UK Drug Recovery Champion first annual report (accessible version)
Updated 9 December 2021
January 2021
Ministerial Foreword
Recovery from drug dependence is a key aspect of our approach to tackling drugs and reducing drug harms. While we support prevention activity which reduces the demand for drugs, and we work with law enforcement partners to choke off the supply of drugs, we must recognise that there are many people over whom drugs have taken a hold often leading to problems with dependence and addiction. Some individuals recover on their own, but many need support through treatment and other types of services to do so. Some of these individuals are extremely vulnerable, face multiple complex needs such as poor mental health, deprivation and isolation, and require significantly more support. This is why the range of peer support, medical, housing, employment, education and other services matter.
Dr Ed Day was appointed to the role of Recovery Champion in May last year to provide leadership on key aspects of the recovery agenda. He will offer a national perspective on the health of the ‘recovery system’, holding both national Government and local partners to account for doing what is needed to improve outcomes for those in recovery or considering starting their recovery journey. He plays a pivotal role in assessing the current treatment system and sharing insight as to how the UK Government can work with external stakeholders and partners to give people the best chance of recovering from substance misuse. Dr Day will inform the Government’s policy and practice in the context of our ambition to protect vulnerable people who are dependent on drugs and reduce drug misuse.
We are very grateful to Dr Day for his keynote speech at the UK Drugs Summit held in Glasgow in February this year, in which he set out very clearly the challenges, but also the extent to which recovery can provide hope and help people to turn their lives around. Ministers, leading experts and those with lived experience from across the UK were present and found the presentation engaging and thought-provoking. Dr Day has also been working closely with Dame Carol Black to inform her review of Prevention, Treatment and Recovery, which will provide a major contribution to the Government’s approach to tackling drug misuse. This review will help inform a significant part of the work of the Recovery Champion over the course of the coming months.
One of the greatest benefits of Dr Day’s expertise as Recovery Champion is his ability to consolidate wider research and evidence from across the sector, offering a pragmatic view as to how evidence-based practice can be realistically applied and implemented. Successful or innovative recovery-focused activities can then be fed directly into relevant service user groups, including Public Health England run networks and service provider groups, as well as Government officials and Ministers.
This annual report sets out the work already undertaken by Dr Day and his plans for the coming period. It offers an exciting opportunity to strengthen our collective responses in this area and I look forward to working alongside Dr Day to achieve our ambitions and shape more positive outcomes on drug recovery.
Jo Churchill MP
Minister for Prevention, Public Health and Primary Care
Department of Health and Social Care
Kit Malthouse MP
Minister for Crime and Policing
Home Office
Introduction to the Recovery Champion
I am a psychiatrist specialising in the treatment of drug and alcohol use disorders, and I combine clinical work in the NHS with research and teaching. I have over twenty years’ experience in the field and throughout my career much of my research has focused on developing new pharmacological and psychosocial treatments. Through this work I have come to understand the importance of addressing addiction holistically, helping individuals not only to stop using substances but to make wider changes in their whole outlook on life. People who have overcome drug dependence often say that the opposite of addiction is ‘connection’. Addiction is a disorder of the social environment, and there is a need to consider the family and the wider community in order to help an individual to achieve lasting improvements in their health and quality of life.
My desire to take on the role of the UK Government’s Recovery Champion came from my clinical and academic experiences of recovery. When I first began working in the field of addiction the landscape was strikingly different to today, but it was my initial experience of working with service users that sparked my interest in this area of medicine. Although addiction can destroy the lives of individuals and their families, treatment can dramatically reduce these harms and frequently saves lives. The journey to stable recovery is often a long one, and requires great strength and determination. However, listening to an individual share their story is both humbling and inspiring, and only by listening to these narratives will we start to overcome the stigma that addiction brings.
The concept of ‘recovery’ involves more than just control over substance use. It requires better mental and physical health, but just as importantly it involves the development of a meaningful life. Recovery is a process that often takes time to achieve and effort to maintain. Medical interventions and professional treatment services only form one part of the total picture, and I believe that the creation of a ‘Recovery Orientated System of Care’ (ROSC) offers the best chance of helping people move out of addiction. A ROSC involves an equal partnership between ‘professionals by training’ and ‘professionals by experience’, and I hope my first annual report will reflect the views of the many people with lived experience that I have spoken to over the past 12 months.
Understanding the Recovery System
Addiction is not an all-or-none phenomenon, and exists along a spectrum of severity that varies from substance to substance. Although people may use psychoactive substances without significant issues, harms can accumulate quickly and become self-perpetuating. The term ‘dependence’ describes a chronic, recurring condition with physical, psychological and social dimensions. It is characterised by a loss of control over one’s substance use, and is usually associated with unsuccessful attempts to cut down or control use. Substances are taken in larger amounts or over a longer period than was intended, and considerable time is spent in obtaining, using, or recovering from the effects of the drugs. This leads to a reduction in other social, occupational, or recreational activities, but use continues despite the drug-related problems. Most psychoactive substances, if used regularly, can produce some degree of dependence.
Recovery is about much more than the control of problem substances, and requires a gradual accumulation of positive benefits. The complications caused by drug dependence mean that addiction is associated with overwhelming negativity and stigma. Drug users often come into contact with multiple agencies, including drug treatment, criminal justice, mental health, welfare, and primary health care services. Interactions with any of these services may trigger a turning point in an addiction trajectory for some individuals, and a ROSC must include all these elements working together. The pathway to recovery may utilise various types of support and interventions or may occur without any formal external help: there is no ‘one size fits all’. Recovery is a process, not a single event, and takes time to achieve and effort to maintain. It must be voluntarily-sustained in order to be lasting, although it may sometimes be initiated by ‘coerced’ or ‘mandated’ interventions within the criminal justice system.
Over the past half century the focus of healthcare has changed from ‘curing’ acute problems such as infections to ‘managing’ chronic ones such as diabetes. Serious substance use disorders are chronic conditions that can involve cycles of abstinence and relapse, often over several years. An episode of treatment that leads to abstinence cannot be said to be a cure, and in order to stay drug-free an individual will need to make changes to all areas of their life. If the drug use problems are low level in terms of severity, or the individual has significant social and recovery capital, deciding to stop may end a chapter in that person’s life that never recurs. In more severe cases, a broader change in behaviour, outlook and identity is required, moving from immersion in the culture of addiction to the culture of recovery. This change occurs over a period of time, and will inevitably alter how the individual thinks about themselves and their lives.
The diversity in routes to recovery has sometimes led to debate about the value of some pathways over others. An unhelpful split occurred in the UK about 10 years ago where recovery became equated with abstinence, and was presented as being in opposition to ‘harm reduction’ approaches such as opioid agonist treatment (e.g. with methadone or buprenorphine). This led to further divisions between people with expertise through training and those with expertise through experience. In reality, a chronic disease often requires both intensive and extensive treatment to bring about remission, and the ideal system of care blends both professional treatment services and peer-led recovery support services in a seamless ROSC.
The values underpinning a ROSC are based on the recognition that the individual is the agent of his or her own recovery, and all services can be organized to support recovery. Person-centred services offer choice, honour each person’s potential for growth, focus on a person’s strengths, and attend to the overall health and wellness of a person with addiction. There is an increasing understanding that recovery-oriented services should be provided in communities, in specific environments of need, and be provided by professionals, family members, and peers. A ROSC arranges services to address the long-term and complex needs of people living with addiction. It should be built on the core values of individual choice and person-centred services, and support multiple non-linear pathways to recovery.
Addiction is often rooted in pain, and two key themes are important in overcoming and managing it. Firstly there must be hope, a promise that things can and do change, that today is not the way it will always be. Secondly there must be a search for meaning, purpose and direction in one’s life. People derive meaning from different things: through work or social relationships, advocacy or spiritual understanding. The ROSC must support their attempts to build hope and meaning if control over substance use is to be maintained in the long term. Recovery is a reality: it can and does happen.
The Current State of Recovery
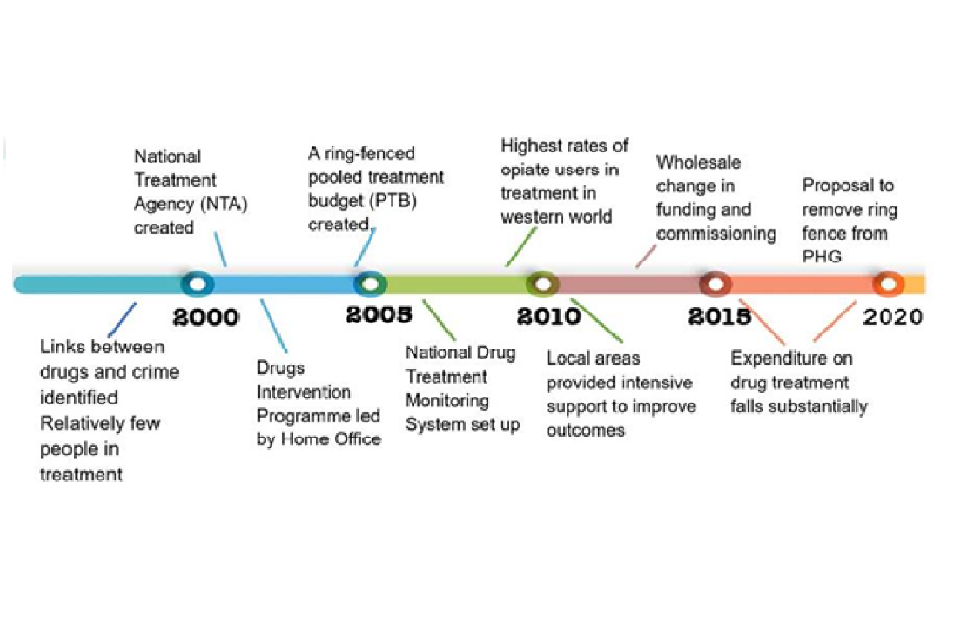
My 20 years working in the addictions treatment field in England have seen a rise and fall in service provision. The period from 2001 to 2010 saw unprecedented investment in the treatment system, and an extensive system of oversight and monitoring through the National Treatment Agency for Substance Misuse. The last 10 years have been characterised by the marketisation of the addiction treatment system In England, with frequent re-tendering of service provision in each local area. This approach has brought some benefits, including excellent examples of innovative working through the third sector and peer-led community organisations. However, sustained cuts to Local Authority funding have had an impact on the quality and variety of provision, and peer-led recovery support services have often been the victims. The cuts have also led to a focus on achieving targets that are not always relevant to the process of sustaining long-term recovery. When combined with workforce issues and a loss of expertise in the field, and a steady uncoupling of the specialist addiction services from the mainstream NHS, there are concerns that we are moving away from the optimal Recovery Orientated System of Care.
In February 2020 Dame Carol Black published her Independent Review of Drugs. Some of the key messages were that:
- Expenditure on drug treatment has fallen since 2013/14 along with similar falls in the numbers in drug treatment during this time, against a backdrop of increases in the prevalence of problematic drug use.
- Some areas are starting to ‘ration’ treatment, setting higher thresholds for those who can access it and/or just offering a minimum service due to workers having such large caseloads.
- The number of residential rehabilitation services has reduced significantly, removing a core treatment component for those that need it to support their recovery.
- Recovery is much wider than just substance use treatment with many drug users having multiple complex needs in terms of health (both physical and mental), employment, homelessness and offending.
- Many key indicators (deaths, unmet need, recovery rates) are going in the wrong direction and there is significant variation in both local spend in relation to need and the achievement of recovery and other outcomes.
- There is significant local variation, but outcomes tend to be worse in the north of the country and particularly in the North East, often these areas have higher rates of opiate and crack use and higher rates of drug related mortality.
- Levels of rough sleeping are rising, prevalence in the population is increasing: need is not being met and the problem is worsening with the levels of mortality at the highest since records began.
- The IPS employment trial is showing very promising early success in finding employment for people in drug and alcohol treatment.
Dame Carol’s report included an evidence pack, including some data bearing on recovery which I include below, this highlights the range of complex needs drug users have, which require support to enable and maintain recovery.
Complex need factors at start of treatment - opiate clients
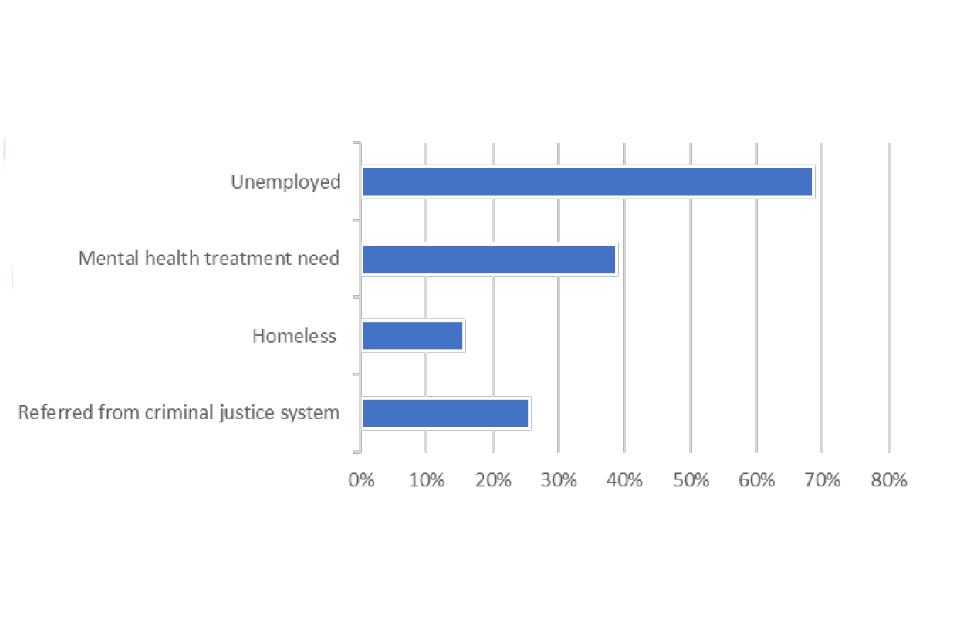
- Nearly 70% of opiate users are unemployed at the start of treatment;
- With 40% having a mental health need;
- And a quarter having been referred from the Criminal Justice System.
Multiple complex needs at start of treatment- opiate clients
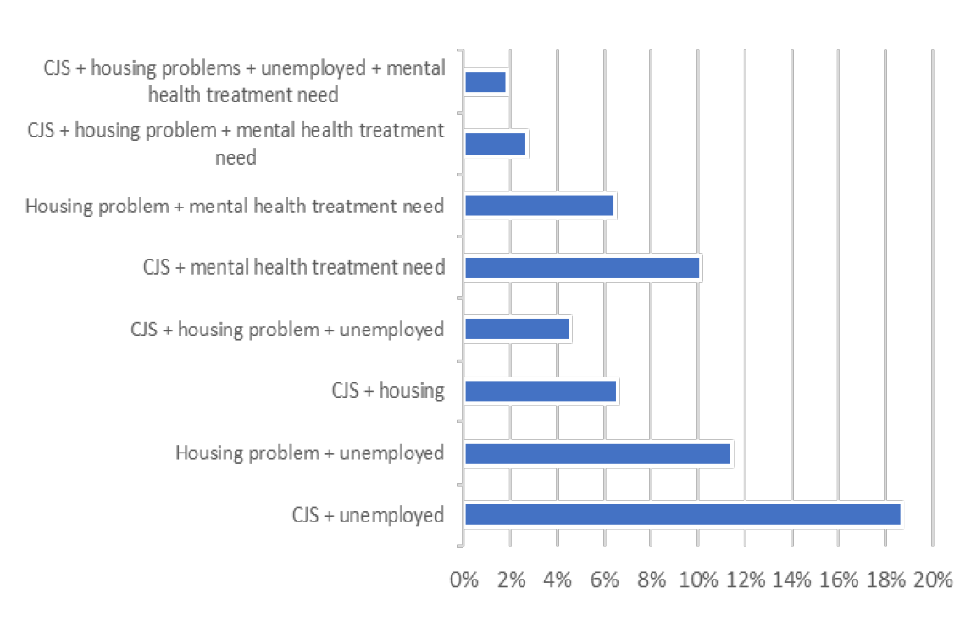
- Over 60% of opiate clients have two or more complex needs alongside their drug use;
- With nearly 1 in 5 being unemployed and referred from the CJS;
- One in 10 having a mental health need and being referred from the CJS;
- And 1 in 50 having all four complex needs
There is more evidence that I would like to see captured in relation to recovery, which I will address in later sections of this report, to ensure evidence-based policy and practice in the prevention and treatment of drug misuse. It is only by ensuring we have sufficient data to inform policy makers of the reality of recovery for those in need that we can champion best practice and improve outcomes for all.
Activity in Year 1 and Planned activity
Consulting widely across the drug misuse treatment sector to understand the state of recovery in the UK
After being appointed Recovery Champion by the Home Secretary in May last year, I have spent much of my time in the role talking to a diverse range of stakeholders across the sector. A list of many of the individuals and organisations I have met with can be found at Annex A.
Prior to the COVID-19 pandemic I met with people with a broad range of different perspectives including people with lived experience running recovery support services, service users, service providers, commissioners, Directors of Public Health, Police & Crime Commissioners, Ministers and officials from Government departments. I have spoken at conferences and meetings around the country, as well as giving presentations to the Advisory Council on the Misuse of Drugs, All-Party Parliamentary Groups, and the Drug Strategy Board. I also participated in a World Health Organisation event in Vienna about over-coming the stigma of addiction.
Since the onset of the pandemic this work has intensified. Recovery support services led the way in the community response to COVID-19, quickly moving support provision online, and mobilising community resources to support those most in need. Peer-led services were some of the first providers to return to face-to-face contact when safe to do so, recognising the importance of connection in sustaining recovery.
These engagements have been invaluable in testing the temperature of drug treatment services and ROSC in different communities around the UK. Much of the information I have gathered informed my input into the Dame Carol Black review.
Developing methods of systematically capturing the views of service users and people with lived experience of addiction
On taking up my role as Recovery Champion it became clear that the Government has no systematic method of surveying users of treatment services, people in early recovery, and those with lived experience of developing peer-led services. I have therefore been working with a variety of groups to establish regular and reliable ways of developing a two-way conversation between policy makers and people with lived experience of drug problems.
Three ongoing initiatives are worthy of note:
1. Attendance at the Mutual Aid Reference Group at Public Health England. This group includes representatives from the 12-Step Fellowships, SMART Recovery and other peer- led mutual aid groups, and provides a valuable point of contact for people with a variety of perspectives.
2. The ‘Recovery Connectors’ group. The UK has a diverse range of ‘Lived Experience Recovery Organisations’ (LEROs) whose methods are driven by mutual support, community engagement and a commitment to individual and group wellbeing. These organisations began to flourish with changes to UK drug treatment services from 2010 onwards, but more recently they have come under threat from reduced budgets and the competitive tendering process utilised in England. Unlike the professional services, LEROs are not underpinned by established membership bodies or governance and inspection frameworks, and there are no established annual forums to allow the sharing and exchange of good practice or innovation.
Working with Professor David Best, one of the leading researchers in the field of recovery, we have established a weekly Recovery Connectors group that has met online during the COVID-19 pandemic. This group aims to identify and champion innovation in LEROs, and provide connections and support for recovery leadership. The group is working on developing definitions of best practice and standards of care within recovery support services. The aim is to share this with the wider field in a collaborative process looking to build consensus.
3. Using the SURE Recovery App. Working with Public Health England and NHS England, I have been exploring ways to develop a regular, easy to access method that Government can use to seek opinions of service users about key issues in the field. The SURE Recovery mobile phone app was developed by a group of peer researchers at King’s College London led by Professor Jo Neale. It contains a variety of useful tools to assist recovery from addiction, but also includes a facility for posing regular questions about key issues affecting people with drug use problems. The anonymised responses can then be analysed systematically to build up a picture of service user views which can be presented to policy makers. The app has been promoted extensively through key publications in the UK addictions field.
Tackling issues with the workforce
My personal experience of working in specialist treatment services has highlighted a growing workforce crisis within the field. The combination of steadily reducing budgets for treatment provision and structural changes in the way services are commissioned since 2012 have led to a steady loss of expertise. This has been compounded by the lack of up- to-date national occupational standards for practitioners in the field, whether they come from a professional or lived experience background. This has been a widespread view when speaking to people around the UK, and is an issue that must be addressed,
With this in mind, I have contributed to a Royal College of Psychiatrists workforce strategy which has made practical recommendations to stem the steady decline in specialist doctors working in the field since 2012.
Furthermore, I contributed to a meeting convened by the Department of Health and Social Care in October 2019 in conjunction with the Home Office and other Government departments, treatment providers and the Local Government Association to explore this issue. This issue was featured prominently in Dame Carol Black’s report on Drugs for the Home Office in February 2020, and will be addressed by part 2 of her report on prevention, treatment and recovery.
Supporting the Government in developing effective policy
One of the key goals of the Recovery Champion post was to ensure that the Government implements evidence-based practice in the prevention and treatment of drug misuse. Although it is clear that the UK has developed an extensive and impressive evidence base for the treatment of problematic drug use, this has been increasingly hard to implement as service funding has reduced.
Furthermore, the peer-led recovery support service component of the ROSC has been largely neglected by researchers in the UK. The extent and impact of mutual aid groups has not been fully explored, and the methods of linking professional services to them. In particular, there is a need to collect meaningful outcome data about all aspects of recovery once an individual leaves professional treatment at the end of an episode of care.
Future Plans
Working with partners to share best practice and continue to promote dialogue about recovery, using a range of conferences, events and media to do so.
I will build on my extensive discussions with people across the sector during the past year, and will be keen to hear from others with a perspective to offer. I plan to continue to work on the development of feedback mechanisms from both users of treatment services and people in early and late recovery. The goal will be to support people with lived experience in developing quality standards for peer-led services and training and accreditation for roles in recovery support services. I also plan to conduct the first national survey of people in recovery.
Supporting Government in developing its policy on recovery and broader approach to drug misuse, including through my support for the Review of Prevention, Treatment and Recovery.
I will continue the work that I have started in informing the Review of Prevention, Treatment and Recovery led by Dame Carol Black, which has strong support from Government and will make an important contribution to policy development when it presents its findings in late 2020.
I also expect to maintain regular discussions with policy makers in the Home Office, Department of Health and Social Care, Public Health England and other parts of Government to advise on issues as they arise and to make my views known and to share examples of practice on the ground.
Establishing a UK Addiction Recovery Research Institute
The UK drug treatment system is built on a solid evidence base. Extensive work by the National Treatment Agency for Substance Misuse, Public Health England, and the National Institute for Care Excellence amongst others has reviewed and clarified the evidence base for effective treatment interventions. The National Drug Treatment Monitoring System (NDTMS) is a sophisticated data collection system that provides an excellent picture of the impact of treatment services.
However, once an individual leaves the treatment system they become less visible, and the outcomes of peer-led recovery support services can lost. It is likely that this has contributed to their decommissioning as budgets have been reduced.
Building upon the work of Professor John Kelly at the Recovery Institute at Harvard Medical School in the United States, I want to bring together expertise from around the country and develop a similar organisation in the UK. A Recovery Research Institute would set out to enhance the impact of addiction recovery research through the summary, synthesis, and dissemination of scientific findings, evaluation of efforts at facilitating recovery and their implementation in the UK, and the undertaking of novel research.
My initial aspirations for the Institute would include
-
Creating a network of researchers and people with lived experience interested in research both nationally and internationally, bringing together the best research and disseminating it as widely as possible.
-
Developing a ‘road map’ for further research that is co-produced by people with lived experience alongside researchers, clinicians and policy makers.
-
Developing standardised methods of measuring recovery and social support, and working with LEROs to implement these in routine practice.
-
Conducting a national cohort study of people leaving treatment in order to better understand some of the barriers to long-term recovery.
-
Developing the UK evidence base for mutual aid groups (e.g. Twelve-step Fellowships, SMART Recovery), and exploring the possibility of developing a range of additions to the existing provision.
-
A national survey of recovery to build a rich data set that can provide a broader understanding of the recovery landscape over time.
-
Create good practice handbooks and websites that set an international standard in recovery.
-
Developing a broader understanding of the involvement of families and other network members in the recovery journey.
The work of the UKARRI would be underpinned by a process of co-production between people with lived experience of addiction, their families and significant others, academics, service providers and policy makers, utilising the principles of network and capacity building. The definition of ‘addiction’ will be broad and include behavioural addictions as well as dependence on psychoactive substances (e.g. illicit drugs, prescribed medications, or alcohol). It will take a holistic approach embedded within a life-course model of addiction and recovery.
A ROSC includes multiple interacting elements, including prevention, harm reduction, engagement, treatment and on-going pathways of recovery support. There will be a focus on early recovery (i.e. paths out of addiction in young people) as a form of prevention. The UKARRI will help to disseminate the biomedical evidence base for addiction treatment, but integrate this into a wider community-based recovery model, and will build an evidence base for the UK around contextual and systemic factors that support and facilitate recovery.
Moving recovery ‘upstream’ – considering young people
Dependence on drugs usually has its roots in the first 25 years of life. Recent advances in the understanding of the neurobiology of the adolescent brain shed new light on how young people interact with psychoactive substances and other potentially addictive behaviours. Substance use before the age of 20 is usually a symptom of wider problems, and dependence has rarely developed at this point. Effective intervention could therefore potentially lead to a very different life path, but may need to include a variety of elements beyond a focus on substance use: trauma-focused care, treatment of mental health issues, social and educational support, criminal justice diversion interventions.
Evidence collected for Dame Carol Black’s report has shown that the number of school age and young people using drugs is increasing, although the number entering professional treatment is decreasing. Recovery-based services for young people are rare, and there is no real recovery culture for young people in the UK. Educational difficulties associated with early substance use (or living in a family with alcohol or drug problems) may limit access to higher education for this already marginalised population.
Furthermore, the contrast between their age and developmental level, and the middle-age focus of 12-step and other peer-led groups, means that the support provided by affiliating with conventional 12-step groups alone may not provide these young adults with the support they need to maintain abstinence and build strong recovery while simultaneously growing into mature young adults.
Therefore, one area that I intend to develop is recovery support in schools, Colleges and Universities. Academic institutions in the USA have begun to create programs designed to support the recovering student and to increase access to treatment for the student still in active addiction. These programs, termed Collegiate Recovery Programs (CRPs), exist in small numbers in higher education institutions, and preliminary data suggest that they effectively promote recovery, prevent relapse, and improve educational outcomes for the individuals participating in them. The first attempt to create something similar in the UK has recently started at Teesside University, and I have been working to develop a CRP at my own institution, the University of Birmingham. Over the next year we intend to create a national forum to share learning about this approach, and work with student groups to support CRPs across the UK.
Recovery from Substance Misuse and COVID-19
Over the past 10 months we have faced unprecedented restrictions on our daily life due to the impact of COVID-19, and this has made the process of recovery from drug or alcohol use disorder particularly challenging. Connection with others lies at the heart of recovery, but this was initially challenged by essential life-saving public health measures such as lockdown, shielding and social distancing.
The response of both professional services and the peer-led communities was amazing, with huge efforts made to protect treatment and replace face-to-face meetings with online alternatives. The ‘Everybody In’ initiative has started to tackle the issue of homelessness and rough sleeping, and there has been increased awareness of mental health issues arising from social isolation.
It is too early to say definitively what impact this has had on drug or alcohol use, but it is likely that there will be an increased need for treatment and recovery support services as the pandemic recedes. Many patients receiving treatment for drug misuse also have co- existing medical conditions that make them vulnerable to COVID-19. It is possible that the virus will disproportionately affect this group, and it will be important to ensure that the most vulnerable people in society remain connected to physical and mental health services.
The pandemic has seen a huge increase in the use of digital technology, and especially videoconferencing platforms. For many this has been a vital lifeline, allowing them to connect to others to give and receive support. The Twelve-Step Fellowships (such as Alcoholics Anonymous, Narcotics Anonymous, Cocaine Anonymous) report a huge increase in online meetings, as well as an increase in newcomers to the Fellowship. It seems that many people found it easier to attend online meetings than attend in person. However, it remains to be seen whether this trend will continue, and many members of the Fellowships have told me how important it will be to return to face-to-face meetings as soon as it is safe to do so.
Specialist addiction treatment agencies have also increased their use of telephone and video appointments. This has compensated to some degree for the necessary restrictions on numbers able to attend services, and many of these innovations will continue even when the pandemic recedes. However, it is important to remember that many of the most vulnerable people in society do not have access to smart phones or data, and so remain isolated. We need to work out the best way of retaining the benefits of digital interventions whilst monitoring their efficacy and ensuring that personal contact is not lost.
Conclusion
This is my first annual report as Recovery Champion. This is a new role, and it will take some time to work out how I can make the most impact. However, I will continue to prioritise the promotion of evidence-based strategies for treating addiction, and arguing for a strengthening of the professional workforce and recovery orientated treatment systems. However, perhaps the most important role is to bring professionals and people with living and lived experience of drug addiction together to work as one to overcome one of the biggest challenges in society. Addiction remains heavily stigmatised, and yet I see people overcoming it every day and leading happy, healthy and productive lives.
Annex A – Meetings with Key Stakeholders
- Discussion with Ministers and experts from across the UK at the UK Drugs Ministerial meeting, September 2020
- Speech at the UK Drugs Summit in Glasgow, February 2020
- Presentation to the Ministerial Drug Strategy Board in June 2019, at which HO, DHSC, MoJ, HMT, DfE, MHCLG Ministers among others were present
- Meeting with the then Minister of State for Crime and Policing, Victoria Atkins MP (now Minister for Safeguarding)
- Public Health England
- Acer Unit, Bristol NHS Inpatient Unit
- Presentation at the UKESAD conference
- Steve Dixon CEO Changes UK, Birmingham
- David Jamieson, West Midlands Police and Crime Commissioner
- NHS Substances Misuse Providers Alliance, NHSSMPA conference
- Mutual Aid Reference Group, PHE
- Presented at Full Council, Advisory Council on the Misuse of Drugs
- Dot Smith, CEO Recovery Connections, Middlesbrough
- Jardine Stewart, CEO Scottish Recovery Consortium
- Presentation and Q&A at 5th East Riding Recovery College Meeting
- Mike Wheatley, Home House Recovery Prison
- Prof David Best, University of Derby
- Substance Misuse Workforce Meeting, DHSC
- Prof John Kelly, Recovery Research Institute, Harvard University
- ESH Works Residential Rehabilitation Service in South Warwickshire
- Teleconference with Wendy Dossett and Dot Turton on Recovery Campus
- Alice Wiseman, Director of Public Health in Gateshead and Chair of ADPH Drug and Alcohol Group
- Roger Howard, Chair of Build on Belief, London
- Alcohol Clinical Guidelines Meeting, Public Health England
Recovery Connectors Group
Prof David Best, University of Derby
Stuart Green, Aspire, Doncaster
Dave Higham, Well Community, Cumbria
Michaela Jones, Scottish Recovery Consortium
Tim Leighton, Action on Addiction, Bath
Tim Sampey, Build on Belief, London
Jardine Simpson, Scottish Recovery Consortium
Dot Smith, Recovery Connections, Middlesbrough
Stephen Youdell, Double Impact, East Midlands
