Pre-entry health assessment protocol for UK-bound individuals under various resettlement schemes (accessible)
Updated 27 March 2025
March 2025
Any enquiries regarding this publication should be sent to us at ukresettlementcasework@homeoffice.gov.uk
The following changes will take effect as of March 2025:
-
The Global Mental Health Assessment Tool - Primary Care Version (GMHAT/PC) will be used in a phased roll out across health assessment locations, and will replace the multiple assessments contained in the protocol
-
Introduction of Special Educational Needs and/or Disability Guidance
-
Scope extended to include pre-entry health assessments for individuals under various UK resettlement schemes
-
Urinalysis is no longer recommended as universal screening
-
Women and girls who are pregnant should undergo a risk assessment to ensure access to appropriate affordable care while waiting to be resettled to the UK
-
Screening for hepatitis B, hepatitis C, HIV and syphilis is now universally recommended for individuals who are covered by this protocol
-
Appendices referred to in this document are available at www.gov.uk/government/publications/pre-entry-health-assessments-guidance-for-uk-refugees
Executive Summary
This protocol describes the aim, objectives and scope of the pre-entry health assessment for individuals who are resettled to the UK. It is applicable to the UK Resettlement Scheme and the Afghan Resettlement Programme and may be applicable to similar ones which may be introduced in the future. The protocol is intended as a resource for International Organization for Migration (IOM) clinical staff, UK based accommodation providers and organisations supporting resettlement in the UK, and for UK health and social care providers.
The protocol has been developed drawing on four basic principles:
a) The health assessment is primarily for individual benefit. It aims to identify health conditions for which treatment is required prior to or on arrival to the UK, and those who may require special travel arrangements or early follow up in the UK. It also informs the accommodation needs of individuals when planning resettlement.
b) The protocol is based on UK standards of care, recognising that some elements of healthcare delivery and affordable access to healthcare while awaiting resettlement are context specific. IOM are not required to treat conditions but if needed should refer onto appropriate services or liaise with the Home Office to agree necessary treatment (including funding) where this is feasible.
c) It is acknowledged that there may be delays to travel for a variety of reasons, and where possible an individual’s health should not be put at excessive risk by a delay to travel for example due to a lack of appropriate accommodation. As above, IOM are requested to liaise with the Home Office where needed.
d) Individuals going through the health assessment are by definition part of a vulnerable population, with a high likelihood of traumatic experiences. The health assessment should be culturally sensitive, trauma-informed and should not add to an individual’s vulnerability.
| Section | Summary of content | Page number |
|---|---|---|
| Scope | For the purposes of this document, the term ‘individual’ includes those eligible for resettlement under the following UK resettlement schemes: the UK Resettlement Scheme and the Afghan Resettlement Programme and similar ones which may be introduced in the future. The UK Home Office directs which schemes this protocol applies to. |
7 |
| Consent, counselling, and approach | Individuals will be informed of the procedures of the health assessment; that examination findings will be shared with the necessary UK authorities; and will be asked to complete an informed consent form (Appendix 1). A hardcopy of the medical form will be given to the individual on their journey to the UK. As part of the consent process, individuals will be informed that they may refuse any element of the health protocol aside from screening for tuberculosis and completion of treatment as necessary. Any other elements that are refused should be clearly documented. Mandatory components may be subject to change depending on national and international circumstances. Individuals will be informed that health conditions are not a barrier to immigration, see below for specific conditions. Individuals should have a right to expect UK standards of confidentiality [footnote 1] around the health assessment. Outside of agreed health assessment information sharing, personal information shared in confidence should not be disclosed without legal authority or justification. Recognising the likely high prevalence of trauma for individuals, practitioners should take a trauma informed approach to assessment, as defined in UK practice [footnote 2]. If treatment is required for a condition this will be arranged locally, with support from UK authorities where required. |
9 |
| General assessment | Medical history (including pregnancy), physical examination and the radiology/ laboratory examinations are conducted by clinical staff and recorded on the medical form. | 12 |
| Specific conditions | Tuberculosis Process per the UK Tuberculosis Screening Technical Instructions. Active TB disease screening should be offered to all those who meet all of the following criteria: - They are coming to the UK for 6 months or more - They have lived in a country with an incidence of TB that is greater than 40/100,000 for more than 6 months - They were living in this country (or another country with incidence of 40/100,000) within the last 12 months (this time period is extended for resettlement cohorts from the standard 6 month period in the Technical Instructions – see section 3.1 for further detail) |
15 |
| Laboratory testing | Testing for Hepatitis B and C is recommended for all individuals. Testing for HIV and syphilis is recommended for all individuals Testing for helminthic infections should replace presumptive treatment if facilities are available and if it is epidemiologically justifiable. Testing for malaria should replace presumptive treatment if operationally feasible and epidemiologically justifiable. Testing may be offered for other conditions as per clinical judgement, including eGFR, blood count and liver function. |
22 |
| Immunisation | All individuals should be immunised according to the UK immunisation schedule. In practice not all immunisations may be available pre-entry, therefore as a minimum it is recommended that: - One dose of measles containing vaccine should be administered to all individuals older than 9 months. - All individuals coming from countries identified by the World Health Organization as exporting or with circulating wild or vaccine-derived Polio should receive at least one dose of inactivated poliovirus vaccine (IPV). - Hepatitis B vaccine should be given to family members and close contacts of identified cases. Vaccination history in the form of a vaccination card (Appendix 3) will travel with the individual along with other medical records. |
22 |
| Additional Clinical Assessments | Additional assessments, tests and evaluations can be requested in order to promote individual health and well-being, define healthcare needs post resettlement and outline travel requirements. These focus on chronic physical health conditions, mental health conditions including problem alcohol/drug use and psychosocial development, neurodevelopmental and special educational needs (SEN). |
23 |
| Medical escorts | Adequate medical escort(s) should be provided for all resettlement cases in need of special assistance during the air travel to the UK. For individuals needing a medical escort, a Significant Medical Conditions Form and an Activities of Daily Living report (where applicable) will be completed. | 25 |
| Documentation flow | Data should be captured electronically and all medical results/records should be communicated securely and regularly with the appropriate UK Authorities including the Home Office (for applicant management) through the existing platform providers. | 25 |
| Future revisions | This protocol will be reviewed on a regular basis, as deemed appropriate by stakeholders. |
Definitions and acronyms
AUDIT: Alcohol Use Disorders Identification Test
BASHH: British Association of Sexual Health
BBV: Blood borne virus
BCG: Bacillus Calmette–Guérin
BHIVA: British HIV Association
BIS: British Infection Society
CXR: Chest X-ray
DPA: Data Protection Act 2018
DUDIT: Drug Use Disorders Identification Test
eGFR: Estimated Glomerular Filtration Test
EIA: Equivalent enzyme immunoassay
ELISA: Enzyme-linked immunosorbent assay
EPTB: Extra-pulmonary TB
GMC: General Medical Council
GMHAT/PC: Global Mental Health Tool Primary Care version
GP: General Practitioner
HBV: Hepatitis B virus
HCV: Hepatitis C virus
HBsAg: HBV surface antigen
HIV: Human Immunodeficiency Virus
IOM: International Organization for Migration
Individual: Those eligible for resettlement under existing UK resettlement schemes: the UK Resettlement Scheme and the Afghan Citizens Resettlement Scheme and similar ones which may be introduced in the future
IPV: Inactivated poliovirus vaccine
LTBI: Latent Tuberculosis Infection
MMR: Measles, Mumps and Rubella
MOU: Memorandum of Understanding regarding the award of Grant Funding in support of pre-arrival outcomes for the United Kingdom’s Resettlement Schemes between the Secretary of State for the Home Office and the International Organization for Migration
OHID: Office for Health Improvement and Disparities
PA: postero-anterior
RDT: Rapid Diagnostic test
RPR: Rapid Plasma Reagin
RUDAS: Rowland Universal Dementia Assessment Scale
SEN: Special Educational Needs
TB: Tuberculosis
TP: Treponema pallidum
TPHA: Treponema pallidum haemagglutination assay
UKHSA: UK Health Security Agency
UNHCR: United Nations High Commissioner for Refugees
VDRL: Venereal Disease Research Laboratory test
WB: Western Blot
WHO: World Health Organization
1. Pre-entry health assessment
This protocol applies to those eligible for resettlement under the UK Resettlement Scheme and the Afghan Resettlement Programme. The schemes which are covered by this protocol may change, and its use is directed by the Home Office.
Following the health assessment, the individual’s information will be shared with the necessary institutions in the UK for appropriate follow-up, in accordance with the Data Protection Act 2018 [footnote 3] and applicable confidentiality regulations [footnote 1]. Information will be routinely shared with receiving accommodation providers and organisations supporting resettlement in the UK. Additional sharing of information with health, social care or other supporting organisations may be beneficial to the individual prior to arrival, and this should be through liaison with the Home Office.
Individuals will be given a paper copy of their health assessment. They should be advised to register with a General Practitioner (community doctor) on arrival in the UK, and to take this document with them.
This protocol was developed by a steering group based in the Home Office, the Office for Health Improvement and Disparities (OHID), the UK Health Security Agency (UKHSA) and IOM, with extensive expert and stakeholder consultation (Annex 1 outlines the contributors).
1.1 Aim and objectives of the assessment
Pre-entry health assessments aim to facilitate the early integration of individuals who are to be resettled in the UK. The objectives of the assessment are:
-
to identify health conditions for which treatment is recommended before the individual travels to the UK, primarily for personal benefit, but also:
-
to ensure the individual is resettled in a location and accommodation that has appropriate facilities to meet their health and social care needs
-
to identify and treat individuals with pulmonary tuberculosis (TB), ensuring current screening practice is met in all pre-entry assessments
-
to identify and address conditions and diseases with public health significance before travel;
-
-
to offer immunisation, wherever possible, for the benefit of the individual and of society;
-
to assess the individual’s fitness to travel to the UK and to both their transitional and permanent destination within the UK and to arrange special travel requirements (from a medical point of view) for the most vulnerable cases, when air travel might present additional risk to their health condition;
-
to identify and share medical information with the resettlement authorities in the UK, and those which are involved in supporting the process or providing accommodation, for the purpose of organizing adequate care and treatment upon arrival in the UK;
-
to identify and share medical information with UK health authorities – primarily through transfer of information to primary care at the point of registration with a GP.
1.2 General principles
All adults and children being considered for resettlement to the UK will be health assessed through IOM clinics in accordance with the Memorandum of Understanding (MOU) regarding the award of Grant Funding in support of pre-arrival outcomes for the United Kingdom’s Resettlement Schemes between the Secretary of State for the Home Office and the International Organization for Migration.
The assessment should be carried out using a trauma-informed approach [footnote 2], and individuals may request additional measures such as a friend, relative or chaperone present, or time to consider the assessment. Requests such as these should be accommodated where possible and appropriate.
Findings of the health assessment, lab test results, vaccines and administered treatment should be recorded in the medical form.
The clinician is not obligated to treat acute or chronic medical conditions detected in the health assessment. If any medical condition is detected or suspected, the clinician must inform the individual (or his/her parent(s) or legal guardian(s)) of this and of any associated healthcare needs and facilitate treatment, if needed.
Individuals may have medical conditions that pose a risk to themselves or others during travel, or which might worsen while awaiting resettlement. If clinicians are concerned that this is the case, they should raise this with the Home Office to consider arrangements for pre-travel treatment and stabilization, or in some cases, facilitate transfer to the UK for treatment. This will be done on a case-by-case basis and after consultation and approval from the Home Office. The need for consulting UK authorities will depend on access to healthcare prior to travel. The guiding principle is that people should have affordable access to an equivalent standard of healthcare as they would receive in the UK for conditions requiring urgent treatment prior to travel. The need for urgent treatment is subject to clinical judgement and should as a minimum be considered where there is a risk to life.
The individual should receive a hard copy of the medical form at the airport/point of departure, which they should carry with them to the UK. If the individual requests a copy of their medical form prior to departure, this should be offered.
The health assessment is intended to be a thorough and unbiased appraisal of the individual’s state of health pre-departure. However, due to the individual circumstances, the nature of some health conditions, and/or the sensitive nature of certain conditions, it cannot be assumed that all health or medical conditions of the individual will be identified through the health assessment.
1.3 Emergency resettlement
Whilst all adults and children being considered for resettlement to the UK should be health assessed pre-departure, there may be situations when this is not possible due to the urgency of the need to travel to the UK. In these circumstances the public health risk should be considered and advice sought from partner organisations including UKHSA, OHID and the appropriate public health bodies in the devolved administrations where relevant, regarding appropriate mitigations.
1.4 Consent and counselling
UK standards of consent will be used, meaning all parts of the assessment require consent that is voluntary and informed, and the individual must have capacity (see below for details around capacity)[footnote 4] [footnote 5]. Individuals with capacity have the right to withdraw their consent at any point. If consent is refused or withdrawn this should be noted on the medical form and Home Office should be notified.
The individual must give consent by completing an Informed Consent Form (Appendix 1), which can be paper-based or electronic, in a language that they understand (or with steps taken to ensure they understand) before the health assessment starts. The informed consent form will be written in both English and in the individual’s spoken language, which they will sign electronically or on paper.
For individuals who cannot read the consent form, or who have further questions, verbal explanation should be offered and an opportunity to discuss the assessment process, and any individual elements of it.
The clinician should keep the consent form and give a copy of it to the individual.
For immigration purposes, TB screening and completion of treatment (if this is required) are mandatory. If there are other elements of the health assessment which an individual does not consent to, this should be recorded. The mandatory elements of the health assessment are subject to change, depending on national and international developments.
Capacity
All individuals over the age of 18, or over the age of majority (in the instance that it is greater than 18 years in the country where the health examination is taking place), are presumed to be competent to give consent for themselves, unless the opposite is documented or suspected by a clinician. A person lacks capacity if they have an impairment or disturbance (permanent or temporary) that affects the way their mind works and that makes them unable to make or communicate a specific decision at the time it needs to be made [footnote 6].
Where the individual has not reached the age of majority or is deemed not to have capacity to understand and sign the consent form, the form must be signed by their parent or legal guardian, or accompanying adult, in accordance with regulations of the country where the assessment is taking place.
If an individual is mentally competent to give consent but is physically unable to sign the consent form, the clinician should complete the form as usual, and ask an independent witness to confirm that the individual has given consent orally or non-verbally.
Where the individual concerned is an unaccompanied minor, an accompanying adult (usually an UNHCR representative) will sign the consent form on behalf of the minor.
Freedom
Consent must be given voluntarily and freely, without pressure or undue influence being exerted on the individual. UK standards on supporting clinical decision making are available from the GMC. [footnote 7]
Individuals are entitled to withdraw their consent to the health assessment or use of their data, any parts thereof, at any time before or after signing the form. However, because the health assessment is a key part of the resettlement procedure, the Home Office has the right to determine what impact the withdrawing of consent for the assessment may have on the resettlement process.
Information and confidentiality
The consent form documents the agreement (or otherwise) of the individual to proceed with the health assessment in accordance with the UK protocol. The consent is only valid if the individual (or his/her parent/guardian or an independent witness) signs the form after sufficient explanation of the process.
An information sheet (Appendix 2), written in English and which summarises the important information about the health assessment, will be used by the clinician to aid the verbal explanation given to the individual.
The information provided to the individual should cover the entire health assessment process, its benefits and risks, the options or alternatives to the assessment proposed, and the consent process.
The clinician should further ensure that the individual understands and accepts that any relevant personal information collected during the assessment process, including health records and test results, may be shared with UK health and social care providers. The individual should be informed that, under the Data Protection Act (DPA) 2018 [footnote 3], the use of confidential patient information is restricted to activities directly concerned with or supportive of patient healthcare or the resettlement process on a “need-to-know” basis. In the case of pregnancy or a passenger’s complex medical needs patient information may also be shared with the airline carrier for the purpose of travel.
Individuals are likely to be in vulnerable circumstances, and clinicians should maintain the confidentiality of information disclosed during health assessments. The presence of interpreters or any others during the assessment should be mutually agreed with the individual, considering any vulnerabilities they may have. These people should also maintain the confidentiality of the individual’s information disclosed during the assessment.
The individual should be given the opportunity to ask questions and be given sufficient time to reflect on the answers given.
Counselling
Individuals should be offered counselling or pre-test discussion regarding the tests being undertaken, including TB, viral hepatitis, HIV, syphilis and pregnancy testing. Pre-test discussion can be offered at the same time as information about consent and can be done in groups if the individual agrees. The discussion should be trauma-informed and conducted with sensitivity to culture, language, gender and age, and provided by a health professional with experience in this area.
Pre-test discussion should clarify the nature of the tests and the actions required depending on the results, including after resettlement. It should be made clear that the purpose of this health assessment is not to identify conditions that lead to the exclusion from the UK or barriers for travel; on the contrary, it is focused on the promotion of individual health and well-being.
It should be clear to individuals that test results will not impact on their ability to resettle to the UK, but that some conditions may require or benefit from treatment before travel, travel arrangements may change, and in some cases their travel may be delayed pending further tests or treatment. In the UK, healthcare will be available free at the point of access to individuals, and their results will not impact on this entitlement.
Individual post-test discussion shall also be offered in the event of positive or inconclusive results. Post-test discussion should include informing the individual about the results of the test and referral of the individual to appropriate care. Apart from information sharing as agreed within the health assessment processes, and in accordance with UK standards for confidentiality [footnote 1], results must be kept confidential except where there is a legal obligation to share them with third parties or for the purpose of organising resettlement movements.
Additional Procedures
The clinician must retain the Informed Consent Form for at least three years (electronic copy is sufficient) and, upon request, make the form available to the necessary UK authorities or those they direct.
2. General Assessment
2.1 Medical history
- Before beginning the clinical assessment, the health professional (physician or nurse) who first sees the individual should ensure they have had the opportunity to clarify any questions about the health assessment in a personalised and confidential manner.
- Medical history should be taken by clinical staff (physician or nurse) following standard practices.
- Medical history should include current medication. This should include the generic name, dose, indication, start date and finish date (if appropriate).
- Individuals with chronic conditions should be advised to receive and carry four weeks’ supply of medication on their person from the point of embarkation to the UK.
- The examination should also address the mental health status of the examinee, (if available through the use of the Global Mental Health Assessment Tool/Primary Care GMHAT/PC) and seek to identify signs and symptoms of mental illnesses that are serious enough to warrant further specialised assessment, treatment, follow up, or interfere with individuals’ self-sufficiency (including ability to care for self, attend school or engage in other age-appropriate activities).
- Special attention may be needed for particular issues, such as history of torture, gender or sexuality-based violence, or physical, sexual or psychological abuse (this list is not exhaustive). The health assessment is not designed to detect these issues, but the clinician should be prepared to manage them appropriately in the context, including recording the need for follow up.
-
The detection of any disease of public health concern, in the medical history or throughout the health assessment, should prompt the clinician to follow local guidance on the notification of the local health authorities, where applicable.
- The assessment should also cover the neurodevelopmental and special educational needs of the individual as appropriate. This will help to identify those individuals with special educational needs at the earliest opportunity, assist in ensuring better placements with receiving authorities, and help to make sure appropriate support/schooling is in place upon their arrival in the UK.
2.2 Pregnancy
- For women and girls of reproductive age (15 to 49 years of age), record the date of their last menstrual period.
- A pregnancy test should be carried out on all women and girls between 15 and 49 years of age (the age range can be expanded if pregnancy is suspected), at both health assessment and pre-embarkation check or pre-departure medical screening (unless the woman is with confirmed/obvious pregnancy or menstruating). This should be carried out with full informed consent, with an understanding that pregnancy would not exclude an individual from resettlement.
- For pregnant women or girls, a risk assessment including local access to care for high-risk pregnancies and deliveries and risk of travel should be undertaken. This should be repeated as part of ongoing antenatal care and included in pre-departure medical screening as well. Guidance from Medecins Sans Frontieres should be used to identify high risk pregnancies and situations for specialist care during the antenatal period and delivery [footnote 8]. If a pregnancy requires higher level monitoring or special precautions for delivery, this should be ensured locally, or IOM should liaise with the Home Office around expediting travel if needed [footnote 9]. General recommendations on travel in pregnancy and on fitness to travel [footnote 10] [footnote 11] are also available.
- Clinicians should refer the pregnant woman or girl for routine antenatal care [footnote 12] https://www.nice.org.uk/guidance/ng201 which should include a general health assessment of both the woman and the foetus, with specific attention to nutrition and anaemia, and a risk assessment (as above). Where feasible, IOM doctors should access antenatal care records and/or discuss with antenatal care providers in order to assess risk. Where this is not feasible, IOM doctors should use their clinical judgement to determine risk.
- Date of last menstrual period, pregnancy test results and/or assessment of the woman and foetus should be registered in the medical form. Pregnant women and girls, regardless of the stage of pregnancy, should have a Significant Medical Conditions form (Appendix 4) filled out.
- The ‘must travel before’ date, typically set at 34 weeks and 6 days for pregnancies without complications, and the ‘expected delivery date’ should be indicated on the medical form for all pregnant women and girls.
- MMR is contraindicated in pregnant women and should not be offered. When MMR vaccine is given to adult women, they should be advised to guard against pregnancy for one month.
2.3 Physical examination
Physical examination should include:
- assessment of mobility and ability to perform daily tasks independently.
-
vital signs measurement, including:
-
respiratory and heart rates
-
blood pressure
-
head circumference for children below 2 years of age
-
body temperature
-
height and weight
-
visual acuity
-
hearing acuity
-
-
assessment of:
-
developmental milestones for children
-
nutritional status/indicators for children and pregnant women
-
musculoskeletal system, including mobility
-
neurological system, including reflexes
-
respiratory system
-
cardiovascular system
-
gastrointestinal tract
-
lymph nodes
-
oral and dental examination
-
skin examination
-
head and neck
-
- External genitalia and female breast examination should be done only if the clinician suspects the individual has a condition that requires assessment and/or treatment urgently before travel to the UK. It must be done following the UK’s standards for intimate examinations [footnote 13] and be culturally and gender sensitive. Individuals must be informed of the procedure, what to expect before the examination is carried out and must give permission for the examination. Where the individual has not reached the age of majority for the country concerned (where the health examination is taking place), or lacks the mental or other capacity to understand and give permission, permission must be sought from their parent or legal guardian or accompanying adult. The individual can withdraw their permission at any time during the examination. Whenever possible, the clinician should be of the same gender as the individual. The presence of a chaperone must be offered in all intimate examinations. The examination must be done in a proper environment, in which privacy is safeguarded and the dignity of the individual is ensured.
- Individuals with significant needs, such as a physical or sensory impairment, are twice as likely to report signs of psychological distress [footnote 14]. It is recommended that the clinician pay particular attention to the mental health of these individuals.
- Individuals with reduced mobility should have a completed Activities of Daily Living Form (Appendix 5) and Accommodation and Mobility Form (Appendix 6).
- Individuals with significant mobility problems requiring a wheelchair, stretcher or special accommodation must have the Significant Medical Conditions form filled out. Temporary arrangements and long-term accommodation needs should be set out clearly in the Accommodation Mobility Form.
2.4 Mental health assessment
-
The clinician should look for signs and symptoms of mental illnesses that are serious enough to warrant treatment and follow up, interfere with the applicant’s self-sufficiency, represent a risk of harm to the individual or to others, or represent a need for extensive social services.
-
Where available, assessment of mental health conditions will be carried out using the GMHAT/PC [footnote 15] to identify mental health needs of the individual. The outcome of the assessment will inform the receiving agencies to provide appropriate help and care. The GMHAT/PC assessment supports detection of all mental disorders including developmental problems (such as intellectual disability, autism spectrum disorder, attention deficit hyperactivity disorder and personality issues), substance misuse (drugs and/or alcohol), self-harm risk, trauma and abuse and cognitive impairment [footnote 16] [footnote 17]. A brief yet comprehensive assessment report inclusive of descriptive details will be transferred to the receiving UK health and social care agencies to support meeting the individual’s mental health care needs.
-
To the extent possible, clinicians need to make sure that refugees with mental health conditions receive appropriate counselling and connected to the available support programs prior to travel to the UK. IOM should liaise with the Home Office for any additional needs that cannot be addressed locally.
-
Where GMHAT/PC is not yet available, AUDIT and DUDIT [footnote 18] [footnote 19] should be used to assess for substance misuse issues, and the Rowland Universal Dementia Assessment Scale (RUDAS) to screen for cognitive impairment [footnote 20]. The use of these tools should be based on clinical judgement, or if the individual answers yes to any of the following questions:
-
Do you drink alcohol? (If yes, to complete AUDIT)
-
Do you use any drugs that are not prescribed? (If yes, to complete DUDIT)
-
Do you or your family and friends have any concerns about your memory? (If yes, to complete RUDAS)
-
Scores for AUDIT, DUDIT and RUDAS should be recorded on the Significant Conditions Form, and local pathways for investigation, and/or support followed as needed
-
See section 8: Additional Clinical Assessments for more detail on substance misuse assessment.
-
-
Training to use GMHAT/PC is advisable, and available for IOM providing pre-arrival services through liaison with Home Office authorities.
2.5 Child development and special educational needs (SEN) assessment
-
The clinician should assess the neurodevelopmental and special educational needs of the individual as appropriate, and the outcome recorded in the medical form to identify those individuals with special educational needs at the earliest opportunity. This will assist in ensuring better placements with receiving authorities and appropriate support/schooling is in place upon their arrival in the UK.
-
It is not feasible to complete a full assessment of child development and SEN during the health assessment. The aim is to screen for potential issues that would merit fuller assessment (and potential support) in the UK. For instance, it could be highlighted that children with potential developmental delay would benefit from the Ages and Stages Questionnaire assessment [footnote 21] on arrival.
2.6 Urinalysis
- Chronic kidney disease should be screened for using eGFR testing in all individuals aged 15 years or older. Universal screening with urinalysis is no longer recommended. It may be used based on symptoms or clinical judgement.
3. Infectious diseases
3.1 Tuberculosis
TB screening is outlined in detail in the UK TB Technical Instructions[footnote 22].
Active TB disease screening should be offered to resettlement cohorts who meet all of the following criteria:
-
They are coming to the UK for 6 months or more
-
They have lived in a country with an incidence of TB that is greater than 40/100,000 for more than 6 months
-
They were living in this country (or another country with incidence of 40/100,000) within the last 12 months (this time period is extended for resettlement cohorts from the standard 6 month period in the Technical Instructions due to additional risk factors identified for this population)[footnote 23].
The technical instructions should be referred to for the different screening processes for adults, pregnant women and children under 11 years old.
Anyone who presents with potential TB symptoms should be reviewed and clinically assessed with appropriate diagnostic testing regardless of TB incidence in country of residence.
Screening of individuals of age 11 years and older will include all of the following:
- a symptom screen (cough, haemoptysis, weight loss, night sweats)
- medical history taking, including any history of previous TB, any close contact with a case of active pulmonary TB (shared the same enclosed air space or household or other enclosed environment for a prolonged period for days or weeks)
-
a physical examination where clinically indicated
- a standard postero-anterior (PA) chest X-ray (CXR)
The process is the same for pregnant women except in relation to the CXR. A pregnant woman should be counselled on the small risk of radiation for the unborn baby, particularly in the first trimester, and be offered 3 options to choose from:
- postpone the CXR (and TB clearance) until after the delivery,
- undergo CXR examination using double shielding
- opt for TB clearance based on negative cultures from 3 appropriately taken sputum samples.
Screening of children under the age of 11 will include all of:
- a symptom screen (note the clinical expression of TB may be different in children than adults, and for children may only include generalised findings such as fever, night sweats, growth delay, and weight loss. Clinicians should be aware that children are more prone to extra-pulmonary TB (EPTB))
- medical history taking, including any history of history of previous TB, any close contact with a case of active pulmonary TB
- physical examination
Where a child has symptoms or signs of active pulmonary TB, or a history of previous TB, or a history of recent contact with a case of active pulmonary TB, then the child is required to have either a CXR or 3 sputum samples or gastric lavage (on 3 occasions) for laboratory mycobacterial examination (including culturing for mycobacteria).
The following points apply to TB screening:
- All X-rays must be interpreted by a qualified radiologist, and further reviewed by the clinician.
- Where the CXR is suggestive of either active or previous pulmonary TB, for individuals with signs or symptoms of pulmonary TB, or for pregnant women who do not wish to have a CXR, 3 early-morning sputum specimens on consecutive working days must be taken. These will be assessed for acid fast bacilli and cultured for Mycobacteria at a laboratory designated by the UK or its international partners for this purpose. Culture processing should be equivalent to the UK Standards for microbiology investigation of specimens for Mycobacterium species which requires culture on liquid and solid media.
- Individuals who have active pulmonary TB should be fully treated and certified clear of pulmonary TB before resettlement. There may be extenuating circumstances that require immediate travel. In these circumstances, the Home Office should be informed and direct medical advice should be sought from UKHSA.
- Suspected laryngeal TB should be investigated the same way as pulmonary TB. Further guidance can be found in the NICE guidelines. [footnote 24] The detection of EPTB is not a reason to delay resettlement, but the individual should be offered appropriate treatment at the earliest opportunity and follow up arrangements in the UK ensured.
- Only pre-entry screening for active TB needs be carried out. Latent TB testing is not required, given its non-infectious nature. Individuals may be eligible for community based latent TB infection (LTBI) screening following arrival in the UK. Further information can be found on LTBI testing and treatment here[footnote 25].
- There is no legal requirement to screen for EPTB given the diagnostic challenges. However, if EPTB is suspected or identified and healthcare services (diagnostics and/or treatment) are required on arrival to the UK, then the International Health Regulations National Focal Point team should be informed (via IHRNFP@ukhsa.gov.uk).
- Further guidance on TB among migrant populations, including screening for LTBI, can be found in the relevant section of the Migrant Health Guide [footnote 26].
3.2 Syphilis
- All individuals should be offered and recommended syphilis testing.
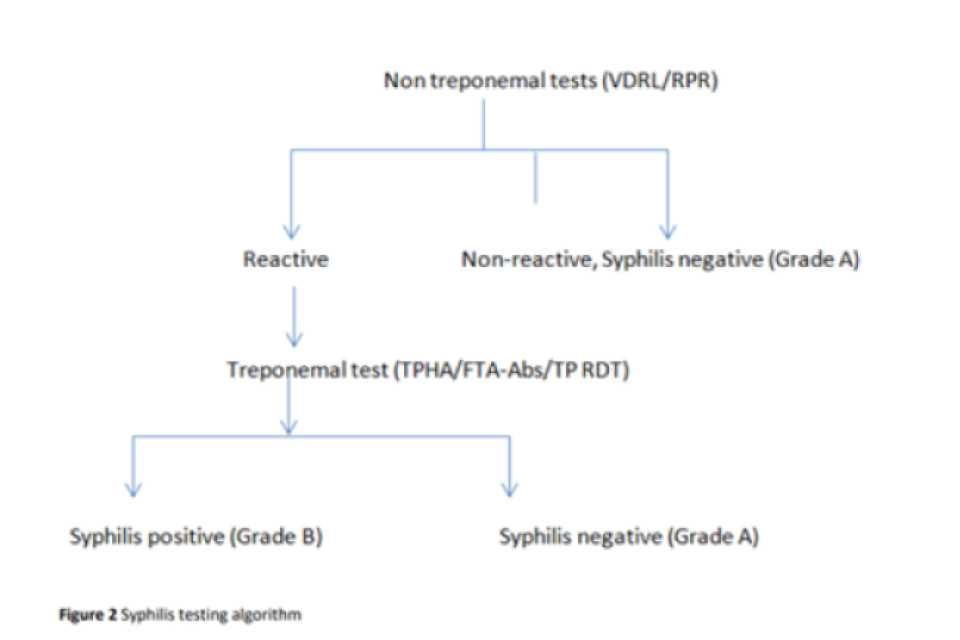
- The testing algorithm (Figure 1) includes the primary non-specific screening test (rapid plasma reagin [RPR], or Venereal Disease Research Laboratory [VDRL] test).
- If the initial screening test is negative, the test result is reported as negative.
- Positive screening tests should be confirmed with a treponemal (specific) test, such as the Treponema pallidum (TP) haemagglutination assay (TPHA), the Abbott Determine TP test (rapid test) or equivalent.
- If the confirmatory specific test is negative, the advice is to repeat the test in 2 weeks’ time to ensure this was not early syphilis.
-
If the confirmatory specific test is positive, the test result is reported as positive.
-
The recommended first line treatment for individuals in all stages of syphilis is penicillin G, administered parenterally. The preparation, dosage and length of treatment are determined according to clinical stage and manifestations of the disease.
-
The full recommendations, including dosages, are given in detail in the British Association of Sexual Health and HIV (BASHH) guidelines. [footnote 27]
- Confirmation of a syphilis diagnosis should prompt the clinician to consider screening for other sexually transmitted infections (STIs).
Figure 1 Syphilis testing algorithm
3.3 Human immunodeficiency virus (HIV)
-
All individuals should be offered and recommended HIV testing alongside other blood borne virus (BBV) testing. The clinician should ask whether they have previously been diagnosed with a BBV including HIV. This is a change from previous guidance to test based on country of origin and specific risk factors. The change has been put in place to simplify the testing process and to reduce the risk of stigmatisation.
-
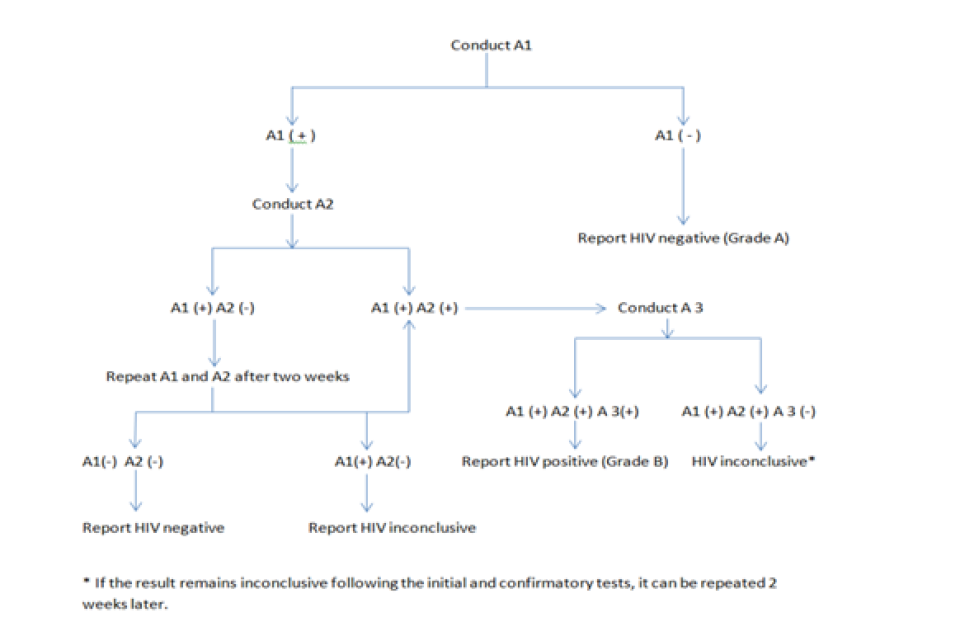
The primary first line assay (A1 in Figure 2) to be used is a fourth generation assay, such as the enzyme-linked immunosorbent assay (ELISA) test or equivalent enzyme immunoassay (EIA), which tests for HIV antibody and p24 antigen simultaneously. If it is negative, no further testing is required, and the sample is reported as negative. If positive or indeterminate, a secondary test (A2 in Figure 2) and a confirmatory test (A3 in Figure 2) should be performed, on the same sample.
-
The secondary test to be used is an ELISA or EIA test from a different brand or manufacturer.
-
The confirmatory test (third test; A3 in Figure 2) to be used is a western blot (WB), where and when available; or another ELISA test of different manufacturer, or a rapid test for HIV 1 and HIV 2 when WB testing is not available.
-
In case of non-availability of ELISA and WB, a set of three different WHO approved rapid tests for both HIV 1 and HIV 2 can be used, in accordance with the country of screening regulations and accepted HIV testing protocol.
-
Equivocal or indeterminate results should be re-tested after 2 weeks.
- Confirmation of an HIV diagnosis should prompt the clinician to consider screening for other sexually transmitted infections (STIs).
- People who are on antiretroviral therapy (ART) for HIV should have a 4-week supply of medication made available where possible at the point of travel to the UK.
- Testing recommendations are set out in the UK National Guidelines for HIV Testing 2020, from the British HIV Association (BHIVA), BASHH and the British Infection Society (BIS) [footnote 28].
Figure 2: HIV testing algorithm
3.4 Hepatitis B and C
-
All individuals offered and recommended testing for hepatitis B virus (HBV) and hepatitis C virus (HCV). This is a change from previous guidance to test based on country of origin and specific risk factors. The change has been put in place to simplify the testing process and to reduce the risk of stigmatisation.
-
HBV testing should start with HBV surface antigen (HBsAg) testing, with further HBV markers if HbsAg positive (usually, HbeAg, anti-HBe, anti-HBc & Hep B DNA). HCV testing should start with antibodies to HCV (anti-HCV), followed by HCV RNA if anti-HCV positive. Refer to the UK Standards for Microbiology for investigation of hepatitis B infection[footnote 29] for further information.
- Diagnosis of HBV or HCV in an individual should lead to testing of household and sexual contacts. For HBV, all close contacts including children should be offered vaccination.
- Direct-acting antivirals should be made available for people who are hepatitis C positive where available. A 4-week supply should be made available where possible at the point of travel to the UK.
- People with a chronic hepatitis B diagnosis should be linked into appropriate care once in the UK so that an assessment can be made about eligibility for treatment. Those already on treatment at the point of the health assessment should have sufficient medication available until the point that they are transferred and linked into care in the UK
3.5 Malaria
- Any febrile illness in an individual originally from or residing in a malaria endemic country should be investigated and malaria should be excluded at the pre-departure check stage, and managed as per the best clinical practice during the health assessment stage. A test and treat approach ideally with a blood film and malaria rapid diagnostic test (RDT) should be undertaken wherever operationally feasible. WHO recommends prompt parasite-based diagnosis by light microscopy or malaria RDT in all patients suspected of malaria before antimalarial treatment is administered [footnote 30]. Light microscopy entails visualisation of the malaria parasites in a thick or thin smear of the patient’s blood. The British Society for Haematology does not recommend the use of malaria RDTs alone [footnote 31].
- Presumptive antimalarial treatment is only indicated in settings where a test and treat approach is not possible or feasible, such as during malaria epidemics.
- Individuals coming from or travelling through malaria-endemic countries should be clearly informed that possible malaria is a medical emergency and that, if fever develops after arrival to the UK, they should seek immediate medical assistance and state where they have travelled from [footnote 32]. General information about malaria can be found in the malaria factsheet [footnote 33] and in the relevant section of the Migrant Health Guide [footnote 4].
3.6 Helminthic infections
Individuals who come from or reside in the Middle East, Africa, Asia, Latin America and the Caribbean should be offered the following tests during the pre-departure checks:
- stool test for ova, cysts and parasites
- serology for strongyloidiasis and schistosomiasis
-
Individuals should be treated based on their test results.
- Exceptionally, if testing is not available or is logistically impractical and depending on the epidemiological situation, presumptive treatment with albendazole is indicated during the pre-departure checks for individuals coming from the Middle East, Africa, Asia, Latin America and the Caribbean. Doses are as follows:
- a single dose of albendazole 400mg for all individuals except pregnant women and children under 2 years of age
- a single dose of albendazole 200mg for children aged 12 to 23 months
- Testing and treatment guidance for helminthic infections is available online from the UK Migrant Health Guide [footnote 34].
4. Immunisations
- Where possible, follow the UK immunisation algorithm [footnote 35] for vaccination of individuals with uncertain or incomplete immunisation status.
- In addition to the routine vaccine catch-up, Bacillus Calmette–Guérin (BCG) vaccine should be given at the earliest opportunity for those that meet the criteria as per Green Book recommendations and after active/latent TB has been excluded [footnote 36].
- One dose of measles containing vaccine, preferably MMR, should be administered to all departing individuals older than 9 months MMR is contraindicated in pregnant women and should not be offered. When MMR vaccine is given to adult women, they should be advised to guard against pregnancy for one month.
- All individuals arriving to the UK from the countries identified by the WHO as countries exporting wild polio or vaccine-derived polio virus or where wild polio virus is still circulating should receive at least one dose of IPV.
- Additional vaccinations or advice may be offered where there is an outbreak situation occurring in the country that an individual is based in.
- In some locations, certain vaccines may not be available or conditions may not be suitable for health assessment providers to organise a full immunisation schedule.
- Immunisations should ideally be administered more than 3 to 4 weeks prior to the scheduled departure to the UK, to allow for building immunity, while reducing virus-shedding post immunisation.
- Additional vaccinations against invasive meningococcal disease, varicella and rotavirus should be considered if the individual is living in overcrowded conditions.
- When indicated, close contacts of individuals with certain infectious diseases, such as hepatitis B, should also receive appropriate immunisation, in line with UK guidance [footnote 37].
- Vaccines may be contraindicated in specific groups, such as those with confirmed history of anaphylactic reaction to a vaccine component or previous dose, or those who are immunosuppressed or pregnant, in line with UK guidance[footnote 38]. Vaccination history in the form of a vaccination card (Appendix 3) should travel with the individual along with other medical records.
5. Laboratory testing
When required, testing must be done by laboratory services that meet internationally accepted laboratory standards, which include the following:
- individuals must be reliably identified prior to sample taking
- health staff shall reliably identify the individual and code the blood samples, before handing them over to the laboratory for testing
- use of quality assured supplies and equipment
- infection control and safety measures
- accurate, timely and confidential reporting of results
6. Additional clinical assessments
6.1 Chronic physical health conditions
Additional investigations or clinical assessment can be undertaken at the discretion of the clinician, in order to:
- diagnose or characterise medical conditions in need of treatment,
- diagnose or characterise medical conditions that might benefit from additional pre-departure planning to ensure any health and care or accommodation needs are met upon resettlement to the UK,
-
better characterise conditions that might impact travel to the UK, or benefit from earlier resettlement.
- For those individuals who have chronic conditions where there are possible complications (for example renal damage in a patient with diabetes, cardiovascular disease in a patient with arterial hypertension), further investigation and treatment should be offered either by the clinician or by referral to appropriate healthcare services.
- Individuals with limited mobility, visual or hearing impairment or with severe intellectual or physical disability should be assessed using the Activities of Daily Living Form. The Significant Medical Conditions form should also be completed for these individuals. The Accommodation Mobility Form should be completed, which will help to clarify whether temporary travel arrangements are required, and what long-term accommodation needs the individual has.
- Chronic medical conditions should be adequately described in the medical form, together with the findings of further specialist evaluation, additional tests and investigations. An assessment of future health needs should also be described.
6.2 Problem alcohol or drug use
- Problem alcohol or drug use can be defined as substance use that is associated with “a pathological pattern of behaviours related to the use of the substance” [footnote 39]. In this context, problem alcohol or drug use are of particular concern if they represent a risk to the individual, or a risk to others, most commonly in the form of physical violence. Any problem alcohol or drug use should be assessed in order to appropriately link to the UK health services upon resettlement. Assessment should follow local pathways, which may include referral to a psychiatrist for assessment before travel. The individual should be informed that this will not be a barrier to resettlement.
- Alongside assessment and onwards referral where needed, the clinician may take the opportunity to offer brief advice about potentially harmful behaviours, including for example reducing alcohol consumption, reducing or stopping drug use, and avoiding risky behaviour associated with substance misuse such as needle sharing.
- If the individual responds “yes” to the question “Do you drink alcohol?” in the initial health assessment then the AUDIT tool should be completed [footnote 18].
- If the individual responds “yes” to the question “Do you use any drugs that are not prescribed?” then the DUDIT tool should be completed [footnote 19].
- Both tools may also be used based on clinical suspicion of substance misuse.
- Scores should be included in the information transferred to UK authorities, and local pathways followed for offering follow up assessment and support.
- Neither AUDIT or DUDIT are required if GMHAT/PC is used.
- In the Significant Medical Conditions form, problem alcohol or drug use should also be characterised in terms of:
- substance(s) used, route(s) of administration and combinations of substances used together
- co-occurring mental health problems (for example post-traumatic stress disorder, depression)
- co-existing physical health conditions (for example epilepsy, pregnancy)
- risk of harm to self (for example risk of suicide or deliberate self-harm)
- risk of harm to others (for example risk of criminal activity, risk of harmful physical behaviour)
- health and social needs for the UK system (for example need for social care, rehabilitation treatment)
6.3 Psychosocial and neurodevelopment and special educational needs (SEN)
- All individuals with suspected cognitive impairment or dementia should be assessed against the Rowland Universal Dementia Assessment Scale (RUDAS, [footnote 20]). This is not required if GMHAT/PC is used.
-
All individuals with significant suspected or obvious developmental issues and/or requiring special schooling or employment needs should have the Significant Medical Conditions form filled out, highlighting the need for full assessment after resettlement. If there are associated medical issues or care needs, these should be investigated, treated or recorded in the Significant Medical Conditions form as appropriate prior to travel.
-
Assessment of special educational needs should be carried out using the SEN Guidance (Appendix 7) to identify learning difficulties and/or disabilities specifically relating to 4 broad categories of need:
-
communication and interaction
-
social emotional mental health
-
cognition and learning
-
physical and sensory disabilities
-
- The outcome of the SEN assessment should be included in the medical report. Details should be provided in the Remarks to the physical examination section. Medical Conditions Remark on the front page of the form should indicate “SEN: diagnosis (if available)”. The condition should be classified as Grade B, Others, and SMC form should be filled out.
7. Medical escorts
- IOM should identify, train and provide adequate medical escorts for all resettlement cases to the UK in need of special assistance during the travel to the UK.
- A Significant Medical Conditions form should be completed for those requiring medical escorts to travel to the UK.
- The medical escort should be selected based on their clinical skills and the specific condition and medical needs of the patient, taking into account the language, gender, age and cultural sensitivity and a trauma-informed approach.
- Medical escorts might be requested to accompany severely ill patients to a health facility in the UK.
- Medical escorts must hand over the patient to the receiving-end agency or a health professional at the most appropriate point decided by the pre-arrival service provider.
- Medical escorts should brief the receiving-end health professional of any event or change in the health condition of the escorted patient. Relevant medical documentation or files should also be shared with the receiving health practitioners in the UK, as appropriate.
8. Documentation flow
- IOM should provide the health assessments, Pre-Departure Medical Screening reports, including Pre-Embarkation Check report in accordance with the MOU.
- All medical records/results should be captured electronically. The health assessment findings should be communicated to the UK Authorities as soon as they are executed and completed through:
- a cumulative Excel spreadsheet containing the most important and relevant details of the individual health assessments, if requested by the Home Office,
- electronic copies of the duly completed health assessment forms through the best possible and secure means of electronic transmission, as agreed and requested by the Home Office. Such file transmission includes transmission of all relevant supplementary medical forms (such as the Significant Medical Conditions and Activities of Daily Living Forms) where indicated.
- IOM should be able to update the Home Office authorities of the progress and actions undertaken with regards to the cases/individuals that are placed on medical hold, those whose medical forms are pending and those where the health assessment is still not finalised (treatment, specialist review, determination of fitness to travel, etc.). If processes are likely to cause significant delay, seek advice from the Home Office authorities on submission of the health assessment.
- In accordance with the DPA 2018 [footnote 3], the use of confidential patient information should be restricted to activities directly concerned with or supportive of patient healthcare and resettlement or programme monitoring on a “need-to-know” basis. Therefore, individual health information will only be shared with the necessary UK authorities. The exceptions include sharing individual information with offshore health care providers if a refugee requires referrals for additional investigations or treatment, local health authorities in case of detection of a notifiable condition and airline carrier in the case of pregnancy or a passenger’s complex medical needs.
9. Future Revisions
This protocol will be reviewed on a regular basis to determine whether any significant changes need to be made. It may also be revised in response to major changes to UK medical or governmental guidance.
Annex 1 - Acknowledgements
The following members from the Home Office, UKHSA, OHID (DHSC), and the International Organization for Migration (IOM) led and supported the development of the revised instructions, with consultation and input from a number of UKHSA, DHSC and external experts. All input is not listed here, but our thanks to those involved, and to previous authors:
-
Dr Olga Gorbacheva, Senior Programme Coordinator, Health Assessment Programmes, IOM Geneva, Switzerland
-
Dr. Alex Klosovsky, Senior Migration Health Advisor, IOM Geneva, Switzerland
-
Dr Kathryn Hamilton, Public Health Registrar, Addiction and Inclusion Directorate, OHID, DHSC
-
Dr Ines Campos-Matos, Public Health Consultant and Deputy Director, OHID, DHSC
-
Dr Fatima Wurie, Migrant Health Evidence and Delivery Lead, OHID
-
Kate Yorke, Public Health Consultant, Inclusion Health, UKHSA
-
Bharat Sibal, Consultant in Communicable Disease Control, Border Health, UKHSA
-
Robert Sookoo, Head of Border Health, UKHSA
-
UKHSA experts in the TB Unit; Vaccine-Preventable Diseases and Immunisations; Blood Safety, Hepatitis, STIs and HIV Division; and Travel Health
-
Judith Harvie, Policy Manager- Quality, Patient Safety and Maternity, DHSC
-
Sarah Mo, Operational Lead, UNHCR Resettlement Schemes, Home Office
-
Gill Turner, National Lead Nurse for Children and Young People 0-19 Public Health, OHID, DHSC
-
Ruth Atkinson, Senior Policy Manager, Child Health, DHSC
-
Prof Vimal Sharma, Professor of Global Mental Health Research, University of Manchester and consultant psychiatrist, CANDDID, Cheshire and Wirral Partnership NHS Foundation TrustProf Mahesh Odiyoor, Consultant Psychiatrist, Psychiatry of Intellectual Disabilities; Strategic Clinical Director, ID/ NDD/ABI care-group and Centre for Autism, Neurodevelopmental disorders and Intellectual Disabilities (CANDDID); Clinical Lead and Deputy Chair, North-West LD and ASD Operational Delivery Network; Finance Officer/ Chair of the faculty A&T network, Royal College of Psychiatrists, Faculty of Intellectual Disabilities; Visiting Professor - University of Chester
-
Department of Health, “Confidentiality: NHS Code of Practice,” 2003. [Online]. Available: https://www.gov.uk/government/publications/confidentiality-nhs-code-of-practice ↩ ↩2 ↩3
-
Office for Health Improvement and Disparities. Working definition of trauma-informed practice. Guidance. 2022. Available: https://www.gov.uk/government/publications/working-definition-of-trauma-informed-practice/working-definition-of-trauma-informed-practice ↩ ↩2
-
Office for Health Improvement and Disparities. 2021. Migrant Health guide: countries A to Z. Available: https://www.gov.uk/government/collections/migrant-health-guide-countries-a-to-z ↩ ↩2
-
Department of Health, “Reference guide to consent for examination or treatment, 2nd ed.,” 2009. ↩
-
Office of the Public Guardian. 2020. Mental Capacity Act Code of Practice Available: https://www.gov.uk/government/publications/mental-capacity-act-code-of-practice ↩
-
General Medical Council. Decision making and consent. 2020. Available: gmc-guidance-for-doctors—decision-making-and-consent-english_pdf-84191055.pdf (gmc-uk.org) ↩
-
Medecins Sans Frontieres. Monitoring Complicated Pregnancies. Essential obstetric and newborn care. Available: https://medicalguidelines.msf.org/en/viewport/ONC/english/1-3-monitoring-complicated-pregnancies-51415999.html ↩
-
United Nations Population Fund. 2020. Implementation Manual for developing a National network of Maternity units. Available: https://www.unfpa.org/sites/default/files/pub-pdf/UNFPA_Implementation_Manual_for_EmONC_facility_network_Sept_2020_web.pdf ↩
-
Royal College of Obstetricians and Gynaecologists, “Air Travel and Pregnancy (Scientific Impact Paper No. 1),” 2013. [Online]. Available: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/sip1/ ↩
-
Civil Aviation Authority, “Assessing fitness to fly: Guidance for health professionals,” 2015. [Online]. Available: http://www.caa.co.uk/Passengers/Before-you-fly/Am-I-fit-to-fly/Guidance-for-health-professionals/Assessing-fitness-to-fly/ ↩
-
National Institute for Health Care Excellence (NICE), “Antenatal care for uncomplicated pregnancies: Clinical guidance,” 2019. [Online]. Available: https://www.nice.org.uk/guidance/cg62/chapter/1-Guidance#clinical-examination-of-pregnant-women ↩
-
General Medical Council, “Intimate examinations and chaperones,” 2013. [Online]. Available: http://www.gmc-uk.org/guidance/ethical_guidance/21168.asp. ↩
-
HelpAge International & Handicap International, “Hidden victims of the Syrian crisis: disabled, injured and older ,” 2014. Available: https://www.helpage.org/silo/files/hidden-victims-of-the-syrian-crisis-disabled-injured-and-older-refugees.pdf ↩
-
Sharma V.K, Lepping P, Cummins AGP, Copeland JRM, Parhee R, Mottram P. The Global Mental Health Assessment Tool- Primary Care Version (GMHAT/PC). Development, reliability and validity. World psychiatry (2004) 3(2) 115-19. Available: https://pubmed.ncbi.nlm.nih.gov/16633473/ ↩
-
Vimal K Sharma, Peter Lepping, Murali Krishna, Shazia Durrani, John R. M. Copeland, Patricia Mottram, Rashmi Parhee, Bennett Quinn, Steven Lane and Anthony Cummins. Mental health diagnosis by nurses using the Global Mental Health Assessment Tool: a validity and feasibility study. British Journal of General Practice, (2008) 58 (551), 411-416, Available: https://pubmed.ncbi.nlm.nih.gov/18505618/ ↩
-
Carrie Hough, Emily O’Neill, Florence Dyer, Katharine Beaney, Alison Crawshaw (Home Office and Public Health England) The Global Mental Health Assessment Tool (GMHAT) pilot evaluation: 2019, Research report 108 The Global Mental Health Assessment Tool (GMHAT) pilot evaluation: Final report (publishing.service.gov.uk) ↩
-
Alcohol Use Disorders Identification test. WHO. 1989. Available in multiple languages: www.auditscreen.org ↩ ↩2
-
Drug Use Disorders Identification Test. Available in multiple languages: https://www.emcdda.europa.eu/drugs-library/drug-use-disorders-identification-test-dudit_en ↩ ↩2
-
Dementia Australia, Rowland Universal Dementia Assessment Scale (RUDAS) Available: https://www.dementia.org.au/resources/rowland-universal-dementia-assessment-scale-rudas ↩ ↩2
-
Ages & Stages Questionnaires. Available: https://agesandstages.com/ ↩
-
UK Visas and Immigration; The Rt Hon Mark Harper, “UK tuberculosis technical instructions,” 2019. [Online]. Available: https://www.gov.uk/government/publications/uk-tuberculosis-technical-instructions. ↩
-
Tuberculosis prevention and care among refugees and other populations in humanitarian settings: an interagency field guide (who.int) ↩
-
NICE, Tuberculosis: Diagnosing Pulmonary Including Laryngeal TB In All Age Groups. 2019. Available: https://www.nice.org.uk/guidance/ng33/chapter/recommendations#diagnosing-pulmonary-including-laryngeal-tb-in-all-age-groups ↩
-
Public Health England, “Latent TB infection (LTBI): testing and treatment,” 2019. [Online]. Available: https://www.gov.uk/government/publications/latent-tb-infection-ltbi-testing-and-treatment ↩
-
Office for Health Improvement and Disparities, “Tuberculosis (TB):Migrant Health Guide,” 2023. [Online]. Available: https://www.gov.uk/guidance/tuberculosis-tb-migrant-health-guide ↩
-
British Association for Sexual Health and HIV: “BASHH Guidelines, Syphilis”. 2015 [Online]. Available: https://www.bashhguidelines.org/current-guidelines/genital-ulceration/syphilis-2015/ ↩
-
British HIV Association/BASHH/British Infection Association “BHIVA/BASHH/BIA Testing guidelines”. 2020. [Online] Available: BHIVA/BASHH/BIA Adult HIV Testing guidelines 2020 ↩
-
The Royal College of Pathologists UK Standards for Microbiology Investigations ↩
-
World Health Organization, “Malaria: Microscopy,” 2021. [Online]. Available: http://www.who.int/malaria/areas/diagnosis/microscopy/en/. ↩
-
British Society for Haematology, “Guidelines for the laboratory diagnosis of malaria”. 2022. [Online]. Available: Guidelines for the laboratory diagnosis of malaria (b-s-h.org.uk) ↩
-
UK Health Security Agency. 2023. “Malaria prevention guidelines for travellers from the UK”. [Online]. Available: https://www.gov.uk/government/publications/malaria-prevention-guidelines-for-travellers-from-the-uk. ↩
-
Public Health England, “Malaria factsheet: Guidance,” 2013. [Online]. Available: https://www.gov.uk/government/publications/malaria-prevention-transmission-symptoms/malaria-transmission-incubation-period-symptoms ↩
-
UK Health Security Agency. “Helminth infections: Migrant Health Guide”. 2021. [Online] Available: Helminth infections: migrant health guide - GOV.UK (www.gov.uk) ↩
-
UK Health Security Agency. “Vaccination of individuals with uncertain or incomplete immunisation status: Guidance,” 2023. [Online]. Available: https://www.gov.uk/government/publications/vaccination-of-individuals-with-uncertain-or-incomplete-immunisation-status. ↩
-
UK Health Security Agency. “Tuberculosis: the green book, chapter 32”. 2018. [Online]. Available: Tuberculosis: the green book, chapter 32 - GOV.UK (www.gov.uk) ↩
-
UK Health Security Agency. 2020, “Immunisation against infectious disease,” 2020. [Online]. Available: https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book ↩
-
UK Health Security Agency. 2017. “Contraindications and special considerations: the green book, chapter 6,” Immunisation against infectious disease, 2013. [Online]. Available: https://www.gov.uk/government/publications/contraindications-and-special-considerations-the-green-book-chapter-6 ↩
-
American Psychiatric Association, Diagnostic and statistical manual of mental disorders: DSM-5, 5th ed. Washington, D.C., 2013. ↩
