four types of curve shape: falling (for example, panel 122), peaked (for example, panel 332), rising (for example, panel 133) and flat/nearly flat (for example, panel 233). Their meanings are as follows:
-
‘falling’: the area or areas assessed are all immature, indicating that the individual is more likely to be a minor
-
‘peaked’: a combination of mature bone and/or tooth with an immature clavicle, with a peak in the age range 19 to 22 years
-
‘rising’: the area or areas assessed are all mature, indicating that the individual is more likely to be an adult
-
‘flat or nearly flat’: a combination of outcomes unlikely to be seen at any age – such as mature clavicle in the presence of immature limb and/or tooth
7.30. Ignoring the ‘flat’ category, the relative support at age 18 for each curve indicates the value of that combination of areas for age assessment. There are three alternatives:
-
strong relative support: the individual is more likely to be a minor (under age 18)
-
weak relative support: the individual is more likely to be an adult (aged 18 and over)
-
moderate relative support: no clear conclusion
7.31. Taken together, the panels provide evidence on the individual’s likely age, though the value of the evidence depends on the pattern seen:
-
if the areas assessed are all immature – that is, the curves are all falling and the panel numbers do not contain 3 – the individual is more likely to be under 18
-
equally, if the areas assessed are all mature – that is, the curves are all rising and the panel numbers contain 3 – the individual is more likely to be over 18
-
but if some areas assessed are immature and some mature, this is consistent with a range of ages around 18 years, and misclassification is possible in either direction
-
immature teeth without limb assessment (panels 121 or 122) are consistent with any age up to 23 years.
Figure 13: Likelihood plots in males for all 27 combinations of limb, tooth and clavicle assessment outcomes. The three areas of limb (either hand/wrist or knee), tooth and clavicle can each be either immature or mature, so this provides 2 x 2 x 2 (or eight) possible alternative outcomes from the assessment. All three markers may be immature, or just one of them mature and the other two immature, or two mature/one immature, or all three mature. Each of these eight alternatives has its own associated likelihood plot which is given a number based on whether each of the three areas were; not done (1), immature (2), or mature (3). Non-zero probability below age 18 is shown shaded. The curves are either falling, peaking, rising or flat – see the text for details.
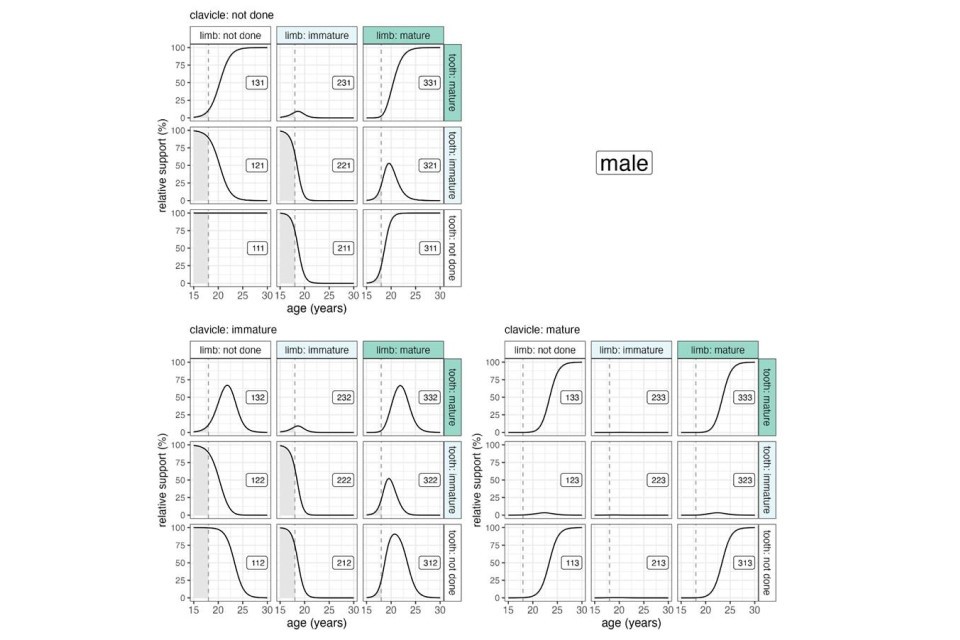
Graphs described above
Figure 14: Likelihood plots in females for all 27 combinations of limb, tooth and clavicle assessment outcomes. The three areas of limb (either hand/wrist or knee), tooth and clavicle can each be either immature or mature, so this provides 2 x 2 x 2 (or eight) possible alternative outcomes from the assessment. All three markers may be immature, or just one of them mature and the other two immature, or two mature/one immature, or all three mature. Each of these eight alternatives has its own associated likelihood plot which is given a number based on whether each of the three areas were; not done (1), immature (2), or mature (3). Non-zero probability below age 18 is shown shaded. The curves are either falling, peaking, rising or flat – see the text for details.
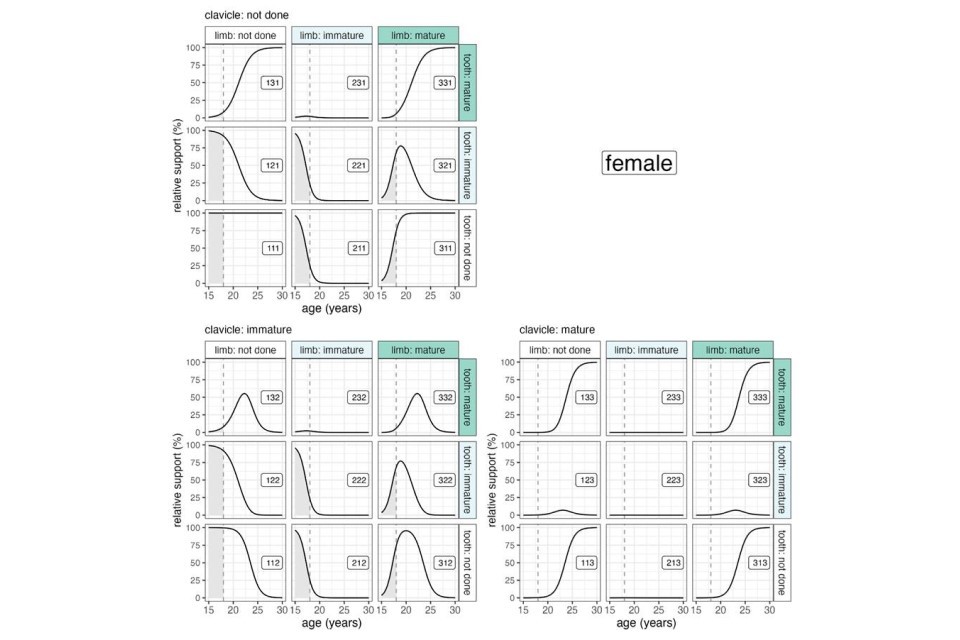
Graphs described above
7.32. One important conclusion from figures 13 and 14 is that assessments of limb (be it hand/wrist or knee) or tooth should be performed in combination. As explained above, this materially reduces the false positive misclassification rate.
7.33. The young person’s Merton assigned age can be compared with their claimed age using the likelihood plots in figures 13 and 14. The likelihoods relating to the two ages are read off the panel curve corresponding to the biological assessment results and the likelihood ratio calculated. The likelihood ratio summarises the support or ‘weight of evidence’ in favour of the Merton assigned age versus the claimed age. If the likelihood ratio is greater than one, this shows that the biological age assessment supports the Merton assigned age more than it does the claimed age. Conversely, if it is less than one then the claimed age carries stronger support. The likelihood ratio expresses the ‘balance of probabilities’ as a single number.
Recommendation 10: Consider adopting a likelihood ratio approach, using biological evidence of age to compare the weight of evidence or ‘support’ for the Merton assigned age versus the claimed age.
7.34. The outcome of the biological assessment must not be shared with the social worker until their initial assessment is complete as this separation is necessary for statistical independence to allow calculation of the likelihood ratios.
7.35. The size of the likelihood ratio is key. If it is greater than 100 or less than 1/100 (that is, 0.01) then it shows strong support for one age over the other. Conversely, if it is less than 10 or greater than 1/10 (that is 0.1) then this suggests limited or weak support for either age. Intermediate values for the likelihood ratio indicate moderate support for one age over the other (Royal Society, 2020). See the worked examples for illustrations of the use of likelihood ratio.
7.36. Figures 13 and 14 show the levels of relative support for different assessment outcomes at different ages, and allow the calculation of likelihood ratios to compare the support for alternative UASC ages. It is important to note that taking just one level of support in isolation and viewing it as a probability is not a valid way to measure the evidential value of that assessment at that age—it needs to be expressed relative to the support for an alternative age, in the form of the likelihood ratio.
7.37. There is potential to use an individual’s claimed age and their biological age assessment results to calculate the likelihood ratios for a range of possible assigned ages. This could be done with or without knowledge of the Merton assigned age. The results would indicate whether or not there was an assigned age with sufficient relative support to prefer it over the claimed age. This idea needs further consideration by the full Age Estimation Science Advisory Committee.
8. Worked examples
8.1. Data from Kent County Council demonstrate that the overwhelming majority of minors seeking asylum are male (90 - 95%) and of these, the majority have a claimed age of 16 or 17 years. This group makes up about 70% of the cohort, with under 16s (both sexes) making up 25% of the cohort; the final 5% are females claiming to be 16 and 17 years of age. These numbers vary from month to month but are a good approximation of the cohort at any one time.
8.2. Whilst it is unlikely for individuals who arrive by small boats and lorries from France to claim an adult age when in fact they are a minor, these circumstances can occur when children are being actively trafficked and exploited for onward movement into the UK. In such cases an ability to determine quickly that someone is very likely to be a child beyond their physical appearance will provide an important safeguarding tool, particularly as adults may be relocated overseas for processing their asylum claim.
8.3. The largest number of age challenges occurs in males claiming to be aged 16 to 17 years when they are believed by Immigration Officers to be adults aged between 18 and 21 years. A recent Supreme Court ruling (R (BF (Eritrea)) v Secretary of State for the Home Department, 2021) held that the Home Office’s policy of treating individuals as adults where their physical appearance and demeanour very strongly suggest that they are significantly over 18 years to be lawful, but it remains the case that some individuals over 18 continue to find their way into children’s social care services. An ability to determine whether this cohort represents adults or minors will provide the greatest levels of safeguarding.
8.4. Individuals presenting to a local authority as a child may be given the benefit of the doubt and a full age assessment may not be performed in all cases. This follows case law that states that “if the decision maker is left in doubt, the claimant should receive the benefit of that doubt” (R v London Borough of Croydon and WK v Kent County Council [2009] EWHC 939). This approach fits with the current biological evidence that the committee has been reviewing.
8.5. For those claiming to be under 16, where there is doubt about that age and there are concerns about the consequences of placing older individuals into foster care, schools and health settings designed for younger children, an age assessment would be undertaken. The committee considers that additional biological evidence to support this assessment would be of significant additive value.
8.6. Worked examples are provided for both a male and a female, demonstrating potential scenarios where biological evaluation may, or may not, support the claimed age.
8.7. Note that the stages used in the worked examples could be replaced by other systems that use appropriate sample sizes. The following are provided merely as examples of how the process could operate.
Worked example for male of claimed age 17 years
Case details
8.8. An Iranian male UASC arrived in the UK claiming to be aged 17 years. He was unable to present any documentation to confirm his date of birth. His age was challenged at the border because he was believed to be older than his claimed age but as he did not look significantly over the age of 18 years (as per the Supreme Court ruling above) he was issued with the relevant age challenge documentation and referred to the local authority to be treated as a child, pending possible further age assessment. Having spent a couple of weeks in the care of the local authority it was agreed that there was significant doubt that he was under the age of 18 years, and a Merton-compliant age assessment was carried out. The individual’s age was assessed to be 21 years and not 17 years. This Merton assigned age was subsequently challenged by the young male and in support of this age assessment, in this worked example a biological evaluation could be requested by the local authority following the sequential approach set out in section 6.
8.9. The young male was 17 years and 7 months old at the time of assessment if the claimed date of birth was correct. He consented to biological evaluation and the following biological age assessment methods would be most appropriate for assessment of someone of that age:
-
assessment of third molars
-
assessment of hand/wrist or knee
-
assessment of clavicle
Possible output where biological evaluation supported the claimed age
Third molars
| Tooth | Description | Stage(Demirjian et al., 1973) |
|---|---|---|
| Left mandibular molar | Root growing – immature | G |
| Right mandibular molar | Root growing – immature | G |
8.10. The appearance of the radiograph of the dentition corresponds most closely with Demirjian stage G. There are no appropriate published data from Iran; however, stage G corresponds to an age range of 15 to 20 years for males from Chile (Pinares Toledo et al., 2021); 14 to 22 years for Hispanic males from Texas (Kasper et al., 2009); 15 to 22 years for Korean males (Lee et al., 2009); of 15 to 25 years for both males and females from Malaysia (Johan et al., 2012); and 16 to 23 years for both males and females from Thailand (Duangto et al., 2017).
8.11. Given the range of possible ages from these data sets, this stage of dental development suggests that the claimed age is possible.
Hand/wrist
| Bone | Times of fusion/appearance | Radiograph |
|---|---|---|
| Epiphyseal fusion of distal end of metacarpals 2 to 5 | 16.5 years | Fused |
| Epiphyseal fusion of proximal end of metacarpal 1 | 16.5 years | Fused – epiphyseal scar still in evidence |
| Epiphyseal fusion of proximal phalanges | 16.5 years | Fused |
| Epiphyseal fusion of middle phalanges | 16.5 years | Fused |
| Epiphyseal fusion of distal phalanges | 16 years | Fused |
| Appearance of last carpal (pisiform) | 12 years (other carpals appear 3/4 months to 12 years) | Has appeared and shows adult morphology |
| Appearance of sesamoid bone (s) | 13 to 18 years | Has appeared and shows adult morphology |
| Epiphyseal fusion at distal ulna | 17 to 20 years | Fused – with remodelling across fusion line complete |
| Epiphyseal fusion at distal radius | 17 to 20 years | Partially fused |
8.12. The appearance of the radiograph of the hand/wrist corresponds most closely with standard 29 in the Greulich-Pyle atlas which corresponds to an age range of 15 years 9 months to 18 years 1 month.
8.13. This stage of limb development suggests that the claimed age is possible.
Clavicle
| Bone | Description | Stage (Schmidt et al., 2017) |
|---|---|---|
| Left medial clavicle | Small epiphyseal flake in evidence covering approximately ⅓ of the diaphyseal surface of the medial clavicle | IIb |
| Right medial clavicle | Small epiphyseal flake in evidence covering approximately ⅓ of the diaphyseal surface of the medial clavicle | IIb |
8.14. The appearance of the epiphyseal flake at the medial face of each of the left and right clavicles correlates to stage IIb which in turn corresponds to an age range of 16 years 6 months to 18 years 9 months. Note that there are other staging systems for the clavicle and it is not necessary to use the same staging system as the one in the example.
8.15. This stage of clavicular development suggests that the claimed age is possible.
8.16. These results correspond to all 3 areas assessed being immature. This represents panel 222 in figure 13, where the likelihood ratio of the Merton assigned age (21 years and 7 months) versus the claimed age (17 years 7 months) is 0.0027 or 1/375, strong evidence that the claimed age of 17 years is more likely than the Merton assigned age of 21 years. Therefore, the claimed age would be supported.
Possible output where biological evaluation did not support the claimed age
Third molars
| Tooth | Description | Stage (Demirjian et al., 1973) |
|---|---|---|
| Left mandibular molar | Root apex closed – mature | H |
| Right mandibular molar | Root apex closed – mature | H |
8.17. The appearance of the radiograph of the dentition corresponds most closely with Demirjian stage H which corresponds to a minimum age of 15 years.
8.18. As maturation can occur before the age of 17 years and 7 months, taken on its own, this stage of dental development suggests that the claimed age is possible.
Hand/wrist
| Bone | Times of fusion/appearance | X-ray |
|---|---|---|
| Epiphyseal fusion of distal end of metacarpals 2 to 5 | 16.5 years | Fused |
| Epiphyseal fusion of proximal end of metacarpal 1 | 16.5 years | Fused – epiphyseal scar still in evidence |
| Epiphyseal fusion of proximal phalanges | 16.5 years | Fused |
| Epiphyseal fusion of middle phalanges | 16.5 years | Fused |
| Epiphyseal fusion of distal phalanges | 16 years | Fused |
| Appearance of last carpal (pisiform) | 12 years (other carpals appear 3/4 months to 12 years) | Has appeared and shows adult morphology |
| Appearance of sesamoid bone(s) | 13 to 18 years | Has appeared and shows adult morphology |
| Epiphyseal fusion at distal Ulna | 17 to 20 years | Fused – with remodelling across fusion line complete |
| Epiphyseal fusion at distal Radius | 16 to 20 years | Fused – with remodelling across fusion line complete |
8.19. The appearance of the radiograph of the hand-wrist corresponds most closely to the Greulich-Pyle standard 31, which shows a mature hand/wrist relating to an individual aged 19 years. The minimum age at which this hand/wrist morphology is achieved according to the Greulich-Pyle atlas is 16.5 years. Because the hand wrist radiograph shows full maturity it is not possible to give an upper age, since the bones are fully mature.
8.20. As maturation can occur before the age of 17 years and 7 months, taken on its own, this stage of limb development suggests that the claimed age is possible.
Clavicle
| Bone | Description | Stage (Schmidt et al., 2017) |
|---|---|---|
| Left medial clavicle | Epiphysis has ossified and begun to fuse with the medial surface of the diaphysis with approximately half of the physis (or growth plate) fused | IIIb |
| Right medial clavicle | Epiphysis has ossified and begun to fuse with the medial surface of the diaphysis with approximately half of the physis (or growth plate) fused | IIIb |
8.21. The appearance of the epiphyseal flake at the medial face and stage of fusion of each of the left and right clavicles correlates to stage IIIb, which for males corresponds to an age range of 18 years 6 months to 22 years 1 month). This suggests that the claimed age is not supported.
8.22. From the results of the biological assessment, the claimed age was possible given the assessment of the dentition and the hand/wrist, both of which were mature and only a minimum age can be given for these areas. However, the developmental stage of the clavicle did not support the claimed age and the overall conclusion was that the claimed age of 17 was not supported. The age range for this individual is likely to be between 18 years 6 months to 22 years 1 month.
8.23. In this example the limb (hand/wrist) and tooth are mature while the clavicle is immature, which corresponds to panel 332 in figure 13. Reading off the plot gives a likelihood ratio for the Merton assigned age (21 years 7 months) versus the claimed age (17 years 7 months) of 56. This shows moderate support for the Merton assigned age over the claimed age.
Worked example for female of claimed age 16 years
This example is a rare case and provided only to demonstrate how the triage approach could be applied to a female UASC.
Case details
8.24. A Vietnamese female UASC arrived in the UK claiming to be aged 16 years. The young female was unable to present any documentation to confirm her date of birth. Her age was challenged at the border because she was believed to be older than her claimed age but she did not look significantly over the age of 18 years as per the Supreme Court ruling (above). She was issued with the relevant age challenge documentation and referred to the local authority to be treated as a child pending possible further age assessment. Having spent a couple of weeks in the care of the local authority it was agreed that there was significant doubt that the individual was a child under the age of 18 years and a Merton-compliant age assessment was carried out by the local authority. The individual’s age was assessed to be 20 years by Merton compared to the claimed age of 16 years. The assigned age was subsequently challenged and in this worked example a biological evaluation could be requested.
8.25. At the time of the assessment the young female’s age would be 16 years and 6 months, if the claimed date of birth was correct. She consented to biological evaluation and the following biological age assessment methods would be of value in assessing whether the claimed age could be correct:
-
assessment of third molars
-
hand/wrist or knee
-
assessment of clavicle
Possible output where biological evaluation supported the claimed age
Third molars
| Tooth | Description | Stage (Demirjian et al., 1973) |
|---|---|---|
| Left mandibular molar | Root growing – immature | G |
| Right mandibular molar | Root growing – immature | G |
8.26. The appearance of the radiograph of the dentition corresponds most closely with Demirjian stage G which corresponds to an age range of 14 years to 24 years for Korean females (Lee et al., 2009), 15 to 25 years in Malaysian females (Johan et al., 2012) and 16 to 23 years in Thai females (Duangto et al., 2017).
8.27. This stage of dental development indicates that the claimed age is possible.
Knee
| Bone | Description | Stage (Vieth et al., 2018) |
|---|---|---|
| Distal femur | In the T1-w sequence a discontinuous thin and serrated line of intermediate signal intensity between the epiphysis and the diaphysis is visible. In the continuity of the line, thicker sections with no signal intensity can be seen. In the T2-w sequence a thin single, discontinuous or dotted line of hyperintense signal is visible in the same position as the described thin line of the corresponding T1-w sequence. In the continuity of the line, thicker hyperintense sections can be seen |
Stage 4 |
| Proximal tibia | In the T1-w sequence a discontinuous thin andserrated line of intermediate signal intensity between the epiphysis and the diaphysis is visible. In the continuity of the line, thicker sections with no signal intensity can be seen. In the T2-w sequence a thin single, discontinuous or dotted line of hyperintense signal is visible in the same position as the described thin line of the corresponding T1-w sequence. In the continuity of the line, thicker hyperintense sections can be seen. |
Stage 4 |
8.28. The appearance of the distal femur correlates to stage 4 (Vieth et al, 2018) which corresponds to an age range of 14 years 10 months to 16 years 10 months for females. The appearance of the proximal tibia correlates to stage 4 which corresponds to an age range of 14 years 4 months to 16 years 6 months for females.
8.29. This stage of limb development indicates that the claimed age is possible.
Clavicle
Stage of development:
| Bone | Description | Stage (Schmidt et al., 2017) |
|---|---|---|
| Left medial clavicle | Small epiphyseal flake in evidence covering approximately ⅔ of the diaphyseal surface of the medial clavicle | IIc |
| Right medial clavicle | Small epiphyseal flake in evidence covering approximately ⅔ of the diaphyseal surface of the medial clavicle | IIc |
8.30. The appearance of the epiphyseal flake at the medial face of each of the left and right clavicles correlates to stage IIc for females, which corresponds to an age range of 16 years 6 months to 20 years 1 months. This stage of clavicular development indicates that the claimed age is possible.
8.31. Using figure 14 panel 222 for immature knee, tooth, and clavicle gives a likelihood ratio of 1/136, indicating moderately strong support for the claimed age (16 years) over the Merton assigned age (20 years).
Possible output where biological evaluation did not support the claimed age
Third molars
| Tooth | Description | Stage (Demirjian et al., 1973) |
|---|---|---|
| Left mandibular molar | Root apex closed – mature | H |
| Right mandibular molar | Root apex closed – mature | H |
8.32. The appearance of the radiograph of the dentition corresponds most closely with Demirjian stage H which corresponds to a minimum age of 17 years in Korean females (Lee et al., 2009), 18 years in Malaysian females (Johan et al., 2012) and 19 years in Thai females (Duangto et al., 2017).
8.33. As maturation is unlikely to occur before the age of 16 years and 7 months this stage of development suggests that the claimed age is unlikely to be supported.
Knee
| Bone | Description | Stage (Vieth et al., 2018) |
|---|---|---|
| Distal femur | There is full fusion at the distal femur. In the T1-w sequence a continuous thin line of intermediate signal intensity between the epiphysis and the diaphysis is visible. The T2-w sequence shows a single thin, discontinuous or dotted line of hyperintense signal in the same position as the described thin line of the corresponding T1-w sequence |
Stage 5 |
| Proximal tibia | There is full fusion at the distal femur. In the T1-w sequence a continuous thin line of intermediate signal intensity between the epiphysis and the diaphysis is visible. The T2-w sequence shows a single thin, discontinuous or dotted line of hyperintense signal in the same position as the described thin line of the corresponding T1-w sequence |
Stage 5 |
8.34. The appearance of the distal femur correlates to stage 5 (Vieth et al, 2018) which corresponds to an age range of 18 years to 22 years 6 months of age. The appearance of the proximal tibia correlates to stage 5 which corresponds to an age range of 17 years 4 months to 22 years 6 months of age.
8.35. This stage of limb development suggests that the claimed age is possible.
Clavicle
Stage of development:
| Bone | Description | Stage (Schmidt et al., 2017) |
|---|---|---|
| Left medial clavicle | Epiphysis has ossified and begun to fuse with the medial surface of the diaphysis with approximately half of the physis (or growth plate) fused | IIIb |
| Right medial clavicle | Epiphysis has ossified and begun to fuse with the medial surface of the diaphysis with approximately half of the physis (or growth plate) fused | IIIb |
8.36. The appearance of the epiphyseal flake at the medial face and stage of fusion of each of the left and right clavicles correlates to stage IIIb for females, which corresponds to an age range of 17 years 8 months to 21 years. This stage of clavicular development does not support the claimed age.
8.37. In this example, mature knee, mature tooth and immature clavicle correspond to panel 332 of Figure 15, and a likelihood ratio of 54. So in this case, there is moderate evidence in favour of the Merton assigned age (20 years).
9. Medical and ethical risks
9.1. The committee was asked to provide guidance on the ethical use of medical imaging techniques. The committee was also asked to consider any medical or ethical risks to the person being assessed and whether these risks would apply equally to all groups who may be assessed.
9.2. It is important to first be clear that, in the case of UASC, the imaging techniques discussed above are better termed ‘biological’ techniques as they are not ostensibly for a direct ‘medical’ purpose or outcome (that is, for investigation or diagnosis of illness). However, age assessment of UASC does have anticipated potential wellbeing benefits for those identified as children, such as access to statutory support and appropriate safeguarding. This supports the principle of justice for the individual and appropriate targeting of limited resources to those for whom they are intended.
9.3. The Merton-compliant age assessment interview process is known to cause some level of distress for individuals and is not ‘harm neutral’. A combinatorial approach of methods that can support the accuracy of the result and reduce the number of prolonged, often challenging Merton interviews, may help to reduce psychological distress to the individual concerned. However, use of biological assessments in addition to social worker interviews could increase distress. Therefore, if introduced, an evaluation of the impact on UASC of carrying out biological assessment should be carried out.
Medical and ethical risks from the use of ionising radiation
9.4. The potential benefits of improved accuracy and swiftness of result, just allocation of resources, justice and protection for UASC with respect to appropriate safeguarding as belonging to a vulnerable group, should be weighed against the risks of using the proposed imaging technique(s). There are known potential risks from the use of ionising radiation. However, for the methods the committee proposes, these risks are extremely low and the committee has been minded to explicitly exclude those biological techniques that rely on imaging that uses higher radiation doses (CT) or exposes areas of the body to radiation that are more radiosensitive (pelvis, clavicle). The committee has focused solely on those imaging techniques that have the lowest ionising radiation dose or none (MRI).
9.5. The committee acknowledges the wider general concern about using ionising radiation and is clear that this biological imaging method is proposed only as a temporary measure. Development of methods using MRI would allow the proposed low-dose ionising radiation methods to be phased out. When weighed against the risks of the Merton-compliant process with its known concerns and drawbacks set out above, it is reasonable to consider the additional options of using the imaging techniques proposed above for the potential long-term wellbeing benefits they can provide to the ‘bona fide’ individual concerned. It should also be borne in mind that following dental and medical screening undertaken by the local authority, the young person may already have medical/dental images of the body area of interest and so no additional radiographic imaging would be required if consent was freely obtained to use these images for age assessment.
Consent
9.6. Any young person under the age of 16 is able to consent to procedures or investigations if they are found to be Gillick competent; that is, that they are felt to have a level of maturity to make their own decisions and are able to understand fully the implications of those decisions, without the need for parental permission or knowledge.
9.7. The person undergoing biological assessment of age should be supported to give a valid informed consent to undergo the biological imaging methods proposed, with information explaining the risks and benefits and they should be free to withhold consent.
9.8. In line with the guidance produced by the European Union Agency for Asylum (EUAA, 2018) no automatic assumptions or consequences should result from refusal to consent to biological age assessment and, in cases of refusal, the applicant should not be automatically considered an adult. The consequences of refusal should not be so disproportionately adverse as to bias the applicant towards consent.
Recommendation 11: UASC should be provided with clear information explaining the risks and benefits of biological evaluation in a format that allows the person undergoing the process to give informed consent and no automatic assumptions or consequences should result from refusal to consent.
9.9. The reasons for refusal should be explored on a case-by-case basis and it should be accepted that there may be many reasons why UASC might not consent to biological assessment. UASC should have the equivalent right as citizens to make decisions that others might regard as unwise. Everyone has their own values, beliefs and preferences which may not be the same as those of other people. For example, many UASC may have witnessed or experienced trauma from their own homeland’s government institutions and may view all authority with suspicion and fear.
9.10. If the applicant decides not to undertake biological age assessment without any justification for the refusal, the application can continue utilising the existing Merton-compliant process.
9.11. The legislation covering mental capacity in England and Wales, Scotland and Northern Ireland (Mental Capacity Act, 2005; Mental Capacity Act (Northern Ireland), 2016; and Adults with Incapacity (Scotland) Act, 2000) should be regarded as applicable to all UASC aged 16 or over. This helps protect and restore power to this vulnerable group of people, some of whom may lack capacity to consent to a decision to undergo a biological age assessment for various reasons (for example, severe mental distress or illness). All professionals involved in the care, treatment and support of UASC have a duty to comply with the codes of practice and principles associated with the relevant legislation.
9.12. If a UASC is found to lack capacity, then any decisions around consent should be made in the best interests or to the benefit of the young person.
9.13. Anyone caring for, or supporting, a UASC who may lack capacity should follow the two-stage functional test of capacity to assess this:
-
Stage 1. Is there an impairment of, or disturbance in, the functioning of the person’s mind or brain? If so,
-
Stage 2. Is the impairment or disturbance sufficient that the person lacks the capacity to make a particular decision?
9.14. The Mental Capacity Act (2005) states that a person is unable to make their own decision (that is, lacks capacity) if they cannot do one or more of the following four things:
1. Understand information given to them
2. Retain that information long enough to be able to make the decision
3. Weigh up the information available to make the decision
4. Communicate their decision – for example by talking, writing, sign language or gesture.
9.15. Capacity is ‘decision’ specific and ‘time’ specific and may need to be reassessed with the UASC if circumstances change.
Impact of the proposed methods on people and groups with protected characteristics
9.16. It is important to recognise that the UASC group comprises people from all over the world. This heterogeneous group will include people of all characteristics, including those deemed protected under the Equality Act 2010 and relevant separate pieces of legislation in Northern Ireland. The protected characteristics are age; disability; gender reassignment; marriage and civil partnership; pregnancy and maternity; race; religion or belief; sex; and sexual orientation. The potential impact of biological age assessment on those with protected characteristics is unknown and if implemented, research in this area would be beneficial.
Recommendation 12: Further research to gauge the differential impact of the proposed age assessment processes on UASC with respect to the protected characteristics in the Equality Act 2010 should be undertaken.
Age and sex
9.17. The proposed additional biological age assessment methods aim to address the heterogeneity within the UASC group and try to more accurately discern amongst those who require the appropriate statutory child services and safeguarding support (minors) and those who do not qualify (adults). The combinatorial approach proposed allows for the selection and use of a specific biological imaging method for a specific UASC whose age is in question, based on the person’s biological sex and claimed age.
Ethnicity
9.18. There is a relative lack of comparative data on age estimation in different populational or geographical subgroups. The interim committee recommends supporting research into biological age assessment methods that will look at larger samples reflecting the diverse ethnic populations of the world to improve the accuracy and applicability of these methods over time and to address disparities in the scientific literature over sample populations.
Recommendation 13: Research into biological age assessment methods based on a wide range of ethnic or geographical sub-groups to confirm and improve accuracy and applicability of these methods should be supported.
Disability
9.19. The interim committee acknowledges that UASC who have specific physical and/or mental disabilities may not be able to undergo one or all of the biological age assessment methods proposed, either by choice or practical limitations. No negative inference should be made from a refusal to consent to undergo a biological age assessment investigation if there is evidence of psychological distress, trauma or mental illness.
10. Conclusion
10.1. The interim committee was asked to advise on methods that that could be implemented within 12 to 18 months as a means to support the existing Merton-compliant process of age assessment.
10.2. The committee acknowledges that there is no infallible method for either biological or social-worker-led age assessment that will provide a perfect match to chronological age.
10.3. The methods that the committee believes could be implemented in this timeframe are those that use imaging to assess both dental and skeletal development.
10.4. The committee recommends that biological age assessment should be carried out using a combination of; radiography of the third molar, radiography of the hand/wrist or MRI of the knee, and MRI of the clavicle. This is based on the substantial body of research published in peer reviewed scientific literature, age assessment based on both dental and skeletal development.
10.5. The committee recommends consideration of biological age assessment via a likelihood ratio approach to discern which is more likely – the claimed age or the Merton assigned age.
10.6. The committee recognises the risk and harm of using ionising radiation and recommends that the use of ionising radiation in age assessment should be limited, with the ultimate aim of eradication and research into the use of non-ionising radiation imaging, such as MRI, should be supported.
Methods for future consideration
10.7. The interim committee has considered the use of facial age estimation and DNA methylation to assess age. It was the view of the interim committee that there was potential for these methods to be used to assess the age of UASC, but that further independent research and development was required to improve accuracy and develop tools applicable to the demographics of UASC. The interim committee recommends that a watching brief should be maintained over the development of these, and other, methods and their potential for use in assisting with assessing the age of UASC be re-evaluated periodically.
Recommendation 14: A watching brief should be maintained over the development of emerging age estimation methods including, but not restricted to, facial images and DNA methylation.
10.8. The interim committee recommends further investigation into development of the following methods to assist with the assessment of age:
1. Assessment of maturation of the third molars by MRI.
2. Assessment of maturation of the hand/wrist by MRI.
3. Baseline assessment of accuracy and repeatability of the Merton-compliant age assessment process.
4. Use of the likelihood ratio to compare the relationship between claimed age and Merton assigned age via biological methods.
11. References
A v London Borough of Croydon and WK v Kent County Council [2009] EWHC 939. Available at https://www.bailii.org/ew/cases/EWHC/Admin/2009/939.html (viewed on 26 April 2022).
Auf der Mauer, M, Säring, D, Stanczus, B, Herrmann, J, Groth, M and Jopp-van Well, E, (2019). ‘A 2-year follow-up MRI study for the evaluation of an age estimation method based on knee bone development’. International Journal of Legal Medicine, 133(1), pages 205-215.
Benchimol, D, Koivisto, J., Kadesjö, Xie-Qi, S, (2018) ‘Effective dose reduction using collimation function in digital panoramic radiography and possible clinical implications in dentistry’. Radiol. Available at https://pubmed.ncbi.nlm.nih.gov/29722543/ (viewed on 27 June 2022).
Black, SM, Aggrawal, A and Payne-James, J, 2010. ‘Age Estimation in the Living: The Practitioner’s Guide’, Oxford, Wiley-Blackwell.
Bogin, B, (1988). ‘Patterns of Human Growth’, Cambridge, Cambridge University Press.
BoneXpert (2019). ’Automated bone age estimation’. Available at https://bonexpert.com/ (viewed on 8 March 2022).
Carneiro JL, Caldas IM, Afonso, A and Cardoso HFV, (2017). ‘Examining the socioeconomic effects on third molar maturation in a Portuguese sample of children, adolescents and young adults’. International Journal of Legal Medicine, 131(1), pages 235-242. DOI: 10.1007/s00414-016-1476-3.
Chiang, KH, Chou, A B, Yen, PS, Ling, CM, Lin, CC, Lee, CC and Chang, PY, (2005). ‘The reliability of using Greulich-Pyle method to determine children’s bone age in Taiwan’. Tzu Chi Medical Journal, 17.
Cole, TJ, (2015). ‘The evidential value of developmental age imaging for assessing age of majority’. Annals of Human Biology, volume 42, issue 4, pages 377-386. DOI: 10.3109/03014460.2015.1031826.
Cole, TJ, Rousham, EK, Hawley, NL, Cameron, N, Norris SA and Pettifor JM, (2015). ‘Ethnic and sex differences in skeletal maturation among the Birth to Twenty cohort in South Africa’. Archives of Disease in Childhood, volume 100, pages 138-143. DOI: 10.1136/archdischild-2014-306399.
Cunningham, C, Scheuer, L and Black, S, (2016). ‘Developmental Juvenile Osteology’, Academic Press.
Dattani, MT and Brook GD eds., (2020). ‘Brook’s Clinical Pediatric Endocrinology’, seventh edition. Wiley, Oxford. Available at: https://onlinelibrary.wiley.com/doi/pdf/10.1002/9781119152712.fmatter (viewed on 27 June 2022).
Dedouit, F, Auriol, J, Rousseau, H, Rougé, D, Crubézy, E and Telmon, N, (2012). ‘Age assessment by magnetic resonance imaging of the knee: a preliminary study’. Forensic Science International, 217(1-3), pages 232-e1.
Department of Health (2011) ‘Quality criteria for young people friendly health services’. Available at: https://www.gov.uk/government/publications/quality-criteria-for-young-people-friendly-health-services (viewed on 22 July 2022).
De Tobel, J, Bauwens, J, Parmentier, A, Pauwels, N, Verstraete, K and Thevissen,P, (2020). ‘Magnetic resonance imaging for forensic age estimation in living children and young adults: a systematic review’. Pediatric Radiology, 2020, 50: 1691-1708.
De Tobel, J, Hillewig, E and Verstraete, KL, (2017). ‘Forensic age estimation based on magnetic resonance imaging of third molars: converting 2D staging into 3D staging’. Annals of Human Biology, 44, pages 121-129. Available at https://doi.org/10.1080/03014460.2016.1223884 (viewed on 27 June 2022).
De Tobel, J, Phlypo, I, Fieuws, S, Politis, C, Verstraete, KL and Thevissen, PW, (2017). ‘Forensic age estimation based on development of third molars: a staging technique for magnetic resonance imaging’. Journal of Forensic Odontostomatology, 2, pages 125-145.
Demirjian, A, Goldstein, H and Tanner, JM, (1973). ‘A new system of dental age assessment’. Human Biology, 45(2), pages 211-227. Available at https://www.jstor.org/stable/41459864 (viewed on 30 June 2022).
Duangto, P, Iamaroon, A, Prasitwattanaseree, S, Mahakkanukrauh, P and Janhom, A, (2017). ‘New models for age estimation and assessment of their accuracy using developing mandibular third molar teeth in a Thai population’. International Journal of Legal Medicine, 131, pages 559-568. Available at https://doi.org/10.1007/s00414-016-1467-4 (viewed on 27 June 2022).
Dvorak J, George J, Junge A and, Hodler J, (2007). ‘Application of MRI of the wrist for age determination in international U-17 soccer competitions’. British Journal of Sports Medicine, 41(8): pages 497-500. Available at https://bjsm.bmj.com/content/41/8/497 (viewed on 27 June 2022).
Dvorak J, George J, Junge A and Hodler J, (2007b). ‘Age determination by magnetic resonance imaging of the wrist in adolescent male football players’. British Journal of Sports Medicine, 41(1): pages 45-52. Available at https://bjsm.bmj.com/content/41/1/45 (viewed on 27 June 2022).
Elamin, F and Liversidge, HM, (2013). ‘Malnutrition Has No Effect on the Timing of Human Tooth Formation’. PLoS One 8, pages 1-8. Available at https://doi.org/10.1371/journal.pone.0072274 (viewed on 27 June 2022).
Ekizoglu, O, Hocaoglu, E, Inci, E, Sayin, I, Solmaz, D, Bilgili, MG and Can, IO, (2015). ‘Forensic age estimation by the Schmeling method: computed tomography analysis of the medial clavicular epiphysis’. International Journal of Legal Medicine, 129(1), pages 203-210.
Ekizoglu O, Er, A, Bozdag, M, Basa, CD, Kacmaz, IE, Moghaddam, N and Grabherr, S, (2021). ‘Forensic age estimation via magnetic resonance imaging of knee in the Turkish population: use of T1-TSE sequence’. International Journal of Legal Medicine, 135, pages 631-637.
European Asylum Support Office (2018) ‘EASO Practical Guide on age assessment’ 2nd Ed. Available at: https://euaa.europa.eu/sites/default/files/easo-practical-guide-on-age-assesment-v3-2018.pdf (viewed 22 July 2022)
Eveleth, PB and Tanner, JM, (1990). ‘Worldwide Variation in Human Growth’, Cambridge, Cambridge University Press.
Gallia, SE, (2020). ‘Dental Development in a UK Population: Does Ethnicity Matter?’ (Doctoral thesis, University of Cambridge). Available at https://doi.org/10.17863/CAM.69763 (viewed on 27 June 2022).
Garn, SM, Lewis AB, and Blizzard RM (1965). ‘Endocrine Factors in Dental Development’ Journal of Dental Research, 44(1); 243. Available at https://journals.sagepub.com/doi/pdf/10.1177/00220345650440012001 (viewed 23 August 2022).
Garn, SM, (1980). ‘Human growth’. Annual Review of Anthropology, 9, pages 275-292.
Greulich, WW and Pyle, SI, (1959). ‘Radiographic Atlas of Skeletal Development of the Hand and Wrist’, Stanford, Stanford University Press.
Groell, R, Lindbichler, F, Riepl, T, Gherra, L, Roposch, A and Fotter, R, (1999). ‘The reliability of bone age determination in central European children using the Greulich and Pyle method’. British Journal of Radiology, 72, pages 461-464.
Guo, YC, Lin, XW, Zhang, WT, Yan, CX, Pan, F, Yan, TL, Li, JP, Chen, T, Schmeling, A and Zhou, H, (2015). ‘Chronology of third molar mineralization in a northern Chinese population’. Rechtsmedizin 25, pages 34-39. Available at https://doi.org/10.1007/s00194-014-0998-6 (viewed on 27 June 2022).
Hackman, L and Black, S, (2012). Does mirror imaging a radiograph affect reliability of age assessment using the Greulich and Pyle Atlas? Journal of Forensic Sciences, 57(5): 1276-1280.
Hackman, L and Black, S, (2013). ‘The Reliability of the Greulich and Pyle Atlas When Applied to a Modern Scottish Population’. Journal of Forensic Sciences, 58, pages 114-119.
Heldring, N, Larsson, A, Rezaie, AR, Råsten-Almqvist, P and Zilg, B, (2022). ‘A probability model for assessing age relative to the 18-year-old threshold based on magnetic resonance imaging of the knee combined with radiography of third molars in the lower jaw’. Forensic Science International, 330, 111108. Available at https://doi.org/10.1016/j.forsciint.2021.111108 (viewed on 27 June 2022).
Hillewig, E, De Tobel, J, Cuche, O, Vandemaele, P, Piette, M and Verstraete, K, (2011). ‘Magnetic resonance imaging of the medial extremity of the clavicle in forensic bone age determination: a new four-minute approach’. European Radiology, 21, pages 757-767.
Hillewig, E, Degroote, JEROEN, Van der Paelt, T, Visscher, A, Vandemaele, P, Lutin, B, D’Hooghe, LIES, Vandriessche, V, Piette, M and Verstraete, K, (2013). ‘Magnetic resonance imaging of the sternal extremity of the clavicle in forensic age estimation: towards more sound age estimates’. International Journal of Legal Medicine, 127(3), pages 677-689.
Jimenez-Castellanos, J, Carmano, A, Catalina-Herrera, CJ and Vinuales, M, (1996). ‘Skeletal Maturation of Wrist and Hand Ossification Centres in Normal Spanish Boys and Girls: A Study Using the Greulich-Pyle Method’. British Journal of Radiology, 72, pages 461-464.
Kasper, A, Austin, D, Kvanli, AH, Rios, TR and Senn, DR, (2009). ‘Reliability of third molar development for age estimation in a Texas Hispanic population: A comparison study’. Journal of Forensic Sciences, 54, pages 651-657. Available at https://doi.org/10.1111/j.1556-4029.2009.01031.x (viewed on 27 June 2022).
Kellinghaus, M, Schulz, R, Vieth, V, Schmidt, S, Pfeiffer, H and Schmeling, A=, (2010). ‘Enhanced possibilities to make statements on the ossification status of the medial clavicular epiphysis using an amplified staging scheme in evaluating thin-slice CT scans’. International Journal of Legal Medicine, 124, pages 321-325. Available at https://doi.org/10.1007/s00414-010-0448-2 (viewed on 27 June 2022).
Kellinghaus, M, Schulz, R, Vieth, V, Schmidt, S and Schmeling, A, (2010b). ‘Forensic age estimation in living subjects based on the ossification status of the medial clavicular epiphysis as revealed by thin-slice multidetector computed tomography’. International Journal of Legal Medicine, 124, pages 149-154.
Koc, A, Karaoglanoglu, M, Erdogan, M, Kosecik, M and Cesur, Y. (2001). ‘Assessment of bone ages: is the Greulich-Pyle method sufficient for Turkish boys?’. Pediatric International, 43, pages 662-665.
Krämer, JA, Schmidt, S, Jürgens, KU, Lentschig, M, Schmeling, A and Vieth, V, (2014). ‘Forensic age estimation in living individuals using 3.0 T MRI of the distal femur’. International Journal of Legal Medicine, 128(3), pages 509-514.
Lee, SH, Lee, JY, Park, HK and Kim, YK, (2009). ‘Development of third molars in Korean juveniles and adolescents’. Forensic Science International, 188, pages 107-111. Available at https://doi.org/10.1016/j.forsciint.2009.03.033 (viewed on 27 June 2022).
Levesque GY, Demirjian A and Tanguay R, (1981). ‘Sexual Dimorphism in the Development, Emergence, and Agenesis of the Mandibular Third Molar’. Journal of Dental Research, 60, pages 1735-1741.
Lewis, AB, (1991). ‘Comparisons between dental and skeletal ages’. Angle Orthodontist, 61(2), pages 87-92. Available at https://meridian.allenpress.com/angle-orthodontist/article/61/2/87/57048/Comparisons-between-dental-and-skeletal-ages (viewed 23 August 2022).
Little, R, Howell, J, and Nixon, P, (2020). ‘COVID-19 and beyond: implications for dental radiography. British Dental Journal, 229(2). Available at https://www.nature.com/articles/s41415-020-1842-x.pdf?origin=ppub (viewed 21 July 2022)
Liversidge, HM, (2008). ‘Timing of human mandibular third molar formation’. Annals of Human Biology, 35, pages 294-321. https://doi.org/10.1080/03014460801971445
Liversidge, HM and Marsden PH, (2010). ‘Estimating age and the likelihood of having attained18 years of age using mandibular third molars’. British Dentistry Journal 209, E13. Available at https://www.nature.com/articles/sj.bdj.2010.976 (viewed on 27 June 2022).
Pinares Toledo, J, Retamal Yermani, R, Ortega Pinto, A and Villanueva Conejeros, R, (2021). ‘Development of the third molar in Chileans: A radiographic study on chronological age’. Forensic Science International: Reports, 3. Available at [https://doi.org/10.1016/j.fsir.2021.100177] (viewed on 27 June 2022).
Public Health England (2011), Ionising radiation: dose comparisons. Available at Ionising radiation: dose comparisons - GOV.UK (www.gov.uk) (viewed on 30 June 2022).
Radiologyinfo.org (2021). ‘Radiation Dose in X-ray and CT Exams’. Available at [https://www.radiologyinfo.org/en/info/safety-xray] (viewed on 21 March 2022).
Royal Society (2020). The use of statistics in legal proceedings, a primer for court. Available at https://royalsociety.org/-/media/about-us/programmes/science-and-law/science-and-law-statistics-primer.pdf (viewed on 8 September 2022)
Schmeling, A, Reisinger, W, Loreck, D, Vendura, K, Markus, W and Geserick, G, (2000). ‘Effects of ethnicity on skeletal maturation: consequences for forensic age estimations’. International Journal of Legal Medicine, 113, pages 253-258.
Schmeling, A, Schulz, R, Reisinger, W, Muhler, M, Wernecke, K-D and Geserick, G, (2004). ‘Studies on the time frame for ossification of the medial clavicular epiphyseal cartilage in conventional radiography’. International Journal of Legal Medicine, 118, pages 5-8. Available at https:// doi.org/10.1007/s00414-003-0404-5 (viewed on 27 June 2022).
Schmidt, S, Mühler, M, Schmeling, A, Reisinger, W and Schulz, R, (2007). ‘Magnetic resonance imaging of the clavicular ossification’. International Journal of Legal Medicine, 121(4), pages 321-324.
Schmidt, S, Henke, CA, Wittschieber, D, Vieth, V, Bajanowski, T, Ramsthaler, F, Püschel, K, Pfeiffer, H, Schmeling, A and Schulz, R, (2016). ‘Optimising magnetic resonance imaging-based evaluation of the ossification of the medial clavicular epiphysis: a multi-centre study’. International Journal of Legal Medicine, 130(6), pages 1615-1621.
Schmidt, S, Ottow, C, Pfeiffer, H, Heindel, W, Vieth, V, Schmeling, A and Schulz, R, (2017). ‘Magnetic resonance imaging-based evaluation of ossification of the medial clavicular epiphysis in forensic age assessment’. International Journal of Legal Medicine, 131(6), pages 1665-1673.
Schulz, R, Muhler, M, Mutze, S, Schmidt, S, Reisinger, W and Schmeling, A.,(2005). ’Studies on the time frame for ossification of the medial epiphysis of the clavicle as revealed by CT scans’. International Journal of Legal Medicine, 119, pages 142-145.
Tanner, JM, Whitehouse, RH, Marshall, WA, Healy, MJR and Goldstein, H, (1975). ‘Assessment of Skeletal Maturity and Prediction of Adult Height’. London, Academic Press.
Thompson, GW, Anderson, DL and Popovich, F, (1975). ‘Sexual Dimorphism in dental mineralization’. Growth 39, pages 289-901.
Thodberg HH, Martin DD. Comment on ‘The evidential value of developmental age imaging for assessing age of majority’ by Cole, Annals of Human Biology 2015. Ann Hum Biol 2016;43:577-8.
Tisè, M, Mazzarini, L, Fabrizzi, G, Ferrante, L, Giorgetti, R and Tagliabracci, A, (2011). ‘Applicability of Greulich and Pyle method for age assessment in forensic practice on an Italian sample’. International Journal of Legal Medicine, 125, pages 411-416.
UNHCR (2009), ‘Guidelines on International Protection No. 8: Child Asylum Claims under Articles 1(A)2 and 1(F) of the 1951 Convention and/or 1967 Protocol relating to the Status of Refugees’. Available at [UNHCR - Guidelines on International Protection No. 8: Child Asylum Claims under Articles 1(A)2 and 1(F) of the 1951 Convention and/or 1967 Protocol relating to the Status of Refugees, 22 December 2009] (viewed on 18 March 2022).
Uys, A, Bernitz, H, Pretorius, S and Steyn, M, (2018). ‘Estimating age and the probability of being at least 18 years of age using third molars: a comparison between Black and White individuals living in South Africa’. International Journal of Legal Medicine, 132: pages 1437-1446. Available at http://doi: 10.1007/s00414-018-1877-6 (viewed on 27 June 2022).
Van Rijn, RR, Lequin, MH, Robben, SGF, Hop, WCJ and Van Kuijk, C, (2001). ‘Is the Greulich and Pyle atlas still valid for Dutch Caucasian children today?’. Pediatric Radiology, 31, pages 748-752.
Varkkola, O, Ranta, H, Metsäniitty, M and Sajantila, A, (2011). ‘Age assessment by the Greulich and Pyle method compared to other skeletal X-ray and dental methods in data from Finnish child victims of the Southeast Asian Tsunami’. Forensic Science, Medicine, and Pathology, 1-6.
Vieth, V, Schulz, R, Brinkmeier, P, Dvorak, J and Schmeling, A, (2014). ‘Age estimation in U-20 football players using 3.0 tesla MRI of the clavicle’. Forensic Science International, 241, pages 118-122.
Vieth, V, Schulz, R, Heindel, W, Pfeiffer, H, Buerke, B, Schmeling, A and Ottow, C, (2018). ‘Forensic age assessment by 3.0 T MRI of the knee: proposal of a new MRI classification of ossification stages’. European Radiology, 28(8), pages 3255-3262.
Widek, T, Genet, P, Merkens, H, Boldt, J, Petrovic, A, Vallis, J and Scheurer, E, (2019). ‘Dental age estimation: The chronology of mineralization and eruption of male third molars with 3T MRI’. Forensic Science International, 297, pages 228-235. https://doi.org/10.1016/j.forsciint.2019.02.019
Wu X, Chen W, Lin F, Huang Q, Zhong J, Gao H, Song Y and Liang H, (2019). ‘DNA methylation profile is a quantitative measure of biological aging in children’. Aging, 11(22), pages 10031-10051.
Yoti (2021). ‘Yoti Age Estimation’. Available at [Yoti Age Estimation White Paper - October 2021 - 20211026] (viewed on 8 March 2022).
Zafar, AM, Nadeem, N, Husen, Y and Ahmad, MN, (2010). ‘An appraisal of Greulich-Pyle Atlas for skeletal age assessment in Pakistan’. Journal of the Pakistan Medical Association, 60, pages 552-555.
12. Authors
Chair
Professor Dame Sue Black, Baroness Black of Strome. President, St John’s College, Oxford.
Committee members
Professor Lucina Hackman, (Deputy Chair), Principal Investigator in Education and Training in Forensic Science, University of Dundee
Dr Adil Akram, Consultant Psychiatrist, Governor of St George’s University Hospitals NHS Foundation Trust and Medical Member, First Tier Tribunal Service, Ministry of Justice
Professor Tim Cole, Professor of Medical Statistics, Great Ormond Street Hospital Institute of Child Health, University College London
Sarah Hammond, Director of Integrated Children’s Services, Kent County Council
Professor Helen Liversidge, Professor of Dental Anthropology, Queen Mary University, London
Dr William Ramsden, Consultant Paediatric Radiologist, Leeds Children’s Hospital and Vice-President Clinical Radiology, Royal College of Radiologists
Dr Tabitha Randell, Consultant in Paediatric Endocrinology, Nottingham University Hospitals NHS Trust and Chair of the British Society for Paediatric Endocrinology and Diabetes
Appendix 1: Glossary
| Term | Definition |
|---|---|
| Age of attainment [of maturity] | The chronological age when maturity is attained. |
| Attainment of maturity | The state of being mature following cessation of growth. |
| Binomial regression | A form of linear regression analysis where the outcome variable is a proportion between 0 and 1, a special case being a binary outcome such as no/yes or immature/mature. Two common forms are probit regression and logistic regression. |
| Bone dysplasia | A range of disorders present during development that affect bones and joints and may impact on growth and bone structure. |
| Clavicle | The collar bone. |
| Computed tomography (CT) | A medical imaging process that uses x-rays taken in multiple directions to take images of the body in 3 dimensions. |
| Demirjian stage H | Appearance of mature tooth where root growth has ceased. |
| Diaphysis | The shaft or central part of a long bone. |
| Distal femur | The knee end of the thigh bone. |
| Distal radius | The wrist end of the outer bone of the forearm. |
| DNA | Deoxyribonucleic acid, the chemical in the cells of an organism that comprises that organism’s heritable material used in development, functioning and reproduction. |
| Epiphysis | The end of a long bone, which initially grows separately until eventually fusing with the shaft of the bone. |
| Intra-oral images | Radiographic images that require the x-ray plate to be placed inside the mouth. |
| Ionising radiation | High energy radiation used in some medical imaging techniques, for example radiography, computed tomography. |
| Likelihood ratio | The weight of evidence in favour of one hypothesis compared to an alternative hypothesis. Here the hypothesis is that the Merton assigned age is correct, while the alternative is the UASC’s claimed age being correct. The likelihood ratio is calculated as the probability of the hypothesis divided by the probability of the alternative hypothesis. |
| Logistic regression | See binomial regression. |
| Mandibular | Pertaining to the lower jaw. |
| Magnetic resonance imaging (MRI) | A medical imaging process that uses radio waves and a powerful magnet to create images of the body in 3 dimensions without radiation. |
| Maturation | The process of growth and development that leads to physical maturity. |
| Mean | The average of a distribution of data, the sum of the values divided by the number of values. |
| Median | The value at the middle of a distribution of data, with half below and half above the median. |
| Medical imaging techniques | Patient imaging techniques most frequently used in medical situations, for example radiography or MRI. |
| Merton-compliant process | A recognised subjective age assessment generally undertaken by social workers. |
| Millisievert (mSv) | Millisievert is a measurement of radiation. |
| Orthopantomogram (OPG) | A panoramic radiograph of the teeth taken from outside the mouth. |
| Probit regression | See binomial regression. |
| Proximal fibula | The knee end of the outer bone of the lower leg. |
| Proximal tibia | The knee end of the shin bone. |
| Radiography (x-ray) | The use of ionising radiation to view the internal form of a body in a single direction as a radiograph. |
| Radiographic | As it relates to radiography. |
| Relative support | A measure of the weight of evidence in favour of a hypothesis (see Likelihood ratio). |
| Sectional orthopantomogram | A partial OPG that views only areas of interest, for example third molars. |
| Standard deviation | A measure of the spread of data around the mean. |
| Third molar | Wisdom tooth. |
| Tibia | The shin bone. |
| Ultrasound (US) | A medical imaging process that uses sound waves to create images of the body without radiation. |
Appendix 2: Regression coefficients for probability plot curves
The figures with probability plots show curves estimated by binomial regression. Their regression coefficients are tabulated here to allow the curves to be reproduced. Except where stated, the coefficients were calculated from published raw data.
| Figure | Region | Description | Sex | Slope | Intercept | Median age (years) |
|---|---|---|---|---|---|---|
| 4[1] | Third molar | Pinares Toleda – Chile | Male | 0.71 | -13.3 | 18.7 |
| 4 | Third molar | Kasper – US Hispanics | Male | 0.50 | -9.74 | 19.3 |
| 4 | Third molar | Lee – Korea | Male | 0.78 | -15.4 | 19.7 |
| 4 | Third molar | Johan –Malaysia | Male | 0.51 | -10.5 | 20.5 |
| 4 | Third molar | Uys – South Africa Black | Male | 0.59 | -11.3 | 19.2 |
| 4 | Third molar | Uys – South Africa White | Male | 0.53 | -10.5 | 19.8 |
| 4 | Third molar | Duangto – Thailand | Male | 0.74 | -15.4 | 20.8 |
| 6[1] | Distal radius | Thodberg –Switzerland | Male | 0.89 | -16.6 | 18.7 |
| 8[2] | Distal femur | Heldring – meta-analysis[3] | Male | 1.57 | -29.3 | 18.7 |
| 8 | Distal femur | Heldring – meta-analysis | Female | 1.45 | -25.0 | 17.3 |
| 10[2] | Medial clavicle | Schmidt – Germany[4] | Male | 1.08 | -25.3 | 23.3 |
| 10 | Medial clavicle | Schmidt – Germany[4] | Female | 1.03 | -24.3 | 23.5 |
| 11[2] | Third molar | Heldring – meta-analysis[3] | Male | 0.92 | -18.7 | 20.3 |
| 11 | Third molar | Heldring – meta-analysis | Female | 0.78 | -16.4 | 21.1 |
[1] probit regression
[2] logistic regression
[3] coefficients kindly provided by Nina Heldring
[4] coefficients calculated by imputing data from the published summary statistics
Table of raw data for mandibular left third molar stage H (mature) in males.
| Age[1] | RCHIL | NCHIL | RHISP | NHISP | RKOR | NKOR | RMAL | NMAL | RSAB | NSAB | RSAW | NSAW | RTHAI | NTHAI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15.5 | 1 | 47 | 0 | 87 | 0 | 61 | 0 | 45 | 0 | 30 | 0 | 33 | 0 | 56 |
| 16.5 | 0 | 44 | 11 | 117 | 0 | 64 | 0 | 45 | 1 | 35 | 0 | 30 | 0 | 65 |
| 17.5 | 10 | 42 | 21 | 127 | 0 | 56 | 0 | 45 | 7 | 30 | 1 | 33 | 0 | 57 |
| 18.5 | 26 | 55 | 51 | 131 | 6 | 54 | 9 | 45 | 12 | 30 | 11 | 34 | 3 | 89 |
| 19.5 | 40 | 51 | 34 | 69 | 32 | 55 | 14 | 45 | 17 | 32 | 13 | 31 | 16 | 93 |
| 20.5 | 34 | 42 | 41 | 58 | 47 | 56 | 26 | 45 | 29 | 37 | 27 | 31 | 45 | 91 |
| 21.5 | 30 | 30 | 38 | 42 | 51 | 57 | 36 | 45 | 27 | 30 | 25 | 30 | 61 | 93 |
| 22.5 | 40 | 44 | 51 | 55 | 40 | 45 | 31 | 32 | 27 | 31 | 82 | 92 | ||
| 23.5 | 40 | 45 | 31 | 31 | 30 | 32 | 50 | 51 | ||||||
| 24.5 | 43 | 45 | 30 | 31 | ||||||||||
| 25.5 | 44 | 45 | 30 | 30 |
[1] midpoint of age group, R response number of individuals at stage H, N number of individuals in age group, RCHIL response Chile, NCHIL N Chile, RHISP response Hispanics, NHISP N Hispanics, RKOR response Korea, NKOR N Korea, RMAL response Malaysia, NMAL N Malaysia, RSAB response South Africa Black, NSAB N South Africa Black, RSAW response South Africa White, NSAW N South Africa White, RTHAI response Thai, NTHAI N Thai.
Data from Pinares Toleda, 2021; Kasper et al., 2009; Lee et al., 2009; Johan et al., 2012; Uys et al., 2018; Duangto et al., 2017.
