Productive healthy ageing and musculoskeletal (MSK) health
Published 6 December 2017
Summary
This resource for health professionals and local authorities makes the case for action to support healthy productive later life.
Longer healthier lives
There has been a steady increase in average life expectancy in recent decades, and there are now half a million people in their 90s in the UK according to the Office for National Statistics (ONS), more than two and a half times the number in 1985. By 2041 in the UK, the ONS estimates that there will be an 3.2 million people aged 85 years and older.
This is a public health success story. Longer lives are a benefit to society in many ways, including financially, socially and culturally, because older people have skills, knowledge and experience that benefit the wider population. There is an opportunity to utilise this increased longevity as a resource, whilst challenging ageism and the view that retirement is about ‘sitting more and moving less’.
However, the opportunities available to each of us as we age will be dependent on one important characteristic - our health.
As life expectancy rises, we must promote the concept of productive healthy ageing, which involves:
- improved health and wellbeing
- increased independence and resilience to adversity
- the ability to be financially secure through work and build resources
- engagement in social activities
- being socially connected with enhanced friendships and support
- enjoying life in good health
Longer, healthier lives can be a benefit to society, but this requires over-65s to be more active community and economic participants.

Infographic explaining productive healthy ageing
The World Health Organisation’s Global Healthy Ageing Strategy talks not of age, but rather ‘functional ability’, which is a combination of intrinsic ability (our physical and mental abilities) and environmental factors (transport, housing, relationships).
However, there are inequalities in people’s health experience as they age as highlighted in PHE’s Health profile for England.
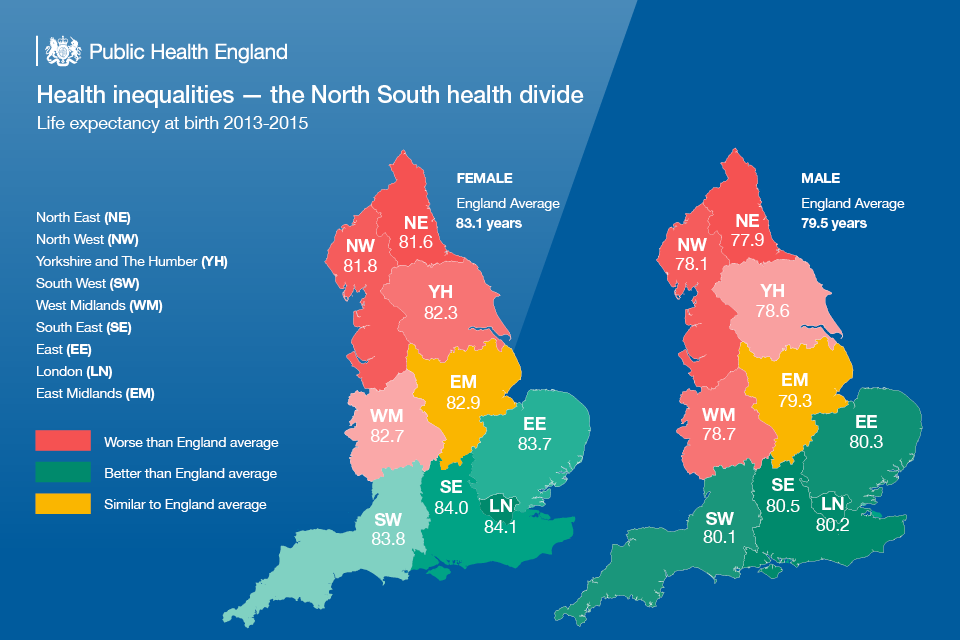
Infographic showing health inequalities in England
Whilst life expectancy has risen, people are living longer in poorer health, particularly those in more deprived parts of the country. The additional years in poor health are a consequence of the increase in life expectancy. The proportion of life spent in poor health has remained constant.
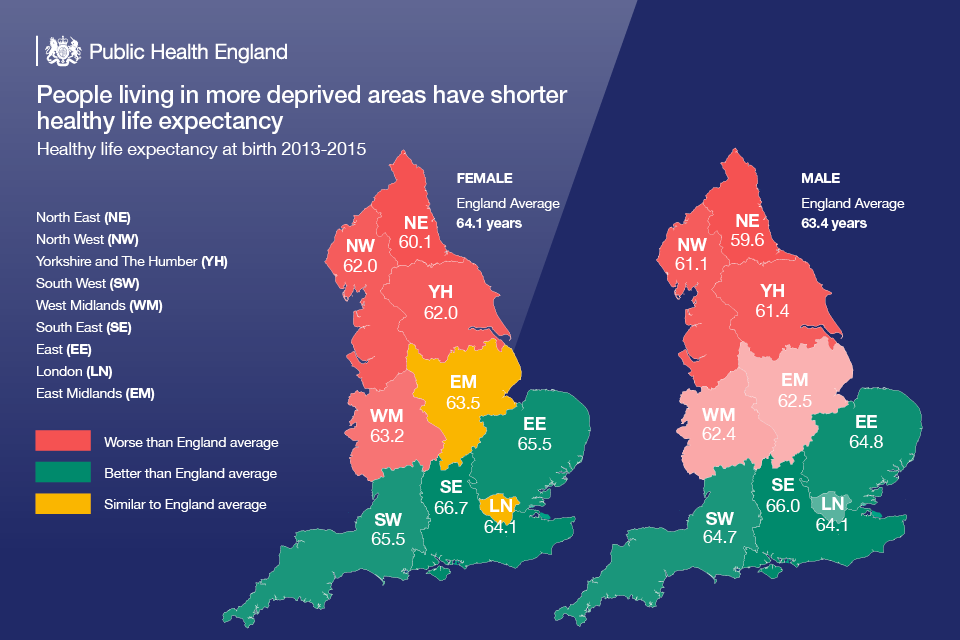
Infographic showing life expectancy in different parts of England
The older a person is, the more likely they are to experience chronic diseases and disabilities such as poor MSK health. This edition of Health matters focuses on the burden of MSK conditions.
MSK conditions are problems of the bones, joints, muscles and spine, and are a common cause of severe long term pain and physical disability. There are 3 groups of MSK conditions:
- inflammatory conditions, for example rheumatoid arthritis
- conditions of MSK pain, for example osteoarthritis, back pain
- osteoporosis and fragility fractures, for example fracture after fall from standing height
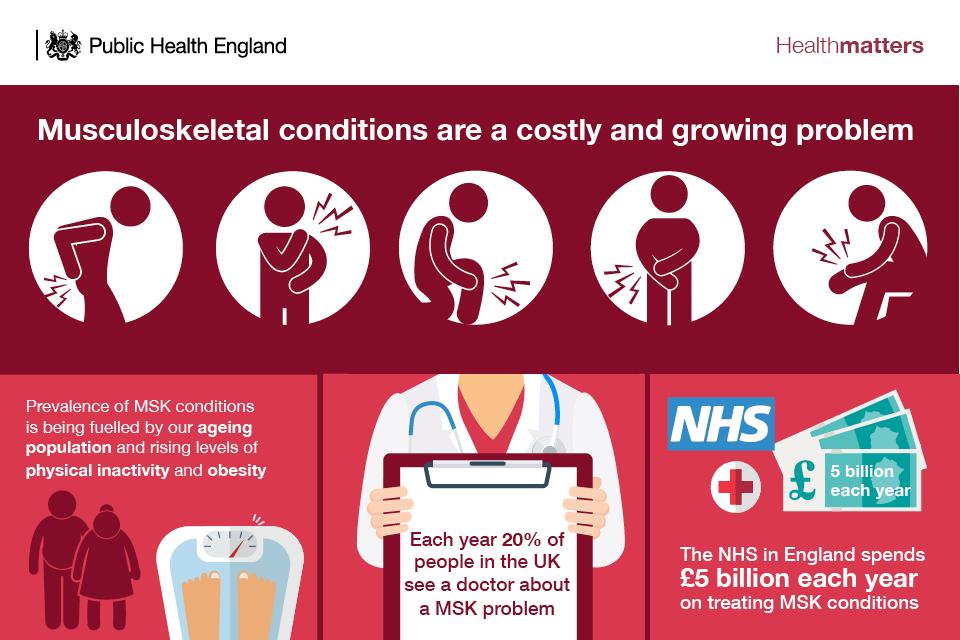
Infographic showing the prevalence and cost of MSK conditions
Lower back and neck pain were the leading causes of disability in England from 1990 to 2016. These conditions accounted for 2,221 years lived with disability (YLD) per 100,000 population.
Estimated levels of musculoskeletal conditions in England for 2012 also found that 18% and 11% of people aged 45 years and above have knee and hip osteoarthritis, respectively. An estimated 17% of all ages have back pain.
Fractures, which are often a consequence of falls, are one of the most serious MSK problems seen in the older population. An audit by the Royal College of Physicians found that fractures and falls in people aged 65 and over account for over 4 million hospital bed days each year in England.
There are multiple risk factors that can heighten people’s susceptibility to MSK problems, including age, being overweight or obese, lack of physical activity, and poor health habits such as smoking.
Two risk factors that often coincide are increasing age and reduced physical activity. As people age, they take part in less physical activity - in the 19 to 24 year age group 76.6% of people are physically active compared to 24.7% in individuals aged over 85 years.
Impact of MSK conditions on employment
The pain and disability of poor MSK health limits independence and the ability to participate in family, social and working life. According to Arthritis Research UK only 59.4% of people of working age with an MSK condition are in work, and around 1 in 5 people with arthritis has depression.
In 2016, MSK problems were the second most common cause of sickness absence, which accounted for 30.8 million days lost in work (22.4% of total sickness absence). This was only slightly surpassed by absence due to minor illness such as cough and colds, which accounted for 34 million days lost (28.8% of total sickness absence).
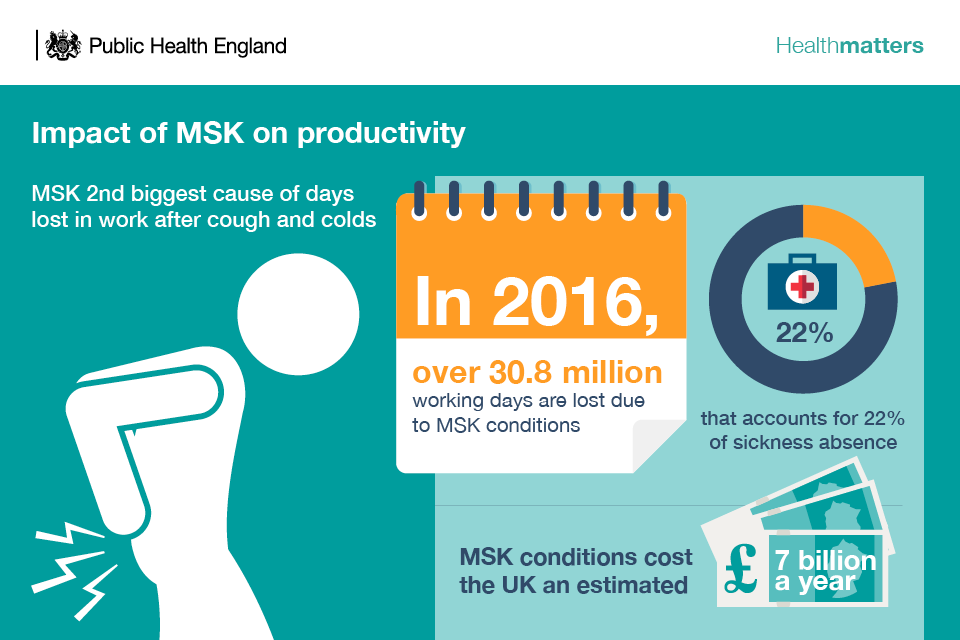
Infographic showing impact of MSK on productivity
Why invest in prevention of MSK conditions
As well as being a big problem for individuals and employers, MSK conditions place a considerable strain on the NHS. They account for the third largest area of NHS spending with a programme budget of £4.7 billion in 2013 to 2014.
With tighter budgets across the NHS and local government, it’s more important than ever before to make the strongest possible economic case for interventions, and being able to calculate the return on investment (ROI) means decision makers can opt for the most cost-effective ways to improve and protect health.
The evidence for providing cost-effective interventions for preventing and treating MSK conditions is overwhelming. To help commissioners to do this, PHE has launched an MSK ROI tool, produced by the York Health Economics Consortium, which tailors results to local areas, outlining what they can do to take action.
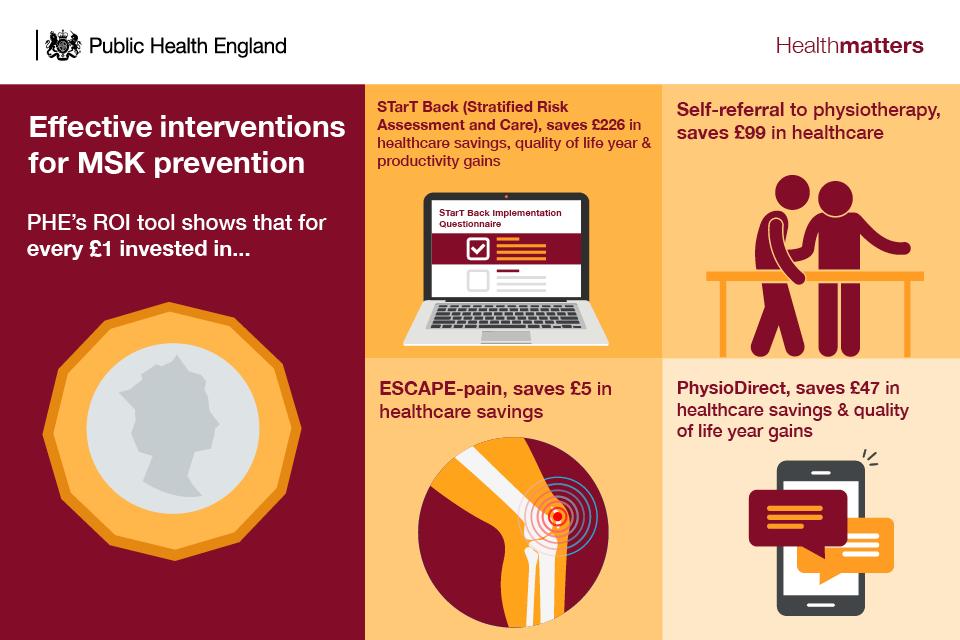
Infographic showing effective interventions for MSK prevention
Read the case study: ESCAPE-pain for knee pain.
Read the case study: implementing stratified care for low back pain: the STarT Back approach.
Interventions to prevent the onset of MSK
Living for longer does not mean a lifetime of pain and ill-health. There are steps that we can take throughout our lives to maintain healthy productive lives, reduce the risk of developing MSK conditions and better manage our health.
Health professionals and commissioners should encourage patients to make healthy behaviour changes to lower the risk of developing MSK conditions and prevent falls.
Read the case study: Better Bones Osteoporosis Service from Kingston Public Health.
Physical activity
There is typically a common decline in physical activity, and the benefits that are gained from it, with age.
Adults in England should aim to take part in at least 150 minutes of moderate intensity physical activity each week, in bouts of 10 minutes or more, according to physical activity guidelines for adults from the UK Chief Medical Officers (CMOs).

Infographic showing recommended physical activity levels
Moderate intensity physical activities, such as brisk walking or cycling, cause adults to get warmer and breathe harder and their hearts to beat faster, but they can still carry on a conversation.
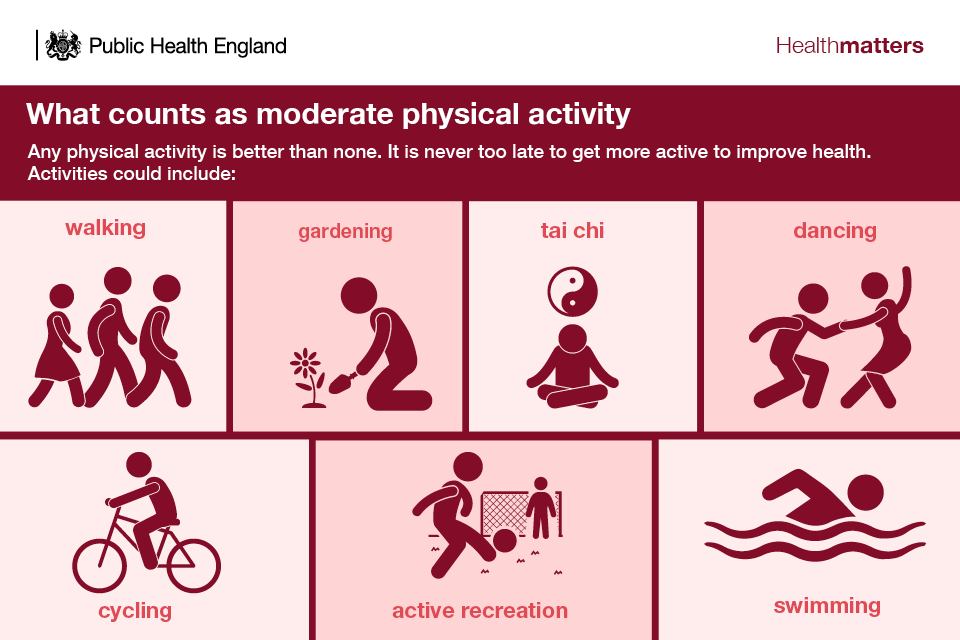
Infographic showing examples of moderate physical activity
All adults should aim to be active daily and should include undertaking physical activity to improve muscle strength on at least 2 days a week, such as exercising with weights, yoga or carrying heavy shopping. This can help lower the risk of sarcopenia, or loss of muscle mass, which is associated with ageing but can occur in response to immobility at any age. Older adults at risk of falls should also incorporate physical activity to improve balance and co-ordination on at least 2 days a week.
Older people are recommended to carry out exercises to improve balance twice a week. This can include:
- dancing
- tai chi
- bowls
Read the case study: Dancing in Time.
However, people in the UK are around 20% less active now than in the 1960s. If current trends continue, we will be 35% less active by 2030.
Figures from the Health Survey for England 2012 show that 61 of people in England were classed as physically active (the proportion of respondents aged over 16 years doing at least 150 moderate intensity minutes physical activity per week).
Males were significantly more physically active than females - 67% compared to 55%
Both males and females in the highest household income quintile were significantly more likely to be physically active than the lowest household income quintile - 76% compared to 55% for men and 63% compared to 47% for women.
As well as being physically active, all adults are advised to minimise the time spent being sedentary (sitting) for extended periods. Even among individuals who are active at the recommended levels, spending large amounts of time being sedentary may increase the risk of some health outcomes, including early death, type 2 diabetes and some types of cancer. Sedentary behaviours are impacted by age, gender, socio-economic conditions, occupation, weight status and some characteristics of the physical environment.
Read the case study: Improving primary prevention of falls for Newcastle’s over 65s.
Many adults spend in excess of 7 hours per day being sedentary, and this typically increases with age. Regular physical activity in line with the CMO recommendations and exercise at every stage of life can reduce the risk of many MSK conditions. The National Institute for Health and Care Excellence (NICE) has a number of clinical pathways that highlight the role of physical activity in preventing and managing illness including MSK conditions.
PHE and the National Centre for Sport and Exercise Medicine have developed an e-learning module to provide information about the benefits of physical activity for older adults and in particular those who are beginning to experience a decline in their physical function, referred to as those who are ‘in transition’.
Physical activity can also benefit those who already have MSK conditions. However, many people with MSK conditions often mistakenly believe that physical activity will make their condition worse. The more conditions you have the more you need to improve the core aspects of fitness:
- strength
- stamina
- balance
Maintain a healthy weight and balanced diet
Supporting people to maintain a healthy weight along with advocating the CMOs’ recommendations for physical activity from an earlier age can reduce the risks of developing MSK conditions such as back pain and osteoarthritis of the knee.
In 2015, 58% of women and 68% of men were overweight or obese according to NHS Digital statistics. Obesity prevalence has increased from 15% in 1993 to 27% in 2015.
Obesity prevalence varies with age for both males and females, with the highest levels in the 55 to 64 age group.
Obesity is a strong risk factor for the development of osteoarthritis of the knee. A meta-analysis of observational studies published in 2011 estimated that people with a healthy weight (a body mass index below 25) are less likely to develop osteoarthritis of the knee than those who are obese.
A healthy balanced diet is also important for good bone health, to prevent osteoporosis in later life. According to the Scientific Advisory Committee on Nutrition (SACN) this should include vitamin D and calcium, which are both important dietary components for MSK health through maintaining healthy bones, teeth and muscles.
PHE advises that in spring and summer, the majority of the population get enough vitamin D through sunlight on the skin and a healthy, balanced diet. During autumn and winter everyone will need to rely on dietary sources of vitamin D. Since it is difficult for people to meet the 10 microgram recommendation from consuming foods naturally containing or fortified with vitamin D, people are advised to consider taking a daily supplement containing 10 micrograms of vitamin D in autumn and winter.
People whose skin has little or no exposure to the sun, like those in institutions such as care homes, or who always cover their skin when outside, risk vitamin D deficiency and need to take a supplement throughout the year. Ethnic minority groups with dark skin, from African, Afro-Caribbean and South Asian backgrounds, may not get enough vitamin D from sunlight in the summer and therefore should consider taking a supplement all year round.
Calcium is needed for good bone health. Eating a diet consistent with the Eatwell Guide will provide all the calcium your body needs.
Stop smoking
A PHE commissioned review has shown that smoking plays a role in the progressive decline of the body’s major systems, including MSK, respiratory and cardiovascular systems, cognitive function, oral health and vision.
Smoking has a negative impact on bone mineral density, with evidence of damage apparent from as early as the late teens that increases with age.
Much of the MSK harm and risk caused by smoking arises from smoking in middle years. However, it can be prevented by cessation as a young adult or partially reversed by quitting in later years.
The review showed that smoking is associated with various MSK conditions. Smokers and ex-smokers experience 60% more pain in the back, neck and legs and a 114% increase in disabling lower back pain.
Smoking:
- appears to be associated with poorer development of the hip, spine and neck, and lower bone mineral density among men as young as 18 to 20
- has a particularly greater impact on reduced bone mineral density among postmenopausal women
- is associated with more bone fractures and slower healing and is associated with up to a 40% increase in the risk of hip fractures among men
- is a significant cause of rheumatoid arthritis, especially among men, and can also reduce the impact of treatment
Meaning and purpose as we age
Workplace Health
The UK workforce is ageing, working for longer and retiring later. From 2004 to 2010, the average age men and women left work rose by a year to 64.6 for men and 62.3 for women, according to the CMO’s annual report of 2015.
The last 20 years (to the end of 2014) have seen a gradual increase to 75.3% in the proportion of people aged 50 to 64 years working or looking for work.
1 in 5 workers do not expect to retire until they are over 70, according to research by the Department for Work and Pensions.
Read the case study: SWAP: delivering primary care vocational advice.
For most people being in ‘good work’ - having a secure job with good working conditions - is good for personal health, organisational productivity and economic prosperity. Having a job can also contribute significantly to boosting self-esteem.
It is important to ensure that employers and employees recognise the critical role the workplace can play in promoting health and wellbeing. There is also a lot that can be done in the workplace to reduce any threats to MSK health, including adapting physical environments and work practices, as well as early interventions to identify and address problems.
Read the case study: Supporting musculoskeletal (MSK) health at work.
Of the 7.2 million people aged 50 to 64 who are employed, 42% report that they are living with at least one health condition or disability.
The most prevalent health conditions affecting people aged 50 to 64 are:
- MSK conditions (21%)
- cardiovascular conditions (17%)
- depression and anxiety (8%)
PHE, with partners, has produced a MSK Employers toolkit to encourage employers to be proactive, creating a healthy working environment where employees feel they can approach managers if they feel stressed or are experiencing pain and discomfort as a result of a mental health or MSK condition.
Being socially connected
As well as being in work, activities such as volunteering, pursuing hobbies, travelling, or taking up learning opportunities can provide meaning and purpose and help to keep people healthy in later life.
Keeping active and challenged throughout life can help to reduce the risk of MSK conditions as well as:
- lowering the risk of dementia
- improving your mood
- relieving stress
- reducing the risk of depression
- reducing loneliness
PHE has developed a guide to community-centred approaches that outlines evidence-based community-centred approaches to health and wellbeing.
Mental wellbeing
Mental health conditions can increase the likelihood of developing some MSK disorders. For example, people with depression are at greater risk of developing back pain. Here lies a vicious cycle, as MSK conditions can also have a significant impact on mental health. Living with a painful condition can lead to anxiety and depression, and depression is 4 times more common among people in persistent pain compared with those without pain.
PHE has developed a mental health toolkit for employers that can help every organisation support the mental health and wellbeing of its employees. It will help employers take positive actions to build a culture that champions good mental health and provides a greater understanding of how to help those who need more support.
Call to action

Infographic showing call to action to stakeholder groups on productive healthy ageing
Local government
Support discussions between the wider public health workforce which may include planning teams, housing officers, transport officers and health and safety executives to promote a healthier ageing environment through the use of leisure centres, parks, well designed built environments and social care activities.
By working together, local service planners and commissioners need to ensure that they have pooled information to ensure effective service planning for people who suffer from MSK conditions.
Engage with local businesses to investigate the potential to develop local workplace health standards.
Promote the use of tools and resources to support employers such as the MSK Employers Toolkit and the Mental Health Employers Toolkit.
Facilitate access to local physical activity provision for those with an MSK condition.
Use metrics and tools to measure and monitor pain and its impact on people’s functional ability to manage and undertake daily tasks.
Commissioners
Commission relevant training to improve the skills and competencies of the current and future workforce.
Service specifications need to consider relevant behavioural risk factors that impact on MSK health for improved health outcomes such as developing local workplace health standards.
Commission evidence based interventions for people with specific MSK conditions and enable individuals who may be at risk or have developed early signs of a musculoskeletal disorder to access appropriate prevention support in a timely manner.
Commission evidence based strength and balance activities.
Use PHE’s Musculoskeletal Diseases profile to help understand the health needs of your local populations, the number of people accessing services and the outcomes services deliver.
Use PHE’s ROI tool to assess interventions designed to prevent and treat individuals with MSK conditions.
Use PHE and the National Falls Prevention Coordination Group’s ‘Falls and fracture consensus statement’ and resource pack, including the commissioners checklist, to support a whole system approach to commissioning falls and fracture prevention.
Healthcare practitioners and providers
All healthcare practitioners should consider how they can influence behaviour to improve MSK health as part of making every contact count (MECC).
Make sure that all employees are aware of the tools and resources to assist in raising awareness about the main risk factors associated with MSK health and signposting to the support available in the local area such as PHE’s One You resources and MECC.
Raise awareness about the positive actions, such as strength and balance type activity, that individuals can take to look after their bones, muscles and joints across during their life, provide information to enable individuals who may be at risk or have developed early signs of a MSK disorder to access appropriate help and support in a timely manner.
Voluntary Sector
The voluntary sector continues to be a strong advocate for people with musculoskeletal conditions, empowering local communities and influencing and shaping policy decisions based on evidence.
Strengthen links between partners and local communities, creating new opportunities to support people with MSK conditions using the model of social prescribing.
Continue to work in partnership with the public sector to promote best practice, improve data and information on MSK and share the expertise and knowledge gained through research programmes.
Private Sector
Actively promote and encourage the use of evidence based tools and resources to maximise the efforts in creating a healthy, safe and productive working environment.
Recognise the need to go beyond legislated minimum standards, and adhere to the highest standards of corporate social responsibility.
Royal Colleges and Associations
The royal colleges and professional associations can support MSK health and productive ageing by providing pre and post-graduate education and professional development for professionals including resources focussing on prevention.
They should also provide guidelines and policy statements to inform professionals and the public.
Resources
Download the Health matters infographics.
Read the Health matters blog.
Watch Health matters videos.
Read the case study: Supporting musculoskeletal (MSK) health at work.
Read the case study: Implementing stratified care for low back pain: STarT Back.
Read the case study: ESCAPE-pain for knee pain.
Read the case study: SWAP: delivering primary care vocational advice.
Read the case study: Better Bones Osteoporosis Service from Kingston Public Health.
Read the case study: Improving primary prevention of falls for Newcastle’s over 65s.
Read the case study: Dancing in Time.
