Report: Qualitative research with working people exploring decisions about work and care
Published 7 October 2024
Crown copyright 2024.
You may re-use this information (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit the National Archives.
or write to:
Information Policy Team
The National Archives
Kew
London
TW9 4DU
or email psi@nationalarchives.gov.uk
This document/publication is also available on GOV.UK
If you would like to know more about DWP research, email socialresearch@dwp.gov.uk
First published October 2024
Report number 92
ISBN 978-1-78659-676-5
Views expressed in this report are not necessarily those of the Department for Work and Pensions or any other government department.
Executive summary
This report presents findings from qualitative research with working people who were making, or had made, decisions about work and care. This project explored:
- their experiences;
- the decisions people faced and their information needs;
- the extent to which these needs were met by information available online.
Research design
Two strands of primary research were conducted.
The first strand consisted of 15 depth interviews and 10 follow-up interviews with working people who had learnt within the past year that a family member would need support, or increased levels of support.
In the second strand, four focus groups were conducted with people who had been providing care for a family member for one year or more. All were in work when they first started to provide care. Participants were recruited via four local carers centres, through which they were receiving support or information at the time of the focus groups.
Together, these two strands provided a combination of real-time and retrospective views and experiences. This report presents findings from both strands.
Experiences of providing care
While each participant’s experience of providing care was unique, a pattern or journey involving a number of common stages emerged:
The caring journey
The experience within each stage:
- Identification of need – Learning that a family member would need support.
- Initiation of care – A focus on the present and meeting immediate needs as opposed to planning for the long term. Providing care was reported to be mentally and physically tiring, leading participants to focus on getting through each day or week.
- Managing – Combining work and care and feeling that this was sustainable.
- Stress – Feeling pressure as a result of combining work and care. This was either because of an increase in intensity of care requirements or the length of time over which they had been providing support. Participants described that providing care over a longer period of time became more tiring and hard to manage.
- Crisis – Feeling unable to combine work and care sustainably.
- Receiving support – Gaining access to support for themselves. This tended to be a reactive measure following the preceding stages, rather than a proactive step. Support could help them to overcome feelings of isolation and social exclusion and encouraged them to consider their own wellbeing, including the role of work in their wellbeing and the potential for returning to the labour market.
Initiation of caring activities
Participants did not actively decide to initiate caring activities. Instead they instinctively reacted to learning that their family member needed support.
At this point, participants’ primary concern was meeting the needs of the care recipient. Secondary consideration was sometimes given to how to combine work and care, the financial implications of the person’s care needs or options for external support. Participants rarely considered their own wellbeing or the longer term implications of their actions at this point. When care needs emerged or increased rapidly, participants had to make decisions about care, work, finances and use of external support quickly. In these circumstances, participants reported that family members recognised that help was needed and offered support. In contrast, when care needs increased more progressively, decisions were made more slowly and this seemed to act as a barrier to receiving support from both external information sources and family members.
Regardless, their actions did have long term consequences which were not always anticipated or considered. This provides some support for the hypothesis that improved access to and use of information may improve decisions in the early stages of providing care and improve peoples’ long-term outcomes.
Although starting to provide care was not seen as an active decision, participants did discuss a number of themes that influenced whether they took up the role, and in what way. These included:
- Family circumstances – for example, whether the recipient of care was a parent or partner, and whether or not participants had siblings who were able to provide care
- Proximity – family members who lived nearer to the care recipient reported they took on day to day caring activities, rather than those who lived further away as this seemed a more practical decision at the time
I feel frustrated. Because she lives close to me, I’m the default carer, seven days a week. There wasn’t a proper discussion about sharing the load – Male, 52, Nottingham
- Perceived duty – participants often felt it was their role as a family member to provide support.
- Focusing on the present – a focus on care recipients’ current needs rather than considering what their care needs may be in a few years’ time and what this might mean for the individual providing care.
I’ve just been putting out each fire as it lights up. I haven’t had time to think that far into the future about help – Female, 54, Nottingham.
- Perceptions of external or ‘formal’ care – lack of awareness of or willingness to use professional care services affected whether or not participants took on care activities themselves.
How participants felt about combining work and care in the early stages of providing care
A range of themes were reported as affecting how participants felt about combining work and care. These are shown below:
Themes which affected how participants felt about combining work and care
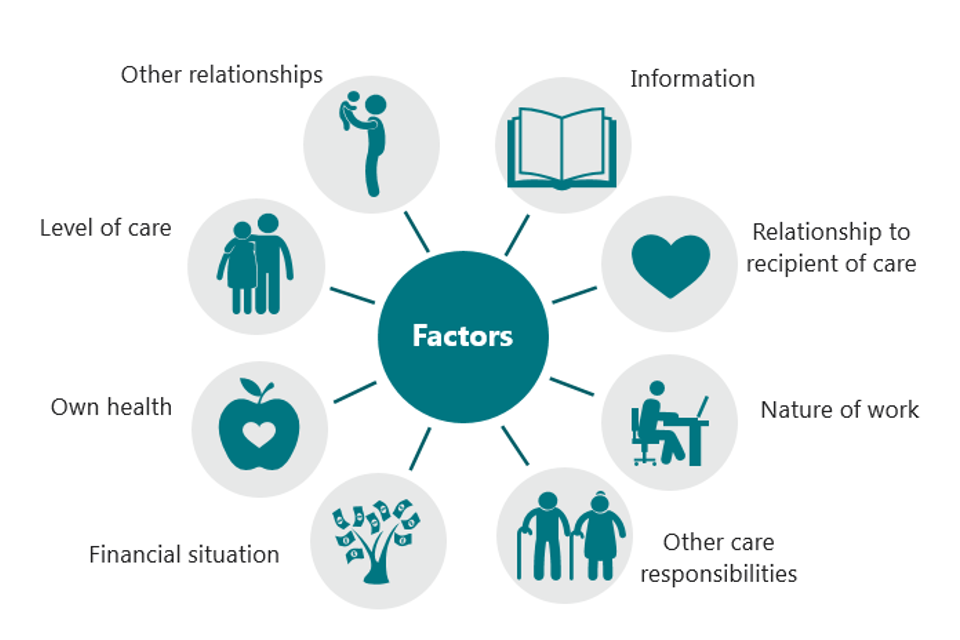
Themes included:
- Information – Participants who had left work could feel that they had no choice but to do so. Participants could then also reflect on whether they might have stayed in employment with more information about financial support, practical support such as the availability of professional care, and the potential long term consequences of leaving work. Early information about employment rights such as flexible working was reported as being key to helping people to combine work and care
- Relationship to care recipient – the type of relationship the participant had with the person needing care (that is whether they were a parent, child or spouse of that person) affected how they felt about meeting their care needs, now and in the future
- Nature of work – whether participants’ jobs were full or part-time; whether they were self-employed or an employee; access to flexible working; how supportive their workplace was and job satisfaction all affected views on the feasibility of combining work and care. Lack of flexibility limited participants’ ability to accommodate short notice care needs or crises. Self-employment was said to bring advantages and disadvantages as it often allowed more flexible working but sole responsibility for generating income also added greater pressure
- Financial circumstances – participants with savings or a higher income were more able to reduce their working hours if needed. However, financial security was also found to act as a barrier to seeking support which could result in people ending up in a worse financial situation than they might otherwise have been
- Own health – participants who had, or whilst caring developed, mental and/or physical health conditions found being able to combine work and care more challenging
- Level of care and other caring responsibilities – the nature, intensity and unpredictability of care activities all influenced the extent to which participants felt able to combine them with work. Providing care for multiple people or living closer to the recipient of care were associated with spending more time providing care overall and so reducing participants’ capability to continue working
- Other family relationships – participants felt they were ‘spreading themselves too thinly’ by trying to combine work and care, they described feeling stressed and anxious about not having enough time for other family members (such us partners or children) as a result
Experiences of people who had been providing care for a year or more
Participants who had been providing care for longer than a year had either:
- continued with the same working pattern including number of hours
- changed their working patterns by either reducing their hours, becoming part-time or moving to more flexible shift work
- changed their employment
- left employment to provide care full-time
Flexibility at work, employer attitudes and the intensity of caring activities were felt to have strongly influenced which of these options participants took. Those who continued to work the same number of hours said that they did so in part because they could not afford not to, or that sharing of activities among their family or someone else better enabled them to combine work and care.
Those who had left the labour market demonstrated enthusiasm to return and wanted to find a way of combining work with their caring activities. They recognised the positive effect that work could have on their wellbeing.
You don’t realise how important work is [until you leave]. If you’re at work, even for just a few hours, it can boost your self-esteem….and it’s part of who you are – Female, North West Focus Group.
Experiences of accessing information and support
Initial information seeking was focussed on the health condition of the care recipient and finding support available to them. Participants rarely searched for information about support for themselves, or how best to combine work and care, unless pointed towards online sources by other people.
Offline information sources were discussed as being most helpful early on, as participants’ questions at this point were broad. Offline sources that participants wanted to use in the early stages of their caring journey included health professionals, family and friends, local charities and support groups. They thought these offline sources could be used to direct them to online information.
I can remember so many of the conversations [with the GP] were about my mother’s condition. Looking back, there wasn’t nearly enough focus on who was going to be providing the care for her – Female, 50, Nottingham.
Online information searches were used to look for answers to specific questions. Sources which were cited as being particularly helpful included condition-specific charity sites, financial advice sites and social media sites. Participants wanted online sources to be trustworthy, easy to navigate, concise and up-to-date, with a warm tone.
You get a bit overwhelmed sometimes looking [online]. It’s a wall of black text and your brain is tired after work. You want it to be short and snappy, not reading a novel – Male, 51, London.
Recognising themselves as a ‘carer’ had a strong influence on how participants looked for and used information. Until participants saw that the role they were carrying out was experienced by others and recognised by society they could feel isolated and were unaware of the support available. This is because they were unaware of what it was to be a ‘carer’ and that there was support available to this group. Recognition that the term ‘carer’ applied to them helped them look for information for themselves, led them to websites targeted at people providing care, networks of other carers providing support and it helped them identify what types of financial support they were entitled to. There was evidence of this recognition taking a number of years to happen and participants in this position said they would have wanted to understand that the term ‘carer’ applied to them earlier because of the support it unlocked. This raises the question of how information should be positioned to be accessed sooner, regardless of whether people identify as a carer or not.
You just feel like you’re a family member who is looking after someone, so at what point do you realise you’re a carer… if there was just a way of knowing that the support are there that bit earlier, to help give your life more balance – Female, North West Focus Group.
Key implications for the development of future information
The following implications for information providers emerged from the research.
Proactively supply information to support the needs of people providing unpaid care
Those in the early stages of providing care tended not to seek information to support their own wellbeing, or manage their new caring activities alongside work. To improve access to this information, it could be proactively given to people, to reduce the challenges experienced by those providing care, when navigating and accessing information independently.
Make use of offline sources to reach those providing care and signpost to further information online
Participants described more readily accessing offline sources in the early stages of providing care. Leaflets and signs in GP and hospital waiting areas were described as being particularly useful.
Target carers more explicitly through online sources in the care recipients’ journey
Participants reported accessing websites about the care recipients’ condition and needs, for example, those with a defined condition would look to condition specific charity websites or to GOV.UK for the support available for them. These websites could more explicitly reference the individual providing care and help signpost them to information about support for themselves.
Design information for time-poor users and make it easier to process
As a result of being time-poor as well as mentally and physically tired, participants preferred information to be clear, concise and easy to navigate.
Make more use of the most trusted and well known information sources
Participants did not always know what online information to trust. Some websites participants accessed early on, however, were more immediately recognised as authoritative and trusted, for example the NHS website and GOV.UK. Signposting from more well-recognised sites to other useful websites that new carers may be unfamiliar with may help them navigate and assess the legitimacy of online information more quickly.
Use a warm tone when providing information to make it more engaging
This signalled to participants that the author, or organisation, understood their experience. Participants reported they were likely to use and engage with sites which demonstrated greater understanding of their circumstances.
Emphasise the value of proactively considering their own long-term needs and options
Participants felt that they would have benefitted from being encouraged to consider their own needs as early in the journey as possible.
Note on interpretation of research findings
Findings in this report are based on research conducted in 2019. While contextual changes since 2019 may affect how people make choices about work and care and should be considered, many of the findings remain relevant to understanding the experiences of working people facing choices about work and care.
Acknowledgements
The authors would like to thank all of the people who gave their time to participate in this research, the Carer’s Trust and the four carers centres who facilitated and hosted the focus groups.
We would also like to thank Dr Carla Groom, Cate Fisher, Lucien Bush and William Downes in the Human-Centred Design Science team, Department for Work and Pensions for their input into the design and support throughout the process.
The Authors
This report was authored by researchers at the Ipsos MORI Social Research Institute. Their roles at the time of the study in 2019 were:
Joanna Crossfield, Associate Director, Ipsos MORI
Yasmin White, Senior Research Executive, Ipsos MORI
Darragh McHenry, Research Executive, Ipsos MORI
Glossary of terms
Attendance Allowance: a benefit for individuals who are over the age of 65 and have care needs due to an illness, disability or mental health condition.
Carer’s Allowance: a benefit payment for those who spend 35 hours or more a week caring for someone who is in receipt of certain disability benefits, and who earn £151 or less per week net of allowable deductions.
Carers centres: independent, local organisations providing a range support services – usually including but not limited to information and advice – to people in the local area who are caring for someone.
Caring activities: supporting someone who needs help with everyday activities due to illness, disability or old age. This included but was not limited to supporting them with grocery shopping, laundry, dressing, cleaning and helping them with their finances or managing professional care.
Professional care: paid-for care provided by professional carers, care homes and day centres.
External support: Where the term external support is used, this refers more broadly to information and help provided both to carers themselves and/or the care recipient.
Personal Independence Payments: a benefit for people aged between 16 and 64 who have an illness, disability or mental health condition to help with some of the extra costs of their condition.
1. Introduction
This report covers findings from two strands of qualitative research. The research was conducted with people who were either currently providing unpaid or ‘informal’ care to a family member or were considering doing so. All participants were in work when they learnt that their family member would need support. Fieldwork took place in January and February 2019. These findings explore experiences of making decisions around caring and working, and information needs in this area.
1.1 Background
The Department for Work and Pensions (DWP), Government Equalities Office (GEO) and Department for Health and Social Care (DHSC) wanted to understand how people approach decisions about meeting care needs for their relatives, combining this with work, and the extent to which the long-term consequences of these decisions are considered. The hypothesis underlying this research was that information deficits can contribute to people who provide unpaid care leaving the labour market, without understanding whether this is the best option for them long term.
The Government aims to help people providing, or considering providing, care to be more aware of the different options available to them, and the implications of the decisions they make.
The overall aim of this project was to explore:
- The experiences of working people who have decided to, or are considering, supporting a family member who needs care
- Key decisions people face and the information they need at those points
- The extent to which their information needs are met by the information available online at the time the research was conducted
The findings will be of particular interest to policy makers, charities and researchers working in this space, and indeed any organisations or professionals providing support to or coming into contact with working people facing decisions about someone else’s care.
1.2 About the research
1.2.1 Aims of this research
This research comprises two strands of primary research. The first explored the experiences of individuals who had learnt within the past year that their family member would need support. The second strand considered the experiences of those who had been providing care for over a year.
The first strand of research, depth interviews with individuals who had learnt their family member would need support or increased support in the past year sought to understand:
- How working people make decisions about how to meet a relative’s care needs, including who is involved and what questions they have
- Working people’s information needs when a family member first has care needs
- Experiences of seeking and using online information to inform decision making
- The key barriers and challenges faced when trying to find or act on information
- Preferences and views around online information tools and resources that meet their needs
The second strand of research; focus groups with people who had provided care for over one year explored:
- The experiences of those further along their caring journey, including their experiences of making decisions and seeking information about providing care
- Where they have sought information and how their information needs have changed over time
- How their employment has been impacted and what role their employer has played.
- What they would have wanted to know earlier in their journey to help them make more informed decisions
- What additional online information would help someone in a similar position to them now
1.2.2 The research design
Strand one: depth interviews with individuals who had learnt their family member would need support or increased support in the past year
Fifteen people took part in face-to-face depth interviews lasting one hour each. Prior to each interview, participants were asked to complete a short diary task. Fieldwork took place in London, York and Nottingham between the 23rd January and 1st February 2019.
Ten participants were selected to take part in 30 minute follow up telephone interviews two weeks after their first interview. The aim of these interviews was to understand if there had been any changes to their experiences and to allow both researchers and participants the opportunity to revisit topics of discussion following a period of reflection[footnote 1].
Sample
Quotas were set to ensure that all participants were currently working and had learnt within the past year that a family member would need support or an increased level of support with day-to-day activities. Participants were either considering or had taken on caring activities. This research did not include those who had decided not to take on caring activities.
Participants were recruited to reflect a range of relationships with the recipient of care; distance lived from the care recipient; their household income and IT literacy.
A full breakdown is shown in Table 2.1.
Table 2.1: Depth interviews sample[footnote 2]
| Quota | Subgroup | No. of interviews |
|---|---|---|
| Work status | Full-time | 5 |
| Work status | Part-time | 7 |
| Work status | Self employed | 3 |
| Gender | Female | 10 |
| Gender | Male | 5 |
| Age | 45-54 | 9 |
| Age | 55-63 | 6 |
| Type of condition of care recipient | Mental Health | 12 |
| Type of condition of care recipient | Physical Health | 9 |
| Type of condition of care recipient | Sensory[footnote 3] | 1 |
Strand two: focus groups with people who had been providing care for longer than one year
Four focus groups were held, one each in North West, South West, London and East Midlands. Fieldwork took place between the 14th February and 25th February 2019.
Sample
Each group consisted of between five and seven people. Every participant was in work when they learnt that their family member needed support and had been supporting this individual for over one year.
Recruitment of participants was carried out by The Carers Trust and focus groups took place in a local carers centre. This meant that all participants were receiving support through these centres.
A full breakdown of this sample is shown in Table 2.2.
Table 2.2: Focus Group samples
North West Focus Group sample
| North West | 55 to 63 | 63+ |
|---|---|---|
| Age | 3 | 2 |
| North West | Male | Female |
|---|---|---|
| Gender | 0 | 5 |
| North West | Spouse/Partner | Sibling | Child | Parent |
|---|---|---|---|---|
| Relationship to care recipient | 1 | 1 | 2 | 1 |
| North West | Physical Health | Mental Health |
|---|---|---|
| Care recipient condition | 3 | 4 |
| North West | Part Time | Self Employed | Caring Full Time | N/A |
|---|---|---|---|---|
| Employment status at time of research | 1 | 1 | 1 | 2 |
South West Focus Group sample
| South West | Under 35 | 45 to 54 | 55 to 63 |
|---|---|---|---|
| Age | 1 | 3 | 3 |
| South West | Male | Female |
|---|---|---|
| Gender | 4 | 3 |
| South West | Child | Parent | Daughter in Law |
|---|---|---|---|
| Relationship to care recipient | 4 | 2 | 1 |
| South West | Physical Health | Mental Health | Sensory |
|---|---|---|---|
| Care recipient condition | 6 | 6 | 1 |
| South West | PT (16-35hrs) | Self Employed | Retired | Caring Full Time |
|---|---|---|---|---|
| Employment status at time of research | 1 | 1 | 1 | 5 |
London Focus Group sample
| London | 35 to 44 | 45 to 54 | 55 to 63 |
|---|---|---|---|
| Age | 1 | 3 | 3 |
| London | Male | Female |
|---|---|---|
| Gender | 2 | 6 |
| London | Spouse/Partner | Child | Parent |
|---|---|---|---|
| Relationship to care recipient | 1 | 1 | 5 |
| London | Physical Health | Mental Health |
|---|---|---|
| Care recipient condition | 6 | 4 |
| London | PT (7-16hrs) | Caring Full Time | N/A | |
|---|---|---|---|---|
| Employment status at time of research | 1 | 5 | 1 |
East Midlands Focus Group sample
| East Midlands | 35 to 44 | 45 to 54 | 55 to 63 |
|---|---|---|---|
| Age | 2 | 2 | 2 |
| East Midlands | Male | Female |
|---|---|---|
| Gender | 1 | 6 |
| East Midlands | Spouse/Partner | Parent |
|---|---|---|
| Relationship to care recipient | 4 | 2 |
| East Midlands | Physical Health | Mental Health | Sensory |
|---|---|---|---|
| Care recipient condition | 4 | 6 | 1 |
| East Midlands | Full Time | PT (16-35hrs) | Caring Full Time | Retired | |
|---|---|---|---|---|---|
| Employment status at time of research | 2 | 1 | 2 | 1 |
1.2.3 Conduct of the research
All fieldwork was conducted by researchers in the Employment, Welfare and Skills team at the Ipsos MORI Social Research Institute. Screening tools were used to allocate participants to quotas. With participants’ consent, interviews were recorded on 256-bit encrypted recording devices and data was handled in line with DWP and GDPR requirements. Reflecting the sensitive nature of this research, participants were offered information sheets with information of organisations they could contact for information or support if required.
1.2.4 Analytical approach
The data collected from these interviews were entered into an analysis grid in Microsoft Excel, used as the basis for analysis to identify common themes. The analysis grid grouped the findings from the interviews into themes, based around the study objectives and those which emerged through analysis. In addition, analysis considered similarities and differences amongst different subgroups such as rural and urban locations, age and gender.
1.2.5 Interpreting the findings in this report
Qualitative research is detailed and exploratory. It offers insights into people’s opinions, feelings and behaviours. All participant data presented should be treated as the opinions and views of the individuals and employers interviewed. Quotations and case studies from the qualitative research have been included to provide rich, detailed accounts, as given by participants.
Qualitative research is not intended to provide quantifiable conclusions from a statistically representative sample. Furthermore, owing to the small sample size and the purposive nature with which it was drawn, qualitative findings cannot be considered to be representative of the views of all people providing care. Instead, this research was designed to explore the breadth of views and experiences, in order to develop a greater understanding of experiences and decisions in regard to providing care and working.
Data in this report are based on self-reported perceptions and views of participants. It is important to note that although such perceptions may not always be factually accurate, and may be subject to the limits of memory, they represent participants’ beliefs and experiences as related during the time of research.
This report is based on findings from those who had taken up caring activities or were considering providing unpaid or informal support to a family member.
2. The Caring Journey
This chapter explores participants’ experiences of the caring journey. It starts by giving an overview of the journey and then focuses on the initiation of care, considerations made and how participants felt about combining work and care.
2.1 The Caring Journey
Participants reported unique caring experiences, with numerous themes influencing the shape of their overall journey. However, there was a pattern of experiences amongst participants in this sample: participants who had left the labour market reported having done so at a time when combining work and care became unsustainable[footnote 4]. This pattern is shown below[footnote 5].
- Identification of need.
- Initiation of care.
- Managing.
- Stress.
- Crisis.
- Receiving support.
The experience within each stage was:
- Identification of need – Learning that a family member would need support.
- Initiation of care – A focus on the present as opposed to planning for the long term.
- Managing – Combining work and care and feeling that this was sustainable.
- Stress – Feeling pressure as a result of combining work and care. This was either because of an increase in intensity of care requirements or the length of time over which they had been providing support. Participants described that providing care over a longer period of time became more tiring and hard to manage.
- Crisis – Feeling unable to combine both work and caring activities sustainably.
- Receiving support – Gaining access to support for themselves. This tended to be a reactive measure following the preceding stages, rather than a proactive step.
Participants in this study accessed support for themselves after recognising themselves as a ‘carer’. There were examples from the focus groups of participants not identifying as a carer until a number of years after they had initiated caring activities. Instead, they initially saw their caring activities as a progression of their relationship with their family member once they required care. Paths to identifying as a carer included:
- picking a leaflet up out of curiosity whilst in hospital with the care recipient and realising that they fitted the description of a carer
- a friend of a neighbour suggesting that a participant was a carer for her mother after seeing them together
- identification by the Jobcentre Plus when applying for benefits and realising they fit the description of a carer as given in the eligibility for Carer’s Allowance when looking for financial benefits
You just feel like you’re a family member who is looking after someone, so at what point do you realise you’re a carer… if there was just a way of knowing that the support are there that bit earlier, to help give your life more balance – Female, North West Focus Group.
Prior to seeing themselves as carers, participants were in need of support but did not know it existed for them. As such, identifying as a carer was reported as being an important part of the caring journey because it showed participants that what they were doing was recognised by society. This opened the door to accessing support for themselves and was reported to give them a sense of identity and unity with others in the same position. Evidence from the focus groups suggests that there was a lack of information aimed at those providing care through the touchpoints and information sources they were using in the course of providing care.
Case Study
One participant had been providing care for their father for the past ten years and only realised they were a carer after providing this support for five years. This realisation happened when their father was seen by a different GP – who suggested that, from what they had described about their activities, they were a carer. Until this point, the participant had explored support for their father, namely what financial support he might be entitled to, but had never looked for support for themselves. After this signposting from the GP they made contact with the local carers centre, which provided help accessing financial support and provided emotional support. It also connected them with other people providing care, helping them feel less isolated.
2.2 Initiation of caring activities
Participants in both strands of research were asked why they decided to take up caring activities to support their family member. Participants responded by clearly stating that taking on caring activities did not feel like a choice or decision. It was their instinctive reaction to the situation.
No, no, no, there was no choice to be made – it’s my mother. Period – Male, 60, London.
At this early stage, individuals were not considering potential effects on themselves, particularly in the long term. This made them less likely to seek information on support available for themselves[footnote 6].
2.2.1 Themes affecting the initiation of caring activities
Although participants emphasised that they did not experience the initiation of caring activities as an explicit choice, a number of themes emerged through discussion that seemed to have influenced their actions:
- Relationship – There were participants who reported that they took on the caring activities as a result of feeling that it was part of their role as a family member. This was the case whether the care recipient was a parent, a child or a spouse. At the initiation of caring activities, participants did not describe experiencing this ‘duty’ or ‘responsibility’ (as they referred to it) in a negative way, it was their response to meeting the needs of their family member. For example, when the care recipient was a spouse or partner, one prominent reason participants took on caring activities was because they saw themselves as the person closest to the care recipient. Participants providing care for adult children reported that this felt like part of their role as a parent
I’d expect that [to provide care], it’s no problem at all – Male, 63, York.
-
Personality – participants in this research who described themselves as having a ‘caring nature’ reported that this contributed to their uptake of caring activities, as doing so fit with their self-image
-
Family dynamics and location – The wider family dynamic influenced the adoption of caring activities, particularly when caring for parents. Participants without siblings took on the caring role for their parent as they had no other immediate family to involve. Within larger families, participants reported that the person who was seen as most able to provide support took responsibility for day to day, physical caring activities such as help with dressing, cooking, cleaning and shopping. This ability seemed to be determined by perceived amount of free time or physical proximity. Those who lived closer or had older families, for example, were more likely to provide day to day caring activities than those who lived further away or had younger children. Participants who lived further away were more likely to take on caring activities such as managing finances
-
Focusing on the present – At the initiation of caring activities, participants seemed to be focused on the present, rather than the future. This was because providing care and meeting the recipients’ needs, along with working, required their full attention, acting as a barrier to taking a long-term view
-
Professional care – Amongst participants who had not used professional care this was due to either lack of awareness or attitudinal barriers. Poor awareness of professional care, either its existence or local availability, affected likelihood of taking up caring activities as participants were unaware of other ways of meeting the care recipients’ needs. Amongst those aware of external support, attitudinal barriers included the participant and/or the person they cared for not wanting a stranger in their home or providing intimate support. This is discussed in more detail within section 2.3.1
The other thing I looked into was finding a carer…. You can find somebody that’s lovely and trustworthy, but there are some horror stories about people that could steal from them, could be nasty. You see these things on TV sometimes. That scared me. I’d rather I do it and know that he’s [father] okay – Female, 58, London.
2.3 Decision making at the start of the caring journey
Soon after their initiation of caring activities participants were thinking about work and care; financial implications for themselves and the care recipient, and use of professional care.
- Work and care – Participants considered how care and work would fit together. At the outset of providing care, participants felt able to continue in their job, however there was a need to be more flexible or take annual leave to attend doctor’s appointments and respond to other emergencies
- Financial implications – Participants reported added financial pressure from taking up caring activities. Examples included higher spending on petrol as a result of travelling more to see the care recipient and reducing working hours to accommodate care activities, resulting in lower pay
- External support to help with care needs – This support ranged from advice from doctors or other healthcare professionals, professional carers, day care centres and care homes. The severity of the recipient of care’s health condition affected the extent to which this was considered
At this point, participants reported that they gave very little consideration to their own needs and wellbeing. From the initiation of caring activities, and onwards, participants prioritised those that they were providing care for over themselves.
I’m always on the back burner… I never spend any money on myself and never look nice – Female, 49, York.
Case Study
One participant had been providing care for her daughter. As part of this she looked after her daughter’s son. In order to do so, she decreased the number of shifts she was working. This had an impact on her household finances.
Effect of the speed of progression of care needs
The extent to which participants reported considering the above themes was influenced by the speed with which the care recipient’s needs became apparent or progressed.
When the recipient of care started to need support rapidly, over a course of a day or up to one month, participants had to respond quickly. They described having to make fast decisions about providing care, work, finances and use of external support. In these circumstances, participants reported that family members recognised that help was needed and offered support.
When care recipients experienced progressive conditions, decisions around meeting care needs were made more slowly as the support required increased incrementally over time. In the early stages of providing care, participants reported feeling able to meet the recipient’s care needs, which acted as a barrier to seeking help at this point. Evidence from the focus groups with those who had been providing care for longer suggested that meeting these needs became more challenging over time, but that there was a time during which participants would have benefitted from support but were not sure how or where to access this.
Participants who experienced this gradual increase in their caring activities reported feeling that the division of caring activities in their family was imbalanced. For example, a participant whose mother moved next door to him over 15 years ago, began helping her with smaller tasks such as shopping. After she had a fall, she required a more intense level of care. This participant felt that he became the default person to provide all care because he lived so close to his mother. This led to frustration and conflict with his siblings.
I feel frustrated. Because she lives close to me, I’m the default carer, seven days a week. There wasn’t a proper discussion about sharing the load – Male, 52, Nottingham.
2.3.1 Themes affecting the use of professional care
Use of formal care[footnote 7] was affected by four themes: awareness of the support available, perceived need, attitudes towards external support, and perceived ability to meet needs.
- Lack of awareness – Participants with low awareness of external care did not know what was available, how much it would cost or whether funded care was available. These individuals felt there was not much public or prominent information about professional care and their lack of awareness acted as a barrier to seeking more information about it. As noted earlier, participants were very time-poor and did not feel they had time or energy to explore potential options
- Perceived need – Those aware of the professional care available to them described assessing their options in terms of the level of care needed and weighing this against their working hours and other responsibilities such as school runs and personal activities
- Attitudes towards professional care – Participants who expressed opposition to using professional care felt this way because they did not want a stranger to provide a family member with intimate care or feared that their family member could experience neglect or even abuse. There were also examples of participants reporting that the care recipient shared these feelings or was too ‘proud’ to accept this help. Participants felt positively towards professional care when it met their needs and enabled them to combine caring activities with work and other family commitments
She’s my wife…what are you supposed to do, put her in a care home!? – Male, East Midlands Focus Group.
My mum wouldn’t have it [professional care]…she’s too proud – Male, 60, London.
- Perceived ability to meet needs – Participants who used professional care reported that it did not consistently meet their needs, meaning they continued to provide high levels of support. For example, professional care was reported not to cover emergencies. There were also accounts of professional care being unreliable and carers not always arriving at the specified time. Participants expressed that this generated more worries or concerns than it alleviated and resulted in them checking on their family member more often. Where the care recipient had more consistent care needs or was less in need of emergency support, participants reported that professional care was better able to meet their needs
We had carers coming in when I was still working. As my mum is in a wheelchair she needed her meals bringing to her, and then the carers wouldn’t turn up or couldn’t make it on time – she has Type 2 diabetes, so she needs meals on time. You need reliable services to make it possible to work – Female, London Focus Group.
Without the carers coming in twice a day, either my wife or I wouldn’t be able to work… it allows us to keep a bit of normality about our routine – Male, 55, Nottingham.
2.4 How people felt about combining work and care in the early stages of the journey
This section is based on interviews with those in the early stages of providing care as well as retrospective views gathered in focus groups.
The themes discussed affected the intensity of participants’ caring journeys and therefore their perceptions of the sustainability of combining work and care.
Themes that influenced how participants felt about combining work and care[footnote 8]
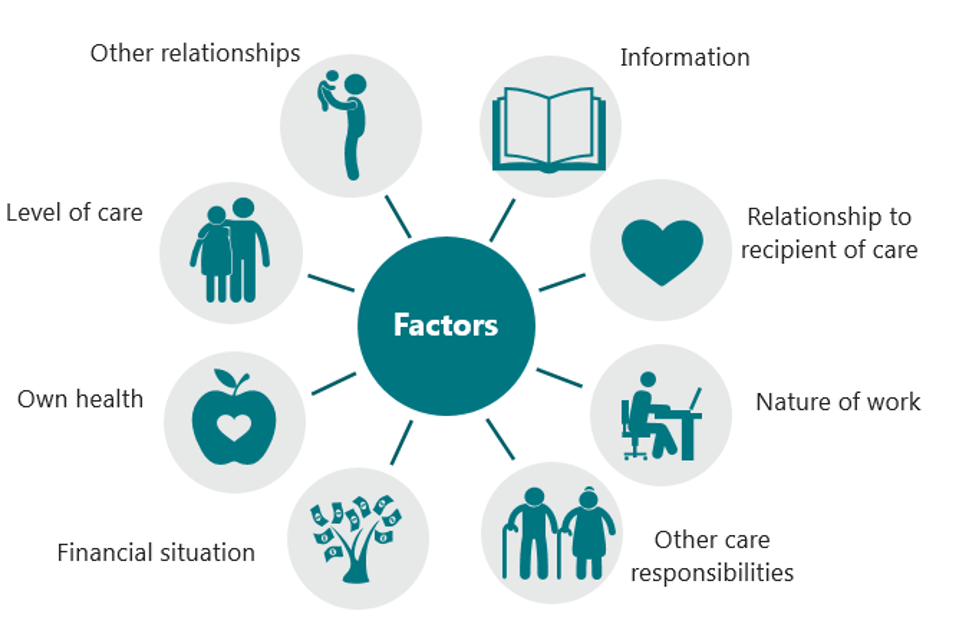
Relationship to care recipient
Participants who cared for a parent recognised that people would need more support as they became older. However, when a partner or child needed care, participants seemed to be less emotionally prepared as it was unforeseen. They expressed concern for both their own future and that of the care recipient. The progression of care needs brought about by old age were experienced more gradually, rather than having a sudden onset. This influenced participant’s ability to combine work and care in the short and longer term.
She’s my mum, she looked after me… I was always going to look after her if something happened – Female, 52, Nottingham.
Nature of work
Nature of work was reported to strongly affect the extent to which participants felt they could sustainably combine work and care. Themes within this included:
- Working patterns – Working part-time and/or flexible hours made working and caring more manageable. Participants who worked full-time found it harder to combine caring activities and work
- Self-employment – Self-employed participants had greater flexibility than those who worked for an employer, which to an extent helped them combine caring activities and work. For example, a hairdresser arranged to see clients on set days of the week so she could see her parents on other days. However, self-employed participants were solely responsible for generating their income and felt that responding to care emergencies could jeopardise this. For example, one participant had to cancel a course she was running due to her father’s care needs. She worried that this made her unreliable, and less likely to be taken on in the future
- Flexible working – Flexible working made responding to emergencies and attending appointments with the care recipient more feasible. Flexibility could vary by sector or type of job: participants in the public sector felt their employers were open to flexible working. Participants in client-facing roles described their commitment to their clients, for example having to attend meetings at particular times meant they had less flexibility
- Work environment – Participants reported feeling that their manager and colleagues were supportive of their care activities to a point. They felt that initially there was understanding that they would need flexibility or time off to support a relative but colleagues and managers did not understand that this would be ongoing. After a certain point participants described feeling guilty about not being able to participate as fully as others at work or for needing time off
- Job satisfaction – Participants with higher job satisfaction stated that they felt work acted as a break from their caring role. Those with more experience of providing care also spoke of work as a positive channel which offered respite from caring activities as it gave them an opportunity to think about something else. In turn, work had a positive impact on wellbeing. This is explored in more detail in section 3.1.2
It [work] gives you sanity – Female, East Midlands Focus Group.
Other caring responsibilities
Providing support to more than one person influenced how participants felt about combining work and care. This was the case for both men and women. For example, one individual cared for to her mother-in-law, her neighbour, her father and mother. She reported that caring for multiple people and combining this with work and other responsibilities made her feel pulled in different directions. She felt she didn’t have time to look after herself which made her question whether she could combine all of these activities.
This [mother in law’s diagnosis of Parkinson’s] tipped us over the edge really. We knew things would never be the same. I was at my wits end trying to juggle everything she did and step up caring for her. My husband buries his head in the sand – Female, 54, York.
Financial circumstances
Those who were struggling financially or did not have savings felt this as an additional pressure. These participants looked to the Government for financial support for either the care recipient or themselves (such as Personal Independence Payments or Carers Allowance) soon after taking up caring activities.
Participants who had savings or a higher income were more comfortable about reducing their working hours to accommodate their caring responsibilities if needed, as they felt less financial pressure to keep working and maintain their standard of living.
However, there were cases in which financial security acted as a barrier to accessing support. One participant who had a well-paid job and savings and left work to care for her parents did not seek financial support for a number of years because she did not need to. This held her back her from identifying as a carer and accessing emotional support for herself, and also meant that she spent her own savings before exploring of the availability of financial support. This can be contrasted to the experiences of less financially secure participants who sought financial support sooner and through doing so, were also able to access support for themselves.
Own health
Participants reported rarely considering their own health and wellbeing. For those participants who developed mental and physical health conditions as time progressed, these added an additional challenge to feeling able to combine work and care. Early stage carers who were providing particularly intensive support quickly became aware that combining work and caring activities was physically demanding which could lead to ill-health.
You cannot think [outside of caring], it’s physically draining. You are living in a constant state of stress every day – Male, London Focus Group.
Level of care
The amount and intensity of support required by the care recipient also affected participants’ ability to work. Working and providing care was more challenging when the family member’s condition was severe and / or there were regular emergencies.
On the other hand, participants who provided non-physical support, such as managing finances, felt this to be less intensive. Working alongside these activities was reported to be more manageable.
Access to both informal and formal support can also impact on the level of care needed. For example, those who shared their caring responsibilities with someone else were better able to combine work and care.
Another factor that affected level of care activities was distance from the recipient of care. Participants who lived with the recipient of care saw their role as a full-time responsibility. In comparison, those who lived further away from their recipient of care and had limited contact did not experience this same level of intensity.
Case Study
A participant had been providing care for her mother for the past five years. In the past 12 months her mother’s care needs had intensified. In response to this, the participant started to share caring activities with her sister. To ensure that one of them is always free the participant works evening shifts, whilst her sister works during the daytime.
Other relationships
Caring activities were described as influencing relationships between participants and other family members, such as school age children and their partner. This influenced how they felt about work and care because they felt they could not meet all of their responsibilities. They felt they were ‘spreading themselves thinly’ and described feeling stressed and anxious. They felt that their family responsibilities were more important than work. This was the case for both men and women providing primary care.
Me and my husband don’t have time together [as I spend time looking for my daughter, care recipient, and her children] … there’s a lot of jealousy from my [younger] children as they get jealous of the time he [grandson, son of care recipient] takes up – Female, 49, York.
2.5 Experiences of people who had been providing care for at least a year
This section of the report provides findings from the focus groups and participants who had been providing care for at least a year. This section explores how their journey had progressed over time, particularly in relation to employment.
As time progressed, the themes outlined above continued to affect the individuals and their employment in the following ways:
-
No change to employment or hours worked – Participants who kept the same number of working hours did so with support from other family members to meet the care recipient’s needs. A key motivation for this was reported to be feeling they could not afford to work fewer hours
-
Adapted employment through changes to working patterns and / or career – Participants who adapted their hours to fit around their caring activities reduced the number of hours worked, moved to part-time employment or took up flexible shift work if the option was available. Participants felt this helped them stay in employment, whilst allowing them time to support their family member. There were also participants who turned down career progression opportunities out of concern about the effect the extra demand of their work would have on their caring responsibilities, or that their caring duties would affect their work performance
I had to drop my hours to care for him [her brother]. There wasn’t much of a choice to be made there – Female, North West Focus Group.
- Changed employment – Participants who had changed employment had moved to a more flexible sector, or a job which offered shorter working hours. For example, one participant had become a taxi driver as this allowed him to choose his hours and work around his caring activities
- Break in employment – Participants who had a temporary break in their employment reported both long-term unpaid leave and shorter-term paid leave. Access to this type of leave largely depended on the flexibility of the organisation participants worked for
I couldn’t get the time off to take my son to his appointments. I didn’t have much of a choice [to leave work] – Female, North West Focus Group.
[Leaving employment is] not the easy way out – you try and juggle, you try to keep drama out of the work place, but eventually it comes to a head – Female, South West Focus Group.
You lose your reliability, so even if you have a choice you don’t take on contracts, you kind of back off. You’re out of the market straightaway – Female, London Focus Group.
The two strongest themes that participants cited as prompting them to leave the labour market were the level of care they provided and their type of employment.
- Level of care – When the level of care required increased, individuals began to feel less able to combine work and caring activities. For example, if the care recipient’s health condition worsened and they required more support this would affect their ability to combine work and care
- Nature of work – Participants in full time work or who had an employer who lacked understanding found it increasingly difficult to combine work and care. There was little knowledge of their employment rights, making it more likely that they would leave the labour market
In addition to making changes to their employment, those with more experience of providing care faced other challenges.
Participants described feeling that, over time, they lost their self-identity and confidence. Their entire focus was on caring for the other person and participants described feeling that the other person’s needs were always greater than theirs. This loss of identity was heightened in those who left the labour market. They reported feeling that being a full-time carer meant they had lower social status as people did not understand what they did. Lack of recognition from society exacerbated their loss of confidence. This had a detrimental effect on their confidence in returning to work.
You don’t realise how important work is [until you leave]. If you’re at work, even for just a few hours, it can boost your self-esteem….and it’s part of who you are – Female, North West Focus Group.
There were also reports of feeling isolated. Those who had left the labour market felt that doing so removed important social ties. Participants also felt that their caring responsibilities meant that they had less time to spend with their friends and that their friends would not understand their experiences as a carer as they were so different to their own lives.
Participants also noted facing financial difficulties. Leaving the labour market, or working fewer hours, reduced their income. As well as day to day challenges meeting living expenses, participants worried that this made it difficult for them to save for the future, specifically their retirement.
Amongst participants who had left the labour market there was enthusiasm to return. Whilst participants providing intensive caring support found it hard to see how they could combine work and caring, they were doing voluntary work where possible as they felt that this would be flexible and reflect their needs. Participants in this position were working with their local carer’s centre to help them prepare to return to the labour market. However, supporting their relative remained their main priority, which led to anxiety about how, and whether, they could combine work and care.
If you’d asked us that question about work when we were in work we’d have had more we disliked. Now it looks like a brilliant place to be! – Female, London Focus Group.
Case Study
A female participant who needed a period of leave approached her employer about taking leave in order to adjust to her new caring responsibilities.
After returning to work after three months, her employer had felt they had met the needs of the participant, believing the caring requirement to have been finite, rather than a continuous process.
The employer was less understanding of the participant’s needs to both stay in her position and care for her father, subsequently she felt she needed to move to another job in order to continue caring activities for her father.
3. Information Seeking
This chapter explores the information and sources that people sought once they began caring activities; how information needs can change over time and what people wished they had known at the start of their journey.
3.1 Questions people had early on
Initial information searches tended to be reactive and focused on supporting the care recipient in the short-term, rather than long term needs or support for the participant. This was because providing care could feel overwhelming, particularly in conjunction with other commitments. Participants reported focusing on getting through each day as it came and managing needs as they arose and not having the time or energy to think beyond these. This seemed to act as a barrier to taking a long-term view.
I’ve just been putting out each fire as it lights up. I haven’t had time to think that far into the future about help – Female, 54, Nottingham.
Upon beginning care activities, participants reported having questions about how to manage their situation. What emerged from this study was that upon beginning care activities, participants were starting from a low knowledge base about what support there was to help them.
Participants’ initial questions were about the health condition of the care recipient. Little was known about this before diagnosis, leading to feelings of fear and uncertainty. Participants wanted to better understand the condition, treatment and prognosis. However, those supporting a child or a partner who felt anxious about the prognosis or potential outcomes reported being reluctant to search for in-depth information about conditions out of fear of bad news, such as if the condition was likely to deteriorate or was untreatable.
I don’t think about it [her daughter’s condition]. I get too upset – Female, 49, York.
Participants also had questions about what financial help might be available to them, or the recipient of care. They sought to establish this when they knew more about the condition and its implications. Participants who reported searching for this information did so as a reaction either to the recipient of care having to stop work or needing more support than they could provide at that time.
People who were supporting someone with a physical health condition looked for information about home modifications, wheelchairs or accessibility aids, including entitlement for disability parking badges. People were often unsure what they might be entitled to and called their local authority to find out.
I called up [name] council. I wasn’t sure what she [his mother] would be entitled to, but I thought I could call and ask – Male, 60, London.
3.2 Sources of information used
The sources used by people in the early stage of their caring journey reflects a reactive approach to information seeking. Rather than proactively searching for specific information, people responded to information given to them. Moreover, participants said that they were not able to search for specific things online as they did not know what they should be searching for. These findings remained true throughout the caring journey for individuals who were providing more intensive care as the time they had to look for information was limited.
Regardless of their point in their caring journey, participants felt that offline sources were better suited to answering broad questions and signposting further information. Online sources were seen as being suited to answering detailed or specific questions. Participants felt that being shown that other people were in the same position as them reduced feelings of isolation and demonstrated that there was support available to them.
I haven’t been looking [online for information], because I didn’t know that I could look for anything – Female, East Midlands Focus Group.
3.2.1 Offline sources
Offline sources, such as healthcare professionals and family or friends with similar experiences, were discussed as being early touchpoints, providing initial information and advice about the diagnosis or condition of the recipient of care.
In particular, participants cited healthcare professionals as a regular point of contact and key source of information. Participants were in regular contact with healthcare professionals such as GPs, nurses and doctors from hospitals, as they supported their family member. However, participants reported that conversations focused on the care recipient and that healthcare professionals were unlikely to have raised the issue of their wellbeing with them.
I can remember so many of the conversations [with the GP] were about my mother’s condition. Looking back, there wasn’t nearly enough focus on who was going to be providing the care for her – Female, 50, Nottingham.
People also reported discussing their experiences with friends and family, particularly those who had similar experiences in the past. As well as a source of informal information, this also acted as a form of emotional support.
Local charities or support groups were also noted by participants. Rather than proactively search for these organisations, people reported finding out about them by chance, for example when walking past, through word of mouth or local advertising.
Case Study
A participant initially looked for emotional support from family members when caring for his mother, but some were distant and frustrated by his mother’s condition, which had worsened in the past year.
He looked to his local authority for professional support, and his GP for information on his mother’s condition, but not for information about supporting himself. He saw an advert for Age UK and called their helpline.
He uses the helpline once a month, both to explore what support is available for his mother and also to talk to someone that he feels understands his situation.
3.2.2 Online sources
As with offline sources, people in the early stage of their journey were pointed towards online information sources by other people, rather than proactively searching for this themselves. Lack of certainty about what they were looking for was another challenge to using online sources. People felt they did not have the time or energy to navigate the vast amounts of information available on the internet. Even when participants knew what they wanted to find, they felt it could be difficult to do so or to assess its legitimacy and accuracy. people defaulted towards sites that were well known or they trusted.
After working all day, it’s hard to motivate yourself [to search for information]. You could be looking for hours and not find what you’re looking for, then find it and second guess yourself as to whether it’s legitimate – Male, 52, Nottingham.
Sites such as the NHS and GOV.UK webpages were reported to be well known and trustworthy and used for information in the early stages of the journey. NHS webpages tended to be the first port of call for information on the recipient of care’s condition, whilst GOV.UK was used for information about financial or other support. People were familiar with the NHS and government. This familiarity, and the perceived legitimacy derived from being government bodies gave people confidence that the information would be accurate.
As with offline sources, people were also directed towards online sources through word of mouth, or through seeing a site advertised.
Participants went to the websites of condition specific charities, for example, Alzheimer’s Society, Age UK, MacMillan, Dementia UK. People reported liking the tailored information for the condition that the care recipient suffered from and clear guidance on what to expect when someone is experiencing that condition. It was also felt that these sites had an empathetic tone. Participants also reported that these sites were likely to offer emotional and practical support for the person providing care, as well as the care recipient. These sites also signposted to other sites offering wider support, such as financial advice.
Financial advice sites such as Money Saving Expert were used to understand what financial support might be available and participants were directed to them by word of mouth. People placed high levels of trust in Money Saving Expert and recognised the website’s founder, Martin Lewis, as a well-respected financial expert. They felt the site was on the side of the individual, providing useful advice in interactions with government and financial institutions. This trust extended to feeling that it is on the side of people providing care, providing information they may otherwise find it difficult to access. Participants were signposted to these sites from other online sources or through word of mouth.
My friend sent me to Martin Lewis Money Saving Expert and it said that ‘you’re living with dementia, you might not have to pay council tax’. How is my father [with dementia] supposed to find that [he doesn’t have to pay council tax] out [otherwise]? There’s a lot of information out there but it can be hard to find – Female, North West Focus Group.
Local Authority websites were seen as a useful way of accessing locally relevant information. This was important as participants reported many support services were provided locally or that provision, for example for professional care, was locally determined. However, participants also reported finding Local Authority websites were hard to navigate and contained outdated information or broken links. Participants also found that these sites adopted a functional tone, which made the content seem less warm and supportive.
People used social media sites such as Facebook to access support and informal information, such as joining groups that shared similar experiences of care activities. This allowed people to share concerns about their care recipient’s condition, as well as express experiences, and potentially frustrations, that they did not feel comfortable sharing with their immediate social circle or family.
The experiences participants relayed of using online and offline information sources shows that one source could not address all user needs, even if it contained all the relevant information. For example, whilst there is trust in Government websites participants also saw value in charities, which could offer specific advice on the condition the care recipient was experiencing and third party organisations perceived to act as advocates for individuals, such as Money Saving Expert.
3.3 How information needs changed over time
Within this sample identifying as a carer strongly influenced how people looked for information. Doing so moved them in to a space where they could look for, and access, support for themselves and this was the key change to information sought over time. Reflecting on this, participants described feeling frustrated that these networks and information had been invisible and inaccessible to them.
I didn’t see myself as a carer, so it’s almost impossible to look for things to help you with your situation – Female, London Focus Group.
It’s taken me three years to get to this point, now. I read this [carer’s] centre’s website in tears [as it made me realise I was not alone and could get support] – Female, London Focus Group.
After identifying as a carer, participants looked for information to support themselves: social networks and financial support. Interacting with other networks of carers helped participants to feel less isolated. These networks also opened them up to options such as volunteering and, with support from someone at the carer’s centre, looking for ways back in to the labour market.
When carers get together and start talking, that is when we learn new things – Female, East Midlands Focus Group.
Beyond enabling access to additional sources of information to support their own wellbeing, the information needs of those who had been providing care for a number of years were consistent with those of people in the earlier stages. They wanted information about the care recipient’s condition, particularly if this was progressive, or the support available could change. They also wanted access to information about external support, for example, childcare.
3.4 What did participants with more experience of providing care feel people should know at the outset?
People who had been providing care for a number of years were asked what advice they would give to working people in a similar position now.
Participants said they would have wanted to understand they were a ‘carer’ sooner because of the support it unlocked. This raises the question of how this information should be positioned so that people can be supported to access it sooner, regardless of whether they identify as a carer or not.
Participants also described wanting information and support to have been given to them proactively by others. They felt they needed someone to reach out and help them, as there were times that they needed help but were not aware or able to articulate their needs because they were so focused on providing support to their family member.
Participants also felt that they needed information on the financial support that they and/or the care recipient might be entitled to as early as possible. Participants reported that this was useful to help mitigate the financial challenges associated with providing care. For example, some participants with savings reported not looking for financial support initially, but in retrospect felt it was unfair that they spent their own savings when support could have been available. In addition, people unable to work due to providing care may be able to get National Insurance credits, which participants recognised as important for protecting their future eligibility for a State Pension.
Participants also felt that they would have wanted information on their employment rights as someone proving care activities, particularly entitlement to leave, or flexible working. This would help people to understand the options for combining work and caring. Participants felt that this knowledge could have opened up more options. As it was, there was a strong feeling amongst those who had left the labour market that at the time they had no choice but to leave their job due to their caring responsibilities. Amongst this group there were those who wondered whether they could have stayed in employment with the right support.
Being a carer can be a minefield… particularly around employment rights, there needs to be clear and concise information – Female, South West Focus Group.
My employer has suggested I cut my hours from 18 to 14 a week… I’m trying to progress my career but you get overlooked for certain tasks, trainings, promotions. I’m not sure what rights are there – Female, North West Focus Group.
Participants also felt it would have been valuable to know that they could access emotional and practical support, such as support networks for carers such as carers centres.
The problem is, when you first start caring, you’re expected to know things that you just don’t know. It needs to be basic where someone sits down with you and talks through everything at the very start [of caring for someone] – Female, North West Focus Group.
3.5 What support people further along the carer journey wanted when interviewed
Those further along the caring journey who were not in employment were keen to find information on how to re-enter the labour market but had low confidence about doing so. These participants worried about having to explain gaps in their work history, as they did not feel that caring was viewed positively or understood by employers. They also worried that their skills had become out of date, particularly those who had worked in sectors which required technical skills such as IT as they felt at risk of their skills becoming outdated quickly.
I’m finding it very difficult to find work. Leaving jobs [to care] and having gaps in employment doesn’t look good on my CV – Female, North West Focus Group.
Those further along their caring journey also reported that they needed more support for their own health. They felt that providing care placed a great physical, mental and emotional strain on them but it was difficult to make sure their own wellbeing was considered. This was even though they recognised that not doing so could cause more problems in the long term as, if they were unable to provide care someone else would need to do so.
I think there needs to be information and support for carers to look after themselves. If the carer’s health suffers, then the person they’re caring for suffers… if the carer can’t work [due to ill health], then you run out of money and more and more problem arise – Female, North West Focus Group.
4. Implications for the improvement of information
This chapter outlines implications emerging from the research about how information for people providing care, particularly those in the early stages of doing so, can be improved.
4.1 Implications
Proactively supply information to support the needs of people providing care
Participants were primarily focused on supporting the care recipient’s needs and did not report proactively seeking information about their own wellbeing or employment either online and offline. However, participants who had been providing care for longer reported that, in hindsight, they wanted to have accessed information to support their wellbeing sooner. To do so, participants felt they would have needed to be either proactively given information or encouraged to consider their own needs by touchpoints in the caring journey, such as nurses and doctors, including GPs.
Make more use of offline sources to reach those providing care and signpost to further information online.
Participants discussed regularly interacting with offline sources such as GPs and hospitals in the course of providing care. Leaflets and posters in GP practice and hospital waiting areas were reported as being particularly helpful sources of information. As participants were there regularly in their role providing care the information would be in the right context for them to engage with it. These forms of communication were seen as a helpful way of raising awareness of the type of support available.
I just happened to see a leaflet at the GP that said, ‘are you a carer’. I thought ‘no’, but then I read it and thought, I do all of what’s being said here – Female, London Focus Group.
One example of this working successfully was carers centres directing people to online resources. Participants felt that they had more trust and certainty in these sources when they had been directed there by the carer’s centre. Ideally, people would experience this signposting earlier on in their experiences of providing care.
Target carers more explicitly through online sources in the care recipients’ journey.
Participants reported accessing websites about the care recipients’ condition and needs, for example, those with a defined condition would look to condition specific charity websites or to GOV.UK for the support available for them.
These websites could more explicitly reference the individual providing care and help signpost them to information about support for themselves.
Design information for time-poor users and make it easier to process.
Participants reported that providing unpaid care affected the time they had to seek out and process information. Ensuring information is clear, concise and easy to navigate may help make information easier to process.
Participants also reported finding it hard to take in lots of information at once, and recognised that one site may not be able to meet all of their information needs, so preferred to be signposted to further information that could be accessed in their own time.
Ease of navigation and clear structure were seen to make online information more easily accessible for people who were emotionally and mentally fatigued, which participants felt they were. Website designs that presented a large volume of text were seen as intimidating and overwhelming. A design that presented clear headings with further information in a dropdown, and condensed material into bitesize amounts was preferred. This allowed people to see the information they wished to see, whilst avoiding material they did not, such as information relating to the recipient of care’s condition that they might find upsetting.
You get a bit overwhelmed sometimes looking (online). It’s a wall of black text and your brain is tired after work. You want it to be short and snappy, not reading a novel – Male, 51, London.
Participants also expressed a preference for simple and easy to understand language. They were navigating unfamiliar territory in terms of both their relative’s condition and the social care system both of which came with technical language. The easier language used in online sources is to understand, the easier it will be to process the information.
Better utilise the role that the most trusted and well known information sources could play.
Participants expressed concerns about the legitimacy and accuracy of some online information. To address this barrier to engaging with information, better utilising the most trusted and well known sources to provide or signpost to other useful information could increase the legitimacy of web sources that individuals had not come across before. Participants reported high levels of trust in sites such as NHS webpages, GOV.UK and charities that felt familiar to them and were therefore given a high degree of legitimacy quickly.
Use a warm tone when providing information to make it more engaging.
Participants wanted the language used to be warm and reassuring, demonstrating understanding for the reader’s circumstances and that they might be afraid, uncertain or isolated. Participants noted that sites which used cold language appeared unsympathetic to the needs of those using it. Participants reported they were likely to continue reading sites which demonstrated greater understanding for their circumstances.
I think the language needs to be softened a bit. Maybe that was just my mood at the time, but it will be a difficult time for people when they’re searching for this – Male, 52, Nottingham.
Charities such as Alzheimer’s, Age UK, and MacMillan, they provide a lot of help and I often direct other carers to these places… they’re very friendly and easy to understand – Male, East Midlands Focus Group.
Emphasise the value of proactively considering their own long-term needs and options.
Those providing care were focussed on the immediate needs of the care recipient, to the extent that there were reports of feeling guilty for considering their own needs. More content could attempt to reassure carers of the importance of considering their own wellbeing and emphasise the value of thinking about their own needs future, explaining potential prospects over the long term, to help carers recognise and weigh options that would be in the better long term interest of both them and the cared-for. People providing care could benefit from initiatives to stimulate thinking around the decisions that will impact their future, such as potential implications of staying in employment, or the value of seeking support for themselves through local networks.
Conclusions
One of the primary aims of this research was to identify how participants made decisions about meeting the care needs of their family member(s). This research found that participants experienced their initiation of caring activities as an instinctive response to a change in circumstances, rather than as an active, deliberated decision.
At the outset of their journey, participants were primarily looking for information about their family member’s health condition, rather than support for themselves. This focus continued throughout the caring journeys of participants in this research. Those with more experience of providing care also reported that decisions they made were often reactive rather than proactive including in relation to combining work and care. Whilst people did not feel they were making an active decision, their actions did have long term consequences which were not anticipated or considered at the time. This provides some support for the hypothesis that people are making decisions in the earlier stages of providing care which have long-term consequences.
As time progressed, the intensity of the care experience could also increase. This was affected by several themes including changes to the level of care required, employment pressure, financial pressures and other family responsibilities. When this occurred, participants found combining care and work more of a challenge. Participants who left the labour market reported that this was provoked by reaching a ‘stress peak’ in their journey, where work and providing care no longer felt sustainable. Those who received support before reaching a crisis point were better able to combine work and care. This suggests that reaching those providing care earlier could lead to them being provided with support for themselves sooner, helping them to make informed decisions about work. In retrospect, later stage carers wished they had known more about their employment rights and the financial and practical support available to them.
When participants were under pressure and stress they reported being more proactive about seeking some form of help. Participants who sought out financial support as a direct or indirect response to taking up the caring activities discussed being made aware of Carer’s Allowance and Attendance Allowance sooner. Recognising that they matched the descriptions enabled people to get help. In cases where people did not have a trigger to self-identify as a carer it took someone else, a friend or a doctor, telling them this and helping them get support.
Participants who had identified as a carer, found that this meant they were then able to access information and support for themselves. Identifying as a carer also helped these participants to feel less isolated. At present, identifying as a carer is important to access support. However, this raises the question of whether people should change to access support, or whether the information and support should be better tailored to reach all people providing care, regardless of whether or not they identify as a carer.
The use of online information was limited amongst those in the early stages of caring. In part this was due to a lack of time. Participants were also unsure of what they needed to look for: their questions at this stage felt broad and more suited to exploring through offline than searching for specific queries through online channels. This was the case even amongst those more digitally confident.
Examples of offline sources used were GPs and hospitals, friends and family and local organisations. GPs and hospitals in particular were a common touchpoint for people providing care as they were regularly visiting these places with the care recipient.
Although offline information sources were preferred, online sources were used and seen as helpful. The NHS website, for example, was used to learn more about their family member’s condition; GOV.UK was used to learn about the financial support available and charities were a key information source, particularly for those whose family member had a specific condition. Charity websites dedicated to a condition were found to be more likely to have information for people providing support to a family member. Those caring for a family member with a less common condition or no specific diagnosed condition could be less likely to receive support as they didn’t reach these channels of information.
Evidence suggests that to make sure information reaches those providing care, it should be provided proactively, as participants were unlikely to seek this information themselves. This could be achieved by targeting people through gateways such as hospitals, GPs, pharmacies and on financial support websites. Participants also cited the importance of trust and legitimacy in online sources. Given how time-poor this group are, sites being clearly structured and early to navigate will help encourage use and support retention of information by those using them. This outcome could also be supported by making sure information is up-to-date, has a warm tone and is concise.
Lack of information seeking presents a challenge to providing support to this group with information about employment choices. However, feelings of isolation, financial difficulty and loss of identity were exacerbated amongst those who had left work, and there was a strong desire amongst this group to return to the labour market. This suggests that better and earlier support with decision making around combining work and care would be welcomed by this group and could help lead to better outcomes for those providing care.
The findings from this research suggest the following implications for information providers:
- Proactively supply information to support the needs of people providing unpaid care
- Make use of offline sources to reach those providing care and signpost to further information online
- Target carers more explicitly through online sources in the care recipients’ journey
- Design information for time-poor users and make it easier to process
- Make more use of the most trusted and well known information sources
- Use a warm tone when providing information to make it more engaging
- Emphasise the value of proactively considering their own long-term needs and options
Appendix A: Pre-task issued before interviews
DWP Carer’s Information User Testing Pre-task
Dear Sir / Madam,
Thanks again for agreeing to take part in this research for the Department of Work and Pensions (DWP).
DWP have asked us (Ipsos MORI) to speak to people who have recently learned (in the last ten months) that a family member’s illness, disability or old age means they need or will need support with everyday life, and are providing or considering how to provide that support. DWP have asked us to conduct this research because they want to understand how they can better support people in this situation.
As part of this research, we would really appreciate it if you could complete this pre-task. As a thank you for your time, you will be given £10 to complete this task. This is in addition to the £50 for taking part in the face to face interview and £30 if you take part in a follow-up telephone interview.
Any information that you provide us in this pre-task and the two interviews will be treated as strictly confidential and all data will be anonymised. No identifiable information will be passed back to DWP and any relationship you have with DWP will not be impacted in any way. If you would like, I can send you Ipsos MORI’s privacy policy which goes into more detail about your data rights. Alternatively, you can contact Yasmin White at Ipsos MORI on [Number redacted].
The pre-task
For this task, we would like you to think back to the point when you first became aware that your family member would need help and support with day to day activities, and write down key changes that have happened since then. These might include any life event or change in circumstance which relates to the news about your family member. Some examples of these key events are outlined below:
- Any changes in how much you support your family member or the types of things you support them with
- Any changes in your thoughts about how you intend to support your family member.
- Any changes to your family member’s health / condition
- A change in job / number of hours you work to accommodate the support you need to / will need to give to your family member
- Moving house to allow you to better support your family member e.g. moving closer to them
Please use the table below to note these key points. Each page asks about a different time period, because we want to understand how things have changed for you over time. Please fill in the boxes that correspond with the time you learnt that your family member would need support. If you learnt that they would need support prior to January 2018, please still use the first box but make it clear when you became aware that your family member would need help. There are also boxes asking about how you were feeling at the time, where you went for information and what you most wanted to find out. This is because we are interested in how this affected your approach to thinking about how your family member could be supported. We understand that some of this information will be personal, so please only write what you are comfortable sharing with us. You can treat this as an exercise in remembering the key points since you learned they would need support. We will want to explore these questions in more detail in the interview, so any notes you can provide now will be helpful prompts for discussion.
Please feel free to take as much time as you like completing this task. During the interview, please have this task to hand – if you do not have a printer, please write down your responses on a separate sheet of paper.
| January to May 2018 | |
|---|---|
| Key events / changes in circumstance for you and your family | |
| How did you feel at this time? (please only share what you are comfortable with sharing) | |
| If you were looking for information, where did go and what did you most want to find out? (In particular, please name any online sources / websites you looked at) |
| June to September 2018 | |
|---|---|
| Key events / changes in circumstance for you and your family | |
| How did you feel at this time? (please only share what you are comfortable with sharing) | |
| If you were looking for information, where did go and what did you most want to find out? (In particular, please name any online sources / websites you looked at) |
| October 2018 - present | |
|---|---|
| Key events / changes in circumstance for you and your family | |
| How did you feel at this time? (please only share what you are comfortable with sharing) | |
| If you were looking for information, where did go and what did you most want to find out? (In particular, please name any online sources / websites you looked at) |
Appendix B: Interview topic guide
Carers Information User Testing Discussion Guide
Note:
- ‘Carers’ and ‘key decisions’ are referred to throughout as short-hand. Moderators will reflect the language used by participants
- Researchers must use the discussion guide as a guide only – not all questions or prompts will necessarily be used during the interview
For moderator only:
Background
Ipsos MORI have been commissioned by DWP to assess the extent to which working people facing decisions about someone else’s care have access to information that can help them to make decisions, specifically decisions around work.
Becoming a carer is a significant decision which can impact the individual’s current and future circumstances, particularly in relation to work. It is also a decision that is made at a time when emotions are likely to be heightened, which may impact on the ability to seek out or assimilate the information to make an informed decision. We want to explore how participants’ describe their cognition and thought processes when making these decisions, and how their situation affects how they seek and engage with information.
DWP want potential and current carers to be fully aware of the different options available to them, and the implications of the decisions that they make. The aim is for working people to have access to the right information, set out in the simplest way to help them understand and visualise the journey they and the person they care for are embarking on and their options along the way. This will help them be aware of and understand the full range of issues which they may need to consider and navigate and the key decision points.
Overview of the research
As part of this research, we will be undertaking 15 face to face interviews. Ten participants will be invited to take part in a follow-up telephone interviews around 10 – 14 days later. One week before the first interview participants will be given the opportunity to complete a short diary exercise. This will either be completed on paper or in the Ipsos MORI app.
The initial face to face interview will last 60 mins, with the follow-up lasting 30 minutes. Individuals will be offered £10 for completing the diary exercise, £50 for taking part in the first face to face interview and £30 for the follow-up telephone interview.
Key points
- There is substantial ambiguity in the use of the term ‘carer’ and what it consists of. As such, the participant may or may not view themselves as a ‘carer’ even if they are undertaking activities that one might consider to be care. Others may or may not be a carer currently undertaking those activities, but may be considering them without thinking of it as ‘care’
- The participant will have learned about a family members’ needs changing in the past 10 months
- We must encourage the conversation to be primarily focused on themselves and their thoughts / considerations / influences/decision-making process rather than about the person receiving care, although the views and preferences of the person receiving care may be relevant if they had a strong bearing on the participant
- Key decisions that are referred to must have occurred in the past 10 months, unless providing context
- Seek to establish a timeline for how they have been thinking about these needs, and how they be could be supported. It is important to understand their thought process in their own terms with regards to any circumstances, decisions or anything else that participants feel have affected how they have been considering those care needs
- Some points throughout the conversation may be highly sensitive
Discussion guide
1. Introduction: 2-3 mins
Orientates interviewee, prepares them to take part in the interview. Outlines the ‘rules’ of the interview (including those we are required to tell them about under MRS and GDPR guidelines).
Thank participant for taking part.
Introduce self, Ipsos MORI: independent research organisation (i.e. independent of Government), we adhere to Market Research Society code of conduct that ensures our research is carried out in an ethical and professional manner.
Introduce research and topic – the Department for Work and Pensions (DWP) has commissioned Ipsos MORI to conduct research with people who currently / are considering supporting a family member with their health, welfare and protection, due to an illness, disability or incapacity which prevents them from independently maintaining their own wellbeing. The aim of the research is to understand what information is available to you to help you make decisions about how to support this person and specifically about the impact this may have on your work and how this could be improved.
Confidentiality – reassure all responses are anonymous and that identifiable information about them will not be passed on to anyone, including back to DWP or any other Government department. Remind them that their participation in this research is completely voluntary and they are able to stop at any point or move on from a question. Also, reassure participants that taking part will not affect their relationship with DWP, nor their benefits.
Interviews should take around 60 minutes. As a thank you for taking part they will be given a £50 incentive.
Ask for permission to digitally record – transcribe for quotes, no detailed attribution.
Any questions before we begin?
2. Background: 5 mins
Provides contextual background information about the participant and their work life.
Moderator explain: To start off with, I’d like to learn a little bit about you
Can you tell me a bit about yourself?
- Can you tell me a little bit about your home life and where you are currently living? Probe around who else is at home; how long they’ve lived there for
- What does a typical day look like for you? Any hobbies or interests?
- Can you tell me a little about your current work? Probe around: role (description); hours worked / shifts; length of time working there; company size; office based / not
- How good would you say you are with searching for information online? Do you regularly use online sources to find out information?
- Do you tend to trust online sources? Which websites are you most / least likely to trust?
3. Care circumstances: 5 - 10 mins
This section explores their care situation. Note to researchers: Use the screener information to gage their current situation and use that as a starting point. If they are caring for more than one person who fits the criteria, shape the interview accordingly. Reflect their own language in yours e.g. whether they term themselves as a carer, whether they are or aren’t currently caring for them.
Moderator explain: Now we are going to move on and talk about how you currently / might support your family member and speak about the family member that you support. If you support more than one person, please tell me about the person who you started supporting in the last 10 months. [If you started supporting more than one person in the last 10 months, please tell me about the person you support/expect to support the most].
Could you tell me a little bit more about how you support [your family member] / will support your family member? Probe around: their role, their relationship; where they live – how far away from the recipient of care; what the journey is like to get to them if not living together;
-
Are you receiving/seeking any form of support? What does this look like? Probe around support from friends, family, local carer centre
-
Can you now tell me a little bit more about their condition and their current care needs? (IF NECESSARY: Reassure participants that they do not have to answer any questions that they feel uncomfortable with) Probe to understand condition; whether this happened suddenly / gradually; how long ago they started developing
-
How do you think their care needs might change in the future? Over what sort of timescale?
What other support are they currently receiving? Probe around who provides this; what with (tasks / activities); frequency; what the participant’s role is
4. Key decisions 15 - 20 mins
This section will be used to understand their caring journey. Every interview is unique so it is important to use language that reflects their circumstance e.g. whether they are or aren’t currently caring for the individual.
Now I’d like to understand the journey you have been through from the point when you learned that this person will need support, up to now – reflecting on how you were thinking about any choices/options you had around your role / how this might have changed, and what you wanted to know
Use timeline to establish key points in their journey and how this made them feel
i) The point where you realised the individual would need support
When did you start thinking about their care needs and how they would need to be met?
- How did you feel?
- What was going through your mind at the time? Probe: did they have any uncertainties or questions?
- How much control did you feel you had over your options/situation?
- Was anyone else involved in discussions/making decisions about your family member’s care needs?
- What choices or options did you feel you had in relation to how to meet their care needs? How did you find out about them?
Explore spontaneously then probe around:
- Meeting their needs myself
- Apply for support from my Local authority
- Pay for care and support services directly
- Get help from friends and other family members
-
Combinations of the above
- For each raised explore:
- How did you find out about these?
- Which options felt more / less realistic? Why was that?
- If participant doesn’t feel that they had options, probe around why this was.
- How did you weigh up the different options? What different factors did you consider? What was top of mind?
Probe:
- Sense of duty, responsibility
- Nature of relationship
- Cared for person’s preferences/expectations
- Expectations or pressures from other family members
- Quality of external care
- Availability of external care
- Cost/funding considerations
- Impact on work
- Impact on home life
- Potential impact on other dependents
ii) Changes since you realised they would need support
- What has changed since you realised that they would need support? [Refer to journey mapping task if they have completed this] Probe: changes to care needs / level of support – when and why this happened, have the changes been gradual or rapid?
- Have you made any changes to your own life to accommodate these changes? Probe: how does this make them feel?
- Have you spoken with your employer about your situation at any point? Why /not? What was the outcome of this conversation?
- Does your employer supply any useful information?
- What are their policies on flexible working more generally?
iii) How you expect your circumstances to change in the future
Are there any further changes you expect to happen / decisions you will be making in the near future? Probe: what will this involve? Who will be involved? How do they feel about these changes? What questions / uncertainties do they have now? What information are they in need of?
N.B. The above points should establish how the participant describes the significant factors that have had bearing on the considerations they have had to make so far in their caring journey. Refer to these key points throughout the rest of the interview.
5. Online information: 20 mins
This section explores the extent to which they have used online information to make care decisions and how useful it was.
Since learning that [your family member] would need support, what questions / queries have you had?
- Prompt if necessary: how to make sure the family member gets the care they need, what support services are available, how to combine caring and working etc.
- Did you try to find information to resolve these questions?
[For each question/issue, or their top two/three is there are many] where did you go for information – who did you speak to and which sources did you consult? Include online and offline sources, and informal sources e.g. friends and family, other carers, social media networks , local authority, charities, the library, carers associations, employers
- Why did you go to these sources?
- How useful did you find this information? Did you find what you needed?
- What is it that you liked or did not like about it?
- Have you used it in combination with the online sources? Why?
Moderator explain: Now we are going to focus on the online sources that you have used for information about supporting someone / caring for them.
Do you remember what online sources you used? Probe for specific names / sites. Refer to diary to explore recent sources.
For each recalled example explore:
- What was the content about? Probe: did the website contain information about the recipient of care or the person providing / potentially providing care? Do you remember any messaging about work and care?
- How did you come across this particular site? What about it appealed to you? Probe: had a particular site been mentioned to them by anyone else?
- Had you used this site before? Do you still use it?
- How did you identify the content as being relevant to you?
- To what extent did it answer your questions?
- Was any information more / less useful? Probe around: what made a site more or less useful compared to others?
- What were the positives? And the negatives? Probe around: language, tone, method of displaying information (video, text etc.), colours, ease of identifying it as being relevant them, organisation running the website, national versus regional information, general versus tailored information
- How did this content make you feel? And about work specifically?
- How credible did the site feel?
Has anything changed over time in the type of information you look for or which you find helpful?
6. Improvements to online information: 5-10 mins
This section explores whether participants feel that the online information available on caring could be improved.
Moderator explain: Finally, we’re going to talk about what improvements you think could be made to online information
What, if any, changes would make information online more useful for you? Probe around:
- Format: video, forums, images, text, checklists, ability to print
- Tone and language
- General information (for all carers) or tailored to their circumstances (e.g. caring for someone with a particular condition)
- National vs regional information
- Information bring brought together in one place?
- Messenger e.g. charity, government, peers on a support forum etc.
Is there anything online sources could learn from offline sources?
Which organisations or individuals do you think are best placed to signpost people to/make them aware of online information? Probe around: JCP, NHS staff, Local Authorities, etc.
What do you think could be done to make it easier for people to access information on caring for / supporting a person and working? Probe: explore any barriers that they have mentioned previously.
7. Summing up: 5 mins
Brings the conversation to a close, and allows participant time to mention anything that has not already been covered.
Moderator explain: Thank participant for their time and explain we are coming to the end of the interview and I have a few final questions before we finish.
Is there anything that we haven’t discussed that you would like to raise?
Overall, what do you think is the one thing I should take away from the discussion today?
Thank and reiterate confidentiality. Incentives = a “thank you” from Ipsos MORI for their time and contribution
- £50 – face to face interview
- £10 – if they have done the diary
- £30 – if / when they take part in the follow up interview
Identify whether they have agreed to take part in the follow up interview and confirm status.
Appendix C: Follow up interview topic guide
Carers Information User Testing Follow-Up Discussion Guide
Note: - ‘Carers’ and ‘key decisions’ are referred to throughout as short-hand. Moderators will reflect the language used by participants. - Researchers use the discussion guide as a guide only – not all questions or prompts will necessarily be used during the interview.
For moderator only:
Background
Ipsos MORI have been commissioned by DWP to assess the extent to which working people facing decisions about someone else’s care have access to information that can help them to make decisions, specifically decisions around work.
Becoming a carer is a significant decision which can impact the individual’s current and future circumstances, particularly in relation to work. It is also a decision that is made at a time when emotions are likely to be heightened, which may impact on the ability to seek out or assimilate the information to make an informed decision. We want to explore how participants’ describe their cognition and thought processes when making these decisions, and how their situation affects how they seek and engage with information
DWP want potential and current carers to be fully aware of the different options available to them, and the implications of the decisions that they make. The aim is for working people to have access to the right information, set out in the simplest way to help them understand and visualise the journey they and the person they care for are embarking on and their options along the way. This will help them be aware of and understand the full range of issues which they may need to consider and navigate and the key decision points.
Overview of the research
As part of this research, we will be undertaking 15 face to face interviews. Ten participants will be invited to take part in a follow-up telephone interviews around 10 – 14 days later. One week before the first interview participants will be given the opportunity to complete a short diary exercise. This will either be completed on paper or in the Ipsos MORI app.
The initial face to face interview will last 60 mins, with the follow-up lasting 30 minutes. Individuals will be offered £10 for completing the diary exercise, £50 for taking part in the first face to face interview and £30 for the follow-up telephone interview.
Key points
- There is substantial ambiguity in the use of the term ‘carer’ and what it consists of. As such, the participant may or may not view themselves as a ‘carer’ even if they are undertaking activities that one might consider to be care. Others may or may not be a carer currently undertaking those activities, but may be considering them without thinking of it as ‘care’.
- The participant will have learned about a family members’ needs changing in the past 10 months
- We must encourage the conversation to be primarily focused on themselves and their thoughts / considerations / influences/decision-making process rather than about the person receiving care, although the views and preferences of the person receiving care may be relevant if they had a strong bearing on the participant
- Key decisions that are referred to must have occurred in the past 10 months, unless providing context
- Seek to establish a timeline for how they have been thinking about these needs, and how they be could be supported. It is important to understand their thought process in their own terms with regards to any circumstances, decisions or anything else that participants feel have affected how they have been considering those care needs
- Some points throughout the conversation may be highly sensitive
Discussion guide
8. Introduction: 2-3 mins
Orientates interviewee, prepares them to take part in the interview. Outlines the ‘rules’ of the interview (including those we are required to tell them about under MRS and GDPR guidelines).
Thank participant for taking part.
Briefly re-cap as participant will have heard previously.
Introduce self, Ipsos MORI: independent research organisation (i.e. independent of Government), we adhere to Market Research Society code of conduct that ensures our research is carried out in an ethical and professional manner.
Introduce research and topic – the Department for Work and Pensions (DWP) has commissioned Ipsos MORI to conduct research with people who currently / are considering supporting a family member with their health, welfare and protection, due to an illness, disability or incapacity which prevents them from independently maintaining their own wellbeing. The aim of the research is to understand what information is available to you to help you make decisions about how to support this person and specifically about the impact this may have on your work and how this could be improved.
Confidentiality – reassure all responses are anonymous and that identifiable information about them will not be passed on to anyone, including back to DWP or any other Government department. Remind them that their participation in this research is completely voluntary and they are able to stop at any point or move on from a question. Also, reassure participants that taking part will not affect their relationship with DWP, nor their benefits.
Interviews should take around 30 minutes. As a thank you for taking part they will be given a £30 incentive.
Ask for permission to digitally record – transcribe for quotes, no detailed attribution.
Any questions before we begin?
9. Background: 5 mins
Warms participant up to conversation.
Note to moderator: Briefly catch-up with participant, use the below as a guide, but tailor conversation to what you had spoken about previously.
To start with, do you want to tell me a little bit about what you’ve been up to since we last spoke?
- How have you been?
- How is your family?
10. Follow-up: 25 mins
This section will explore what they have experienced since the first interview, if their information needs have changed and if they have sought any information.
Moderator explain: Now we are going to move on and talk about what has happened since we last spoke in relation to your caring situation.
Since we last spoke, has anything changed?
Probe: in their own personal life, with the family member they are caring for / their condition
How has work been?
- Has considering the care needs of [family member] affected you at work in any way?
- Have there been any changes in how you manage working and caring?
And since we had our conversation, do you feel differently about anything that we spoke about last time?
- Is there anything you have thought about since that you didn’t mention at the time?
- Have you had any new questions / uncertainties, in relation to [family member] since we last spoke?
- What about? Probe: their family member’s condition, support for the family member, support for themselves – physical, financial or psychological? Combining working and care
- What do you think led you to think about that?
Have you looked at/sought any information since our conversation? (N.B. this may or may not relate to their response to the last question – capture all instances)
- Where did you find this? Probe: online or offline? Why? Was this a new source or something they knew about before?
- What led you to that source?
- Was it useful?
- To what extent did you find what you were looking for?
- What did/didn’t you like about the source?
- Are you still looking for information on this? Where are you planning to look?
- Did it prompt any new/other thoughts? What are these?
Scenarios
As you may be aware, we have been speaking to lots of people in the same position as you. In our conversations, we’ve heard some different things and we wanted to explore how much they do or don’t resonate with you. If you don’t feel comfortable answering or if you simply feel this does not relate to you then we can simply move on to the next question:
1. Some people have mentioned that caring for /supporting someone can change the dynamic in their family
a. is this something you have experienced?
b. how has it affected you?
c. has it affected how you feel about work? And over the longer term?
2. Some people have mentioned that caring for someone means they need a lot of flexibility, for example to leave work at short notice or to attend appointments.
a. is this something you have experienced?
b. could you tell me more?
c. has it affected how you feel about work? Over the longer term?
3. Some people have mentioned that it can become harder to concentrate at work when a close family member is unwell or needs care/support.
a. is this something you have experienced?
b. could you tell me more?
c. what impact could this have on how you feel about work?
4. Some people have mentioned that they find combining everything in their life e.g. family, care responsibilities, work difficult
a. is this something you have experienced?
b. can you tell me more?
c. what impact could this have on how people feel about work?
When we last spoke, I asked you if you thought that online information could be improved in any way to help people like you who have recently started considering / providing someone’s care needs.
Since then, do you think anything else could be done to make it easier for people to find information on caring/ supporting a person and working? Probe: explore any barriers that they have mentioned previously.
And, have you had any more thoughts about ways in which you feel this information could be improved?
Probe around:
- Accessing information:
- How to find information
- How to know it’s relevant for you
- Content:
- Decisions and considerations
- General information (for all carers) or tailored to their circumstances (e.g. caring for someone with a particular condition)
- National vs regional information
- Information bring brought together in one place?
- Tone and language
- Messenger e.g. charity, government, peers on a support forum etc. anything online sources could learn from offline sources?
- Format:
- video, forums, images, text, checklists, ability to print
Are there any other forms of support that you feel are needed for people in your position?
11. Summing up: 2 mins
Brings the conversation to a close, and allows participant time to mention anything that has not already been covered.
Moderator explain: Thank participant for their time and explain we are coming to the end of the interview and I have a few final questions before we finish.
If there is one thing that I could take away from our conversations that could be fed back for this research, what would it be?
Is there anything that we haven’t discussed that you would like to raise?
Moderator explain: Thank participant for their time and explain we are coming to the end of the interview and I have a few final questions before we finish. If there is one thing that I could take away from our conversations that could be fed back for this research, what would it be?
Is there anything that we haven’t discussed that you would like to raise?
Thank and reiterate confidentiality. Incentives = a “thank you” from Ipsos MORI for their time and contribution (£30)
Provide them with the advice sheet if they haven’t been given it already.
Appendix D: Pre-task issued before focus groups
DWP Local Carer Centre Engagement Pre-task
Dear Sir / Madam,
Thanks again for agreeing to take part in this research for the Department of Work and Pensions (DWP). We are looking forward to speaking to you at the focus group.
As part of this research, we would really appreciate it if you could complete this pre-task.
Over the page there are 3 questions that we would like you to think about before coming to the group. You need not write anything down if you don’t have the time but please bring your thoughts / written ideas with you on the day. But feel free to capture as many thoughts as you like – it needn’t be just one of each.
1. Is there any information about caring you know now that would have been useful for you to know sooner – i.e. when your family member first started to need support?
2. Why would it have been helpful to know this?
3. What do you think the barriers were, if any, to you being able to find this information earlier?
Appendix E: Focus group topic guide
Local Carer Centre Engagement Focus Group Topic Guide
For moderator only:
1. This guide indicates the areas to be covered in the discussion, the likely order in which topics will be covered and the kinds of questions and techniques that may be used. As it is qualitative research there will be diversions taken within the dynamics of each interview in order to fully explore respondents’ perspectives. Timings are given for guidance only and will not be strictly adhered to – times spent on each section will be dependent upon the knowledge/ interests of each group.
2. The objectives of the research may be addressed through direction questioning, indirect questioning, observation of non-verbal response in response to stimulus or analysis of data post hoc.
Background
Ipsos MORI have been commissioned by DWP to assess the extent to which working people facing decisions about someone else’s care have access to information that can help them to make decisions.
Becoming a carer is a significant decision which can impact the individual’s current and future circumstances, particularly in relation to work. It is also a decision that is made at a time when emotions are likely to be heightened, which may impact on the ability to seek out or assimilate the information to make an informed decision. We want to explore how participants’ describe their cognition and thought processes when making these decisions, and how their situation affects how they seek and engage with information
DWP want potential and current carers to be fully aware of the different options available to them, and the implications of the decisions that they make. The aim is for working people to have access to the right information, set out in the simplest way to help them understand and visualise the journey they and the person they care for are embarking on and their options along the way. This will help them be aware of and understand the full range of issues which they may need to consider and navigate and the key decision points.
Overview of the research
As part of this research, we will be undertaking 4 focus groups, with between 6-8 people within each group. The groups will last for 90 minutes and participants will be offered £40 for taking part.
Key points
- There is substantial ambiguity in the use of the term ‘carer’ and what it consists of. As such, the participant may or may not view themselves as a ‘carer’ even if they are undertaking activities that one might consider to be care.
- The participant will have been caring for a family member for 1-3 years.
- Some points throughout the conversation may be highly sensitive
Discussion guide
12. Introduction: 2-3 mins
Orientates interviewees, prepares them to take part in the group. Outlines the ‘rules’ of the group (including those we are required to tell them about under MRS and GDPR guidelines).
Thank participants for taking part.
Introduce self, Ipsos MORI: independent research organisation (i.e. independent of Government), we adhere to Market Research Society code of conduct that ensures our research is carried out in an ethical and professional manner.
Introduce research and topic – the Department for Work and Pensions (DWP) has commissioned Ipsos MORI to conduct research with people who have recent experience of caring for someone else and who were in work when they became a carer. The aim of the research is to understand your experiences as a working carer, including how you made decisions about what care activities to take on given you were in work, and what information would have been useful in helping you make those decisions.
Confidentiality - reassure all responses are anonymous and that identifiable information about them will not be passed on to anyone, including back to DWP or any other Government department. Remind them that their participation in this research is completely voluntary and they are able to stop at any point or move on from a question. Also, reassure participants that taking part will not affect their relationship with DWP, nor their benefits.
Explain – you are aware some of the topics will be fairly sensitive for them to discuss. They are free to contribute or not as they wish. However, to help address this we will be trying to keep the group focused on how information about caring can be improved, rather than focusing too much on their personal experiences.
Groups should take around 90 minutes. As a thank you for taking part they will be given a £40 incentive.
Ask for permission to digitally record – transcribe for quotes, no detailed attribution.
Any questions before we begin?
13. Pre-task / Background: 10 mins
Provides contextual background information about warms up participants.
Prior to starting, participants are asked to complete the screener. The pre-task that was given to participants before the focus group should be collected.
Moderator introduce self and explain: To start off with, I’d like to learn a little bit about each of you.
Can you all tell me your names and a little bit more about yourself?
- Probe: Name, who they live with, employment status, hobbies / interests
How long ago did you become a carer and who do you care for?
What job were you doing at the time you first started to look after the person you care for?
14. Initial experiences / considerations and decisions: 40 mins
This section explores their decision making, particularly in relation to work and care.
Moderator explain: Now we are going to move on and talk a little bit more about your experiences since becoming a carer and what information you have been looking for.
Could you tell us about what it was like for you becoming a carer?
- What led you to take on the caring role?
- What types of things were you considering?
- Was anyone else involved at this point? Probe: what conversations were you having? What was the outcome?
[If necessary: I understand it might be a difficult period to think back to so take your time and remember you don’t need to answer any questions you don’t want to]
Moderator: Prompt DWP to ask any follow up questions
Now, I’d like you to focus specifically on your work situation at the time when you first found out the person you care for would need care.
Can you all tell me a bit more about what your job meant to you at the time? E.g. financial impact, social contact/networks, identity etc.
- What was the impact on your work after you learned your family member would need support?
-
How did it make you feel about work?
- And as time passed, after the first few months, did caring impact on your work?
- Did working impact on caring?
- Did you expect this?
- What are the challenges of working and caring at the same time?
- How did you respond to these challenges?
- Are there benefits to working and caring?
- How, if at all, has your employment changed over time? Probe: left employment completely, reduced hours, changed job, work in same job but more flexibly etc.
- What prompted these changes?
- What do you know now that you didn’t before?
- Now thinking about the future, do you think your employment will change in any way?
Exercise:
- How would you sum up the challenges working people face when making decisions about caring?
- What are the main questions or uncertainties that working people in this situation might be asking/facing?
Moderator: Prompt DWP to ask any follow up questions
15. Information about caring and work: 40 mins
This section will be used to understand what information they have used and how they feel it could be improved.
[Show Grid A]
Now I’d like you to think a bit more broadly about the places you’ve got information and advice about caring from. That includes online or offline, and more formal sources such as government/Local authority helplines and websites, charities and carer centres, and your employer, as well as informal sources such as forums and blogs, social media, friends and colleagues.
- Looking at this grid, where were you looking to answer your key uncertainties/questions?
- Did you find what you were looking for?
- What have the best or most helpful sources of information been that you’ve found?
- What made them helpful?
- What have the worst or least helpful sources been?
- What made them particularly unhelpful?
[IF NOT MENTIONED PREVIOUSLY] Now thinking about online sources…
- What have the best or most useful online sources been and why?
- What have the worst or least useful online sources been and why?
We’re interested in what’s missing from information that’s on the internet.
What have been the hardest things to find out about online? Probe around work and care specifically.
Looking at this list of different topics [SHOW LIST A], which of these did you look for information on?
LIST A (add others if mentioned)
- Employment [FOCUS]
- Emotional
- Care and support provided by your Local authority
- Care and support that you have to pay for yourself
- Health issues
- Financial management
- Support for carers
- Employment rights
- Other
For each, probe:
- What questions did you have about this?
- Did the information have an impact on the decisions you made? What were these?
- How helpful was the information that you found on these topics?
- For which of these did you feel there was information lacking?
- Are any sorts of information that you wanted or needed to know about missing from this list?
- Which of these topic areas is most important for you?
- Which of these topics (if any) would you not expect to find information about online?
Moderator: Prompt DWP to ask any follow up questions
16. Summing up: 5 mins
Brings the conversation to a close, and allows participant time to mention anything that has not already been covered.
Moderator explain: Thank participant for their time and explain we are coming to the end of the interview and I have a few final questions before we finish.
Based on your experiences at the start of your caring journey, what piece of advice or information would you give to working people in this position now?
Lastly, if there is one thing that I could take away from our conversations today that could be fed back for this research about supporting working people to make the best decisions around caring and working, what would it be?
Thank and reiterate confidentiality. Incentives = a “thank you” from Ipsos MORI for their time and contribution (£40 voucher)
-
A full overview of all materials can be found in the Appendix ↩
-
Numbers total 15 except for in the ‘type of condition of care recipient’ row, because some participants had two or more types of condition. ↩
-
This is any condition which affects the senses e.g. deafness or blindness. ↩
-
Whilst this research does not contain direct responses from those at the ‘crisis’ stage, retrospective experiences relayed by those with more experience of providing care confirmed this journey. ↩
-
This presents an overview of the experience: not all participants went through each stage, nor did every individual experience each stage for the same amount of time. ↩
-
This is explored in more detail in chapter four. ↩
-
When referring to professional care, this includes formal care support including professional carers, care homes and day centres. ↩
-
The factor ‘Information’ is covered in detail in chapter four. ↩
