Tuberculosis (TB): action plan for England, 2021 to 2026
Updated 15 March 2023
Applies to England
The aim of the tuberculosis (TB) action plan 2021 to 2026 is to improve the prevention, detection and control of TB in England. The action plan will focus on the needs of those affected by TB and TB services while recognising the impact and learning of the coronavirus (COVID-19) pandemic.
The TB action plan will support a year-on-year reduction in TB incidence and in-UK TB transmission and enable the UK to meet its commitment to the World Health Organization (WHO) elimination targets by 2035.
Introduction
The priorities and actions outlined in this plan will provide the NHS, UK Health Security Agency (UKHSA), NHS England (NHSE), UKHSA regions, NHSE regional teams, integrated care systems (ICSs), integrated care boards (ICBs), primary care, local authorities and the third sector with the tools to reduce TB incidence in all our communities. Multi-stakeholder collaboration will be essential to the implementation of the action plan including support for staff and action on inequalities.
The TB action plan includes actions linked to the outcomes of the Collaborative TB Strategy for England 2015 to 2020, particularly the challenges and recommendations outlined in the TB strategy end of programme report.
Oversight of the TB action plan will be provided by UKHSA and NHSE through their governance structures. A review of the TB action plan regarding implementation, delivery and outcomes has been carried out in 2022 with stakeholders and partners, to enable appropriate amendments to improve the impact of the priorities and actions.
The review included an update of functions and responsibilities, relevant to TB, to align with the reforms of the public health system which took place in 2021 to 2022 and the establishment of NHS integrated care systems in 2022 in England.
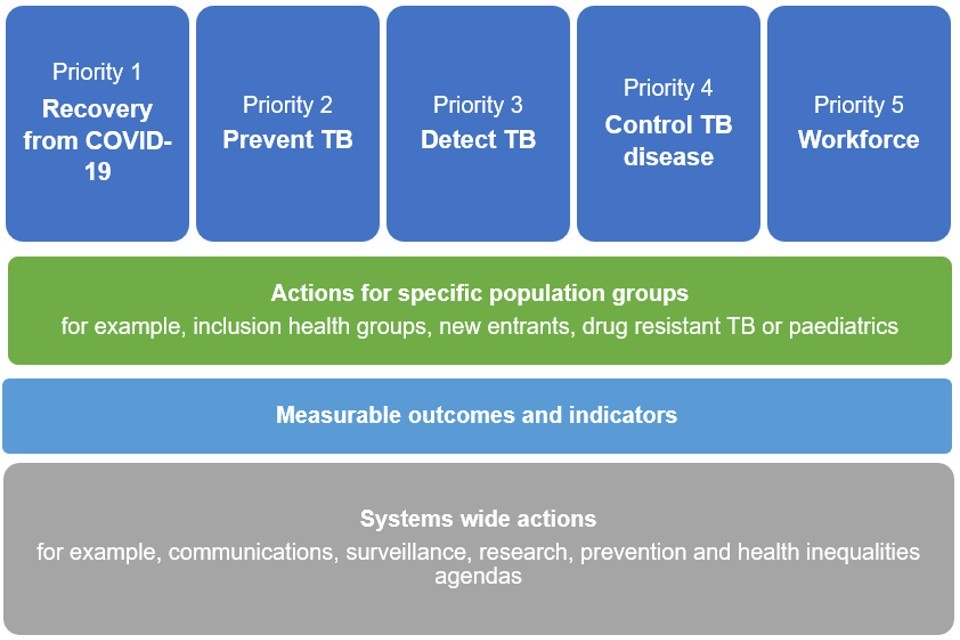
The 5 key priorities of the TB action plan are:
- Recovery from COVID-19
- Prevent TB
- Detect TB
- Control TB disease
- Workforce
These priorities are underpinned by:
- actions for specific population groups, that is, those with social risk factors, new entrants, people with drug resistant TB and children with TB
- measurable outcomes and indicators
- systems wide actions, that is, communications, surveillance, research and ensuring TB is included on prevention and health inequalities agendas
The recovery of services is priority one of the action plan due to the significant impact the COVID-19 pandemic has had on the detection, control and prevention of infectious diseases, including TB. For TB this includes missed diagnosis, delayed diagnosis, late presentation and delayed initiation of treatment. The probable effect will be to increase the pool of undetected and unreported cases of active disease and latent infection which is likely to contribute to increased morbidity and disease transmission.
Figure 1. Priorities for the TB action plan for England, 2021 to 2026: summary
It will be important, using a people-centred approach, to strengthen the patient pathway from the onset of symptoms or detection of infection, to prevent transmission, to utilise the latest technology, treatment and diagnostics, for example, whole genome sequencing (WGS).
A central tool to support the action plan is the national TB surveillance system which supports the monitoring of the prevention and control efforts in England and informs service improvement. UKHSA’s TB unit has been restructured to include new partnership posts working across UKHSA and the NHS and will work collaboratively with the UKHSA regions to deliver the action plan.
The incidence of TB has fallen significantly since 2011 with most new cases resulting from infection acquired outside the UK and approximately 25% of cases from transmission in England. However, in 2019 the rate of decline reversed, increasing by 2.4% and then, in 2020, recorded incidence fell. The significant impact of the COVID-19 pandemic will require continued monitoring of TB notifications and the outcomes of those affected by TB.
Figure 2. Number of TB notifications and rates, England, 1971 to 2020 (provisional data)
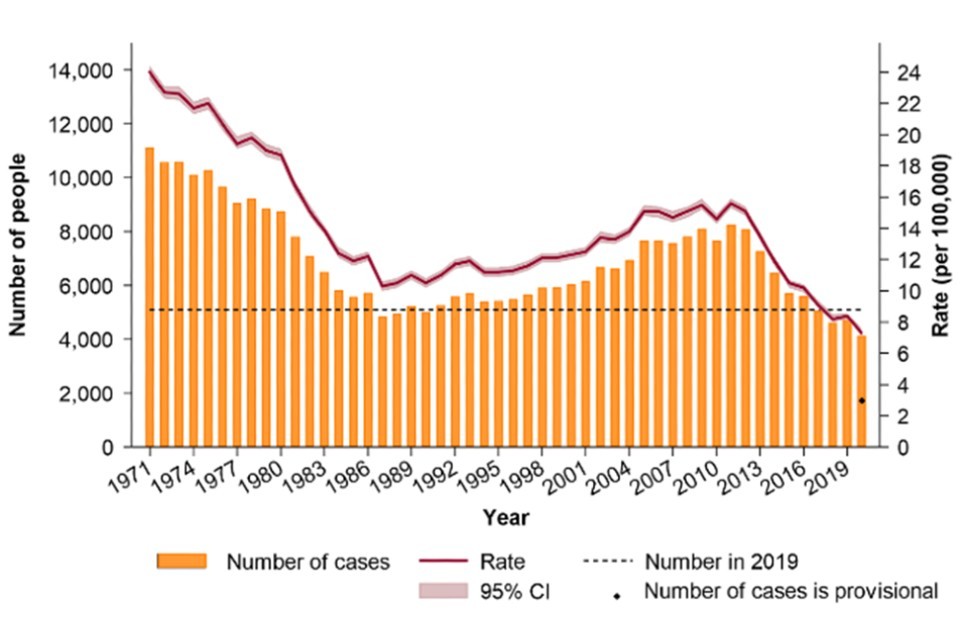
The graph in figure 2 shows the trend in TB incidence in England since 1971, with the most recent peak in notifications seen in 2011, at 8,250, declining to just over 4,000 cases in 2020.
In the following tables the year referred to is the financial year.
Priority 1. Recovery from COVID-19
| Actions | Outcomes and indicators | Key stakeholders and partners |
|---|---|---|
| 1.1 Plan and optimise the recovery of TB case detection and control, affected by the COVID-19 response, in the next 2 years to reduce the risk of active and latent TB disease by: | NHSE | |
| 1.1.1 Monitoring TB notifications, rates and trends, monthly and annually, locally, regionally and nationally. | 1.1.1 Monthly and annual reports on TB incidence and trends in TB data | UKHSA national and regions |
| 1.1.2 Increasing the number of people tested for latent TB infection (LTBI) as part of the national new entrant LTBI testing and treatment programme, to minimise the backlog of people eligible for LTBI testing. | 1.1.2 Report LTBI programme outcomes quarterly and annually | ICBs, providers |
| 1.2 Build on the innovation developed during the pandemic in the restoration and recovery of services impacted by the COVID-19 pandemic to ensure all TB services have access to: | ICBs, providers, NHSE | |
| 1.2.1 Laptops, mobile phones, Attend Anywhere or virtual clinics, MS Teams. | 1.2.1 Report annually for 2 years (2022 to 2023, 2023 to 2024) on access to laptops, mobile phones, Attend Anywhere or virtual clinics, MS Teams against a baseline established in 2021 to 2022 | Providers, NHSE regions |
| 1.2.2 Adequate outpatient clinic space for face-to-face patient interactions as necessary. | 1.2.2 Report annually for 2 years (2022 to 2023, 2023 to 2024) on access to outpatient clinic space | |
| 1.3 Ensure access to TB services and related services for people affected by TB by: | ||
| 1.3.1 Clear messaging for patients and staff on how to access TB services, face to face and virtual. | 1.3.1a. Review information on TB service providers websites on access to TB services by October 2021 | NHSE, providers |
| 1.3.1b. Recommend NHS and non-NHS websites provide information on TB service provision and access by March 2022 | NHSE, providers, third sector, UKHSA national | |
| 1.3.2 Use of learning regarding drivers of behaviours that influence staff and patients’ access to health care. | 1.3.2 Review behaviour toolkits, developed for COVID-19 work, to support 1.3.1 during 2021 to 2022 | Providers |
| 1.3.3 Facilitating appropriate use of technology for appointments and directly observed therapy (VOT/DOT). | 1.3.3 Review and report in 2022 to 2023 TB patients’ technological access to TB services and other healthcare providers | Providers |
| 1.4 Share, maintain and extend the learning from the impact of COVID-19 through continuation of the regional TB nurse peer support meetings | 1.4 Publish annual summaries of meetings. To note: work now completed with national report published on Establishing tuberculosis (TB) nurse peer support forums during the COVID-19 pandemic | UKHSA and NHSE national teams |
| 1.5 National team to provide advice to support health protection teams (HPTs) under pressure from ongoing COVID-19 response duties | 1.5.1 Audit and publish a report on HPTs TB capacity and workload in 2021 to 2022 | UKHSA national |
| 1.5.2 Act on the findings of the report by drafting appropriate action in 2022 to 2023 to ensure HPTs have the capacity to manage the TB workload | UKHSA national | |
| 1.5.3 Regarding audit in 2023 to 2024 | UKHSA national | |
| 1.6 Maintain the multi-agency UKHSA regions and TB control boards including new links to ICSs to provide oversight of the implementation and outcomes of the TB action plan at regional and local level | 1.6.1 Publish annual report on the work of UKHSA regions | UKHSA regions |
| 1.6.2 Monitor and report annually TB incidence at UKHSA regions, NHSE regional and commissioning levels | ICBs, UKHSA regions |
Priority 2. Prevent TB
Prevent and protect susceptible people in our population from acquiring TB infection and developing active disease.
| Actions | Outcomes and indicators | Stakeholders and partners |
|---|---|---|
| 2.1 Reduce active TB disease in people entering the UK after having negative TB tests overseas for a UK visa application | 2.1 Reduce the proportion of active TB cases diagnosed in people born outside of the UK in whom TB occurs within 5 years of entry by 5% annually, using the 3-year average, 2017 to 2019, as a baseline | UKHSA national, Home Office, UKHSA Port Health |
| 2.2 Improve the detection and treatment of LTBI in new migrants | 2.2.1 Increase the national LTBI programme uptake of the LTBI test by a national average of 15% per year using 2019 to 2020 as a baseline | ICBs, providers |
| 2.2.2 Increase national LTBI programme treatment completion rates by an average of 20% per year using 2019 to 2021 as a baseline | Providers | |
| 2.2.3 Review and report on local TB epidemiology in 2021 to 2022 to inform future local LTBI programmes | UKHSA national, ICSs and ICBs | |
| 2.2.4 Monitor and report quarterly and annually on the delivery and outcomes of local LTBI programme plans | UKHSA national | |
| 2.2.5 Report annually on the national LTBI programme monitoring indicators | UKHSA national | |
| 2.3 Update the published LTBI guidance and advice | 2.3 Update the published LTBI guidance and advice by end 2021 to 2022 | NHSE, UKHSA national |
| 2.4 Strengthen prevention, detection and treatment of active TB and/or LTBI in higher risk groups including: a) targeted screening in asylum seekers, including unaccompanied asylum seeking children b) healthcare workers through occupational health c) the immunocompromised d) the homeless e) those in contact with the criminal justice system f) people newly starting biological therapies, and demonstrating active engagement with local authorities, their public health teams and the third sector. |
2.4.1 Establish baselines and trajectories in 2021 to 2022 for screening for active TB and/or LTBI in groups a) to f) to improve proportions of people screened in groups a) to f). | Providers, local authorities, health and wellbeing boards (HWBs), ICBs |
| 2.4.2 Report on an annual basis the progress in increasing the proportion of people screened for active TB and/or latent TB in groups a) to f). | Providers, local authorities, HWBs, ICBs | |
| 2.5 Optimise contact tracing to rapidly identify and treat contacts of cases in whom infection is present by: | ||
| 2.5.1 Monitoring contact tracing outcomes | 2.5.1a. Report annually on the target of 90% of pulmonary or infectious TB cases to have a minimum of 5 close contacts (household and non-household) identified and screened | UKHSA national, providers |
| 2.5.1b. Establish a baseline and trajectory in 2021 to 2022 and report annually on the improvement in the proportion of people who are contacts with a positive LTBI test completing LTBI treatment | UKHSA national, providers | |
| 2.5.1c. Work towards systems able to monitor and report annually the proportion of close contacts of pulmonary or infectious TB who progress to active TB disease | UKHSA national, providers | |
| 2.5.2 Enhancing contact tracing through appropriate use of technology, for example, WGS | 2.5.2 Agree audit standards in 2022 to 2023 and report annually on the use of WGS by TB services to identify wider transmission networks for contact tracing | UKHSA national, providers |
| 2.6 Develop and implement national contact tracing evidence-based guidance and/or toolkits for HPTs, TB services, occupational health services including: | 2.6 Demonstrate and report biennially on the use of guidance and/or toolkits by local teams through local assurance mechanisms | UKHSA national, providers |
| 2.6.1 Standard contact tracing, contact tracing in congregate settings and occupational health (OH) contacts | 2.6.1a. Publish a standard contact tracing toolkit in 2022 to 2023 | UKHSA national |
| 2.6.1b. Publish national evidence-based guidance on occupational health screening for TB in 2023 to 2024 | ||
| 2.6.2 Manage TB incidents and outbreaks in health care, schools, prisons and the community | 2.6.2 Publish national guidance on managing incidents and outbreaks in 2023 to 2024 | UKHSA national |
| 2.7 Review and improve the effectiveness and delivery of communications used to increase awareness of TB in at-risk populations and healthcare workers, particularly those in primary care and emergency departments by: | 2.7 Review (2021 to 2022) and update material (2022 to 2023) to support targeted local community awareness programmes and awareness raising sessions including World TB Day | UKHSA national, UKHSA regions, providers, local authorities, ICSs, third sector |
| 2.7.1 Reviewing exemplars of communications in TB and other healthcare areas to inform the development and delivery of communications to those affected by TB | 2.7.1a. Report and make recommendations from review of exemplars of communications in 2022 to 2023 | UKHSA national, NHSE |
| 2.7.1b. Draft delivery plan in 2022 to 2023 to implement recommendations of review | NHSE, providers, local authorities, ICSs, third sector | |
| 2.8 Optimise Bacillus Calmette–Guérin (BCG) vaccine provision through commissioning and specification to: | 2.8 Commencing September 2021 monitor and report annually on BCG uptake in those eligible by the following indicators: a) offer BCG to 100% of those eligible b) 80% uptake of the vaccination at 4 weeks for those eligible |
Providers, NHSE |
| 2.8.1 Support BCG programme change to vaccinate at 4 weeks | 2.8.1 Report annually on uptake of the vaccination at 4 weeks for those eligible | Providers, NHSE |
| 2.8.2 Review commissioning, evidence and provision of BCG to age groups not included in current provision. | 2.8.2 Review the outcomes of TB disease in age groups not included in current provision to inform the review of commissioning and provision of BCG to those groups in 2022 to 2023 | NHSE, UKHSA national |
Priority 3. Detect TB
| Actions | Outcomes and indicators | Stakeholders and partners |
|---|---|---|
| 3.1 Improve early detection of TB by identifying, investigating and acting on the evidence and components that contribute to patient (people affected by TB) delay by: | Reduce the average delay in diagnosis in people with infectious or pulmonary TB year by 5% per year from 75 days in 2019 to 56 days in 2025 to 2026. The trajectory may require amendment to account for the impact of COVID-19 | UKHSA national, providers |
| 3.1.1 Developing a national survey to identify the components that contribute to patient delays in diagnosis. | 3.1.1 Report the outcomes of the national survey for people affected by TB in 2023 to 2024 | UKHSA national, NHSE, providers, patients’ representatives |
| 3.1.2 Discussing with modellers how to use the identified components that contribute to delay in diagnosis. | 3.1.2a. Identify the components of delays in diagnosis on a regional and national basis through TB service provider MDT workshops to collate the components in 2022 to 2023 | NHSE regions, providers, ICSs |
| 3.1.2b. Each TB service and/or UKHSA region or TB Control Board (TBCB) to develop and publish an action plan in 2022 to 2023 to address local components of delays in diagnosis | Providers, UKHSA regions | |
| 3.1.3 Publishing actions based on the identified components that contribute to delay in diagnosis | 3.1.3 Publish and report annually, commencing 2023 to 2024, on the identified components that contribute to delay in diagnosis | UKHSA national, NHSE |
| 3.1.4 Developing metrics to monitor patient and healthcare diagnostic delay. | 3.1.4 Develop metrics in 2022 to 2023 to monitor annually the key components of patient and healthcare diagnostic delay | UKHSA national, NHSE |
| 3.2 Reduce healthcare system delay by reviewing and improving access and delivery to diagnostics and treatment by: | 3.2 Reduce healthcare diagnostic delay in people with infectious or pulmonary TB annually by 5% per year using 2021 or 2022 as the baseline | UKHSA national, providers |
| 3.2.1 Reviewing and identifying the components of diagnostic delay on a regional and national basis. | 3.2.1 In 2022 to 2023 review, identify and publish the components of healthcare diagnostic delay on a regional and national basis | UKHSA national, providers |
| 3.2.2 Publishing and planning action based on 3.2.1. | 3.2.2 Report annually cohort review monitoring of diagnostic delay | UKHSA national and regions |
| 3.3 Improve and optimise diagnostics in high and low incidence areas for a) adults affected by TB b) children affected by TB, to include: |
3.3 Increase culture confirmation rates by 5% per year with trajectory based on 2020 to 2021 baseline | UKHSA national, providers |
| 3.3.1 Improving standards of laboratory practice. | 3.3.1a. Monitor and report annually on the target of 100% compliance in PCR use in accordance with National Institute for Health and Care Excellence (NICE) guidance in all pathology networks or TB services (paediatrics and adults) for all pulmonary or infectious TB cases | UKHSA national, providers |
| 3.3.1b. Annual reports on laboratories reporting reference laboratory results within a week maximum of receipt of report in accordance with ISO 15189:2012 requirements and within 24 hours for DR-TB | Providers | |
| 3.3.2 Increasing the proportion of culture confirmed cases, nationally and regionally. | 3.3.2a. Increase the proportion of cultured confirmed cases to the European standard of 80% for pulmonary TB by 2024 to 2025 | Providers |
| 3.3.2b. Reduce regional variation in culture confirmation of pulmonary TB (2019, 57.5% to 73.4%) with all areas progressing to achieve 80% by 2024 to 2025 | Providers | |
| 3.3.3 Annual routine monitoring of diagnostics including microbiology and radiology. | 3.3.3 Monitor and report annually on diagnostic delay due to delayed referral based on abnormal X-rays using ad hoc sampling | Providers |
| 3.3.4 Three-yearly audit of TB provision in microbiology laboratories. | 3.3.4 Plan and implement a 3-year audit of TB provision in microbiology laboratories commencing 2022 to 2023. | Providers |
| 3.4 Through the use of surveillance data and WGS diagnostic capabilities: | ||
| 3.4.1 Monitor and reduce transmission of TB. | 3.4.1 Automate process to provide cluster and transmission data routinely to TB services in 2022 to 2023. | UKHSA national and National Mycobacterial Reference Service (NMRS) |
| 3.4.2 Recognise and manage active TB, drug-resistant TB, TB clusters, outbreaks and incidents, particularly in those with social risk factors with a focus on public health interventions | 3.4.2a. 100% culture-positive TB cases have WGS relatedness data reviewed as part of decisions around contact tracing or public health intervention annually | UKHSA national and regions |
| 3.4.2b. Analyse and report on transmission pathways and networks 2023 to 2024 using metrics developed in 2022 to 2023 to monitor outcomes from public health actions | UKHSA national, providers | |
| 3.5 Focus on improving the detection and management of TB in people with social risk factors with the support of the ‘Tackling TB in USPs’ Resource | 3.5.1 Increase by 5% a year the number of people notified with TB and a social risk factor who complete treatment using 2020 to 2021 as a baseline | Providers, ICSs |
| 3.5.2 Report annually reports using National TB Surveillance System (NTBS) and cohort review data on the detection and management of TB in those with social risk factors | UKHSA national | |
| 3.6 Support the new NTBS development and roll-out | 3.6.1 Complete NTBS roll-out R2: 4 (go live to users) in 2021 | UKHSA national and NMRS |
| 3.6.2 Complete NTBS roll-out: R5 and 6 (pending approval) in 2022 | ||
| 3.7 Support the development of direct WGS from TB specimens in the NHS and maintain the TB reference service to support diminishing NHS capacity for culture, identification and UKHSA diagnostic sensitivity test (DST) | 3.7.1 Implement use of WGS direct from clinical specimens commencing 2023 to 2024 | UKHSA national and NMRS, providers |
| 3.7.2 Phenotypic susceptibility testing capacity for new and re-purposed TB drugs commencing 2022 to 2023 | UKHSA national and NMRS |
Priority 4. Control TB disease
Prepare and respond to emerging threats from TB transmission clusters, outbreaks and incidents and drug-resistant TB.
| Actions | Outcomes and indicators | Stakeholders and partners |
|---|---|---|
| 4.1 Improve and optimise diagnosis, treatment and patient-centred care in high and low incidence areas for a) adult patients b) paediatric patients by ensuring that: |
4.1a Decrease TB incidence each year as required to meet the 2035 WHO target for TB elimination: as of 2021 data this is estimated to be 13.4% per year | All |
| 4.1b Promote the use of ‘Getting it Right First Time‘ (GIRFT) across healthcare systems including TB services and other clinical services | ||
| 4.1.1 All partners in TB diagnosis, treatment and patient-centred care in high and low incidence areas work to the national TB service specification including: a) TB services and commissioners achieve and maintain 85% treatment completion rates and work to achieve 90% treatment completion rates by 2026 b) provision of both doctor and nurse led clinics c) a consistent approach to enhanced case management (ECM) d) an integrated approach to multi-disease prevention for those with social risk factors and others with TB, blood borne viruses (BBVs) and other conditions. |
4.1.1a. Report annually on TB completion rates. | NHSE national |
| 4.1.1b. Achieve 90% treatment completion rates for TB drug sensitive cases by 2026 | Providers | |
| 4.1.1c. Report biennially, commencing 2022 to 2023, on patient-centred care in high and low incidence areas work to the national TB service specification using the examples detailed | UKHSA national and regions | |
| 4.1.1d. Report on biennial patient satisfaction surveys, commencing 2022 to 2023, to support reviews on the quality of TB service care | Providers, ICSs | |
| 4.1.2 We partner low incidence TB services and commissioners with high incidence areas. | 4.1.2 Report annually, at regional and/or ICB level, the partnering of low incidence TB services and commissioners with high incidence areas | UKHSA regions, ICBs |
| 4.1.3 TB pathways are in place for adults and children which include access to TB advice and support from a specialist TB Service via a ‘hub and spoke’, ‘virtual clinic’ or shared care model. | 4.1.3 Audit TB pathways through commissioning arrangements biennially commencing 2022 to 2023 | ICBs, providers |
| 4.1.4 Strengthen TB clinical networks (adult and paediatric) with a clear reporting role to UKHSA regions, NHSE regions, commissioners and all health services involved in caring for people with TB are members of the local TB clinical network. | 4.1.4 UKHSA and NHSE regions to annually report on TB clinical networks membership as part of their annual reports | UKHSA regions, NHSE regions, providers |
| 4.1.5 Access to appropriate anti-TB medications, preparations and newer drugs for adults and children. | 4.1.5 Monitor and report annually on anti-TB medication issues | Providers |
| 4.1.6 Use of current national TB guidelines such as NICE and Royal College of Nursing (RCN) and collaborate with NICE to update the TB guidance. | 4.1.6 Confirm the national TB service specification in 2021 to 2022 is consistent with NICE TB guidance and initiate work in 2022 to 2023 to update the NICE TB guidance. | NHSE, UKHSA national |
| 4.2 Ensure timely and complete reporting or notification by NHS teams. | 4.2a. A minimum percentage and annual improvement for data submissions, standards and completeness to be agreed in 2022 to 2023 | UKHSA national |
| 4.2b. Report annually, by region and TB service on data quality standards and completeness in NTBS, UKHSA | UKHSA national, providers | |
| 4.3 Ensure analysis and dissemination of national TB surveillance data with the provision of timely analysis to NHS teams at a scale that supports local and national services. | 4.3a. Report on analysis and dissemination of national, regional and local data in 2022 to 2023 | UKHSA national |
| 4.3b. Report annually on user ratings and feedback reports | UKHSA | |
| 4.4 Improve operation of the WGS system by: | UKHSA-NMRS, UKHSA Data and Analytical Sciences | |
| 4.4.1 Agreeing and implementing governance framework, for the sharing of TB genomic data by the NHS and UKHSA for TB diagnosis and transmission, as an extension of statutory duties. | 4.4.1 UKHSA to report in 2021 to 2022 governance framework in place | |
| 4.4.2 NHS and other sequencing providers ensure mechanisms are in place for appropriate sequence sharing. | 4.4.2 Annual update on data sharing agreements or equivalent in place with all users | UKHSA national and NMRS, providers. |
| 4.4.3 Ensuring and maintaining capacity for WGS computational analysis and storage in UKHSA including data shared from other sequencing providers. | 4.4.3 UKHSA to ensure the WGS system is included in its IT strategic planning, 2021 to 2022 | UKHSA national and NMRS |
| 4.5 Contribute to global sharing of non-identifiable genomic data to enable recognition of global transmission and engage in international efforts to standardise genomic prediction of drug resistance, UKHSA drug susceptibility testing and shorten treatment for drug resistant TB. | 4.5 Demonstrate compliance with WHO requirements and active contribution to international collaborations annually as reported in WHO updates | UKHSA national |
| 4.6 Ensure effective management of cases of multi-drug resistant (MDR-TB) in association with the British Thoracic Society (BTS) MDR-TB Clinical Advice Service (CAS). | 4.6a. Increase the proportion of MDR-TB cases routinely submitted to the BTS MDR-TB CAS for review – currently 80% – and increase by 5% per year to 100% in 2024 to 2025 | BTS MDR-TB CAS |
| 4.6b. Review sustainability of funding support to the BTS MDR-TB CAS for 2021 to 2022 and future | NHSE | |
| 4.7 Through research, evaluation, translation and innovation develop, drive and evaluate new approaches to share evidence to improve the detection and response to TB disease. | 4.7 Set up an annual reporting mechanism to report and disseminate information on TB research projects, progress and outcomes | UKHSA national, providers, academia |
Priority 5. Workforce
| Actions | Outcomes and indicators | Stakeholders and partners |
|---|---|---|
| 5.1 Develop and maintain the healthcare workforce to ensure workforce capacity to detect, case manage and control TB by: | UKHSA national, NHSE | |
| 5.1.1 Reviewing TB services against the national TB service specification. | 5.1.1 Commencing 2021 to 2022 biennially review TB services and compliance against the national TB service specification. | UKHSA national, NHSE |
| 5.1.2 Ensuring every trust has a designated lead TB clinician and/or TB nurse lead. | 5.1.2 Report in 2022 to 2023 on trusts able to report designated lead TB clinician and number of programmed activities (PAs) and TB nurse lead | NHSE national, providers |
| 5.1.3 Surveying and reporting on the workload of the nurses and medical workforce particularly: a) patient case load b) baseline staff levels c) skill sets. |
5.1.3 Report on TB service workforce survey in 2022 to 2023 | UKHSA national, NHSE |
| 5.1.4 Determining the minimum number of people affected by TB required to provide a ‘safe’ TB service and maintain staff expertise. | 5.1.4a. Organise a national workshop in 2023 to 2024 in collaboration with BTS, RCN, British Association of Paediatric Tuberculosis (BAPT), royal colleges and so on to identify the minimum number of people affected by TB to provide a ‘safe’ and appropriate TB service and maintain staff expertise in response to GIRFT report recommendations | UKHSA national, NHSE, RCN, royal colleges, BAPT |
| 5.1.4b. Draft and publish guidance and recommendations in 2023 to 2024 regarding a ‘safe’ and appropriate TB service and TB workforce provision | NHSE, UKHSA national | |
| 5.1.5 Publish guidance and recommendations on the levels of staff and skill mix based on evidence (that is, RCN TB nurse competency framework), competence based practice and exemplars of best practice to inform TB workforce provision and support career progression including: a) nurse prescribers b) phlebotomy competency c) qualified as advanced nurse practitioners d) employed as nurse consultants e) admin support f) social care or outreach staff support. |
5.1.5 Biennially monitor and report provision of access to practical skills training, for example, prescribing, phlebotomy, education or training in signposting patients to benefits and housing support to inform TB service provision | UKHSA national, NHSE regions, ICBs |
| 5.1.6 Ensuring the majority of TB nurses with a caseload are competent or qualified to carry out phlebotomy and nurse prescribing using learning from the COVID-19 pandemic. | 5.1.6 Biennially report on TB nurse competency and qualification in phlebotomy and nurse prescribing | UKHSA national, providers |
| 5.2 Improve education, training and peer support for the TB workforce through clinical and nursing networks, TB networks, educational programmes, and multidisciplinary team working by: | ||
| 5.2.1 Ensuring training needs of the TB service workforce (medical, nursing and non-clinical) are focused on future ways of working. | ||
| 5.2.2 Ensuring 100% provision of induction training (national template and reword) for the TB workforce at a local and regional level. | 5.2.2 Commencing in 2022 to 2023 biennially report on the provision of induction training for the TB workforce | Providers |
| 5.2.3 Ensuring access to adequate and appropriate continued professional development (CPD) events at local, regional and national level that meet national and professional guidance. | 5.2.3 Report, in summary format, annually, provision of CPD events | Providers |
| 5.2.4 Ensuring TB components for medical and pre-registration nurse training inform TB education modules. | 5.2.4a. Review in 2022 to 2023 medical and preregistration nurse training for TB components | RCN, royal colleges |
| 5.2.3b. Action appropriately in 2023 to 2014 | RCN, royal colleges | |
| 5.2.5 TB services facilitate student nurse visits or placements. | 5.2.5 Survey and report on student nurse visits or placements in TB services in 2023 to 2024 | Providers |
| 5.2.6 Providing access to education, educational resources and training for hospital doctors, nurses and GPs including webinars, the Royal College of General Practitioners (RCGP) e-learning module, formal university courses and the professional awareness and resource available on the TB Alert website. | 5.2.6 Biennially, commencing 2023 to 2024, review provision, use and access to TB educational | NHSE, RCGP, providers |
| 5.2.7 Reviewing induction training for staff in primary care and emergency departments to ensure includes TB awareness information. | 5.2.7 Report on review of induction training and update awareness raising session materials for health and non-healthcare services in 2022 to 2023 | NHSE, RCGP, providers |
| 5.3 Future proof TB services by ensuring: | NHSE, UKHSA national, ICBs | |
| 5.3.1 The TB workforce aligns with the workforce section of the NHSE long-term plan. | 5.3.1 In 2022 to 2023 review and report on how the TB workforce aligns with the workforce section of the NHSE long-term plan | NHSE, UKHSA national, ICBs |
| 5.3.2 Appropriate service transformation to provide a people centred TB service that can sustain the management of people with active TB disease, the LTBI programme, meet the needs of incidents, outbreaks and surge capacity. | 5.3.2 Commissioners and/or ICBs and/or TB service providers to review and report on the provision of TB services in 2023 to 2024 in response to GIRFT report recommendations | NHSE, UKHSA national, ICBs |
| 5.3.3 The workforce reflects the requirements of local people with TB and the community underpinned by the NHSE LTP workforce section. | 5.3.3 Report on future provision to meet changing local population and workforce needs from 2023 to 2024 onwards | NHSE, UKHSA national, ICBs |
| 5.3.4 Encourage use of new tools such as digital and social media to raise awareness of TB in at-risk populations and healthcare workers. | 5.3.4 Report annually on new tools and use to raise awareness in at-risk populations and healthcare workers | Providers, third sector |
