Investigation into monkeypox outbreak in England: technical briefing 7
Updated 19 December 2024
Applies to England
The UK Health Security Agency (UKHSA) is working with the National Health Service (NHS) and the public health agencies of the 4 nations to investigate the monkeypox outbreak. This briefing is produced to share data useful to other public health investigators and academic partners undertaking related work. It includes early evidence and preliminary analyses which may be subject to change.
Data reported in the technical briefing is as of 26 August 2022 (or as specified in the text) to allow time for analysis.
Potential levels of the outbreak in England
The outbreak can be considered to fall into 1 of 4 potential levels of transmission.
Level 1
Incursions from rest of the world – small numbers of imported cases with limited onward transmission.
Level 2
Transmission within a defined sub-population.
Level 3
Transmission within multiple sub-populations or larger sub-population.
Level 4
Wider significant community transmission – with potential for endemic and local epi-zoonotic disease.
These may be refined with better understanding of modes of transmission.
At present, England is judged to be in level 2.
Part 1. Risk assessment as of 31 August 2022
UK trajectory
Nowcast and growth
There is continued decline in daily case numbers. This is subject to uncertainties around ascertainment. Importation is likely to be contributing to case numbers.
It is likely that multiple factors, including but not limited to vaccination, are contributing to the decline in transmission (moderate confidence).
Assessment (confidence): Negative daily case growth (high).
Geographic spread
The proportion of new cases which are in London has decreased over the course of the outbreak but has ranged between 50 and 70% since July 2022. Daily case numbers are decreasing in and outside of London, with some regional variation.
Assessment (confidence): Approximately stable geography within England (moderate).
Ascertainment
Whilst testing is freely available, testing is likely to be influenced by known risk factors and therefore it is likely that there is under ascertainment. Atypical symptoms, including single or scarce lesions, are reported and there are increasing international reports of subclinical infection.
UK transmission
Outbreak level
Assessment (confidence): Insufficient information.
Level 2 is defined as transmission within a defined sub-population, currently gay, bisexual and men who have sex with men (GBMSM) connected by sexual networks. Enhanced surveillance data does not suggest a change in case mix, although it is available for only 30% (987 out of 3,239) of cases in England and may not be representative of the whole cohort. Out of 3,215 cases with known gender, 99% are men, and there are 41 women. There is no robust evidence of sustained transmission outside some sexual networks of GBMSM, although the increase in cases who are women requires close surveillance.
Assessment (confidence): Level 2 (moderate).
Route of transmission
Whilst the primary reported route is through close or sexual contact, monkeypox virus has been detected in air and environmental samples in the hospital room of infected patients. There are no confirmed instances of airborne transmission. Limited household transmission has been described in the UK.
Detailed investigations have found small numbers of cases with no identified route of acquisition. There are preliminary indications from a small number of cases that transmission may be occurring early in infection, which may include before individuals have identified that they are symptomatic.
Assessment (confidence): Transmitting primarily through close or sexual contact (moderate).
Severity
Observed clinical severity
There are no reported deaths in the UK and a small number of deaths reported globally linked to the outbreak. There is significant morbidity amongst people who are admitted to hospital for clinical care reasons, including severe pain and complications due to secondary bacterial infection. Encephalitis has been reported although it appears uncommon.
Based on genomic surveillance the majority of the outbreak falls in lineage B.1 and these clinical severity attributes cannot be extended to other lineages of monkeypox. There is insufficient data to comment on severity for other lineages.
Assessment (confidence): In current population group, low mortality but significant morbidity (moderate). In wider population, insufficient data.
Virological characterisation
The outbreak falls within Clade IIb, within which the majority of sequenced cases are lineage B.1 or descendants. A small amount of diversity has developed within lineage B.1 both in and out of the UK.
A small number of genomes from other clade IIb lineages have also been detected in 2022. The most prominent additional lineage is A.2. These additional lineages require separate characterisation.
There is very limited laboratory data and it is not currently possible to determine whether the differences between lineages are likely to have biological significance.
There is evidence suggestive of sustained human transmission prior to the 2022 outbreak but not clear-cut evidence of adaptation for improved human transmission.
Assessment (confidence): The primary outbreak lineage is B.1, however additional lineages may be co-circulating (moderate).
International transmission
Routes of transmission reported by other countries
Cases in previously non-endemic countries are reported as primarily in GBMSM. Small number of cases are reported in women and children. In countries with a longer history of monkeypox, apparent wider population transmission is reported with unclear routes. Phylogenetic data suggests that human transmission has been occurring for a number of years in some areas prior to the appearance of the outbreak clade.
Assessment (confidence): Transmitting primarily by close or sexual contact in non-endemic countries (low), unknown transmission routes in endemic countries.
Part 2. Epidemiology update
Whilst data cleaning is carried out routinely, quality assurance samples may have been included from laboratory surveillance systems which will be corrected in subsequent reports.
2.1 Current epidemiological situation
As of 26 August 2022, there were 3,389 laboratory-detected cases of monkeypox in the UK. This includes 3,253 confirmed and 136 highly probable cases. Definitions of cases can be found in previous technical briefings.
Table 1. Number of confirmed and highly probable monkeypox cases by devolved administrations, 6 May 2022 to 26 August 2022
| Devolved administrations | Total | Confirmed | Highly probable |
|---|---|---|---|
| England | 3,239 | 3,103 | 136 |
| Northern Ireland | 27 | 27 | 0 |
| Scotland | 79 | 79 | 0 |
| Wales | 44 | 44 | 0 |
| Total | 3,389 | 3,253 | 136 |
Figure 1 shows the specimen dates of monkeypox cases over time in England.
Figure 1. Confirmed and highly probable monkeypox cases by specimen date* in England as of 26 August 2022
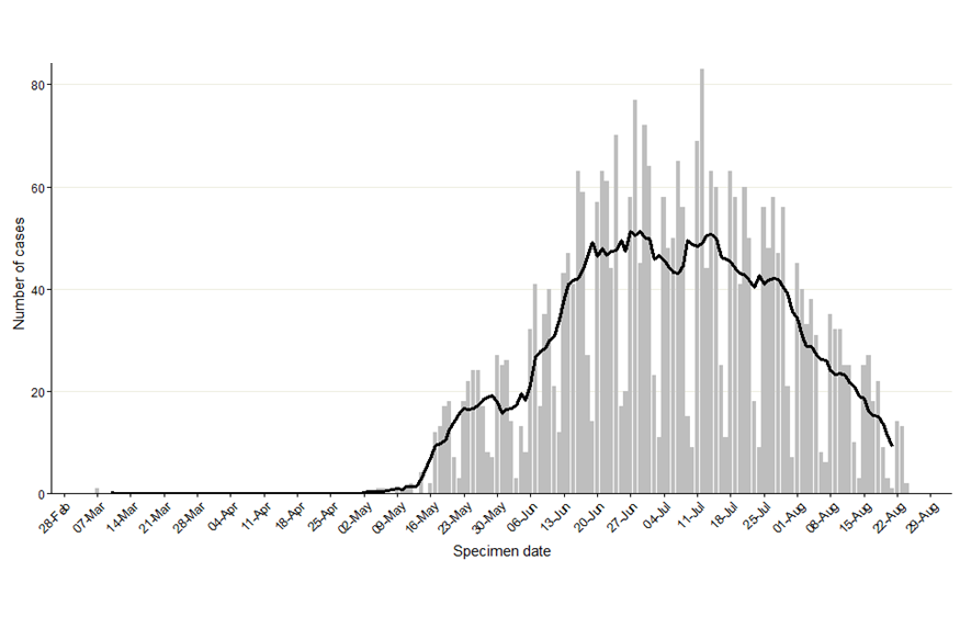
*Where the specimen date is missing, the date the lab received the specimen is used. Where both are missing (mainly among early cases), the date added to the case line list is used (6 out of 3,239).
The data used in this graph can be found in the accompanying spreadsheet.
As of 26 August 2022, 70% of England cases were known to be London residents (2,259 out of 3,225 with reported home address) (Table 2, Figure 2). This has decreased over time, with more than 80% of cases located in London in May 2022 and ranging between 50% and 70% since July 2022 (7-day rolling average proportions seen in Figure 3).
Where gender information was available, 3,174 out of 3,215 (99%) confirmed cases in England were men, and 41 were women (Figure 4). The median age of confirmed and highly probable cases in the UK was 36 years (interquartile range 31 to 44).
Table 2. Number of confirmed and highly probable monkeypox cases by region of residence, England, 6 May 2022 to 26 August 2022
| Region of residence | Total confirmed and highly probable cases | Regional distribution of all cases (% excluding unknown) |
|---|---|---|
| East of England | 111 | 3.4 |
| East Midlands | 50 | 1.6 |
| London | 2,259 | 70.0 |
| North East | 44 | 1.4 |
| North West | 200 | 6.2 |
| South East | 295 | 9.1 |
| South West | 87 | 2.7 |
| West Midlands | 106 | 3.3 |
| Yorkshire and Humber | 73 | 2.3 |
| Unknown | 14 | 0.0 |
| Total | 3,239 | 100.0 |
Figure 2. Cumulative count of confirmed and highly probable monkeypox cases by region of residence in England as of 26 August 2022*
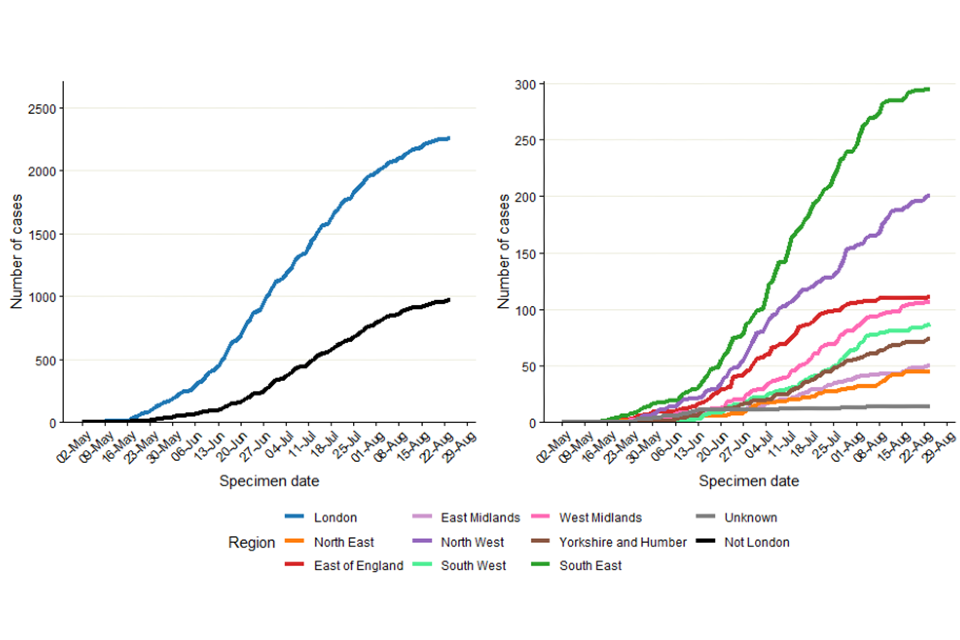
*If the residential postcode is known, then the region of residence is used, otherwise the region of the healthcare facility where the testing occurred at is used. The case with a retrospective specimen date of March 2022 has been omitted from the chart.
The data used in these graphs can be found in the accompanying spreadsheet.
Figure 3. Seven-day rolling average of the percentage of confirmed and highly probable monkeypox cases in London, by specimen date as of 26 August 2022
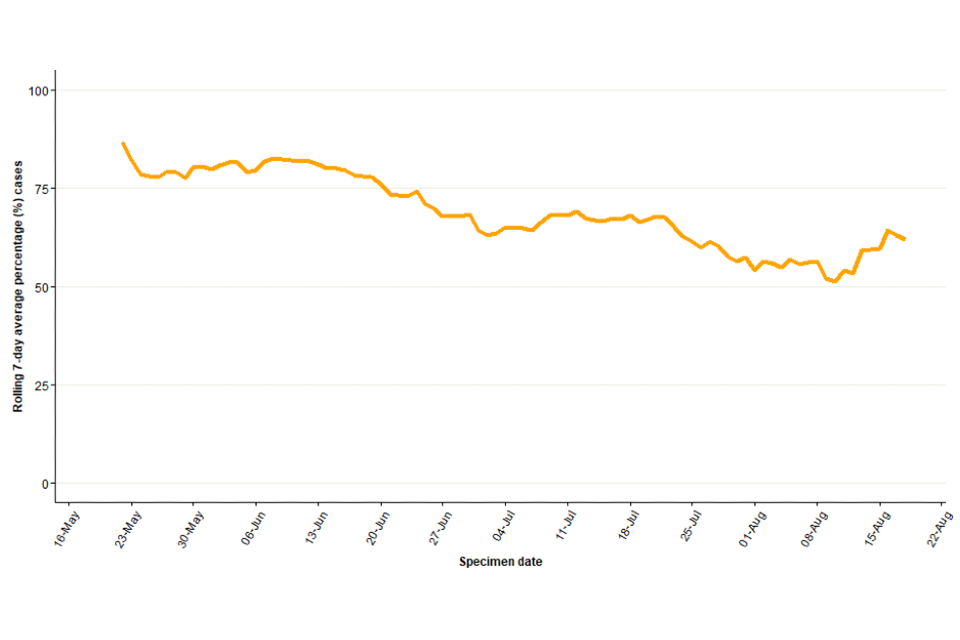
The data used in this graph can be found in the accompanying spreadsheet.
Figure 4. Age and gender distribution of confirmed and highly probable monkeypox cases by lab result date in England as of 26 August 2022
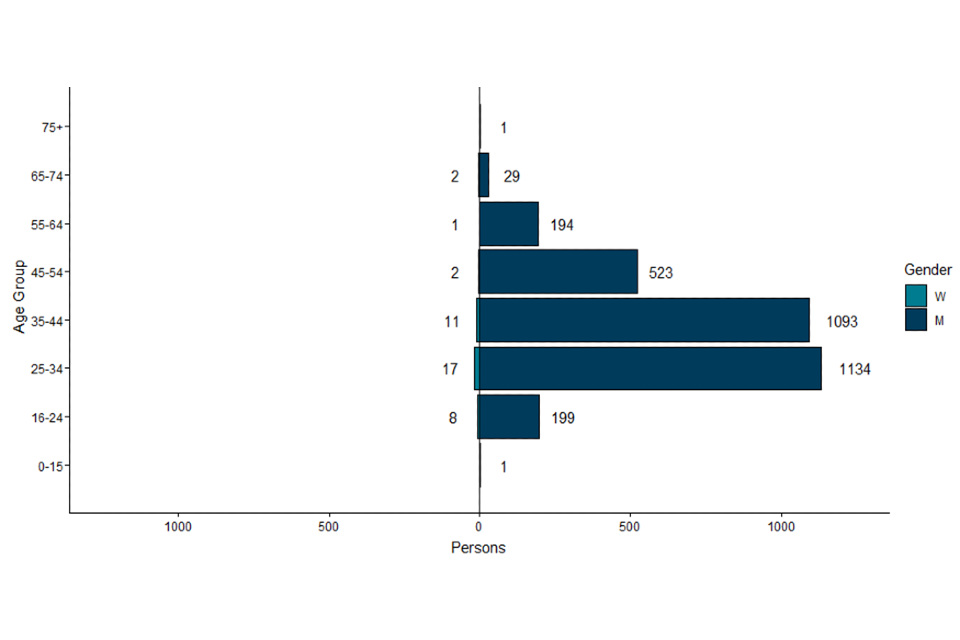
The data used in this graph can be found in the accompanying spreadsheet.
2.2 International travel
In England, 465 confirmed and highly probable monkeypox cases are known to have travelled internationally within the 21 days prior to symptom onset, as of 26 August 2022. The majority of these individuals had travelled to Europe (Table 3), and the most frequently visited country was Spain. Additionally, 7 cases were known to have travelled to endemic countries in West and Central Africa. Travel abroad in the 21 days prior to symptom onset does not equate to acquisition abroad, but this may have occurred for some cases.
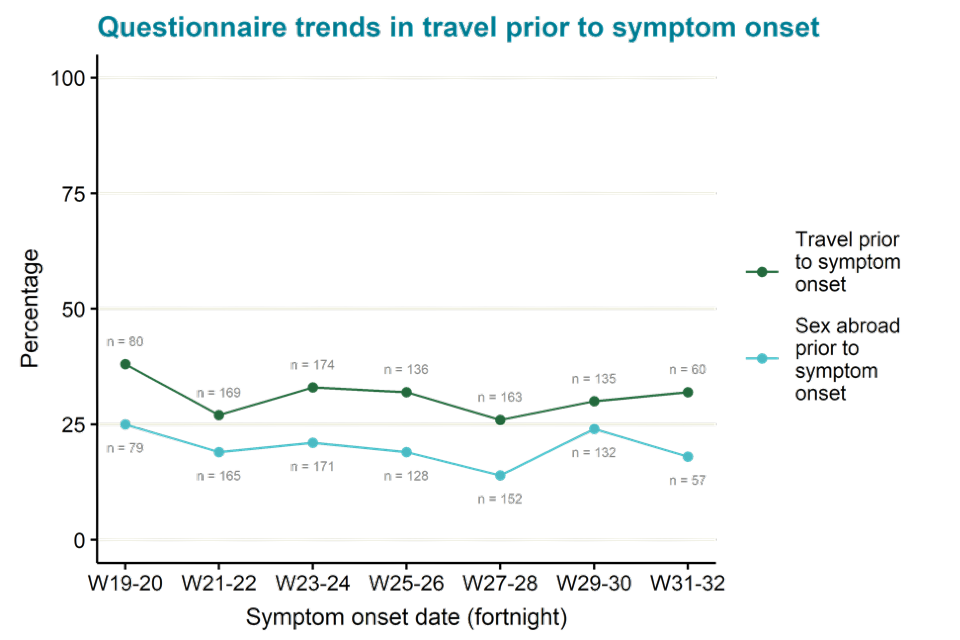
Questionnaire data alone is used for estimating proportions of cases that have travelled, as ascertainment of travel information among all cases has changed over time. As of 26 August 2022, 30% of 963 questionnaire respondents reported travel in the 21 days prior to symptom onset. Among 928 respondents who provided information about sexual activity abroad, 19% (n=180) reported sex abroad. This may mean acquisition abroad was more likely though it is not confirmed.
As shown in Figure 5, travel in the 21 days prior to symptom onset has been relatively stable over time, ranging between 26% (43 out of 163) in week 27 to 28, and 38% (30 out of 80) in week 19 to 20 of respondents, with 32% (19 out of 60) in week 31 to 32.
Table 3. Number of confirmed and highly probable monkeypox cases in England with reported international travel in 21 days prior to symptom onset by United Nations (UN) world region travelled to, as of 26 August 2022
| UN world region | Number of confirmed and highly probable cases with travel history within 21 days prior to symptom onset* | Percentage (%) of total cases | Percentage (%) of cases with pre-symptom travel |
|---|---|---|---|
| Europe | 381 | 11.8 | 81.9 |
| Americas | 38 | 1.2 | 8.2 |
| Asia | 32 | 1.0 | 6.9 |
| Africa | 23 | 0.7 | 4.9 |
| Oceania | 6 | 0.2 | 1.3 |
*Table counts visits to UN world regions by cases. If a case visited multiple regions, they will be counted multiple times in the table. Total proportions may be underestimated as travel data is not available for all cases.
Figure 5. Proportion of questionnaire respondents over time with travel in 21 days prior to symptom onset, from week 19 to week 32, as of 26 August 2022. Numbers next to line represent denominator per 2-week period.
The data used in this graph can be found in the accompanying spreadsheet.
2.3 Findings from enhanced surveillance questionnaires
Of the 3,239 cases identified in England by 26 August 2022, a total of 987 (30%) had completed enhanced surveillance questionnaires by 29 August 2022. Information from enhanced questionnaires should be interpreted with caution, due to the low uptake and because uptake has changed over time. People completing questionnaires may not be representative of all those affected.
Most respondents were of white ethnicity (78%), followed by mixed (9%) and Asian (7%) ethnicities (Table 4). Additionally, most cases were born in the UK or other European countries, although 9% reported being born in Latin American or Caribbean countries.
Table 4. Ethnicity and region of birth from enhanced surveillance questionnaires in confirmed monkeypox cases in England as of 29 August 2022
| Ethnicity | Count | Percentage (%) |
|---|---|---|
| White | 765 | 77.5% |
| Mixed | 93 | 9.4% |
| Asian | 63 | 6.4% |
| Black | 39 | 4.0% |
| Other | 1 | 0.1% |
| Unknown | 26 | 2.6% |
| Region of birth | Count | Percentage (%) |
|---|---|---|
| UK | 534 | 54.1% |
| Europe | 209 | 21.2% |
| Latin America and the Caribbean | 92 | 9.3% |
| Asia | 49 | 5.0% |
| Africa | 30 | 3.0% |
| Oceania | 21 | 2.1% |
| Northern America | 16 | 1.6% |
| Unknown | 36 | 3.6% |
As shown in Table 5 and reported in previous technical briefings, monkeypox is predominantly being transmitted in interconnected sexual networks of GBMSM: the majority of cases report multiple sexual partners in the last 3 months, history of a sexually transmitted infection (STI) in the last year, and/or use of human immunodeficiency virus pre-exposure prophylaxis (HIV PrEP).
Table 5. Selected epidemiological metrics from enhanced surveillance questionnaires in confirmed monkeypox cases in England as of 29 August 2022
N=987, some metrics have smaller denominators due to missing values
| Metric | Count | Denominator (excluding cases with missing responses) | Percentage (%) |
|---|---|---|---|
| Gay, bisexual, or men who have sex with men | 921 | 953 | 96.6% |
| History of STI in the last year | 511 | 966 | 52.9% |
| 4 to 9 partners in last 3 months | 332 | 972 | 34.2% |
| 10+ sexual partners in last 3 months | 284 | 972 | 29.2% |
| Living with HIV | 246 | 934 | 26.3% |
| Ever used PrEP (among HIV negative) | 521 | 673 | 77.4% |
Figure 6 shows trends of the selected epidemiological metrics over time, among cases with completed questionnaires and with symptom onset dates between epidemiological weeks 19 to 32 (from 8 May 2022 to 13 August 2022). Trends continue to remain the same as reported in technical briefing 6.
Detailed analyses of questionnaire data, in combination with manual review of case management notes, was undertaken to describe the small number of cases that are known to be not GBMSM including examining possible routes of acquisition. Of 41 cases who were women aged 16 and above, 15 out of 37 (41%) with available information were transgender women.
Additionally, 18 had evidence of possible transmission during sexual contact (due to sex with a reported case or high numbers of anonymous sexual partners through sex work), 10 appeared to have non-sexual routes of acquisition (either likely household transmission or no reported sexual activity in 21 days prior), and 13 had unclear possible routes of acquisition or no information.
Additionally, there were 24 cisgender men who reported being heterosexual and reported not having had sex with another man in the past 21 days. Of these, a small number had evidence of possible transmission during sexual contact with cisgender women.
Figure 6. Trends of selected epidemiological metrics in monkeypox cases with completed questionnaires, by week of symptom onset in England, epidemiological weeks 19 to 32 (8 May 2022 to 13 August 2022)
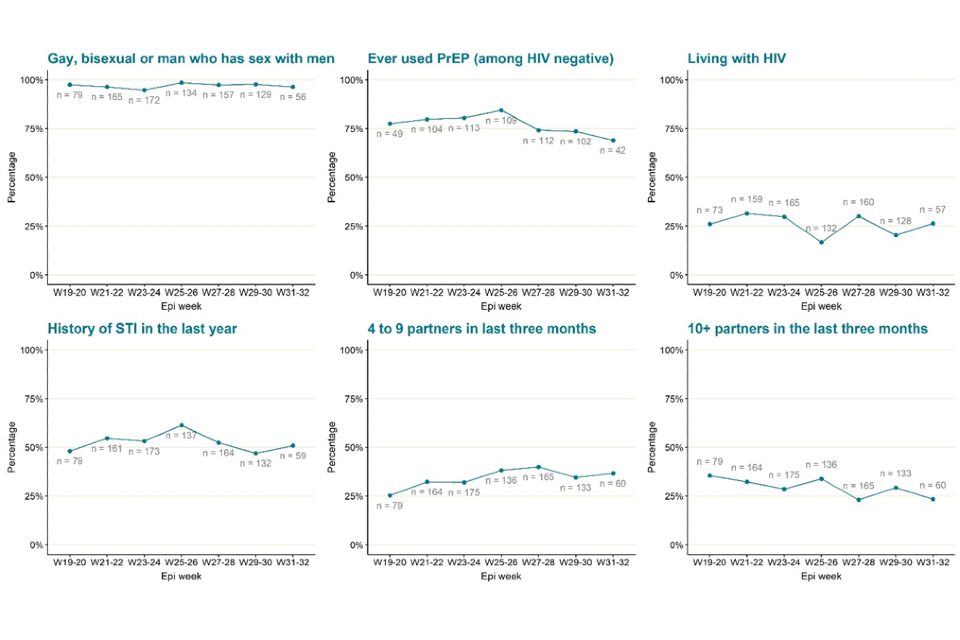
The data used in these graphs can be found in the accompanying spreadsheet. Due to delays between symptom onset and questionnaire completion, data for the most recent epidemiological weeks may change and should be interpreted with caution.
2.4 Testing data
Testing for monkeypox in the UK is conducted by the UKHSA Rare and Imported Pathogen Laboratory (RIPL) as well as NHS and private laboratories that have begun using monkeypox or orthopox polymerase chain reaction (PCR) tests since early July 2022.
Full testing data is available for RIPL. Up to 26 August 2022, 5,724 individuals were tested for monkeypox in this laboratory, of which 42% (2,426) were positive. Further analyses are not included in this technical briefing as RIPL positive tests made up only 32% of all positives in the most recent 2 weeks of data (13 August to 26 August 2022) and the representativeness of RIPL has changed over time, with a lower proportion of London cases detected in RIPL compared to other laboratories throughout July 2022.
Part 3. Monkeypox vaccination
3.1 Vaccines administered
As of 30 August 2022, a total of 38,079 administered doses of vaccine have been recorded, of which 33,918 doses have been administered as pre-exposure vaccination, primarily to gay, bisexual, and other men who have sex with men who are at highest risk of exposure. A further 1,992 doses have been given to healthcare workers managing monkeypox cases and 2,169 doses have been given to close contacts of cases.
Vaccination has been targeted to London where around 70% of the cases have been seen (Table 2).
The recommended groups for vaccination are set out in UKHSA guidance.
3.2 Assessing incidence and vaccine usage over time
UKHSA has analysed the association between the vaccine roll-out mentioned in Section 3.1 and the fall in confirmed cases in the last few weeks. Once lags (between infection and reporting, and vaccination and the onset of immunity) are considered, it is likely that infections started to decrease too early for this to be due to the vaccine programme alone. It is difficult to fully explain the start of this decrease, which also occurred in other countries to different extents. The main possibilities are: i) that we are closer to saturation than previously thought; ii) that case ascertainment has changed in recent weeks; and iii) that behaviour has changed to avoid risk.
Modelling suggests that the early fall in case numbers is unlikely to be fully explained by saturation in the number of susceptible individuals given estimates of various population sizes and what is known about transmission networks. Ascertainment would need to be implausibly low for the current number of cases to represent an outbreak that is approaching the size of the susceptible population. Data on behavioural change will be important to understand to what extent this is contributing as this is likely to be variable over time. It is likely that some combination of these 3 factors has contributed so far, and vaccines will play a larger role in coming weeks.
Part 4. Transmission dynamics
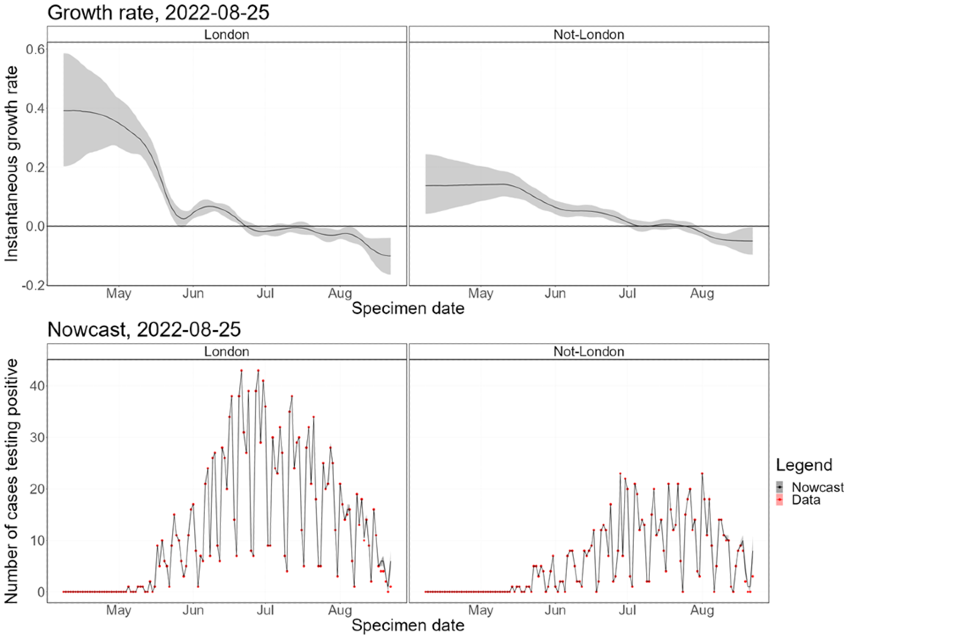
Nowcasting by both specimen date and reporting date continues to indicate a declining epidemic. This is true both inside and outside London.
4.1 Nowcasting by specimen date
The nowcasting using models described in previous technical briefings suggests that the growth in confirmed daily cases is negative (Figure 7). The nowcast estimate of non-travel cases is around 10 per day. The epidemic inside London has declined since mid-July 2022 (Figure 8), with the epidemic outside of London declining since early August 2022.
Modelling on transmission during early infection (mentioned in the risk assessment) will be provided in the next technical briefing.
Figure 7. Nowcast growth rate and incidence of monkeypox cases in England. 7a shows estimates by specimen date, 7b shows estimates by report date
The charts exclude cases associated with travel. The shaded area is the 90% Credible Interval (CrI), the dark shaded area is the 50% CrI and the lighter area is the 90% CrI.
Figure 7a
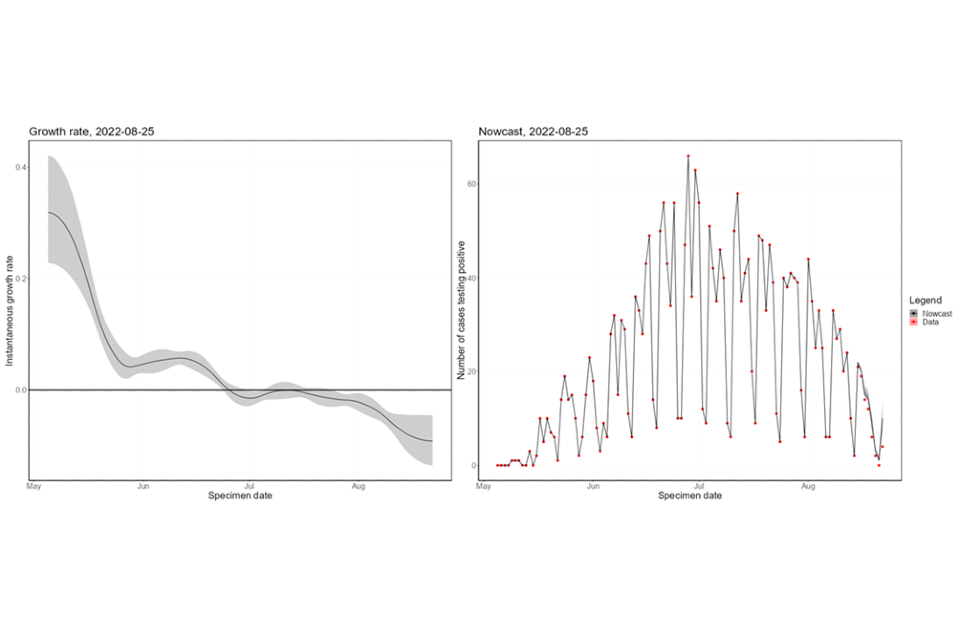
Figure 7b
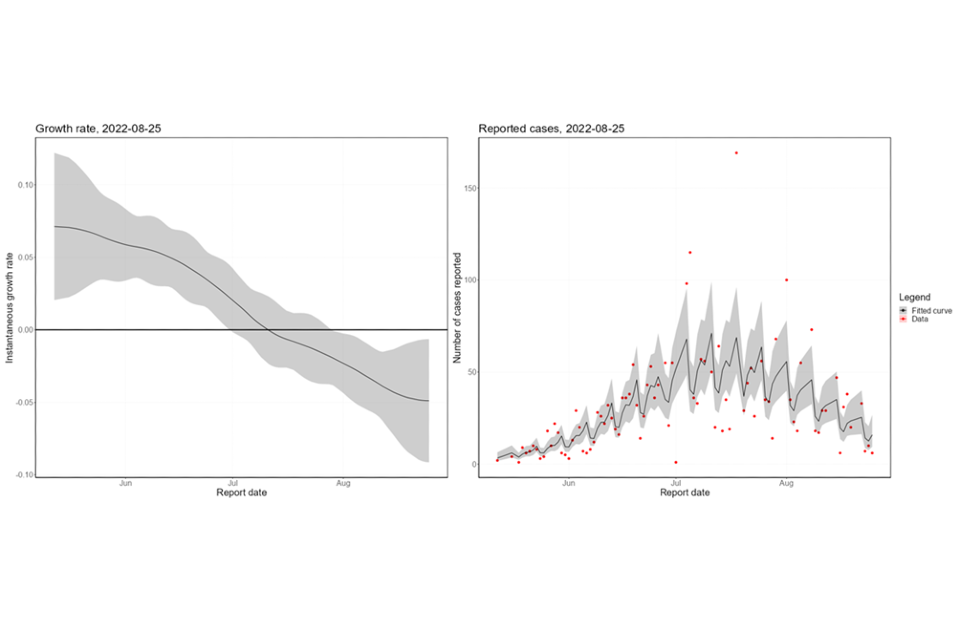
Supplementary data is not available for these figures.
Figure 8. Estimates of nowcast growth rate and incidence by specimen date inside and outside London
The charts exclude cases associated with travel. The shaded area is the 90% Credible Interval (CrI), the dark shaded area is the 50% CrI and the lighter area is the 90% CrI.
Supplementary data is not available for this figure.
4.2 Temporal trends in gender distribution
Thus far, the majority of cases have occurred in defined networks of GBMSM. To assess whether the outbreak is moving away from this initial subpopulation, we investigate temporal trends in the proportion of cases that do not identify as women.
The proportion of non-contact-tracing-linked female cases has increased over the last few weeks, though is currently within statistically significant limits of the distribution (Figure 9). Removing female cases with known links to MSM communities and trans women (n=16) from the count of female cases accounts for most of this overall trend. The data remains under close surveillance, as the decreasing number of cases means confidence in this approach will become lower.
Figure 9. Binomial probability of male cases using a binomial exact test
The purple shaded area is the null hypothesis (which implies no change in the rate). The solid black line is the proportion observed in the latest week, plotted by the first day of the focal week. Plot a) removes 16 cases (at time of analysis) which were known to have a link to a GBMSM primary case or are trans women. Plot b) analysis including all women.
Figure 9a
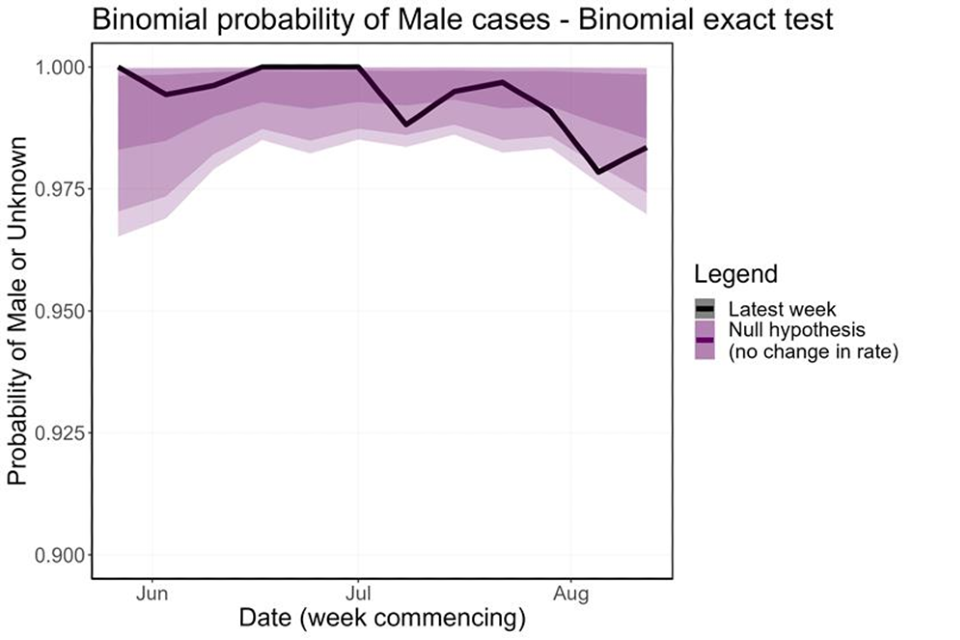
Figure 9b
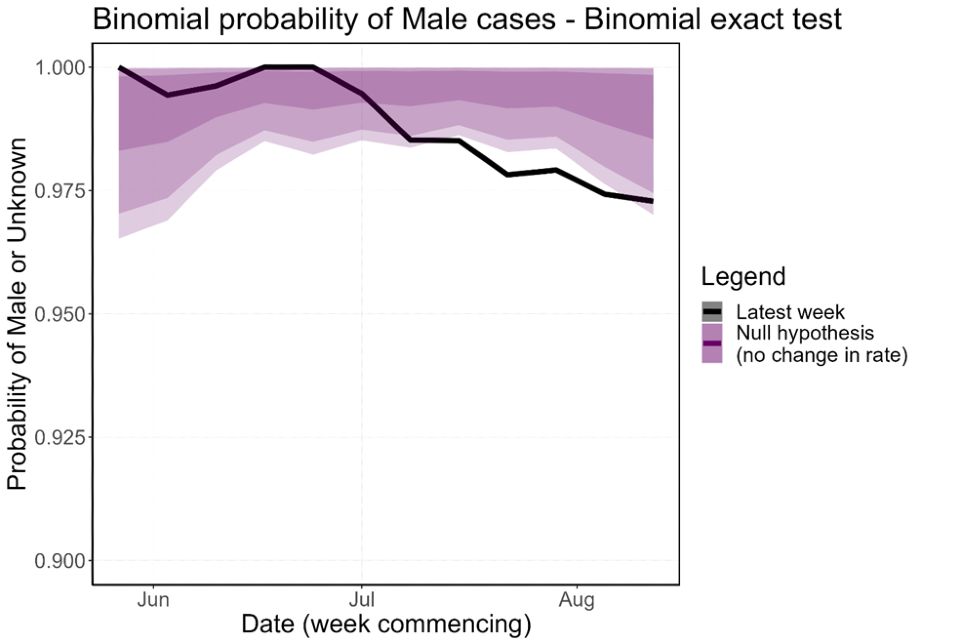
Supplementary data is not available for this figure.
Part 5. UK genomic surveillance
The phylogeny of monkeypox virus is separated into Clade I (formerly known as central African or Congo Basin clade; reportedly associated with more severe outcomes), Clade IIa (formerly known as West African clade; outbreak associated with imported animals), and Clade IIb, which contains the lineage associated with the current outbreak as well as some other genomes. All UK genomes in 2022 fall into Clade IIb.
Of 3,253 confirmed cases in the UK, sequencing has been attempted for 186. A total of 169 cases have at least one sequence that passed quality control (70% genome coverage more than or equal to 30X and 90% genome coverage more than or equal to 20X). A total of 153 cases have one sequence and 16 cases have more than one sequence available. Cases are chosen for sequencing if at least one sample has a monkeypox PCR cycle threshold below 20, or the case is considered a potential high consequence infectious disease case due to recent travel to West or Central Africa.
Of the 169 UK cases with at least one sequence available, all cases fall within Clade IIb. One hundred and sixty-six are lineage B.1, 2 are lineage A.2 and one is not part of a described sub-lineage.
A total of 25 sequenced cases have travel information. Of 16 cases with travel to Europe, all are lineage B.1. Of 5 cases with travel to the African region, 2 are lineage B.1, 2 are A.2 (one is a low-quality sequence, and therefore considered “probable”) and one is currently undergoing investigation but is outside B.1. The 4 other sequenced cases with travel (other regions or unknown destination) were all within the B.1 lineage.
Both globally and within the UK, the primary outbreak lineage remains B.1. Within B.1 in the UK, a small amount of diversity has accrued. In total 247 single nucleotide polymorphisms (SNPs) have been observed (133 non-synonymous). Of 247 SNPs observed, 229 are potentially consistent with the action of apolipoprotein B mRNA editing enzyme catalytic polypeptide 3 (APOBEC3) as described in the linked virological post. The maximum SNPs between any genome and the reference (ON563414.3) is 11 in total (2 sequences) and 5 or 6 non-synonymous.
Sources and acknowledgments
Data sources
Monkeypox virus PCR results are submitted to UKHSA daily by the Rare and Imported Pathogens Laboratory, Porton, UKHSA regional laboratories and NHS laboratories undertaking testing. Data on people testing positive since 6 May 2022 is enhanced with demographic, symptom, epidemiological, and exposure information extracted from the UKHSA Health Protection Team case management system (HPZone), or collected in enhanced surveillance questionnaires. Enhanced surveillance questionnaires include data collected via rapid sexual health questionnaires administered during the initial weeks of the outbreak (used from 27 to 31 May 2022), questionnaires completed by health protection teams during telephone interviews (used from 1 to 24 June 2022), and self-completed questionnaires sent electronically to cases (used from 25 June 2022 onwards).
Authors of this report
Zahidul Abedin, Paula Blomquist, Jessica Bridgen, Chloe Byers, Meera Chand, Kristine Cooper, Fergus Cumming, Julie Day, Eileen Gallagher, Ashley Goddard, Irene Gonsalvez, Alice Graham, Natalie Groves, James Guilder, Susan Hopkins, Luke Hounsome, Jamie Lopez-Bernal, Nicola Love, Richard Myers, Christopher Overton, Karthik Paranthaman, Mateo Prochazka, Andrew Rambaut, James Sedgwick, Roberto Vivancos, Thomas Ward, Nick Watkins, William Welfare, Katie Wrenn.
Contributors
UKHSA Data, Epidemiology and Analytics Cell
UKHSA Research and Science Cell
UKHSA Modelling Cell
UKHSA Genomics Public Health Analysis
UKHSA Sexual Health Liaison Group
UKHSA Monkeypox Incident Management Team
Monkeypox Technical Group
The Monkeypox Technical Group includes members with expertise in clinical infectious diseases, clinical research, epidemiology, genomics, modelling, and virology:
- Meera Chand (Chair), UKHSA
- Andre Charlett, UKHSA
- Andrew Rambaut, University of Edinburgh
- Alison Rodger, University College London
- Allan Bennett, UKHSA
- Ashley Otter, UKHSA
- Calum Semple, University of Liverpool
- Christophe Fraser, University of Oxford
- Claire Dewsnap, British Association for Sexual Health and HIV
- Claire Gordon, UKHSA
- Colin Brown, UKHSA
- David Ulaeto, Defence Science and Technology Laboratory
- Erik Volz, Imperial College London
- Emma Thomson, Medical Research Council-University of Glasgow Centre for Virus Research
- Fergus Cumming, UKHSA
- Giri Shankar, Public Health Wales
- Geoffrey L. Smith, University of Cambridge
- Geraldine O’Hara, High Consequence Infectious Diseases Network
- Health and Social Care Northern Ireland
- Helen Fifer, UKHSA
- Isabel Oliver, UKHSA
- Jake Dunning, University of Oxford and Royal Free Hospital
- Jason Mercer, University of Birmingham
- Maria Rossi, Public Health Scotland
- Matt Keeling, Warwick University
- Matt Phillips, British Association for Sexual Health and HIV
- Natalie Groves, UKHSA
- Neil Ferguson, Imperial College London
- Nicholas Loman, University of Birmingham and UKHSA
- Obaghe Edeghere, UKHSA
- Richard Myers, UKHSA
- Steven Riley, UKHSA
- Susan Hopkins, UKHSA
- Tommy Rampling, UKHSA
Acknowledgements
The authors are grateful to those teams and groups providing data for these analyses including:
- British HIV Association (BHIVA)
- British Association for Sexual Health and HIV (BASHH)
- Sexual Health Services
- NHS England and Improvement
- High Consequence Infectious Diseases Network
- Public Health Scotland
- Public Health Wales
- Public Health Agency, Northern Ireland
