Investigation into monkeypox outbreak in England: technical briefing 2
Updated 19 December 2024
Applies to England
Introduction
The UK Health Security Agency (UKHSA) is working with the NHS and the public health agencies of the 4 nations to investigate the monkeypox outbreak in the past few weeks. This briefing is produced to share data useful to other public health investigators and academic partners undertaking related work. It includes early evidence and preliminary analyses which may be subject to change.
Potential levels of the outbreak in England
The outbreak can be considered to fall into one of 4 potential levels of transmission.
Level 1
Incursions from rest of the world – small numbers of imported cases with limited onward transmission.
Level 2
Transmission within a defined sub-population with high number of close contacts.
Level 3
Transmission within multiple sub-populations or larger sub-population.
Level 4
Wider significant community transmission – with potential for endemic and local epi-zoonotic disease.
These may be refined with better understanding of modes of transmission.
At present, England is judged to be in level 2 and is being closely monitored for any evidence of Level 3.
Summary
As of 22 June 2022, there were 846 laboratory confirmed cases of monkeypox in the UK. Of the confirmed cases 22 were in Scotland, 3 in Northern Ireland, 8 in Wales and 813 were in England.
Epidemiological analyses of enhanced surveillance questionnaires suggest that monkeypox continues to be transmitted in defined sexual networks of gay, bisexual, or men who have sex with men (GBMSM), without signals suggesting sustained transmission beyond these networks (transmission level 2).
Nowcasting modelling suggests that the epidemic is still growing, which is consistent with the data on cases by date of report. After correcting for the interval censoring, right truncation, and epidemic phase bias, the mean incubation period was estimated as 9.22 days.
Part 1. Research and evidence gaps prioritisation
UKHSA has carried out a research and evidence gaps analysis relating to the monkeypox outbreak in the UK. We are working collaboratively with academic partners, including National Institute for Health Research Health Protection Research Units and national research funders, to develop and implement rapid studies to address these.
Part 2. Epidemiology update
2.1 Current epidemiological situation
Cases of monkeypox infection were confirmed in England from 6 May 2022. The outbreak has mainly been affecting people without documented history of travel to endemic countries. Up to 22 June 2022 there were 846 laboratory confirmed cases in the UK. Of the confirmed cases 22 were in Scotland, 3 in Northern Ireland, 8 in Wales and 813 were in England.
Table 1. Number of laboratory confirmed cases by devolved administrations, 6 May 2022 to 22 June 2022 (n=846)
| Devolved administrations | Confirmed cases |
|---|---|
| England | 813 |
| Northern Ireland | 3 |
| Scotland | 22 |
| Wales | 8 |
| Total | 846 |
A high proportion of England cases were known to be London residents (79%, 533 of 671 with reported home address), see Table 3. Where gender information was available, 805 (99%) of 810 confirmed cases were male, with 5 confirmed female cases. The median age of confirmed cases in the UK was 37 years old (interquartile range 31 to 43).
Table 2. Number of laboratory confirmed monkeypox cases by region of residence, England, March to 22 June 2022 (n=813)
| Region of residence | Total confirmed |
|---|---|
| East of England | 21 |
| East Midlands | 9 |
| London | 533 |
| North East | 5 |
| North West | 28 |
| South East | 43 |
| South West | 8 |
| West Midlands | 12 |
| Yorkshire and Humber | 12 |
| Unknown* | 142 |
| Total | 813 |
*Address not yet confirmed.
Figure 1 demonstrates symptom onset dates of confirmed cases in England, where known. The median reporting delay, calculated here as the time between symptom onset date and date first included in UKHSA surveillance data, was 8 days for cases newly reported in the week starting 13 June 2022. The reporting delay has improved since early in the incident, from 12 days for cases reported in the week starting 16 May 2022. Figure 2 shows the number of cases by the day of the laboratory result. Most cases (96%) are in men, aged 19 and over (Figure 3).
Recent foreign travel, within 21 days prior to symptom onset, was reported by 131 cases in England (16%), with 97 of these reporting travel within Europe (Figure 4).
Figure 1. Confirmed Monkeypox cases by symptom onset date in England as of 22 June 2022
The dotted line represents reporting delay (between symptom onset and reporting date) of 16 days, based on 90% of cases between 11 June 2022 and 18 June 2022

The data used in this graph can be found in the accompanying spreadsheet.
Figure 2. Incidence of confirmed monkeypox cases by laboratory result date in England as of 22 June 2022
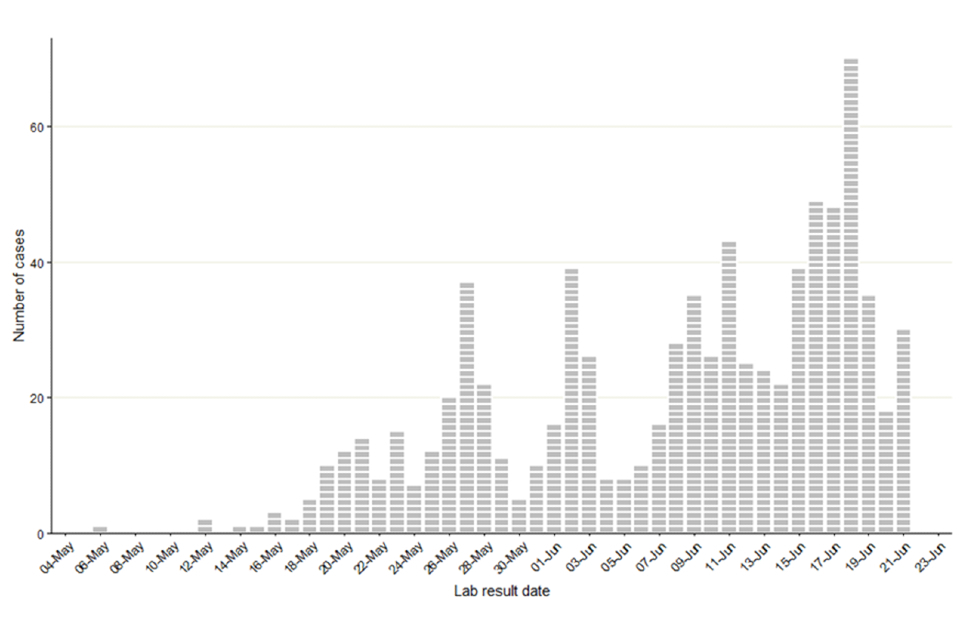
The data used in this graph can be found in the accompanying spreadsheet.
Figure 3. Age and sex distribution of confirmed Monkeypox cases by lab result date in England as of 22 June 2022

The data used in this graph can be found in the accompanying spreadsheet.
Figure 4. Cases with reported foreign travel within the 21 days prior to symptom onset as of 22 June
Travel data obtained from enhanced surveillance questionnaires and Public Health records (HPZone).

The data used in this graph can be found in the accompanying spreadsheet.
2.2 Findings from enhanced surveillance questionnaires
Of the 813 cases identified in England up to 22 June 2022, 321 (39.5%) had enhanced surveillance questionnaires. As reported in technical briefing 1, the majority (96.0%) of cases were gay, bisexual, or men who have sex with men (GBMSM) strongly suggesting transmission in defined sexual networks, both internationally and domestically (Table 3). Cases frequently reported history of a sexually transmitted infection (STI) in the last year (54.2%) and 10 or more sexual partners in the last 3 months (31.8%), suggesting monkeypox is being transmitted in interconnected sexual networks that sustain STI transmission.
Questionnaire data shows that cases have established links with sexual health services for the provision of pre-exposure prophylaxis (PrEP) for HIV (74.2% of those who were HIV negative reported using PrEP, usually daily) or HIV treatment (96.7% of those who were HIV positive reported being on treatment). These existing links with sexual health services will be leveraged to identify GBMSM at highest risk who may benefit from pre-exposure vaccination, as outlined in the vaccination strategy.
Table 3. Selected epidemiological metrics from enhanced surveillance questionnaires in confirmed monkeypox cases in England as of 22 June 2022
N=321, some metrics have slightly smaller denominators due to missing values.
| Metric | N (%) |
|---|---|
| Gay, bisexual, or men who have sex with men | 308 (96.0%) |
| Travel abroad prior to symptom onset (21 days) | 99 (30.8%) |
| Age under 30 years | 68 (21.2%) |
| History of STI in the last year | 174 (54.2%) |
| One of fewer sexual partners in last 3 months | 46 (14.3%) |
| 10 or more sexual partners in last 3 months | 102 (31.8%) |
| Living with HIV | 90 (28.0%) |
| On HIV treatment (among living with HIV) | 87 (96.7%) |
| Ever used PrEP (among HIV negative) | 155 (74.2%) |
Figure 5 shows trends of selected epidemiological metrics in 302 cases with completed questionnaires who had symptom onset dates between epidemiological weeks 18 to 23 (from 1 May 2022 to 11 June 2022). Cases with onset dates before or after these dates were excluded from these analyses due to small numbers. Questionnaire data shows that, between epidemiological weeks 18 to 23, sustained transmission of monkeypox virus in England occurred in defined sexual networks of GBMSM, without significant week-by-week changes in these metrics. Thus, data until 11 June 2022 does not suggest sustained transmission beyond these networks. Ongoing surveillance continues to monitor these trends to inform risk assessments and control interventions.
Figure 5. Trends of selected epidemiological metrics in confirmed monkeypox cases by week of symptom onset in England, epidemiological weeks 18 to 23 (1 May 2022 to 11 June 2022)
N = 302 with completed questionnaires in this time period.

Supplementary data is not available for this figure. Due to delays between symptom onset and questionnaire completion, data for epidemiological week 23 is likely to change and should be interpreted with caution.
Part 3. Transmission dynamics
There is little evidence that transmission dynamics have changed substantially since technical briefing 1. Relatively small numbers of cases means that there remains a great deal of uncertainty about the trajectory of incidence and some of the underlying parameter distributions.
3.1 Incubation period
Data from UKHSA questionnaires show a relatively high number of cases reported travelling to Gran Canaria in early May 2022. Based on these data and international reports, we can therefore infer those individuals who visited Gran Canaria and subsequently contracted monkeypox were likely infected there. That means travel dates to and from Gran Canaria can be used to create an exposure window. Combining this with symptom onset date gives interval censored data on the duration of the incubation period.
We combined the 24 data points obtained through this method with the 9 usable data points on exposure obtained through contact tracing in the UK. This approach gave a sample of 33 individuals, which is more robust than the 9 usable data points obtained through contact tracing alone. After correcting for the interval censoring, right truncation, and epidemic phase bias (Ward and Johnsen, 2021, Overton and Ward, 2021), the mean incubation period was estimated as 9.22 days (90% Credible Interval -CrI: 6.26, 14.8), with the cumulative density function shown in Figure 6.
Figure 6. Cumulative density of estimated incubation period. The red dotted line represents the central estimate, and the red swathe represents the 95% credible interval
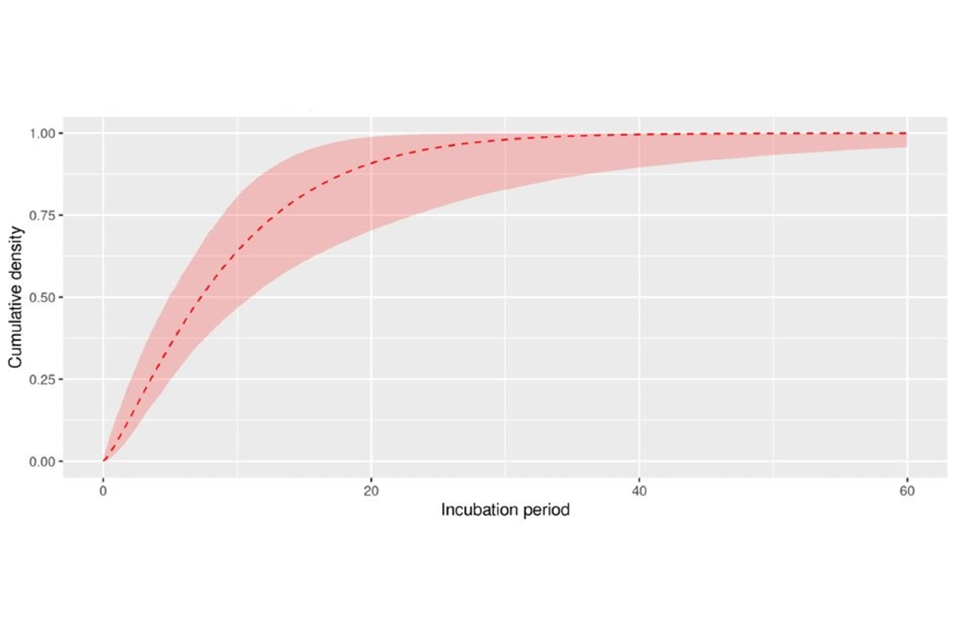
Supplementary data is not available for this figure.
Table 4. Percentiles of the Monkeypox incubation period
| Percentile | 5% | Mean | 95% |
|---|---|---|---|
| 25% | 2.07 | 3.55 | 5.05 |
| 50% | 4.9 | 7.28 | 11.03 |
| 75% | 8.87 | 12.83 | 23.19 |
| 90% | 12.79 | 19.41 | 41.02 |
3.2 Reporting timescales
Understanding the delay from symptom onset to cases being reported is vital for understanding the epidemic trajectory. For cases in the early stages of the outbreak, the reporting delay was long, due to lower public health awareness. As the outbreak has progressed, public health messaging has increased, which should raise awareness of signs and symptoms. To investigate this, we estimated the reporting delay distribution for cases with known symptom onset before 25 May 2022 (N=281) compared to those with known symptom onset after 25 May 2022 (N=245). After correcting for the interval censoring, right truncation, and epidemic phase bias (Ward and Johnsen, 2021, Overton and Ward, 2021), we estimated the mean delay has reduced from 12.7 days (95% CrI: 12.0, 13.4) to 8.38 days (95% CrI: 7.97, 8.81). In addition to a reduction in the mean, variance of the distribution has reduced substantially, with far fewer long reporting delays (Figure 7).
Figure 7. Distribution of lag from symptom onset to case reporting

The area of the curves represents the density of cases with a given reporting lag. The red curve corresponds to more recent cases with known symptom onset after 25 May (blue curve before 25 May 2022).
Supplementary data is not available for this figure.
3.3 Nowcasting by symptom onset date
Visualising the epidemic curve by symptom onset date is affected by the delay from symptom onset and the case being reported. To correct for this delay, nowcasting methods adjust the observed data by the distribution of reporting delays to create predictions of the actual frequency. We use a generalised additive model to nowcast current cases and apply this to non-travel associated cases in England. The nowcasting suggests that the epidemic is still growing (Figure 8), which is consistent with the data on cases by date of report. If travel-associated cases are included, the nowcasting suggests a flatter epidemic curve.
Figure 8. Estimates of nowcast growth rate of Monkeypox cases in England (A) and incidence (B)
The charts exclude cases associated with travel. The shaded area on the A is the 90% CrI, the dark shaded area on B is the 50% CrI and the lighter area is the 90% CrI.
Figure A

Figure B

Note: y-axis denotes incidence of symptom onset.
Supplementary data is not available for these figures.
Sources and acknowledgments
Data sources
Monkeypox virus PCR results are submitted to UKHSA daily by the Rare and Imported Pathogens Laboratory, Porton. Data on people testing positive since 6 May 2022 is enhanced with demographic, symptom, epidemiological, and exposure information extracted from the UKHSA Health Protection Team case management system (HPZone), or collected in enhanced surveillance questionnaires.
Authors of this report
Zahidul Abedin, Charlotte Anderson, Carolina Arevalo, Sooria Balasegaram, Jessica Bridgen, Chloe Byers, Meera Chand, Rachel Christie, Fergus Cumming, Paula Blomquist, Katie Wrenn, Ashley Goddard, Irene Gonsalvez, Diane Hatziioanou, Susan Hopkins, Tim Laurence, Christopher Overton, Karthik Paranthaman, Mateo Prochazka, Cian Ryan, Roberto Vivancos, Thomas Ward, William Welfare
Contributors
UKHSA Data, Epidemiology and Analytics Cell
UKHSA Research and Science Cell
UKHSA Modelling Cell
UKHSA Genomics Public Health Analysis
UKHSA Sexual Health Liaison Group
UKHSA Monkeypox Incident Management Team
Acknowledgements
The authors are grateful to those teams and groups providing data for these analyses including:
British HIV Association (BHIVA)
British Association for Sexual Health and HIV (BASHH)
Sexual Health Services
NHS England and Improvement
High Consequence Infectious Diseases Network
Public Health Scotland
Public Health Wales
Public Health Agency, Northern Ireland
