PSA testing and prostate cancer: advice for men without symptoms of prostate disease
Updated 12 December 2024
The prostate specific antigen (PSA) test is a blood test that can help diagnose prostate problems including prostate cancer. It is not a perfect test. It will miss some prostate cancers, will detect some that would never go on to cause harm and can show a raised PSA level when there is no prostate cancer present.
This leaflet provides clear and balanced information that can help you decide if you want to have a PSA test or not. Before making a decision, you may want to talk to your GP, practice nurse, partner, family members or friends.
Prostate cancer
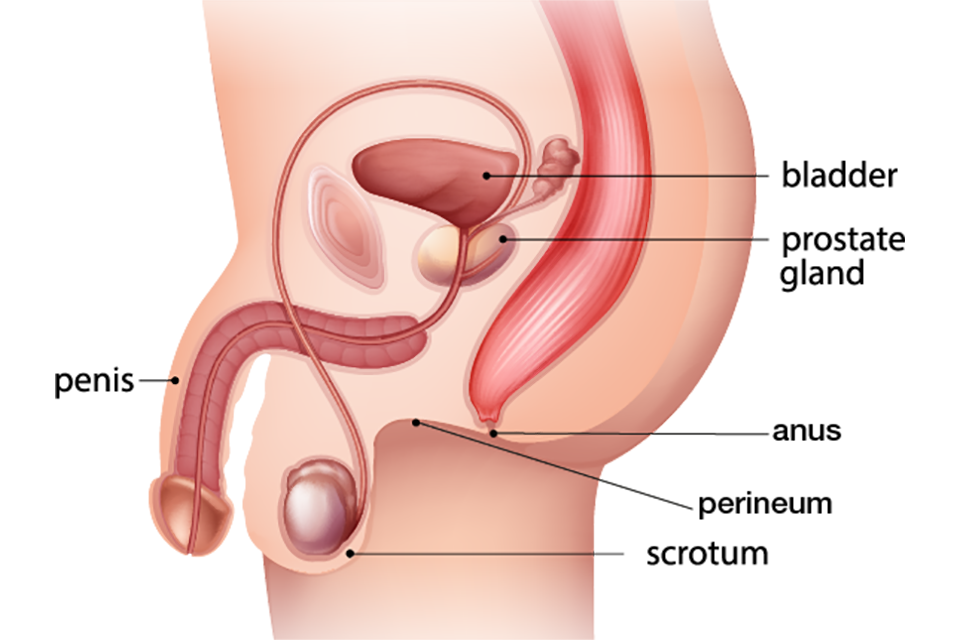
The prostate gland lies just below your bladder. It helps produce healthy sperm. Problems with the prostate gland can affect how you urinate and your sexual function.
Prostate cancer is caused when some cells in the prostate start to grow out of control.
Prostate cancer is the second most common cause of cancer deaths in UK men. Each year about 50,000 men are diagnosed with prostate cancer and about 12,000 die from the disease. More than 75% (3 in 4) of men with prostate cancer survive with the disease for 10 or more years. Prostate cancer is rare in men under 50 and the risk increases with age. Most research into PSA testing has been among men aged between 50 and 69.
Slow-growing cancers are common. Prostate cancer may not cause symptoms or shorten your life.
Symptoms
Most early stage prostate cancers do not have any symptoms.
If you notice anything that is not normal for you, or are worried, you should speak to your GP.
Risk
You are at higher risk of developing prostate cancer if you:
- are aged 50 or older
- have a close relative, for example brother or father, who has had prostate cancer
- are of black ethnic origin (double the risk)
PSA test
PSA is a protein that is made by prostate cells. It is measured using a blood test. Most men will not have a raised PSA level. PSA levels can be raised in a number of conditions, such as a urinary infection, an enlarged prostate, prostatitis or prostate cancer.
If you decide you want a PSA test, you should refrain from sexual activity and vigorous exercise, such as cycling, in the 2 days before the test as they can affect the PSA level.
Having a prostate biopsy or cystoscopy (where a small tube is inserted into the bladder) in the 6 weeks before the test may also affect the PSA level.
Test results and follow-up
If you have a raised PSA level you may be offered another PSA test to check if it remains high.
Your GP may then discuss referral to a specialist (urologist) with you. You may have further investigations, such as a magnetic resonance imaging (MRI) scan of the prostate. Depending on the MRI result, you may then need a biopsy. A biopsy involves taking small samples of your prostate, usually through your back passage or perineum (the skin just in front of the anus), and checking them for cancer.
If further investigations show you have prostate cancer, your specialist will discuss the most appropriate follow-up for you. Regular follow-up (also known as monitoring or surveillance) can be an option for many men who have cancer confined to the prostate gland. Regular follow-up can include blood tests, clinical examination, MRI imaging scans and biopsies. Other options can include surgery, radiotherapy and hormone therapy.
Treatment options for faster growing or advanced cancers include hormone therapy, biopsies and chemotherapy.
See National Institute for Health and Care Excellence (NICE) guidance on Prostate cancer: diagnosis and management (NG131) for more information on the management of:
- localised prostate cancer (section 1.3)
- advanced prostate cancer (section 1.5)
Side effects of prostate cancer treatments can include problems with erections, loss of fertility and bowel and urinary incontinence.
The PSA test and what the results might mean
The image below shows that the prostate gland releases PSA molecules into the blood. The PSA test measures the amount of PSA molecules in a patient’s blood.
It’s normal for all men to have some PSA in their blood. A raised PSA level can be a sign of prostate cancer, but it can be raised for lots of reasons including:
- a urinary or urinary tract infection (UTI)
- prostate stimulation, recent ejaculation or anal sex
- recent vigorous exercise
- other prostate problems, such as an enlarged prostate
If you have a raised PSA, it doesn’t necessarily mean you have cancer. Your doctor should talk to you about your results and what they might mean.

Before you decide whether to have the test, think about the information on this page. Talk to your GP about the possible advantages and disadvantages of the test and your own risk of prostate cancer.
Having a PSA test is a personal decision - what might be important to one person may not be to another and having the test might not be the right thing for you.
Possible advantages
A PSA test can help pick up prostate cancer before you have any symptoms.
A PSA test can help pick up a fast-growing cancer at an early stage, when treatment could stop it spreading and causing problems or shortening your life.
Possible disadvantages
You might have a raised PSA level, without cancer. Many individuals with a raised PSA level do not have prostate cancer.
The PSA test can miss prostate cancer. A small proportion of men who have a low PSA level will later be found to have prostate cancer.
If your PSA level is raised you may need a biopsy. This can cause side effects, such as pain, infection and bleeding. Not all men will need to have a biopsy.
You might be diagnosed with a slow-growing cancer that would never have caused any problems or shortened your life. Being diagnosed with cancer could make you worry, and you might decide to have treatment you do not need.
Treatments can cause side effects which can affect you daily for the rest of your life, such as urinary, bowel and erection problems.
Further information
For more information on prostate cancer, prostate problems and PSA testing visit:
The Office for Health Improvement and Disparities and Prostate Cancer UK created this information on behalf of the NHS.
