National Information Board Prospectus: September 2015
Published 29 September 2015
Foreword
Tim Kelsey, National Information Director Chair, National Information Board
Making better use of data and technology for patients, the public and those who serve them is key to delivering a safe, effective and sustainable health and care service. The National Information Board (NIB) was established to resolve this central challenge for our NHS: how best to harness the power of the information revolution that has transformed the rest of our lives.
The NIB is a unique collaboration which brings together all national health and care bodies, together with leaders in clinical medicine, the third sector and civil society. Since it was set up in April 2014 by Dame Una O’Brien, Permanent Secretary at the Department of Health, members have worked in partnership with citizens across England to develop detailed proposals for a transparent, digitally supported health and care service which empowers people and communities.
The NIB is charged with supporting delivery of the objectives of the Five Year Forward View which sets out the priorities for the NHS to 2020. In its annual report next spring the NIB will report on implementation of those strategic outcomes – this Prospectus reviews progress over the last 18 months.
Last November, NIB published Personalised Health and Care 2020: A Framework for Action (PHC2020). It represents a new consensus: patients and carers need better access to digital services – including access to their own records – to take more control of their care, when they want to; citizens should be able to use safe ‘apps’ and digital tools to help them manage their wellbeing and prevent disease; clinicians need real time patient data so that, wherever they treat a person, they can see their history. Patients are put at risk where paper is the currency of clinical practice.
Real progress is already being made:
- in April, England became the first country in world to offer citizens the ability to access their GP records online and other digital services in primary care. In the first quarter of this year, more than 3.7m repeat prescriptions were ordered online
- more than 96% of people registered with a GP now have a summary care record and 73% of ambulance, 85% of 111 and 35% of A&E services now having access to view, meaning clinicians can treat patients more safely based on knowledge of their medication history and especially allergies and other likely adverse reactions to drugs. A pilot is currently underway providing access from within the ambulance cab itself, giving access directly to paramedics at the point of care. GP’s are now able to include additional information a patients summary care record with their consent, providing a clinically richer data set such as past and present conditions and procedures, as well as care plans and preferences
- MyNHS is a new digital tool that has transformed transparency of local services and allows you to compare the outcomes and effectiveness of more than 37,600 health and care organisations
Much more needs to be done – and the role of the NIB is essential, particularly in ensuring consistent national support for local health and care communities to lead transformation. There are many challenges to effective local delivery – technical capability and capacity and prioritised funding among them.
Ensuring effective implementation of PHC2020 is just one part of the NIB’s work – over the next few months we look forward to reviewing the government’s transparency programme and to working with Baroness Martha Lane-Fox on widening digital participation.
The NIB is committed to transparency and public participation: we livestream our summit meetings, publish all our board papers and welcome your feedback and your engagement.If you’d like to make a comment on this Prospectus please speak to us on Twitter or by email here: nibsecretariat@dh.gsi.gov.uk
I would like to thank all the members of NIB and its excellent secretariat for their commitment and hard work – it has been a great privilege to be your chair. I’d also like, on our collective behalf, to thank colleagues in health and care, industry and civil society who have given their time to work with us.
Will Cavendish, Director General, Innovation, Growth & Technology, Department of Health
Over the course of 2015, National Information Board members, the national organisations that are responsible for health and care services on behalf of the public, have demonstrated their commitment to harnessing the power of technology and digital by collaborating to develop plans to deliver the vision set out in Personalised Health and Care 2020: A Framework for Action (PHC2020) PHC2020 is at the very heart of delivery of the government’s priorities for health and care and builds upon the commitment to exploit the information revolution outlined in the NHS Five Year Forward View.
It is critical that we create the right conditions for this work to thrive and maximise the benefits for patients and citizens whilst ensuring genuine value for money for taxpayers. In my role as Informatics Accountable Officer, I am looking forward to National Information Board members continuing to work together to achieve this.
Introduction
This document acts as an interim review of progress for the National Information Board, in advance of the Annual Report which is due to be published in March 2016.
It aims to:
- describe the impact of PHC2020 for patients, citizens and professionals
- provide an overview of progress to date, including a description of how the NIB has been established and its membership
- set out the PHC2020 commitments which are due to deliver before publication of the annual report in March 2016
- provide a mechanism to set out how the success and impact of the NIB can be measured for patients, citizens and professionals
A year in numbers
The NIB was launched in March 2014, and since then a significant amount of work has been undertaken, with the framework (PHC2020) setting out the strategy and the roadmaps describing the blueprint for delivery. Whilst progress will be reported formally in the Annual Report in March, here is a quick summary of some of the highlights so far:
- 91 commitments made in PHC2020, of which 17 are already delivered
- 47 organisations represented across the NIB
- 40 items of feedback received on PHC2020
- 6 Leadership summits held with 1720 live stream views
- 9 working group meetings
- 4 online publications
- 17 blogs
- 326 twitter followers, and rising
- 66.5k twitter impressions
- 6 independent members appointed
- 10 work streams established
- 8 roadmaps published
Phase 1: establishing the NIB
- March 2014 – Inaugural meeting of the National Information Board
-
June 2014 Leadership summit – Secretary of State, Jeremy Hunt, launches the first NIB Leadership Summit and presents: “Unleashing the power of information and technology for patients and those who serve them – one year on”
- October 2014 – Independent members appointed and Terms of reference published.
The scope of the NIB business includes informatics and information technology and information activity across the health and care system, for which it will agree and set a high level strategy and vision.
The NIB strategy, developed under the leadership of the NIB, and agreed on behalf of the Department, will provide strategy direction on all informatics programmes. It will also provide advice and guidance (via the strategy) to the DH Informatics Accountable Officer (IAO) as to how centrally provided resources should be most effectively deployed to achieve the aims of government policy as reflected in the NIB strategy.
What is the NIB?
The National Information Board (NIB) was established in March 2014, building on the former Informatics Services Commissioning Group (ISCG) hosted by NHS England. Read about the role of NIB.
PHC2020
In November 2014 the NIB produced Personalised Health and Care 2020 (PHC2020), which considers what progress the health and care system has already made and what can be learnt from other industries and the wider economy. PHC2020 is a framework for action that will support frontline staff, patients and citizens to take better advantage of the digital opportunity. PHC2020 builds upon the commitment to exploit the information revolution outlined in the NHS Five Year Forward View (FYFV) and seeks to address the 3 key challenges for health and care the FYFV identifies:
- the health and wellbeing gap
- the care and quality gap
- the funding and efficiency gap
The NIB has committed to 3 design principles in delivery of PHC2020:
- to co-produce proposals with clinical, patient and civil society leaders
- to work in collaboration with local health and care organisations (CCGs)
- to champion Government Digital Service principles of digital design
Who are the members?
The NIB will achieve its aims through developing the necessary strategic consensus with partner health and care system Arm’s Length Bodies (ALBs), stakeholders and others through membership and involvement activity. It will engage public, citizen and patient ‘voice’ in its decisions and it will ensure professional input through its clinical reference structures.
Dame Fiona Caldicott, National Data Guardian
As the new National Data Guardian for health and care, Dame Fiona Caldicott, one of the most authoritative and informed independent voices on issues relating to the use and protection of patient data, will provide an oversight and challenge function to the use of personal health and care information held by organisations.
Dame Fiona will be able to scrutinise and challenge organisations across the health and care system without invitation or constraint. Her findings, and any subsequent advice, will be open and transparent. An independent voice, acting on behalf of citizens, she will play a vital part in building and sustaining public trust.
Partner Health and Care System ALBs and Stakeholders
- Department of Health (DH)
- NHS England
- Health and Social Care Information Centre (HSCIC)
- Public Health England (PHE)
- Human Tissue Authority (HTA)
- National Data Guardian (NDG)
- National Institute for Health and Care Excellence (NICE)
- NHS Blood and Transplant (NHS BT)
- Health Education England (HEE)
- NHS Trust Development Authority (TDA)
- Medicines and Healthcare products Regulatory Agency (MHRA)
- Monitor
- Association of Directors of Adult Social Services (ADASS)
- Healthwatch England
- Care Quality Commission (CQC)
- NHS Litigation Authority (NHS LA)
- Health Research Authority (HRA)
- Local Chief Information Officer Council
- Society of Information Technology Management (SOCITM)
- Local Government Association (LGA)
- Human Fertilisation and Embryology Authority (HFEA)
- NHS Business Services Authority (NHS BSA)
Independent Members
- Sam Smith: represents MedConfidential on NHS England’s Care.data Advisory Board
- Jo Bibby is responsible for the portfolio of work to improve quality at The Health Foundation
- Annie Whelan is the Development Lead for the Mental Health Providers Forum.
- Justin Whatling is the Population Health Management and Clinical Performance Improvement Lead for Cerner in Europe.
- Matthew Campbell-Hill is the Founding Director of Mentor’s DEN CIC.
- Alex Kafetz is the Strategy Director at ZPB
The Richmond Group of Charities
The Richmond Group of Charities is a coalition of 10 of the leading health and social care organisations in the voluntary sector. Collectively the board represents 15 million people, all working together as a collective voice to better influence health and social care policy.
- MacMillan
- British Heart Foundation
- Breakthrough Breast Cancer
- AgeUK
- Asthma UK
- Diabetes UK
- Rethink
- The Neurological Alliance
- Stroke Association
- British Lung Foundation
Strategic Clinical Reference Group
- Clare Marx, Chair of Strategic Clinical Reference Group, President of Royal College of Surgeons of England
- Martin Severs, Vice-Chair Strategic Clinical Reference Group, Interim Director of Information & Analytics and Lead Clinician (Caldicott Guardian)
The SCRG ensures, at a strategic level, that the policies, priorities, strategies, standards and guidance of the NIB support and synchronise with clinical priorities and continually improve quality of care and experience for patients and service users in England.
NIB Meetings
Working Group and Leadership Meetings
The Working Group meets 6 times per year and consists of functional lead directors from member organisations. The agendas for these meetings focus on developing specific subject areas and work themes across member organisations. Meetings will not normally be public sessions.
The Leadership Group meets 3 to 4 a year and includes Chief Executive Officers and lead director.
The agendas for these meetings are strategic and high level and focus on making important strategic decisions relevant to all or some member organisations; for example, formally agreeing the NIB Strategy or commissioning plans.
Phase 2: establishing the vision
23 October 2014: NHS Five Year Forward View published
The NHS Five Year Forward View sets out a vision for the future of the NHS. The Five Year Forward View starts the move towards a different NHS, recognising the challenges and outlining potential solutions to the big questions facing health and care services in England. It defines the framework for further detailed planning about how the NHS needs to evolve over the next 5 years.
13 November 2014 Personalised Health and Care 2020 published
Personalised Health and Care 2020 (PHC2020), which considers what progress the health and care system has already made and what can be learnt from other industries and the wider economy. PHC2020 is a framework for action that will support frontline staff, patients and citizens to take better advantage of the digital opportunity.
November 2014 NIB Implementation team established
The implementation team has 6 clear objectives:
- provide a centralised Programme Management Office function across all work streams supporting delivery of roadmaps and key deliverables
- work closely with NIB Secretariat Team supporting delivery of key events
- co-ordinate work stream plans and interdependencies and have oversight of work stream risks and issues
- act as a central Communication point across all Arm’s Length Bodies regarding the delivery of PHC2020
- ensure alignment of work stream outputs
- provide information and advice to the Transition Steering Group on progress against delivery.
Empowering patients and citizens
For many of us technology changes the way we do things. In other parts of our lives we see the benefits of using technology, such as booking travel and holidays, managing bank accounts, shopping and connecting with friends and family. These are often referred to as “digital services” e.g. websites on our laptops, apps on our phones.
Using technology to create digital health and care services will provide us with more convenient ways to interact with our doctors’ surgeries, pharmacies and hospitals. We will be able to communicate with our doctors at a time to suit us, be it via email, video link or online chat.
Using our laptops, smart phones or other mobile devices we will be able to get online and use these new digital services to:
- register with or change a GP, as well as book and change appointments at GP surgeries.
- order and pay for prescriptions: check information on medicines and receive reminders about when to take them
- book and change hospital appointments.
- claim refunds for medical treatment abroad
- report any side effects of medication
- sign up to take part in appropriate clinical trials
- access personal budgets with links to local care services to suit our individual needs
- spend personal budgets on appropriate care services, locally or nationally
- allow us to nominate a member of our family, close friend or carer to act on our behalf
We will all still need to see our doctors face to face and speak to surgeries and hospitals on the telephone. These ‘digital services’ are in addition to the existing ways in which we receive health and care services and are of course completely optional for us to use.
Many people are already benefitting from access to digital services in health and care, this work will ensure everyone has the opportunity to interact in the way they feel most appropriate.
Technology and data will also help to improve the quality of services available to us. Better information, or data, about how people use health and care services and how effective these are will help to improve the quality and efficiency of services available. This will also help to make sure we are getting the best value for money for the taxpayer from the investment made in health and care services.
There are a number of organisations and institutions that carry out research that aims to better understand what people need from the health and care service and how it can change or provide new services to ensure their needs are met. We will have access to information tailored to suit our needs, including greater transparency about the quality of services available, enabling us to exercise our right to choose which ones we use. Being able to give accurate information about how the health and care system is currently working will mean they can carry out this research and help the NHS provide the very best care.
Empowering health and social care professionals
For clinicians and care professionals, being able to offer a 21st century service to patients and clients means having access to all the appropriate information, from across health and social care services, at your fingertips.
Enabling you to make referrals, recommendations, diagnoses and prescribe with confidence that your decisions are based on up to date and accurate data, without having to repeatedly ask the same questions and knowing that you can share this with both the individual and other professionals involved in their care. PHC2020 looks to build a workforce who feel empowered through access to digital tools, information and training.
You will have the ability to set automatic alerts and notifications to aid decision support, and make use of tools and applications to monitor and communicate remotely. Additionally, patients and citizens will, through improved access to information and tools, be enabled to take a more active role in their care, allowing you to use consultation time to better effect, working collaboratively to achieve the best outcomes.
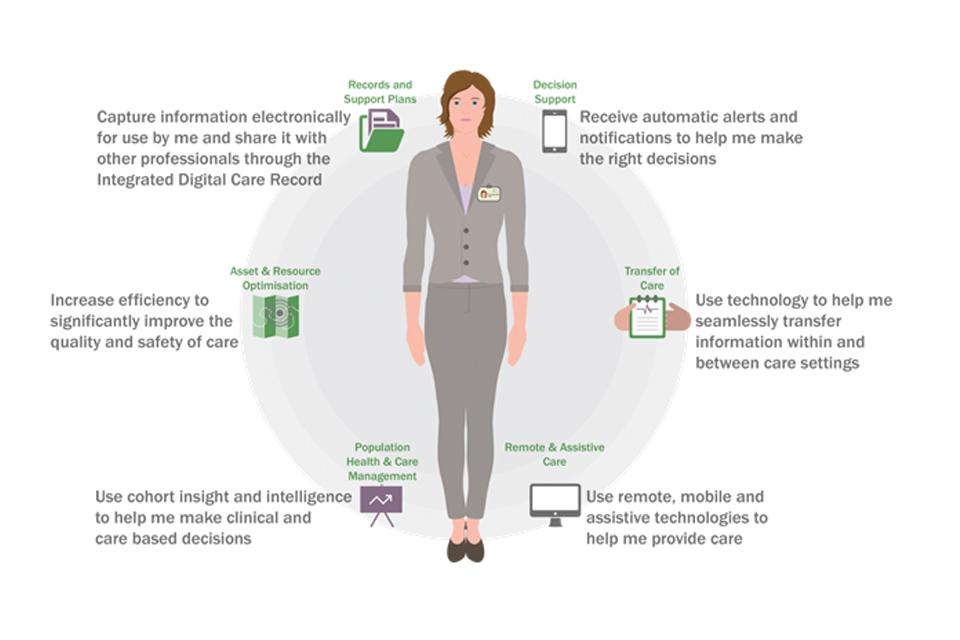
Empowering Health and Social Care Professionals
Empowering commissioners and local providers
Patients and citizens expect that whenever and wherever they access services, those caring for them can easily access comprehensive, accurate and timely information.
Patients and citizens anticipate professionals working with modern information systems that bring together all of the relevant information available – from diagnostic tests and clinical notes, case histories to records of personal preferences. Whether it’s patient frustration about not being remembered or professional concern about managing care in the face of unknown risks, patient experience and the effectiveness and safety of care will be improved through the creation of paper-free environments delivered at the point of care.
Collaboration
We will make use of sharing agreements and information standards to join up information across the health economy, enabling true collaboration between all those involved in the care of the patient or citizen, including the individual themselves. On a regular basis different organisations and sectors will collaborate on data, information and technology initiatives leading to better and more efficient health and care services.
Empowerment
Provision of training and support, combined with access to information and digital tools will empower individuals to take greater control of their health, alongside those who are charged with delivering health and care services.
Communication
Remote monitoring and communication systems enable care to take place at a time and place more convenient to the individual and can reduce unnecessary hospital stays. By communicating more effectively with patients and citizens about how and where their data is used, we can build greater trust in the appropriate sharing of data, enabling us to review our services, improve quality and optimise the use of resources.
To maximise our collective chances of achieving the 2020 ambition, and recognising the importance of implementing workflows and technologies that work for both the clinical and professional workforce within an organisation and for the broader workforce across the health economy, we require health economies to build on existing collaborative working in this area – or in some cases start working together now to embark on this journey.
The first step will be for health economies to produce a local digital roadmap to set out the steps for reaching a paper-free service at the point of care, based around 5 broad capabilities:
- assessments, records and care plans
- transfers, orders and communications
- decision support
- remote and assistive care
- asset and resource optimisation
In order to support this work we will be building a suite of co-designed products and tools to provide guidance and practical assistance throughout the journey, this will include, worked examples, workshops and later in the year publication of a digital maturity index to assist you to baseline progress against the 5 capabilities and benchmark this against other local areas.
Empowering innovators
The stated ambition of the Five Year Forward View is that the NHS will become one of the best places in the world to test innovations that require staff, technology and funding all to align in a health system, with universal coverage serving a large and diverse population.
It will drive new approaches to health and care that transcend traditional delivery boundaries, embrace new technologies and establish new partnerships across geographies and clinical and diagnostic specialisms. It will aid rapid implementation of the innovation pipeline from discovery to adoption and spread into clinical practice. It will transform diagnosis. We can create new collaborations between the NHS, technology companies and patients to unlock the potential of data, technology and digital to create products for smarter, faster and better healthcare and thereby grow the digital health sector, an emerging area of UK innovation.
The creation of an open infrastructure and a transparent framework of standards will be key enablers in encouraging research and innovation. However, more needs to be done.
Enhanced support for innovation will require a realignment of available investment funds, including future Technology Funds, the development of new investment flows, and the strengthening of partnerships with the research community, including the Academic Health Science Networks, Catapult centres and industry. We have an opportunity to combine different technologies and changed ways of working in order to transform care delivery through collaborative working.
Better data about the quality of care received by patients is essential to improving care outcomes. It is vital for effective commissioning and regulatory surveillance, and for the development of new medicines and treatments. Understanding trends and patterns in the costs – and effectiveness – of health and care is key to ensuring that the best value is achieved for taxpayers and the productivity of public resources is maximised.
As we move progressively towards real-time digital record-keeping, we will achieve the objective of collecting all the information required to support direct clinical care and the analytic needs of health and care, once and once only at the point of care. In the interim, it continues to be critical that we adopt a pragmatic step-by-step approach to unlock the rich insights available today.
For these reasons, this framework prioritises the safe development of linked administrative data for all NHS-funded episodes of care, including the care.data initiative; the development of data standards to support new costing, pricing and payment systems to incentivise innovative new models of care; and the improvement of the quality and coverage of clinical audit and disease registration. It is essential that citizens have confidence in all uses of their data and are able to make a decision about whether to share it. Detailed proposals on setting a new standard of NHS vigilance are contained in section eight of the framework PHC2020.
We also know from existing NHS research and the work of organisations like Patients Like Me that patient-reported outcomes data is vital to ensure accurate insight into care quality and to support innovation. For that reason, this framework proposes a series of experiments to develop the evidence base to support better use of patient experience and outcome data in health and care
Phase 2 – building the evidence and requirements
Developing the roadmaps to deliver the ambitions described in Personalised Health and Care 2020 has undoubtedly been a team effort, spanning organisational boundaries, sectors and disciplines. Bringing together representatives from right across the health and care system, including the Department of Health and all the Arm’s Length Bodies, members of the voluntary sector and independent members, notwithstanding the insightful contributions we have had from all those we have engaged throughout the journey, we simply could not have achieved any of this without your dedication, expertise and hard work.
A heartfelt thank you to you all!
- December 9 2014 – Leadership summit, attended by George Freeman – work streams established
- December 10 2014 – Inaugural Transition Steering Group Meeting – work stream chairs appointed
- January 10 2015 – work stream executive teams appointed
- January 20 2015 – Richmond Group of Charities joined the NIB
- February 12 2015 – Strategic Clinical Reference Group work stream representatives confirmed
- March 4 2015 – Leadership Summit at eHealth week
- March 9 2015 – work stream plans published
- June 17 2015 Leadership Summit – Sir Mark Walport joins the NIB
Work streams and work stream membership
Work stream 1.1: Providing patients and the public with digital access to the health and care information and transactions
| Role | Name |
|---|---|
| Chair | Simon Stevens – Chief Executive, NHS England |
| Chair | Jon Rouse – Director General, Social Care, Local Government & Care Partnerships, Department of Health |
| Executive team | Beverley Bryant – Director of Digital Technology, NHS England |
| Executive team | James Hawkins – Director of Programmes Delivery, HSCIC |
| Executive team | Charlotte Buckley – Deputy Director of Local Insight & Resilience, DH |
| SCRG representative | Mike Pringle – President, Royal College of GPs |
Work stream 1.2: Providing citizens with access to a set of NHS and social care apps
| Role | Name |
|---|---|
| Chair | Duncan Selbie – Chief Executive, Public Health England |
| Chair | Andrew Dillon – Chief Executive, NICE |
| Executive team | Diarmaid Crean – Deputy Director for Digital, PHE |
| Executive team | Alexia Tonnel – Director, Evidence Resources, NICE |
| SCRG representative | David Birnie – Ex-Dean of the Faculty of Health Informatics, Royal College of Surgeons of Edinburgh |
Work stream 2.1: Setting the commissioning and regulatory roadmap for implementing of digital data standards by 2018 to 2020
| Role | Name |
|---|---|
| Chair | Stephen Dunn – Chief Executive, West Suffolk NHS Foundation Trust |
| Chair | Rob Tinlin – Chief Executive & Town Clerk, Southend on Sea Borough Council |
| Executive team | Paul Rice – Head of Digital Technology, NHS England |
| Executive team | Mark Golledge – Programme Manager – Health & Care Informatics, LGA |
| SCRG representative | Lesley Anne Baxter – Vice Chair, AHP Federation |
| SCRG representative | Anne Cooper – Lead Nurse for Clinical Informatics, HSCIC |
| SCRG representative | Jonathan Kay – Ex-Director, Clinical Informatics, NHS England |
Work stream 2.2: Roadmap for comprehensive data on outcomes and value of service – ensuring the business intelligence requirements of health and care are met
| Role | Name |
|---|---|
| Chair | Simon Stevens – Chief Executive, NHS England |
| Chair | David Behan – Chief Executive, CQC |
| Executive team | Emma Rourke – Director of Intelligence, CQC |
| Executive team | Geraint Lewis – Chief Data Officer, NHS England |
| Executive team | John Varlow – Director of Information Analysis, HSCIC |
| Executive team | Peter Sinden – Chief Information Officer, Monitor |
| SCRG representative | Tony Newman-Sanders – Chief Clinical Information Officer, Croydon Health Services and Radiology Informatics Adviser, Royal College of Radiologists |
Work stream 3: Make the quality of care transparent
| Role | Name |
|---|---|
| Chair | Una O’Brien – Permanent Secretary, Department of Health |
| Executive team | Cameron Robson – Deputy Director, Information and Transparency Policy & Strategy, Department of Health |
| SCRG representative | Howard Duff – Director of England, Royal Pharmaceutical Society |
Work stream 4 Build and sustain public trust
| Role | Name |
|---|---|
| Chair | Una O’Brien – Permanent Secretary, Department of Health |
| Executive team | Cameron Robson – Deputy Director, Information and Transparency Policy & Strategy, Department of Health |
| SCRG representative | Martin Severs – Interim Director of Information & Analytics and Lead Clinician (Caldicott Guardian), HSCIC |
Work stream 5: Bring forward life-saving treatments and support innovation and growth
| Role | Name |
|---|---|
| Chair | Ian Hudson – Chief Executive, MHRA |
| Chair | Will Cavendish – Director General Innovation, Growth & Technology, Department of Health |
| Executive team | Nicole Mather – Director of Office for Life Sciences |
| Executive team | Catherine Page – Senior Policy Adviser, Office for Life Sciences |
| Executive team | Janet Valentine – Director, Clinical Practice Research Datalink, MHRA |
| Executive team | Rachael Williams – Research Statistician, MHRA |
| SCRG representative | Marina Lupari – Professional Lead for Primary Care & Community Nursing, Royal College of Nursing |
Work stream 6: Support care professionals to make the best use of data and technology
| Role | Name |
|---|---|
| Chair | Nicki Latham – Chief Operating Officer, Health Education England |
| Chair | Andy Williams – Chief Executive, HSCIC |
| Executive team | Rachael Allsop – Director of HR & Transformation, HSCIC |
| Executive team | James Freed – Chief Information Officer, Health Education England |
| SCRG representative | John Williams – Head of Informatics, Royal College of Physicians (of London) |
| SCRG representative | Anne Cooper – Lead Nurse for Clinical Informatics, HSCIC |
| SCRG representative | Oliver Warren – Consultant Colorectal & General Surgeon, Chelsea & Westminster Hospital NHS FT & Honorary Clinical Lecturer |
| SCRG representative | Jonathan Kay – Ex-Director, Clinical Informatics, NHS England |
Work stream 7: Assure best value for taxpayers and open up existing infrastructure
| Role | Name |
|---|---|
| Chair | Tim Donohoe – Director Informatics Delivery Management, Department of Health |
| Executive team | Tim Donohoe – Director Informatics Delivery Management, Department of Health |
| Executive team | Beverley Bryant – Director of Digital Technology, NHS England |
| Executive team | James Hawkins – Director of Programmes Delivery, HSCIC |
| SCRG representative | Alastair Henderson – Chief Executive, Academy of Medical Royal Colleges |
Work stream 8: Technical Platform and Information Standards
| Role | Name |
|---|---|
| Chair | Andy Williams – Chief Executive, HSCIC |
| Executive team | Peter Counter – Chief Technology Officer, HSCIC |
| SCRG representative | Jonathan Kay – Ex-Director, Clinical Informatics, NHS England |
Phase 4 – engagement and planning
Events
During July 2015 we held 4 events across England, aimed at bringing regional and local colleagues from across the health and social care together to share the work carried out by the NIB to date and to seek their views on the plans – particularly on 3 key roadmaps
“Providing patients and the public with digital access to the health and care information and transactions”
Setting the commissioning and regulatory roadmap for implementation of digital data standards
Build and sustain public trust
The first part of the day sought to bring everyone up to a shared level of understanding about the NIB, what has happened to date and what this means for our regional and local colleagues. Each event featured a case study from the area to encourage shared learning and promote good practice. The second part of the day gave delegates and work stream leads the opportunity to consider in greater detail some of the themes of the work which have significant impact at delivery level. There were 3 workshops on offer; delegates were given the opportunity to take part in 2 of these.
You said: we did
Throughout the regional events, we thoroughly enjoyed the opportunity to engage with regional and local colleagues, learning about the great work that is going on across England in line with many of the ambitions of PHC2020. It was also incredibly useful to hear about the challenges and feedback you had for us to take on board.
Work stream specific feedback has been shared with those groups and is reflected in the refining of the roadmaps and future plans, broadly these relate to communication and engagement:
You said:
Communicate clearly, use language which is meaningful to our stakeholders and articulate what the plans mean for them.
Our response:
In this document we have articulated the vision in terms of its impact for 3 stakeholder groups: patients & citizens; clinicians & care professionals, and; commissioner & local providers. We have tested these with representatives from these groups to ensure they are meaningful, however we recognise this doesn’t stop here, and we commit to keep this focus in future publications.
You said:
We need to engage more regularly and in more detail about our work. Events and workshops are the best forum for this to enable real dialogue.
Our response:
We hear you loud and clear! We are moving into the delivery phase for many of our programmes, and we cannot do this without your support. Over the coming months we will be developing wider engagement plans. In the meantime you can always contact us at: nibframework@dh.gsi.gov.uk
You said:
Need a single online resource to share templates, resources and guidance.
Our response:
You’ll notice there is a section in this report titled ‘Resources’, we will be using this section to showcase great examples from all the work going on across England and to share templates and tools relating to their success, wherever possible. This will be updated over the coming months.
Shaping the roadmaps
Since publication of the roadmaps in draft in June, work streams have taken the opportunity to work with key stakeholder groups to ratify direction, challenge, amend and refine the roadmaps.
Enable me to make the right health and care choices
Providing patients and the public with digital access to the health and care information and transactions: Feedback has been positive about the direction of travel described in providing patients and the public with digital access to the health and care information and transactions. These included many helpful suggestions about how to communicate with a wider audience and some suggestions about the things we need to put in place to ensure successful delivery. There is a clear need to communicate much wider using the right language and tools such as the egbot clip. It is very clear that we need to learn lessons from vanguard and pioneer sites and other projects which have gone before. Following this advice a schedule of meetings and events with third sector and patient and public representative groups is planned to refine the language and plans and other suggestions are being absorbed in delivery plans.
Providing citizens with access to a set of NHS and social care “apps”: Providing citizens with access to an assessed set of NHS and social care ‘apps’ has received growing support for plans to assess apps, however there are specific concerns around overall scalability and sustainability and ensuring that the assessment is proportionate to the risk. In response a series of work has been proposed to develop a taxonomy of apps, to investigate user needs and to review benefits for developers.
Give care professionals and carers access to all the data they need
Setting the commissioning and regulatory roadmap for implementing of digital data standards by 2018/2020: 4 focused working groups were established. In addition, 2 national engagement events were held to test assumptions around the proposed new secondary data landscape and direction of travel described in the roadmap for “Giving the right people access to the health and care data they need – developing a roadmap for comprehensive data on the quality, efficiency, and equity of health and care services for secondary uses”. The results of these engagement events have led to a refining and improvement of the roadmap particularly around the clarity of the vision, re-prioritisation of candidate areas for future work in the secondary data arena, and to direct the priorities of future phases of care.data. In addition, a series of SME sessions were held including the establishment of a rapid review group from some of the delegates to take forward specific feedback on emerging proposals.
Roadmap for comprehensive data on outcomes and value of service – ensuring the business intelligence requirements of health and care are met: 4 focused working groups were established. In addition, 2 national engagement events were held to test assumptions around the proposed new secondary data landscape and direction of travel described in the roadmap for “Giving the right people access to the health and care data they need – developing a roadmap for comprehensive data on the quality, efficiency, and equity of health and care services for secondary uses”. The results of these engagement events have led to a refining and improvement of the roadmap particularly around the clarity of the vision, re-prioritisation of candidate areas for future work in the secondary data arena, and to direct the priorities of future phases of care.data. In addition, a series of SME sessions were held including the establishment of a rapid review group from some of the delegates to take forward specific feedback on emerging proposals.
Make the quality of care transparent
This work is focused around the MyNHS site which regularly engages key stakeholders in the defining of metrics around the scorecards it publishes. Further details about this can be found in the Secretary of State challenge section.
Build and sustain public trust
Following publication of the roadmap, there were a number of outstanding questions; an exercise was undertaken to gather the answers through a series of workshops across 4 regional events. The feedback received at these events has provided valuable insights, now distilled into a set of key messages to inform future planning, in particular the review being led by Dame Fiona Caldicott and the CQC into cyber security and objections.
Bring forward life saving treatments and support innovation and growth
This work stream has linked closely with industry colleagues to shape the plans throughout the development of the roadmap. Plans are in place for the further engagement throughout the autumn, in time to inform the delivery of proposals including development of the industry strategy.
Support care professionals to make the best use of data and technology
A Stakeholder Advisory Group was established, to support development of the roadmap, with 2 ‘Challenge Sessions’ held to help facilitate positive challenge, bringing stakeholders together to consult. These Challenge Sessions were important focal points for this work stream; bringing together the specialists, stakeholders and critical friends to help identify workable solutions to objectives/commitments. Membership was from across the health and social care sector, as well as external and academic subject matter experts, and was intended to cover a range of ‘knowledge areas’ and workforce groups related to this work stream. 4 key themes have emerged: competency, leadership, professionalism and collaboration.
Filling in the gaps
Key to making sure our vision is one that is shared, will be continuing and developing the conversation with our stakeholders. Over the coming months we will be reaching out to some groups who we have not yet engaged in as much depth as others, these include:
- patients and citizens – we will be using NHS Citizen to trigger the conversation, the first step will be helping define meaningful success measures
- Industry – from the autumn we will be looking to work with industry partners to build on the conversations we have had so far, starting with TechUK
- the wider workforce across health and social care – following on from the feedback from the regional events, we recognise the importance of keeping the dialogue alive with colleagues from all parts of the health and care system. Many of those engaged so far have an existing interest in our work, we need to extend the conversation to others who are yet to hear about PHC2020, and whose views will be pivotal to its success. In addition we need to develop a conversation with some of the key influencers in this field, for example the Royal Colleges.
Phase 5 – planning for delivery
In order to deliver the ambitions of PHC2020, work is underway to establish a suite of programmes under the umbrella of the domains described in the diagram below. Once these programmes are up and running formal governance will be through the Department of Health’s Informatics Portfolio Management Board. We will develop a set of key performance indicators which will measure achievement of outputs or outcomes which are pivotal to delivery of the overarching vision.
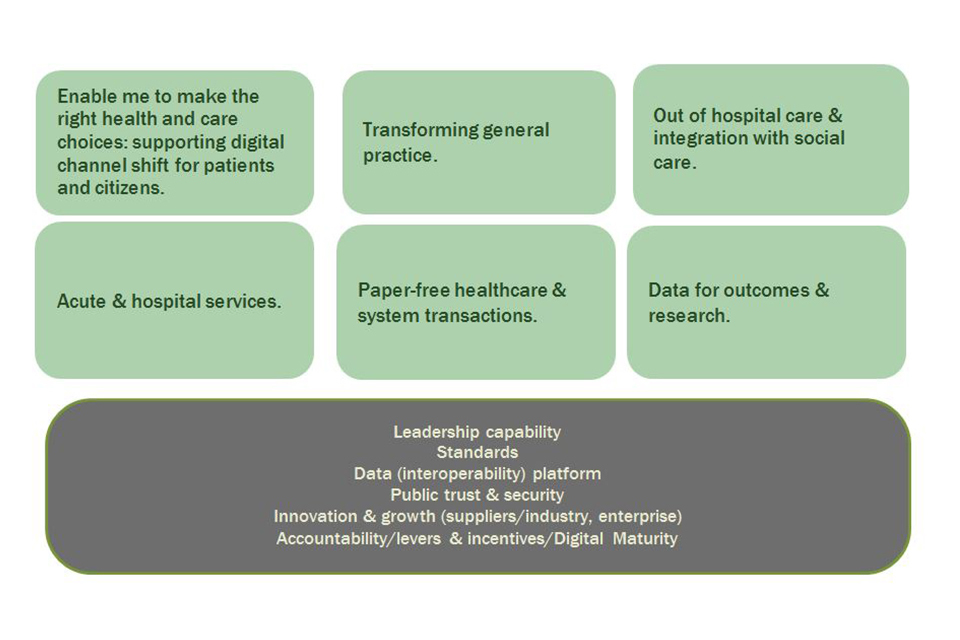
NIB plan final
Secretary of State’s Transparency Challenge
Truly world class performance only comes with a learning culture built around the natural desire that our doctors, nurses and managers have to do the best possible job for patients and the public. Through transparency the NHS is supporting transformation of the performance of entire hospitals, whether on safety, efficiency or quality; it is helping to improve the outcomes achieved by local authorities in public health and social care; and it is helping to tackle the variation in the care offered by residential care homes.
As part of that transition to a more transparent learning culture, last year we launched MyNHS – a world-first where patients and professionals alike can compare the performance of their local hospital, their local GP surgery, their care services and their local authority in an easy-to-understand format with regularly updated information.
This is the first time any major health economy has gathered such a wide range of key performance indicators together in a way that informs the public and helps professionals to improve care by reducing variation and levelling up. No targets, no sanctions – just information that helps health and care professionals and managers do what they are keen to do in any case: improve the safety and quality of care with which they look after NHS patients and their local population.
The key aim is to drive quality improvement through making comparative data publicly available in an easy to understand format.
The MyNHS site, which is part of NHS Choices, uses existing data to present measures which have been identified as of particular interest and is designed:
- to make information clear and accessible to the public, as well as for professionals and organisations
- to compare, in public, the quality and performance of NHS and care services, providers and commissioners including public health
- to support transparency and to stimulate improvements in quality, safety, and efficiency
- to improve public accountability
- to complement other public-facing and publicly available sites (e.g. NHS Choices, Dr Foster, National Cancer Intelligence Network etc).
Jeremy Hunt, Secretary of State for Health
MyNHS Current Site Usage
We currently collect data on a monthly basis covering the number of visits the sites receive and where they go when they get there.
The results for August 2015 are below:
- total number of site visits: more than 289,000 hits since Sept 2014
- total number of completed searches: nearly 272,500
- total number of data downloads: 6,608
- total number of data items from August 2015: more than 689,894
- most popular scorecards: consultants, hospitals
- most popular consultant scorecard: orthopaedics
Future research
Whilst usage data is helpful to gain a view of how many people are visiting the site and which pages draw the highest use, to truly test how successful this has been a piece of research is being commissioned to review the extent of the impact MyNHS has had on the outcomes and behaviours described in the Secretary of State’s Transparency Challenge.
Measuring success
It is important for the success, and credibility, of the NIB, that we routinely check how well we are achieving against our objectives with our stakeholders, including how meaningful the NIB proposals are.
The NIB was launched in March 2014, and since then a significant amount of work has been undertaken, with the framework (PHC2020) setting the strategy and the roadmaps describing the blueprint for delivery.
In order to objectively review progress, we have invited representatives of 3 major stakeholder groups to provide a critique of our progress to date and to recommend the success indicators we should be measuring going forward.
Patients and Citizens
We are working with the NHS Citizen team to launch a discussion about the role of the NIB and PHC2020 and what principles are most important to citizens. In addition the Richmond Group of Charities has a key role in providing advice and critique to the NIB on behalf of their constituents.
Health & Social Care Professionals
We have invited the National Quality Board (NQB) to work with us to define measures around the extent to which the changes proposed will improve quality of care. In addition the Strategic Clinical Reference Group has a key role in providing clinical advice and critique to the NIB.
Commissioners and Provider Organisations
Working closely with the implementing in Localities and Communities work stream we have identified 3 broad areas to measure:
- Effectiveness of Design and engagement
- Delivery/achievement – based around the Digital Maturity Index
- Outcomes – e.g. what differences have we actually made
Resources
Over the coming months we will be building the content in this section, including case studies, templates and tools. If you have any suggestions for things you would like to see here, please get in touch via nibsecretariat@dh.gsi.gov.uk.
