Use of Health and Disability Benefits
Published 15 March 2023
DWP research report no.998
A report of research carried out by National Centre for Social Research on behalf of the Department for Work and Pensions.
Crown copyright 2023.
You may re-use this information (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit The National Archives or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email psi@nationalarchives.gov.uk.
This document/publication is also available on GOV.UK.
If you would like to know more about DWP research, email socialresearch@dwp.gov.uk
First published July 2023.
ISBN 978-1-78659-326-9
Views expressed in this report are not necessarily those of the Department for Work and Pensions or any other government department.
Executive summary
This report presents findings from a large-scale qualitative study exploring how health and disability benefits (including Personal Independence Payment, Disability Living Allowance, Employment and Support Allowance and Universal Credit) are used by recipients alongside other sources of provision and support to meet health and disability related needs.
Drawing on data from in-depth interviews with 120 participants across England, Scotland and Wales, the report provides an overview of additional needs stemming from participants’ health conditions and disabilities; how these needs are met; the role and uses of health and disability benefits in meeting needs and participants’ suggestions for improvements to support available for people with health conditions and disabilities.
Participants of this study had a broad range of health conditions and disabilities that varied in type and severity and they commonly had multiple conditions. Their financial circumstances varied widely and were affected by a range of factors, beyond simply their level of income. These factors included: the level and stability of income; debt levels; the numbers and types of health condition in the household; housing type and quality and proximity to healthcare.
Participants’ health conditions and disabilities prompted additional health-related needs across all areas of their lives including personal care, treatment and aids, support within the home, support going out and help with social participation. These additional needs often resulted in extra costs, ranging from health-specific costs such as for care, medical equipment or therapies, to increased essential day-to-day living costs such as for utilities, clothing and transport. Those with severe or multiple conditions often had more needs, or more consistent needs, than those with less severe conditions or single conditions. However, some participants, particularly those with mental health conditions, had needs such as emotional support, which were less immediately visible, despite having a significant impact on their lives.
Health and disability benefits, alongside other income streams, helped to meet almost all identified areas of additional need relating to health conditions and disabilities. However, informal support networks, health and social care services and the community and voluntary sector also played an important role in helping to meet additional needs.
Health and disability benefits were incorporated into household finances in two main ways: pooled with other income or treated distinctly. The precise use of health and disability benefits was obscured when they were pooled with other income. This approach was widespread across the sample. This meant it was not always possible to identify how health and disability benefits were used to help meet needs. When looking at household income as a whole, the most significant expenditure was on essential day-to-day living costs, including utility bills, groceries, mortgage/rent payments and car expenses.
Health and disability benefits also played a specific role in meeting additional needs through access to passported benefits, such as free prescriptions and support from local authorities with travel and parking. The Motability Scheme helped to meet participants’ travel needs through either making access to a car more affordable, providing a good quality, reliable vehicle; or enabling participants to leave the house independently. Nonetheless there were participants in the sample who were eligible but chose not to use the scheme.
The way in which benefits were used was highly influenced by the wider context of resources available to participants, including their financial circumstances, availability and awareness of free formal support and the strength of their informal support networks. These factors also influenced the degree to which additional health-related needs were met, with those with limited financial resources having to prioritise essential day-to-day living costs over other health-related needs. However, participants across the financial spectrum described a range of unmet needs in relation to social participation and mental health support.
Participants made a number of suggestions for improving support both from DWP and other agencies. Suggestions included greater awareness-raising and signposting to benefit entitlements, enhancing services provided by Jobcentre Plus (JCP) and increasing the amount of certain benefits and giving claimants more choice over when, how frequently in and in what way payments are made.
This research shows that for this group health and disability benefits are a key element of the support that is available. For those with restricted financial circumstances they offered a regular income which provided reassurance that some of their essential day-to-day living costs would be met. However, some of this group reported that they were still unable to meet essential living costs such as food and utility bills.
Health and disability benefits were also key in passporting to other essential benefits such as free prescriptions and support from local authorities, such as free travel. Among those with more financial resources their importance centred more fully on covering emotional wellbeing needs and future-proofing for younger claimants living with their parents.
Acknowledgments
The authors would like to thank Department for Work and Pensions colleagues, particularly Yvette Hartfree and Joshua Meakings who managed the project and provided valuable input and support throughout. We would also like to thank Lucy Glazebrook and Clare Morley for their input and support.
We would also like to thank Professor Roy Sainsbury of York University for providing his expertise and support throughout the project.
We are also grateful to colleagues Mehul Kotecha, Emma Forsyth, Irene Miller, Amelia Benson, Laura Izod, Hannah Biggs, Maria David, Georgia Lucey, Josh Vey and freelance consultant Andrew Thomas for supporting the project and conducting the project fieldwork.
Finally, we would like to thank all the people who gave up their time to participate in this research and share their experiences with us.
The authors
Alison Beck is a Researcher at NatCen
Thomas Barber is a Researcher at NatCen
Malen Davies is a Research Director at NatCen
Ella Guscott is a Researcher at NatCen
Dr Helen McCarthy is a Senior Researcher at NatCen
Dr Martin Mitchell is a Research Director at NatCen
Nilufer Rahim is a Research Director at NatCen
Lana Yee is a Research Assistant at NatCen
Glossary of terms
Additional health-related costs – includes additional expenses incurred because of a health condition or disability. These relate to clothing, transport, utilities, dietary requirements, medical goods/equipment, personal care, home help/ support and social participation.
Carer’s Allowance – A benefit for people who are giving regular and substantial care of at least 35 hours a week to disabled people in receipt of a qualifying extra-costs disability benefit. Carer’s Allowance is a taxable benefit.
Child Tax Credit – Paid to parents responsible for at least one dependant under the age of 16. Child Tax Credit is also available to parents responsible for dependants under the age of 20, so long as these children are in eligible education or training. It is being replaced by Universal Credit.
Council Tax Support – Each local council is responsible for operating their own Council Tax Support scheme, so the amounts of support given across the country may vary.
Disability Living Allowance (DLA) – a tax-free, non-means-tested benefit that contributes towards the extra costs of long-term ill health or a disability for disabled people under the age of 16, or who were aged 65 or over on 8 April 2013 who need help with mobility or care costs. DLA is being phased out for people who were aged 16-64 on 8 April 2013 or who reach the age of 16 and claimants are being invited to claim PIP.
Employment and Support Allowance (ESA) – A type of unemployment benefit offering financial support to people who are out of work due to long-term illness or disability. People claiming ESA are placed into two groups depending on the extent to which their illness or disability affects their ability to work. Its’ non-contributory element (income-related ESA) is being replaced by Universal Credit while its contributory element (contribution-based ESA) is being replaced by New Style ESA.
ESA Work-Related Activity Group (WRAG) – The ESA Work Related Activity Group is for contribution-based or income-related ESA claimants whose Work Capability Assessment outcome considers that they have limited capability for work but will be capable of work at some time in the future and who are considered capable of taking steps towards moving into work (work-related activities). People are required to have regular interviews with an adviser and undertake work-related activities. Its’ equivalent in Universal Credit and New Style ESA is known as the Work Preparation Group.
ESA Support Group – The ESA Support Group is for contribution-based or income-related ESA claimants whose Work Capability Assessment outcome considers they have limited capability for work and work-related activity. People in this group are not required to take part in work-related activities. Its’ equivalent in Universal Credit and New Style ESA is known as the No Work Related Requirements group.
Essential day-to-day living costs – these include housing, utilities, food, transport and clothing costs.
Housing Benefit – A means tested, income related benefit, paid to contribute to the rent for people of both working and pension age, in or out of work. Universal Credit is replacing Housing Benefit for most working age claimants.
Income Support – A type of benefit paid to support people on a low income who are not eligible for ESA or Jobseeker’s Allowance. It is being replaced by Universal Credit.
Jobcentre Plus Work Coach – Front-line DWP staff based in Jobcentres who support claimants into work by challenging, motivating, providing personalised advice and using knowledge of local labour markets.
Motability Scheme – A scheme open to recipients of the mobility component of DLA or PIP at the higher or enhanced rate. Eligible claimants who wish to join the scheme exchange part or all of this benefit to lease a car, accessible wheelchair car, mobility scooter or powered wheelchair.
Passported benefits – Claimants who are on out-of-work means tested benefits or tax credits are also eligible for a range of other support including free prescriptions.
Personal Independence Payment (PIP) – is a tax-free, non-means-tested benefit that contributes towards the extra costs of long-term ill health or a disability for working age people (16 to the day before State Pension age when first claiming) who need help with mobility and/or daily living costs. It replaced DLA for working age people and is available to those both in and out of work.
Scottish Independent Living Fund (ILF) – a fund to support disabled people with high support needs in Scotland.
Universal Credit (UC) – A payment to help with living costs for people on low income or out of work. UC has replaced, for most claimants, six means-tested benefits and tax credits: Child Tax Credit; Housing Benefit; Income Support; income-based Jobseeker’s Allowance (JSA); income-related Employment and Support Allowance (ESA) and Working Tax Credit.
Working Tax Credit – A national benefit paid to workers who are employed for a certain number of hours a week and have an income below a certain level. Also includes support for those who have childcare costs for children they are responsible for. It is being replaced by Universal Credit.
List of abbreviations
DLA - Disability Living Allowance
DWP - Department for Work and Pensions
ESA - Employment and Support Allowance
JCP - Jobcentre Plus
PIP - Personal Independence Payment
UC - Universal Credit
1. Introduction
This report presents findings from a large-scale qualitative study, carried out by NatCen Social Research on behalf of the Department for Work and Pensions (DWP). This report contributes to the evidence base on the experiences of disabled claimants and how health and disability benefits are used in order to inform the design and delivery of future services.
1.1 Context and aims
In recent years the Government has committed to improving support for disabled people and building an evidence base to inform the design and delivery of future services. DWP has announced its intention to publish a Green Paper which will set out how the Government will continue to improve the system, now and in the future, to support disabled people back into work when ready and live independently.
This report has been commissioned as part of this agenda and explores how health and disability benefits, alongside other sources of provision and support, are used by claimants to meet their health and disability related needs.
The key aim of the research was to examine:
- How claimants incorporate different benefits into their household budgeting;
- How they spend these benefits and
- What drives these spending behaviours.
The health and disability benefits explored in this research include those that are intended to help with some of the extra costs of long-term ill health or disability (Personal Independence Payment (PIP) and Disability Living Allowance (DLA)) and those that are intended to help with living costs for those who are out of work (Employment and Support Allowance (ESA) and Universal Credit (UC)).[footnote 1]
1.2 Research design
The study adopted a qualitative approach, using in-depth interviews, each lasting up to 90 minutes. The majority of interviews were conducted face-to-face in participants’ homes, or a location chosen by them (a minority requested an interview over the phone). Interviews took place between August and November 2019.
A topic guide, designed in collaboration with DWP, was used to guide interview discussions (see Appendix A.3). The themes covered included:
- Participant background and contextual information;
- Overview of finances, including key forms of expenditure and debt;
- Impact of health condition or disability on day-to-day life;
- How health-related needs are met and
- Overall views on quality of life.
A purposive approach was used to design the sample of 120 achieved interviews. The interviews were clustered in eight locations in England, Scotland and Wales, encompassing rural villages, rural towns, urban towns and a major urban conurbation. The sample included individuals receiving different combinations and rates of benefits, with a variety of health conditions or disabilities. To ensure the achieved sample included participants with conditions that varied in severity, DLA/PIP rates and ESA/UC groups were used as a proxy to categorise the severity of conditions as high, medium or low. Participants were aged 18 to 64 and included an even split of men and women. While most of those in the sample were not working, a number of participants were in paid employment. A breakdown of the sample and further detail on how the severity levels were defined is given in Appendix A.1 of this report.
Accessibility was a key consideration in the design of the research. Participants had the option of taking part independently (n=77); having a ‘proxy’ interview whereby a formal appointee, relative or carer participated on their behalf (n=16); or participating in a paired interview with a relative, friend or support worker/carer present in a supportive capacity (n=27).
A Research Engagement Group convened by DWP and consisting of expert practitioners working in the field of health and disability was consulted on the research design. The study was subject to ethical review by NatCen’s in-house Research Ethics Committee.
The data was analysed using NatCen’s Framework approach which allows in-depth exploration of the data by case and by theme.[footnote 2]
1.3 Reporting conventions
The report avoids giving numerical findings, since qualitative research cannot support numerical analysis. This is because purposive sampling seeks to achieve range and diversity among sample members rather than to build a statistically representative sample and because the questioning methods used are designed to explore issues in depth within individual contexts rather than to generate data that can be analysed statistically. What qualitative research does do is to provide in-depth insight into the range of experiences, views and recommendations. Wider inference can be drawn on these bases rather than on the basis of prevalence.
Verbatim quotations and case illustrations are used to illuminate the findings. They are labelled to indicate gender, age and whether the quote is from a proxy participant. Further information is not given in order to protect the anonymity of research participants. Quotes and case illustrations are drawn from across the sample.
1.4 Overview of the report
The findings from the research are presented in the following chapters:
Chapter 1: About the participants
Chapter 2: Financial circumstances and money management
Chapter 3: Areas of additional need
Chapter 4: How additional needs are met
Chapter 5: Drivers for how health and disability benefits are used
Chapter 6: Participants’ suggestions for improvements
Chapter 7: Conclusions
2. About the participants
This chapter describes the lives of the study participants in receipt of health and disability benefits. It outlines their characteristics and their varied life circumstances to contextualise the research findings in subsequent chapters of this report.
Key findings
-
Participants in this study had a broad range of health conditions and disabilities that varied in type and severity. Having more than one health condition was widespread across the sample.
-
Participants either lived alone, with others in shared housing, in supported accommodation or with family. The first three groups relied more heavily on care and support from outside their family.
-
Levels of social interaction fell into three broad categories: no social interaction, interaction with household members and close friends only and interaction with the wider community.
-
Participants with severe mobility problems were receiving social care support. Social care support was accessed through local authority funding, the Independent Living Fund Scotland and charitably funded specialist nurses.
-
It was only possible to include eleven people in the study who were in paid work. Their jobs tended to be low-paid, low-skilled and part-time or flexible, although some participants were in full-time or skilled work. Job flexibility was key in maintaining employment. Participants not in work ranged from those not capable of work due to their health condition or disability to those capable and actively seeking work.
-
Four key factors influenced participants’ sense of wellbeing: participants’ health conditions, their financial circumstances, their levels of social interaction and their outlook on life.
2.1 Health conditions and disabilities
2.1.1 Types of health conditions and disabilities
Participants described a vast range of health conditions and disabilities which can be grouped into four types of conditions illustrated in Figure 1.1
While some participants had just one health condition or disability, others had several conditions of the same type, or multiple conditions or disabilities across two or more types. Having more than one health condition and/ or disability was widespread across the sample.
Figure 1.1 Types of health conditions and disabilities
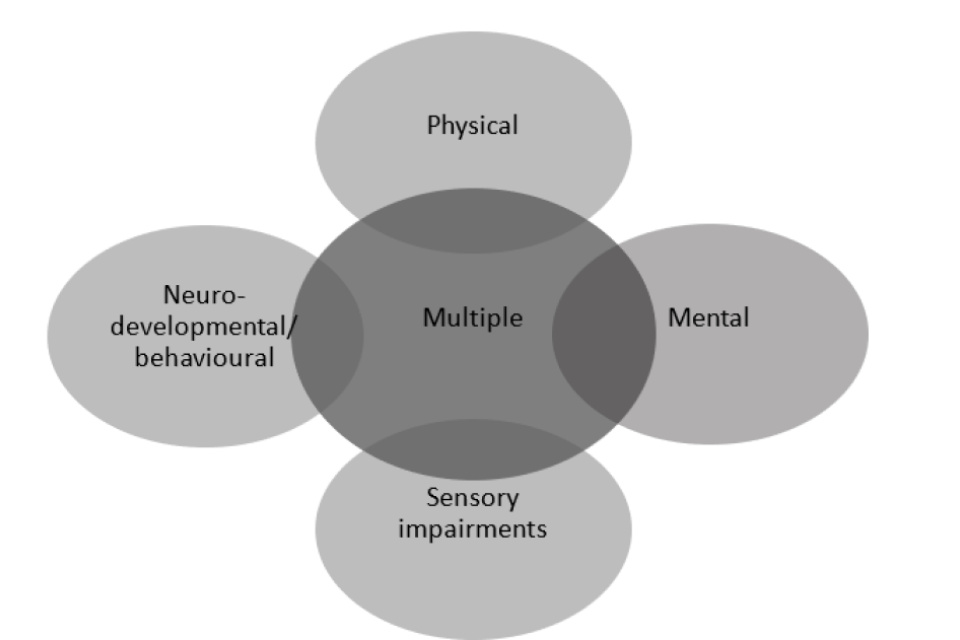
Text only version of figure 1.1:
- Physical
- Neuro-developmental/behavioural
- Mental
- Sensory impairments
- Multiple (combination of above)
The range of health conditions and disabilities included in the research by type of condition can be found in Appendix A.2.
There were four different ways that participants reported diagnosed and perceived links between their health conditions, these were:
- Conditions being or appearing unrelated;
- Conditions where one condition was a known risk factor for another;
- Conditions that were directly or indirectly causally linked or believed to be; or
- Conditions that were collectively caused by an adverse event or incident.
The daily experience of health conditions and disabilities was described as either improving, stable, fluctuating, or progressive. Improving physical and mental health was related to new or better managed treatment, or to a period of rest and recovery. Stable conditions included learning disabilities, unchanging sensory impairments and physical conditions with persistent mobility impairment and/ or constant pain. Fluctuating conditions were characterised by differing levels of pain, mobility, mental state and/or degree of sensory impairment. Progressive conditions showed worsening symptoms over time and were in some cases terminal.
2.2 Household circumstances
Participants broadly described four types of household circumstance which along with other factors, affected their level of perceived care and social support. These were:
- One-person households – claimants living by themselves;
- Claimants living in shared households – for example, as a lodger, or several people sharing the cost of a home (usually unrelated to each other);
- Claimants in supported living or residential care and
- Claimants living with other family members – including those living with partners and single parents with dependent or (adult) non-dependent children.
The first three types of households were more heavily reliant on care and support from outside their family. Participants in supported living stressed the importance of receiving regular formal care or support from an on-site carer, or someone they could call if they needed assistance. Those living with other family members emphasised the difficulties they would face in relation to their care and financial circumstances if they lived alone.
2.3 Social networks
Informal support networks, and the ability for participants to build them, was important in terms of whether their additional health and disability-related needs were met (see chapters 5 and 6 for further details). The level of social interaction, social support or social isolation that participants felt reflected the household circumstances described above, but also a range of other factors. These were:
- Whether participants enjoyed spending time by themselves or with others, including their own family;
- Proximity of their home to family and/ or friends, particularly in terms of their ability to travel easily between them;
- The accessibility of public spaces, including how accommodating they were to participants’ disabilities;
- Financial constraints on their ability to socialise where a cost or charge was involved;
- The ability and desire to involve themselves in activities or events that would enhance their social networks (e.g. volunteering, attending places of worship, going to workshops or conferences) and
- Only being able to socialise on ‘good days’ where they had a condition that fluctuated, or as their condition worsened.
These factors interacted to produce three patterns of social interaction and support networks:
No social interaction
Participants who said they had no social interaction tended to be living in one-person households. They often had no (or infrequent) visitors, but the extent to which this made them feel socially isolated varied. For some participants being alone was their preference. Others described feeling socially isolated, despite living with family members.
Interaction with household members and close friends only
Participants with severe mobility issues interacted only with people in their immediate household (e.g. immediate family or people in supported housing). These participants felt restricted because of the additional planning they had to undertake to establish the accessibility and suitability of social spaces when socialising or attending events, many of which were not found to be accommodating. Having a visual impairment could also limit socialising beyond family members. In some cases, participants were restricted to their home because they felt embarrassed about their health condition or disability, either by poor accommodation of their needs in public spaces, or negative reactions to them from other people.
Interaction within the wider community
Here, participants described higher levels of social interaction with family, friends and the wider community within and outside their immediate household. They expressed their good fortune in having the ability to engage with external networks and noted that without this, they feared boredom and anticipated feelings of social isolation.
Nonetheless, loneliness and isolation could still be experienced by participants with this pattern of social interaction if they had fluctuating conditions or when their condition worsened.
2.4 Social care
The research sought to understand where social care support was accessed and how it was used to help participants meet their health and disability related needs.
Twelve participants said that their needs were being met additionally through social care. These participants had severe mobility problems which meant they could not move around by themselves; conditions such as Alzheimer’s required participants to have 24-hour care; or learning disabilities which meant they were given access to a day care centre provided by their local authority.
Participants were not always clear or explicit about the way in which their social care was funded. Sources included local authority funding, the Independent Living Fund Scotland and specialist nurses funded charitably (e.g. Admiral Nurses who support families living with a family member with dementia). It was unclear whether other sources of care were funded as social care or as health care via the NHS. These sources included an incontinence nurse, occupational therapy and physiotherapy.
The types of social care discussed were:
- Residential care in care homes or retirement villages, sometimes with places funded by local authorities;
- One or more carers funded by local authorities coming into the participant’s home to dress, support them in going to the toilet, wash and feed them;
- Attendance at a local authority funded day care centre, regularly or occasionally, to occupy and stimulate participants and/ or provide respite for their carer;
- Receipt of funding for and installation of, adaptations to their home.
2.5 Work
As PIP is not a means-tested benefit, people are entitled to work while claiming PIP. ESA claimants can also do permitted work to help them make a gradual move into full-time work. This means people claiming ESA can work for less than 16 hours per week with earnings of up to £140 per week (April 2020), for an indefinite period, without it affecting their benefit entitlement. UC claimants in the Work Preparation and No Work Related Requirements groups can have earnings up to a work allowance threshold (which varies depending on claimants’ circumstances- the allowance is higher if they have housing costs or are in the No Work Related Requirements group) without it affecting their benefit award. Any earnings above this work allowance threshold are tapered at 63 per cent.
The research sought to include both participants who were in paid work and those who were not, to achieve a diversity of circumstances and experiences and understand how health and disability benefits were used by those in work. However, it was only possible to include eleven working participants, as very few who met the inclusion criteria for the research were in paid work. They were typically receiving PIP at the standard rate, except one who received PIP at the higher rate. One participant regularly received UC alongside PIP. Another participant only received UC occasionally, when they were between jobs.
Nature of employment
Participants in work tended to be in low-paid, low-skilled, part-time and/or flexible work, on an employed or freelance basis. Although there were examples of participants in full-time or skilled work.
Low pay was associated with low hourly wages and part-time hours. Among those on low pay were participants receiving working tax credits, housing benefit or council tax reductions to compensate for their low income.
Participants’ working patterns varied, from working one day a month on average, to 40 hours a week. On the whole participants said they preferred to work part-time because full-time work would be too tiring or painful (for those with physical health conditions) or stressful or overwhelming (for those with mental conditions). Limitations associated with health conditions were also combined with other reasons for working part-time, including:
- Believing that they would not be eligible for benefits if they worked more than 15 hours a week;
- Because they were raising a child or had other caring responsibilities; or
- Because they were also a full-time student.
Those who had flexibility at work said this was important because it enabled them to organise their work to coincide with periods of relatively good health. Some participants (who were self-employed or signed up to an agency) could choose whether to accept offers of short-term work based on their health at the time. Others worked a set number of hours every week but had flexibility about when to do those hours.
Some of those who were working had conditions that fluctuated daily. There were three reasons why participants managed to hold down a job despite this:
- They had an understanding employer;
- Their hours were flexible so could be adjusted when needed; or
- They were able to take the occasional unpaid sick day because PIP or a partner’s earnings provided a financial cushion.
Aspirations and barriers to work
Participants who were not working fell into one of three groups in relation to their circumstances and aspirations:
- Not capable of any form of work now or in the future due to the severity of their condition(s)/ disability;
- Not capable of paid work currently due to their condition(s)/ disability but could be in future if their health improved (this included participants who had volunteered as a stepping-stone to possible future work); or
- Capable of some forms of paid work now, with some actively looking for work.
Among those who felt capable of paid work, several barriers to work or to seeking work were given. These were:
- The experience or perception that employers would not employ them, or that if they did they would not be willing to make the adjustments necessary to employ them (especially in relation to fluctuating conditions);
- Lacking confidence about working and being a reliable employee; or
- Mistakenly believing that work would affect entitlement to PIP.
Nevertheless, a group of participants who were not working expressed the desire to work because they felt that work offered positive benefits such as relief from boredom, a sense of pride and contact with the outside world.
This case illustration provides an example of a participant who had to stop work because of their condition and had not found work since.
The participant suffers from uncontrolled seizures meaning she cannot be left alone. She has tried 13 different medications to control the seizures but nothing has worked; she is now awaiting brain surgery. Twenty years ago, she worked in a supervisory role in a supermarket but when her seizures worsened, she had to leave because of the risk posed by using equipment. Then she got a job working at a friend’s café, but when a new owner took over the business, they “couldn’t handle” the seizures and she was let go. After that, she started a job with night shifts, but the shift patterns made her seizures worse, so she had to leave that job. Finally, she was offered a new job in a café, but the owner decided she could not employ her because she was an insurance risk. Each time she has an interview and mentions that she has uncontrolled seizures she finds that she has been unsuccessful in her application. She is due to have surgery in the future which is hoped to stop the seizures. If this is successful she is keen to try and begin looking for work again.
Female, 30-49
2.6 Wellbeing
Where wellbeing was concerned participants ranged from being positive, neutral to more negative. Feelings of negativity were widespread across the sample and ranged from participants ‘feeling down’ to wanting an end to their life. Four main factors, often experienced in combination, affected participants’ sense of wellbeing:
-
Number and type of health conditions: those with a poor sense of wellbeing tended to have multiple health conditions, including mental health conditions for which they were not receiving treatment, or which had not stabilised. Those whose wellbeing fluctuated regularly had mental health conditions such as depression, anxiety or bipolar disorder.
-
Financial circumstances: participants who reported having positive wellbeing described themselves as financially comfortable and were often almost entirely debt-free. In contrast, persistent and significant money worries were common among those with poor wellbeing. This included people who were in debt and a group who were worried about their financial situation worsening in future.
-
Level of social interaction: participants with lower levels of social interaction tended to have a poorer sense of wellbeing, which was linked to feelings of social isolation and sometimes to depression. However, this was not always the case. Receiving good mental health treatment or support, owning a pet and having access to the Internet and digital entertainment could also help improve a sense of wellbeing where levels of interaction were lower.
-
Outlook on life: a group of participants said that although their quality of life was poor, they were grateful that things were not worse and tried to maintain a positive outlook on life. They had either come to terms with their poor health or were favourably comparing their current health to much worse health in times past. Another group, who had poorer wellbeing, described feeling powerless to improve their circumstances. They felt it was pointless to imagine a better life because their health conditions made that an impossibility.
3. Financial circumstances and money management
This chapter describes participants’ financial circumstances and the factors that affected them. It explores how claimants incorporated health and disability benefits into their household budgeting and how they managed their income in order to understand what role health and disability benefits played and the factors that drive how they are used.
Key findings
- There were a range of factors that affected participants’ overall financial circumstances including the level and stability of their income; their debt level; the numbers and types of health condition in the household; their housing type and quality and their proximity to healthcare.
- Participants with limited financial resources beyond their health and disability benefits reported that they were often unable to meet essential day to day living costs which caused difficulties with their household budgeting. Those with additional resources outside their benefits were better able to budget to meet essential and additional health related costs.
- Health and disability income was incorporated into households in two main ways: pooled with other income or treated separately. Neither way appeared to be directly linked to a more successful money management approach, although those treating their benefits distinctly did so as part of budgeting techniques.
- Health conditions affected participants’ ability to manage their money in a range of ways and in some cases meant participants were unable to manage their money themselves.
3.1 Financial circumstances
Participants’ financial circumstances varied widely and were affected by a range of factors, beyond simply the level of their income. The extent to which participants could meet essential day-to-day living costs[footnote 3] as well as their additional health-related costs[footnote 4] varied and was influenced by their financial circumstances. Participants fell on a spectrum in this regard. At one end were those with the most restricted financial resources, these participants were sometimes unable to afford essential day-to-day living costs, such as rent, heating or food and almost always unable to pay for additional health-related costs, such as additional therapies or medical goods. At the other end were participants with more financial resources who could afford all essential and additional health-related costs, such as therapies, equipment and higher additional everyday expenses. Where participants fell on this spectrum was influenced by the factors discussed below.
3.1.1 Level and stability of income
One of the key factors impacting participants’ financial circumstances was the value of their personal and wider household income streams and the extent to which they had other assets to draw upon.
Health and disability benefits
The research was designed to include participants on at least one of four main health and disability benefits: DLA or PIP; ESA or UC; or a combination of these. As was described in chapter 1, the research also included a range of different award levels, meaning that the value of health and disability benefits that participants were receiving varied considerably. In some cases, participants were not always aware of which benefits they were receiving or the rates that they were paid at.
Among participants who were in receipt of just one benefit type i.e. UC/ESA or PIP/DLA, this was largely due to being ineligible for the other type. Some participants may have been eligible for the other benefit, but were either unaware of this, or had decided against claiming because they wanted to avoid further contact with the benefit system or believed they would find work soon. In some cases, claimants said that past claims had stopped without participants knowing why.
Other income streams
In addition to health and disability benefits, some participants had a number of other income streams including: pensions (from the participant or someone else); earnings (from the participant or someone else); other benefits that the participant or another member of the household received (Income Support, Working and Child Tax Credits, Housing Benefit, Child Benefit, Carer’s Allowance) and other types of income (income protection insurance, rental income, student loans and investment income).
The level of income in households did not neatly align with differences between working and non-working households. In working households, the most significant income stream depended on the numbers of people in work and the type of work being done. Health and disability benefits were the most significant income streams where only one person was working, was on a low income and/or was working part-time. Often if family members were working part-time, this was because they had caring responsibilities for the participant, which prevented them from taking up full-time employment.
Stability of income
Stability of income was also a factor that determined financial circumstances alongside the level of income. While health and disability benefits provided a certain reliability of income, decreases in award levels following reassessments or transitions between different benefit types (e.g. from DLA to PIP) could cause participants to turn to borrowing. For in-work households, the unpredictable nature of health conditions could also lead to fluctuating income levels, as participants took unpaid leave due to ill health or family members took unpaid leave to provide care. This could also lead to households experiencing a shortfall in their finances.
3.1.2 Levels and types of debt
Debt was widespread across the sample and covered a range of types of borrowing. These included bank loans, credit cards, rent and utility arrears, doorstep lending, catalogue debts, DWP budgeting loans[footnote 5] or overpayments and borrowing from family or friends. Debt was considered unmanageable where participants listed repayments as a significant expenditure and/or where they did not have an active debt management plan in place. Unmanageable debt was found across in-work and out-of-work households and often comprised multiple forms of debt.
This case illustration provides an overview of the level and forms of debt participant experienced.
The participant lives with her two daughters aged 10 and 3. She receives PIP, alongside Income Support, Child Benefit and Child Tax Credits. She has suffered from anxiety and depression all her life, with epileptic seizures beginning nine years ago. She is £8,000 in debt and 70-80% of her income is used to pay debt. The debt was incurred through having to fix damage to her house caused by tenants when she was staying with her parents during a period of particularly poor health. What’s left of her income goes on food, bills and her children.
Female, 30-49
There were a range of reasons as to why participants had fallen into debt, some of which were linked to their health condition or disability. The most common reasons included:
- Unexpected costs (such as for funerals, new white goods);
- Special occasions with additional costs (such as Christmas or birthdays);
- Change in circumstances (for instance job loss or periods of homelessness);
- Issues with financial management (sometimes linked to health conditions) and
- Changes to benefit levels (as result of re-assessments, sanctions, or overpayments).
3.1.3 Number and type of health conditions and disabilities
Households in which more than one individual had a health condition or disability tended to have higher costs and more restricted financial resources. This included households where both partners had health conditions or where a parent and dependent had health conditions.
3.1.4 Housing tenure
Housing tenure and quality also emerged as a factor that impacted on participants’ overall financial circumstances. Participants who were owner-occupiers, particularly those who had already paid off their mortgage, tended to have greater financial resources, as did those who were living in accommodation provided by family members. Those with more restricted resources included those in private rented accommodation and those in socially rented accommodation where housing benefit did not cover their full rent. The quality of housing also impacted on utility costs, with poorly built or insulated housing leaving some participants in fuel poverty. In particular, those in rural areas often discussed the additional costs of heating oil.
3.1.5 Proximity to healthcare services
Proximity to healthcare services was another factor that impacted on participant’s overall financial circumstances. Some participants had a high number of healthcare appointments and so longer distances to doctor’s surgeries, health centres and hospitals meant participants incurred higher travel costs, particularly affecting those who lived in rural areas. This was either as a result of unreliable public transport meaning that participants had to take taxis, or long distances meaning that multiple forms of transport had to be used, with several separate fares needing to be paid each time to reach their healthcare appointments.
3.2 How health and disability benefits are incorporated into household budgets
Health and disability benefits were incorporated into household finances in two main ways: they were either pooled together with other forms of income and spent on general expenditure or treated distinctly to cover specific costs[footnote 6]. However, the different approaches were not completely distinct and did not always determine how spending was prioritised.
3.2.1 Pooling income
Pooling of income was widespread across the sample. This approach was used in both in-work and out-of-work households, across the range of health and disability benefits and award levels covered in this research and in households with varying types and numbers of income streams. Pooling occurred at the individual level (i.e. the participant pooled their health and disability benefit with their own other income streams such as earnings, pensions, or other benefits) and at the household level (i.e. income was pooled with other members’ income streams either earnings, pensions, or other benefits).
Having one ‘general pot’ was seen as the common-sense approach and so the reasons for doing so were not always fully articulated. However, specific explanations given included that additional health-related costs had to be paid for when they arose rather than when health and disability benefit payments were made and that income streams were too small to divide up.
The thing is, we have such a limited income that at the end of the day, it’s absolutely pointless putting money into little pots and saying, ‘Oh, that’s for so-and-so and that’s for something else’. (Male, 50+)
3.2.2 Treating health and disability benefits distinctly
Participants who treated their health and disability benefits distinctly also had a range of benefits and financial circumstances and included in-work and out-of-work households. However, there were three explanations for treating income from health and disability benefits distinctly:
- Firstly, health and disability and other benefits were conceptualised as serving specific purposes. For example, ESA covered household costs, PIP covered health-related expenses and child benefits and child tax credits were for children. In these instances, benefits were used to structure budgeting approaches or to reflect participants’ perceptions of the intended purpose of different benefits.
- Secondly, health and disability benefits were used for different expenses based on the timing of each payment. Here, different payment dates of health and disability benefits, or more frequent payments of the same benefit (e.g. fortnightly ESA payments) were used as a money management tool, forming the structure of participants’ budgeting processes.[footnote 7]
- Thirdly, health and disability benefits were allocated to specific needs, such as costs relating to health or wellbeing (e.g. gym classes), social activities, transport and pets, which helped with wellbeing. This approach was used in households where wider living costs, such as bills and food, were covered by a parent or partner. If financial resources in the household were limited, health and disability benefits were sometimes used to contribute to living expenses, with the remainder spent specifically on participants’ additional needs. Among this group were participants who could not manage their own finances due to their health conditions or disabilities. In these cases, family members were sometimes putting health and disability benefits aside as savings to cover future care needs.
These different approaches to treating health and disability benefits distinctly were also not always completely clear cut and in some circumstances, shortfalls in one area were simply covered by another.
3.3 Approaches to money management
The way health and disability benefits were incorporated into household budgets reflected to some extent how participants managed their money. This varied from very passive management with virtually no strategies to manage their money, to very active management with close monitoring of money and careful budgeting.
3.3.1 Passive management
Participants in this group who managed their income passively spent money when they received it. They had little idea of the state of their finances and reported very few techniques to keep track of their income and expenditure. This group included participants who had little grasp of which benefits they received or the rates of those benefits. They were either pooling their income or had health and disability benefits as their only income source.
Two main barriers to actively managing their money were reported: limited income which made them feel that budgeting was not worthwhile and health conditions that affected their ability to manage their money (see 3.3.3). People who managed their money passively were most likely to be unable to pay for additional health-related costs or sometimes essential living costs. Some participants in this group reported that they borrowed from friends and family or support services, such as foodbanks, to get by.
3.3.2 Active management
Active management ranged from those who had a general overview of their income and had some loose form of management, to participants who had detailed techniques and strategies[footnote 8] and were keeping a close eye on their money. Active management was found both among those who pooled their health and disability income with other income streams and among those who treated it distinctly. Active management did not always fully align with better financial circumstances, in some cases it was a response to having a low income.
3.3.3 The impact of health conditions on money management
Individuals with both physical and mental health conditions described how their conditions affected their ability to manage their money effectively. For instance, fatigue left participants too exhausted to budget and memory problems caused difficulties keeping track of payments. Mental health conditions meant some participants experienced a high level of anxiety in relation to their finances, while others experienced erratic and compulsive spending. Participants with sensory impairments, such a sight loss, experienced difficulties accessing information about their finances and those with neuro-developmental conditions, such as autism, found it difficult to understand the concept of budgeting as well as the costs of everyday things.
Participants responded to these constraints in different ways. For some these barriers severely limited their ability to manage their money, resulting in a completely passive approach or someone else managing their money. Others had developed a range of active techniques and strategies to try to mitigate their difficulties, for instance by noting down payments and dates.
3.3.4 Money managed by others
Finally, there were participants who did not manage their own money or only managed a portion of their own income due to their health condition or disability. Participants in this situation fell into one of three groups:
- Young claimants living with parents who were unable to manage their own money due to their health condition or disability. In these circumstances, parents managed their money and often provided some form of allowance.
- Adults, living with family, whose health condition or disability made it difficult to manage their own money and whose partner managed it for them.
- Adults who lived alone who were unable to manage their own money due to their health condition or disability, had someone external to their household managing their money as part of a paid for service.
4. Areas of additional need
This chapter identifies the additional needs that stem from participants’ health conditions and disabilities to contextualise how health and disability benefits were used.
Key findings
- Participants’ health conditions and/or disabilities gave rise to a wide range of additional needs.
- Those with severe or multiple conditions often had more needs, or more consistent needs, than those with less severe condition or a single health condition.
- There were participants with mental health conditions who had needs which were less immediately visible but had an equally significant impact on their lives to those with severe or multiple conditions.
4.1 Additional needs
The research sought to identify the ways in which participants’ health conditions and disabilities led to additional needs in different areas of their lives, to contextualise findings relating to how health and disability benefits were used, which are discussed in chapter 5.
In this chapter, the needs identified are grouped into eight broad categories described in turn below[footnote 9] . The extent and frequency with which support was needed in these areas depended on the severity of health conditions or the combined effect of multiple conditions. Specific conditions are given as examples of how additional needs arose amongst participants of this research. However, this is not to say that everyone with each named condition identified with the same needs.
4.1.1 The person
Specific dietary requirements
Physical conditions or disabilities, mental health conditions, sensory impairments and neurodevelopmental or behavioural disorders, gave rise to specific dietary needs.
There were participants who required soft, moist food or could not eat solid food, for example due to facial numbness caused by cancer. Other participants were restricted to eating very small portions or needed to follow a specific diet, such as a gluten free diet. Participants with mental health conditions such as Obsessive-Compulsive Disorder (OCD), anxiety and eating disorders, were sometimes compelled to eat specific types of food or to buy food only from certain shops, driven by a need to know exactly what was in their food.
Clothing and footwear
Participants were required to replace clothing more frequently due to soiling from incontinence from conditions such as Crohn’s disease, from ointments required by skin conditions such as psoriasis, or wear and tear caused by epileptic seizures. Side-effects of medication for those with mental health conditions, such as rapid weight gain, could also require additional clothing purchases. Loose clothing was needed to avoid aggravating skin conditions and to allow room for kidney dialysis equipment.
Participants with an uneven gait, arthritis in the foot and misaligned vertebrae required orthotics or specialist footwear. Others with limited mobility required Velcro shoes to minimise bending down to tie shoelaces or shoes with softer materials, to support their feet.
Care and assistance
Across the sample participants required assistance with eating, preparing food, bathing, dressing and taking medication.
In some circumstances conditions such as visual impairments, Alzheimer’s, epilepsy, memory loss and learning disabilities meant participants could not safely cook or prepare food independently. In these instances, participants required care and assistance to cook for them or used aids and adaptations to help with cooking. Help with bathing, dressing, going to the toilet and going to bed was also required by participants with a wide range of conditions, disabilities and impairments which affected mobility or cognition. This included conditions such as osteoarthritis, multiple sclerosis, learning disabilities and Clonus (muscular spasms).
Mental health conditions or learning disabilities could sometimes necessitate the need for others to monitor their medication, to avoid under or overdosing, or to provide reminders.
The frequency of these needs depended on the severity of participants’ health conditions and disabilities. Participants who required 24-hour care tended to have severe or multiple conditions, whilst daily or less frequent care needs resulted from single physical conditions, learning difficulties, less profound multiple conditions and conditions which fluctuated. There were also participants who had a range of health conditions or disabilities across a spectrum of severity levels who lived in supported housing, where they had their care needs met.
4.1.2 The home
Additional needs arising in the home included structural adaptations and help with chores such as cleaning, laundry, DIY and gardening.
Structural adaptations
Structural adaptations, such as walk-in showers, bath rails, chair lifts, hand rails and widened doorways for wheelchair access, were required by participants with a range of physical health conditions, including amputees and participants with various spinal and back conditions. Extra rooms were required by those needing a live-in carer or because some felt unable to share a room if they wanted privacy when dealing with physical conditions (e.g. use of a colostomy bag) or when managing neurodevelopmental disorders (e.g. autism) and mental health conditions (e.g. anxiety). Bigger, accessible bathrooms were required by those who used a wheelchair. Home adaptations were provided for those who needed them in supported living settings.
Help around the home
Help with household chores such as cleaning, laundry, DIY, gardening and ad hoc tasks like changing a lightbulb were required by participants across a range of physical and mental health conditions, neurodevelopmental and behavioural disorders and sensory impairments. This was due to symptoms such as fatigue, chronic pain, anxiety, lack of mobility, lack of motivation or memory loss making these tasks difficult.
My mobility is not good and I can’t bend like I normally could, […] I like getting into all the nooks and crannies and washing down my skirting boards and things. Things like that I would need to get my sister or one of my friends… to help me with that. (Female, 50+)
As with personal care and assistance, the frequency and extent of need varied and depended on the severity of participants’ health conditions and disabilities. For instance, those with physical health conditions that were chronic in nature, such as osteoporosis, required daily help. Others needed more light-touch support, for instance those with learning disabilities or epilepsy which caused memory loss.
4.1.3 Travel
Public transport
Public transport was particularly important for participants who did not have access to a car, could not drive or could not afford taxis to appointments, run errands or go grocery shopping.
Participants reliant on public transport sometimes needed support to access it. Participants with learning disabilities required chaperones to help with navigation and ensure they stayed safe. Wheelchair users in particular could only use accessible public transport. Participants with mental health conditions, such as bipolar disorder or neurological disorders such as autism or Tourette’s Syndrome required emotional support, as using public transport could be anxiety provoking.
She [participant’s daughter] always meets me at the station… Then she’ll walk me back to the station, see me get on my train, because I’m never good with travelling, especially trains […]. (Female, 30-49)
Car
Travel by car was the preferred option for participants who found it difficult to use public transport. This included participants who experienced unpredictable incontinence due to Crohn’s disease, those with conditions such as arthritis for which the bumps and jolts on busses caused too much pain and wheelchair users who could not always use accessible public transport.
In some circumstances, participants needed adaptations to their vehicle such as hoists or specialist steering equipment to be able to drive or be a passenger. This included those with back problems and wheelchair users, who had multiple conditions such as cerebral palsy and epilepsy.
The need to travel by car was greater in rural areas, where public transport was less available or reliable, or where taxis were too expensive due to long distances to the nearest amenities.
He can’t go on a bus because there aren’t any buses, there aren’t any trains, he can’t ride a bike, so he relies on his mother or his father for taking him places. (Male, 50+, proxy interview)
There were also participants with spinal problems or Multiple Sclerosis who used a mobility scooter to travel short distances.
Taxis
Travelling by taxi was an important alternative for participants who could not drive or who did not have friends or family who could offer lifts or accompany them on public transport.
The extent of taxi use varied, participants who could not use public transport, but did not have access to a car, used them regularly. This included participants with conditions or disabilities such as Crohn’s disease, a visual impairment, autism, PTSD and schizophrenia. Others used taxis for specific purposes or situations, such as when they were too exhausted to get public transport, or as a return journey from grocery shopping.
Attending healthcare appointments
Participants who had to travel regularly to hospital appointments incurred additional costs, such as increased mileage and hospital parking or increased taxi or public transport costs. Those who lived in more rural areas, who had to travel longer distances, incurred higher costs. This is discussed further in chapter 6.
4.1.4 Utilities
Specific health conditions and disabilities could lead to greater use of utilities such as power, gas and water.
Power and Water
Power and water were in regular use when participants had to wash clothing or bedding regularly because of incontinence from Crohn’s, leakage from colostomy bags or bleeding from skin conditions. Participants who spent a lot of time at home also cited higher use of electricity from having their television and lights on for long periods of time.
Heating
Participants across a range of physical and health conditions spent long periods of time at home and therefore needed the heating on more often. This included participants with epilepsy, whose seizures kept them at home and those who had anxiety and depression who found it difficult to leave the house. Participants with cancer or chronic pain, experienced mobility issues and limited energy levels which caused them to be housebound.
Others had conditions which caused them to become cold easily or meant they needed to stay warm. For example, cerebral palsy caused poor circulation, HIV and cancer caused shivers and COPD caused a poor immune system, meaning the heating needed to be on most of the time.
4.1.5 Medical goods/equipment
A wide range of medication, medical products and items, equipment and aids and therapies and treatments were being used on a regular basis.
Medication
The use of prescribed medication and treatments was widespread across the sample. The amount, type and regularity within which it was taken varied and depended on a participants’ health condition or disability. Medication was required to relieve symptoms and in some cases, it was life critical to take.
Medical products
Medical products in use included incontinence pads, skin treatments, food supplements and arm splints. Incontinence was related to several health conditions, including Crohn’s disease, learning disabilities, microcephaly and irritable bowel syndrome. Participants with cerebral palsy required arm splints that provided support for their hands. Skin treatments and shampoos were used by those with psoriasis.
Equipment and aids
The use of equipment and aids was widespread across the sample. Products included items to aid mobility, such as wheelchairs, hoists, ramps, walking sticks and standing frames. Participants who used these types of equipment had conditions such as paralysis, arthritis and myopathy (muscle disease). Amputees also had prosthetic legs. Bath boards and shower seats, perching stools in the kitchen and devices for putting on socks or doing up zips were needed for participants with conditions such as lung cancer, spinal conditions and chronic arthritis.
Larger equipment such as hospital beds and special chairs were used by participants with quadriplegia and misaligned vertebrae and safety products including community alarms were used by those with epilepsy, chronic arthritis, microcephaly and cancer.
Devices such as hearing aids and personal listeners for televisions were used by those with hearing loss and voice recognition equipment was used by participants with arthritis to avoid typing. Participants who were unable to communicate verbally due to conditions like quadriplegia used special communication equipment.
Therapeutic services
Participants with chronic pain, depression and sciatica accessed therapies such as cupping, acupuncture, hydrotherapy and oxygen therapy, to relieve pain.
Accessing talking therapies was also mentioned in relation to mental health conditions, which varied from regular use to use when symptoms flared.
Participants with a range of physical or mental health conditions reported that general exercise, including attending the gym or exercise classes, was also needed to manage physical health conditions and support wellbeing. In addition, animals, typically pet dogs, played a therapeutic role in supporting mental wellbeing.
4.1.6 Outside the home
Participants with a range of conditions and disabilities needed to be accompanied outside the home to attend medical appointments, run errands like shopping or banking and go to social activities.
Physical support
Some participants with physical health conditions and disabilities like multiple sclerosis or who had suffered a stroke, needed physical support to leave the house (e.g. help to get into their wheelchair) and to walk around.
Practical support
Participants with visual impairments and learning disabilities expressed the need for practical support when navigating public spaces, and some participants with chronic memory loss required practical help with shopping.
Well, I can’t get out anywhere on my own. I don’t know the times of the buses or anything, even if I wanted to go out. I just wait for [friend’s name] to take me shopping… (Female, 50+)
Emotional support
Participants with visual impairments or mental health conditions such as severe anxiety and schizophrenia required emotional support and often required someone to go with them when going out. These participants found tasks such as shopping highly stressful and anxiety provoking, and crowds caused panic attacks.
Participants with neurodevelopmental and neurological disorders also required help outside the home. Parents or support workers who participated as proxies for participants with learning disabilities explained that they could often lack a sense of danger or could be vulnerable to exploitation. They therefore needed to be accompanied out for safeguarding purposes.
She does get tired very quickly and she doesn’t walk very well, so that’s why we have the wheelchair. She’s got no sense of danger either so it’s also a safety capacity as well. No, she’s safer in the house walking around than she is outside. (Female, 18-29, proxy interview)
4.1.7 Money and administration
Support with money management was required by participants with both mental and physical health conditions, as described in chapter 3. Where participants were unable to physically write, had memory loss or experienced anxiety, help was also needed to complete forms. Participants who found it difficult to process new information, for example due to brain damage, required someone to make phone calls on their behalf.
4.1.8 Social participation / leisure
Having access to forms of entertainment and services at home, along with the ability to keep in touch with others or feel connected with the outside world, was valuable for those who were largely housebound.
Participants who spent most of their time at home due to their mental or physical health condition, such as depression, anxiety, epilepsy and chronic pain, relied heavily on the internet or mobile phones to keep in contact with friends and family or to lift their mood.
It lifts my mood. It’s not always me that rings them or goes to them. Quite often now they’ll ring me, … it’s just nice to have that human interaction, just to hear someone talking… (Female, 30-49)
The internet enabled participants to access games consoles, use laptops and watch the TV. DVDs, mobile phones and music were also used for these purposes. The internet was also used to buy groceries and other products for those who were unable to leave the house due to a physical or mental health condition. Others used the internet for online banking on their phone, meaning they could keep track of money going in and out of their account, or could transfer money between accounts easily.
There were also examples of participants keeping a mobile phone with them at all times in case of an emergency, such as a fall or accident.
4.1.9 Work
Flexibility and the ability to reduce working hours to part-time were the key needs identified amongst those in work. Flexibility was required to allow participants with mental health conditions, who were having ‘low’ days or experiencing adverse effects from their medication, to take sick leave.
In other circumstances where participants had physical health conditions, part of the reason they were able to maintain work was due to their ability to work part-time. Needs in the workplace included ensuring the work environment was accessible for those using wheelchairs. In circumstances where workplaces were not accessible, participants had to turn down job offers.
4.2 Additional needs in relation to severity of condition
This section presents case illustrations that demonstrate how health conditions prompted additional needs and how needs tended to vary according to a participant’s condition. Participants within the sample who had multiple or severe physical health conditions often had a wide variety of additional needs as a result, which were often significant in nature. On the whole, single or less severe health conditions gave rise to fewer additional needs. However, in some cases needs were simply different and could not be considered as greater or lesser due to condition type.
This case illustration demonstrates how multiple additional needs arise from having severe and multiple physical health conditions.
Participant has cerebral palsy, severe epilepsy, learning difficulties, and is profoundly deaf and partially sighted. He lives at home with his parents and brother, who also has complex physical health conditions and disabilities. He uses a wheelchair and requires 24-hour care. He has constant low-level seizure activity and has seizures every day. The type of epilepsy he has also causes gradual loss of abilities and mobility. In the home, he has a stairlift, wide doorways for his wheelchair, and a playroom with specialist play equipment. He needs help with all aspects of personal care, and because he has no speech, relies on others to interpret his wants and needs. His mother acts as his main carer, although NHS carers regularly take him out, and he has access to respite services and attends various clubs operated by the charity Mencap.
Male, 18-29
This case illustration demonstrates how a less severe physical health condition gives rise to fewer additional needs.
Participant lives at home with his partner and works part-time. He has a disease in his back which has worsened with age. His condition is chronic and causes him significant back pain and muscle tension, making it difficult to be mobile or work for extended periods. He uses a combination of rest, medication, muscle relaxants and laser treatment to manage the pain and muscle tightening. He has various adaptations in the home such as a double bannister and walk in shower. If he has a fall at home, he calls his brother to help him up, as his partner is not strong enough. At work his employer has agreed to give him additional breaks so that he can rest his back.
Male, 30-49
Participants with a single or multiple mental health condition sometimes had multiple needs which were less immediately visible, but which had a significant impact on participants’ lives and the lives of those around them.
This case illustration demonstrates how multiple needs, that are sometimes invisible needs, arise from a range of mental health conditions.
The participant lives with her husband and young children. She has psychosis and mania and in 2018 she experienced psychosis episode which lasted for a year. Due to her conditions she experiences heightened states of anxiety when left alone with the children, and also suffers from very heavy sleeping and sometimes cannot be woken. These factors mean she cannot be left alone with the children, and her husband decided to leave work to care full-time for the children and the participant. The participant’s husband is also her appointee, due to her high spending when experiencing mania. She is also not able to leave the house alone, due to experiencing severe paranoia and has to be accompanied by her husband or a family or friend.
Female, 30-49
5. How additional needs were met
This chapter discusses the range of ways in which the additional needs described in chapter 4 were met, including the role played by health and disability benefits. It also explores the uses and views of the Motability Scheme to help meet the costs of mobility.
Key findings
- A combination of general income (including income from health and disability benefits); informal support networks; health services; social services and community and voluntary sector organisations were used to help meet participants’ health-related needs.
- The most significant expenditure of health and disability benefits, alongside other income, was for essential day-to-day living costs, including utility bills, groceries, mortgage/rent payments and car expenses.
- Health and disability benefits played a unique role in helping to meet additional needs through access to passported benefits such as free prescriptions and support with travel and parking provided by the local authority.
- The Motability Scheme helped to meet participants’ travel needs through making access to a car more affordable, providing a good quality, reliable vehicle; or giving participants independence to leave the house. There were also eligible participants who did not use the scheme either because they were unable to drive, felt there was stigma attached to driving a mobility scooter, preferred to keep their PIP payment, anticipated incorrectly that another assessment might take place, or were unaware of the scheme.
5.1 How health and disability benefits are used to help meet needs
5.1.1 Main sources of support
Participants’ additional needs were usually met through a combination of the following sources of support:
- General personal/ household income, including health and disability benefits, earnings, pensions, savings, other benefits and forms of income (e.g. investment income)
- Informal support networks, primarily relatives, also friends, neighbours and faith groups
- Healthcare services, mainly the NHS (including occupational therapy), as well as private providers
- Social care services provided through the Local Authority (LA)
- The community and voluntary sector (CVS) including charities and community interest companies.
The sources of support participants drew on and the extent of their use varied widely across the sample. This mainly depended on a participant’s level of need, wider household and financial circumstances and access to and use of informal support networks. Table 5.1 summarises the sources of support used to meet each health-related need identified.
Table 5.1 How each of area of additional need was met
| Area of need | Income (inc. H&D) | Healthcare services (i.e. NHS) | LA social care services | Informal support networks | CVS |
|---|---|---|---|---|---|
| Person (Specific dietary requirements) | Paid | ||||
| Person (Clothing & footwear) | Paid | Free | |||
| Person (Care & assistance) | Paid, Paid for through funds from multiple sources | Free | Free, Paid for through funds from multiple sources | Free, Paid for through funds from multiple sources | |
| Home (Structural adaptations) | Paid, Paid for through funds from multiple sources | Free, Paid for through funds from multiple sources | Free, Paid for through funds from multiple sources | Free | |
| Home (Larger home) | Paid | Free | |||
| Home (Help around home) | Paid | Free, Paid for through funds from multiple sources | |||
| Travel (Car) | Paid | Free | |||
| Travel (Public transport) | Paid | Free | |||
| Travel (Taxis) | Paid | Paid for through funds from multiple sources | |||
| Utilities (Water) | Paid | ||||
| Utilities (Heating) | Paid, Paid for through funds from multiple sources | Paid for through funds from multiple sources | |||
| Utilities (Power) | Paid | ||||
| Medical goods (Medication) | Paid | Free | |||
| Medical goods (Products/items) | Paid | Free | |||
| Medical goods (Equipment & aids) | Paid, Paid for through funds from multiple sources | Free, Paid for through funds from multiple sources | Free, Paid for through funds from multiple sources | ||
| Medical goods (Therapies) | Paid | Free | Free | ||
| Outside the home (Appointments) | Free | Free | |||
| Outside the home (Errands) | Free, Paid for through funds from multiple sources | Free | |||
| Outside the home (Social activities) | Paid | Free, Paid for through funds from multiple sources | Free | ||
| Money & admin (Managing money) | Paid | Free | Free | ||
| Money & admin (Admin) | Free | Free | Free | ||
| Social participation & leisure (Internet) | Paid | ||||
| Social participation & leisure (In-home entertainment) | Paid | ||||
| Social participation & leisure (Aids/devices) | Paid | Free | |||
| Work (Flexibility) | Paid |
Paid for through funds from multiple sources[footnote 10].
5.1.2 The person
Specific dietary requirements
Costs relating to liquidising food and specific dietary requirements e.g. the need to eat fresh fruit and vegetables, were met by general income, including health and disability benefits. In very limited cases, health and disability benefits were used distinctly to cover these needs. Examples of this included a participant whose health and disability benefits were used to cover the cost of ready meals.
Clothing and footwear
General income, including health and disability benefits, was used among those who regularly had to purchase clothing to replace items they had soiled or spoilt. Participants often found low cost options to meet this need, such as buying items second hand. Footwear needs such as specialist or orthotic shoes were covered by the NHS.
Care and assistance
As explained in chapter 4 the level and nature of care and assistance required varied widely across the sample. Care and assistance was either provided by the local authority, through paid or free informal support networks (including faith groups) or CVS organisations. The type and combination of care and assistance sources used depended upon a participant’s financial circumstances and the extent and strength of their informal support networks.
Where participants had high levels of need and more financial resources, as a result of having additional income streams in the household, local authority care was topped up with privately funded care. In these instances, private care was financed via the household’s general income.
Participants requiring care and assistance, with limited financial resources, either received support from their local authority or accessed free or paid for informal support either from friends or neighbours. Those who chose to pay for informal support had been offered local authority funded care but did not welcome the rigidity and impersonal nature of the care. Instead paying informal networks, using their general income, provided more flexibility, such as choosing when and how their care was provided.
I’ve been able to choose the support that I needed for my situation. Sometimes [local authority] carers come round to put you to bed at eight o’clock at night and I’m like. [..]’ Just no way that’s happening. (Male 50+)
There were also participants who had their care and assistance needs met through supported living. The cost of supported living was met in a range of ways. Those with limited financial resources lived in accommodation covered by housing benefit and used their health and disability benefits to cover costs such as additional management fees that helped to meet the costs of support worker time. Others, with more financial resources, including pensions and savings, had used these incomes sources to access supported accommodation. Examples of this include a participant who had purchased a flat in a care village and could buy-in support from carers, as and when needed.
5.1.3 The home
Structural adaptations
Structural adaptations were either funded through the local authority, health care services, self-funded or through CVS organisations. In some circumstances adaptations were covered using a combination of the above.
Local authority adaptations, such as creating a wet room, were usually undertaken after an in-home assessment by an Occupational Therapist. Similar adaptations were self-funded by others, who could afford to do so and were unaware that they could access local authority funded adaptations, or who may have been deemed ineligible for the support. In some circumstances, participants with limited financial resources, had been provided free structural adaptations from CVS organisations.
There were also participants who required structural adaptations to their home but had not been able to access them. These participants either lived in privately rented accommodation and their landlord had prohibited the introduction of adaptations to the home or were not aware they could access this service via their local authority and had limited financial resources to self-fund structural adaptations. Participants with more financial resources were able to self-fund an extension or adapt their home to provide an extra room to help meet their health-related needs. These participants either lived with their parents or a partner who were working.
Help around the home
Free informal support from family, friends or neighbours was central to providing help around the home with chores related to cleaning, laundry, gardening, DIY and was widespread across the sample.
There were also circumstances where participants paid for help around the home from family, friends or neighbours. The nature of payments ranged from offering one-off small tokens of appreciation for their time, to others having more regular formal payment arrangements with friends or neighbours.
5.1.4 Travel
As explained in chapter 4, access to cars, scooters, taxis or public transport played an important role in helping participants leave the home.
Cars / mobility scooters
The cost of leasing, running and maintaining a car were either met by a participant’s general income, using PIP distinctly to cover these costs or accessing the Motability Scheme, which allowed participants to exchange their PIP mobility component with an allowance to lease a car.
For those who were aware and eligible for a Blue Badge, it provided peace of mind that if they did go out they would be able to leave their car close by and it would help limit the amount of walking needed.
Mobility scooters were self-funded either from pooled general income, health and disability benefits, pensions or savings. Typically, those who had a mobility scooter were already leasing a car through the Motability Scheme, which meant they were unable to lease a scooter via the scheme as well.
To keep costs low, participants reported buying second hand scooters via advertisements on social media or in the Newspaper. Mobility scooters also came with irregular upkeep costs, such as charging the batteries and replacing broken parts, which were covered easily via their general income.
Public transport
Access to a free bus pass[footnote 11] was important for those who were able to leave the house alone and had no other form of transport available. Those who were not eligible for a free bus pass either used other income, if available to cover public transport costs. If this was not available, participants reported a limited ability to travel to appointments and having less contact with family or local support groups.
While it was widespread across the sample for participants to have access to a free bus pass, not everyone met local eligibility criteria. This was despite their own perception that they should be entitled due to their increased need to attend medical appointments.
Taxis
Taxis were generally funded through participants’ general income. Within this group there were participants who were notionally dedicating their PIP mobility payment to cover the cost of taxis. These individuals either thought that the PIP mobility component was specifically meant to cover travel costs or could not give a reason why they had decided to dedicate some of their PIP payment to taxis. Some taxi costs were also subsidised by a Taxicard[footnote 12] .
5.1.5 Utilities
As discussed in chapter 4, there were individuals who spent most of their day indoors, which resulted in higher water, heating and power bills. These costs were largely met through general income, including health and disability benefits. There were some examples of CVS organisations, such as Warm Wales, providing grants to those who were on low incomes to meet heating costs.
5.1.6 Medical goods
As described in chapter 4, participants required a wide range of medication, products and items, equipment and aids and therapies.
Medication
ESA recipients and those aged 60 and above are exempt from paying for NHS prescriptions. Access to free prescription was widespread across the sample of participants. There was concern among those exempt from paying for their medication, that if the NHS did not meet the cost, they would be in financial difficulty. Others in receipt of PIP only, or in work, had to pay for all or some of their NHS prescriptions which were paid for using their general income.
There were participants that designated part of their PIP payment to specifically cover the cost of alternative medication, not prescribed on the NHS. This included items such as ointments that helped relieve symptoms of their health condition or supplements that were used in replacement to prescribed medication for mental health conditions, that participants felt was not working.
Therapies
The cost of treatments and therapies were covered either by the NHS, community and voluntary sector (CVS) organisations or were self-funded. The types of therapies funded by CVS organisations included support with drug and alcohol addiction and oxygen therapy financed by a grant from a charity local to the participant. Others self-funded therapy, such as cupping therapy and acupuncture, was financed through using general income. Some participants said that they felt they would benefit from self-funded therapies, but they could not afford it.
As explained in chapter 4, there were participants who reported that pets, typically dogs, offered them emotional support in and outside of the home. Covering the cost of pets, such as food and vet bills was a priority for these participants and health and disability benefits enabled them to do so.
Talking therapies
Access to talking therapy was met in one of two ways. Those with more financial resources paid for private counselling, as they felt that the waiting list for NHS counselling was too long. Those with fewer financial resources were accessing free counselling through the NHS but had waited long periods of time before they were offered support.
Medical products, equipment and aids
Medical products, equipment and aids were either provided by the NHS, local authorities or were self-funded. Where items were self-funded, smaller or less costly products such as walking sticks were paid for out of the monthly pot of general income, for both those with more and less financial resources. For participants with less financial resources, who required more expensive items such as an orthopaedic chair, they either saved up over the course of some months or sourced second hand items, to keep expenses low.
5.1.7 Help outside the home
Appointments and errands
Informal support networks were key in helping participants get to appointments and run errands outside of the home. Similarly, to care and assistance, there were examples of participants receiving free and paid for informal support to help meet this need. On the whole, where close family provided this support, it was done so on a free basis. Where support networks comprised of neighbours and friends, participants reported feeling obliged to offer a token of thanks.
My [friend] lives [a]round the corner, he’ll pop the washing in or take my washing, do it down at his, bring it back a couple of days later. I’ll give him £10 or £12, washing-up liquid and the time it took him. (Male, 50+)
The internet and online shopping, for those able and willing to use it, also played an important role for participants who had limited informal support networks but were unable to leave the house alone. These costs were met through general income. In some circumstances, where participants were living with parents, PIP was dedicated to covering internet bills, as this was seen as something important to help with social isolation.
Social activities
Support to participate or attend social activities was either met via informal support networks, CVS organisations or faith groups. Younger participants who lived with their parents received support to access social activities via lifts or, parents paid for transport such as taxis, if they were unable to travel via public transport alone. CVS organisations provided support in a range of ways, such as hosting day centres for claimants with learning disabilities and offering chaperone services for participants who experienced sensory impairments. Faith groups helped participants get to church or attend other social activities.
5.1.8 Money and administration
Support with money management and administrative tasks were provided by informal support networks made up of parents, partners or friends. In some circumstances, where informal support networks were limited, participants had formal arrangements with the bank or debt management companies, who managed their money on their behalf, or they were receiving support from adult social care teams.
Support to complete application forms for ESA and PIP was provided either via informal support networks, local authority adult social care teams, or by support workers for those living in supported living.
5.1.9 Social participation / leisure
As explained in chapter 4, participants spending most of their day at home reported relying heavily upon mobile phones, the internet or the TV to aid social participation and help with their wellbeing.
[My] mobile is my life. [It is my] instant communicator. (Male, 50+)
On the whole general income, including health and disability benefits met these needs. However, there were participants who reported distinctly using some of their PIP to cover the cost of TV packages and the internet, as these were products that helped them with their wellbeing.
5.1.10 Work
Among those in work, PIP enabled participants to take unpaid leave when their symptoms flared.
It also gave participants the option of reducing their hours from full-time to part-time.
It’s been a massive help as well because going down to part-time obviously it’s not made the gap up, but it’s helped. (Male, 30-49)
PIP also facilitated access to the Motability Scheme, for those in receipt of the enhanced rate of mobility. For some participants this enabled them access to an adapted car which they needed to commute to work.
5.1.11 Most significant expenditure of health and disability benefits
As described in chapter 3, pooling of health and disability benefits with other income streams was widespread across the sample. This means it was not always possible to identify how health and disability benefits were used to help meet needs, or indeed what the most significant expense health and disability benefits was used to cover.
This case illustration is an example of how a participant uses PIP to help him maintain work by providing a financial cushion when his mental health condition requires him to take unpaid sick leave.
The participant has worked as a facilities manager for the last five years. He works around 40 hours a week. He is the most senior person in his team, so he has autonomy over his working pattern, which depends on how he’s feeling. He has been in and out of work since leaving school at 16. He lives with his wife, son and daughter. His wife manages his money for him because his disorder can cause compulsive spending and has led to significant debt in the past. His main use for PIP is to cover shortfalls in income caused by days off sick, for which he does not receive any sick pay for. Sometimes when his condition worsens he has to begin taking medication, this means he has to take a number of sick days at a time to help get used to the side-effects of the medication.
Male, 30-49
Essential day-to-day living costs, such as housing, utilities, food, transport and clothing costs were the most significant outgoing that general income, including health and disability benefits, was used for. When one participant was asked what their main expenditures were they responded:
It’s food, electric and paying my council to keep the roof over my head. (Male, 50+)
Although less widespread across the sample, there were participants who reported that a large proportion of their general income was spent on either regular or one-off health-specific costs. Regular health-specific costs, which have been addressed in more detail above, included additional care, additional therapies or medical goods. One-off expenditures included purchasing large items such as adapted cars or paying for in-home adaptations, such as ramps or wet-rooms. These participants tended to have more financial resources to draw on, such as a partner or parents’ income, which helped them to meet these large outgoings.
5.1.12 Meeting needs through passported benefits and free support
As set out earlier, there were a range of ways through which participants could access free support to help meet their health-related needs and in some circumstances essential day-to-day living costs.
Health and disability benefits in particular played a unique role in meeting health-related needs, through passporting to other benefits such as free NHS prescriptions and other medical items or enabled access to Blue Badges and free or reduced costs of transport via bus passes and Taxicards which were provided by their local authority.
I think a huge benefit for me is the bus pass. It enables me to, when I can, get out of the house. That is worth more than gold really. It’s a fantastic benefit. It enables me to go to church and see people. (Female, 50+)
Alongside this, participants in some circumstances were also able to access free items and support through local authorities or CVS organisations. When combined, participants who had access to passported benefits and support via their local authority, felt that a large proportion of the health-related needs were being met for free.
However, it is important to note that not all participants in the sample had been able to access free support from their local authority or CVS organisations or had access to passported benefits. Participants who were in this group sometimes reported finding it difficult to afford things such as transport costs or medication. This was either due to a lack of awareness of support available or a lack of eligibility for certain passported benefits or support.
5.2 Motability Scheme
As discussed earlier, the Motability Scheme played a key role in meeting participants’ travel needs. The Motability Scheme allows people to exchange the enhanced/ higher rate of the PIP/ DLA mobility component for the lease of a car, scooter or powered wheelchair. This section explores how the scheme was used to meet participants’ transport needs and the barriers to the scheme among those who were eligible but not using it.
5.2.1 Users’ experience
Among participants who were eligible and using the scheme, all were leasing a vehicle, including examples of participants leasing wheelchair accessible vehicles.
Motivations for using the scheme
Three key motivations for taking up the Motability Scheme were reported:
Enabled access to a car which would have been unaffordable otherwise. Participants explained that without the scheme they would not have been able to finance a car, because of concerns around the long-term financial commitment that comes with a car lease. For them, having a three- or five-year guarantee that PIP would cover the cost of a car was the key factor motivating them to take on a lease.
I couldn’t afford it otherwise. [Its] awfully helpful; they just get it and they take it out of my money every month. (Male, 50+)
Access to good quality and reliable cars. Among participants who said this was their key motivation for taking up the scheme, they had previously had older cars that needed repairs which were costly. Participants also had experience of older cars breaking down, which made those with physical disabilities feel vulnerable.
My husband had cars and they were breaking down and all the rest of it. You always had to put money in to getting them sorted. With the [Motability] car, I have no worry about making repairs. (Female, 50+)
Provided independence and ability to leave the house. Having a car was crucial for participants who could not make use of public transport or taxis because of their health condition. Examples of this included participants with Crohn’s disease who reported that regular and unexpected incontinence made them avoid public transport or taxis.
I can’t catch taxis and I can’t catch buses, so I need a car to get A to B for my hospital appointments. […] I have to go for my bloods every four weeks at the hospital and I don’t want to rely too much on my brother. (Male, 50+)
Barriers to continued use
Larger or more expensive cars required an advance non-refundable payment upfront. Those with limited financial resources explained that the deposit needed for a larger car, made it difficult to either renew or lease a new car. For example, a participant leasing a larger vehicle, to allow them to fit a scooter and hoist, used inheritance to cover the deposit when first leasing their car. However, they were concerned for how they would finance the payment again in the future.
Others reported that the advance payment required for larger cars, limited the size of the vehicle they could lease. For example, a participant who sometimes required a wheelchair when out in public could not fit it in the car they were currently leasing and were concerned they could damage the car if they tried to force it in. They wanted to lease a larger car but could not afford the advance payment required.
Those with wider financial resources were able to draw on these, to save up in anticipation of the advance payment needed when leasing a new car. Examples of this include a younger participant, whose parents were financially supporting them:
There’s money set aside for the deposit for his car, because there is a hefty deposit to be paid when we swap cars. We set money aside for that”. (Male, 18-29, proxy interview)
5.2.2 Eligible and not using the scheme
Those who were eligible and not using the scheme fell into two groups – those aware but had made an active decision not to use the scheme and those unaware the scheme existed.
Among those who were aware but not using the scheme, four barriers to use were reported:
Unable to drive or operate a car or scooter: participants either did not have a driving licence or their health condition or disability, such as visual impairments or heart conditions, stopped them from driving or using a scooter. These participants also lived alone, which meant that they could not rely on others to drive them around.
Stigma attached to scooters: among those who were in the 30-49 age category, there were some who felt deterred from leasing a mobility scooter because they identified them as something older people would use. Others were concerned that a mobility scooter would draw attention to their disability, which they wanted to avoid.
Preference for PIP payment: there were a range of reasons why PIP was preferred, including: participants deciding that they could get a cheaper vehicle elsewhere.
The scheme would still workout expensive. If I need to be driven, I would prefer buying a car which is worth around £1,000, between £1,000 and £2,000. (Male, 30-49)
Concerned with application process[footnote 13] : while this concern was not widespread, there were participants who had assumed there would be an assessment process required to access the car and they wanted to avoid further benefit assessments. This was particularly the case for participants with mental health conditions who had previous negative experience with DWP and social services assessments.
Others had previously used the scheme and were not using the car regularly enough to warrant renewing their lease.
There were also participants who were eligible but were unaware the scheme existed. These participants either already had access to a car, had a health condition or disability which stopped them from driving, such as dementia, or were younger participants with learning disabilities and were being cared for by their parents who were unaware of the scheme.
5.2.3 Characteristics influencing take-up
Participants from a range of different financial circumstances were using the Motability Scheme. Those with more limited financial circumstances explained that they would not have been able to lease a car without the scheme. Those with wider financial resources to draw from also found the scheme helpful, especially in being able to access cars with adaptations. However, they did not see the scheme as essential in being able to access a vehicle. Examples of this included participants who had previously leased cars through private dealerships but switched to the Motability Scheme as they saw benefit in using their PIP to cover the cost of a car.
Among those in the sample using the scheme were participants living in both rural and urban areas. The necessity of the scheme appeared to be more apparent for those living in rural areas, who found locally that there was a lack of availability, reliable or accessible public transport.
Factors that did appear to influence take-up included the extent of a participant’s social networks and the type of health condition or disability they had. Lack of a close social support network, combined with a health condition or disability which stopped them from driving, meant some participants were not able to access the scheme. Participants in these circumstances did report that if they had someone who was able to use a car on their behalf, they might consider using the scheme.
6. Factors driving how health and disability benefits are used
This chapter examines the resources available to participants that drive how health and disability benefits were used to meet health-related needs.
Key findings
- Participants’ access to a number of different resources, from social support, to use of free provision and other income sources, affected how health and disability benefits were used and the degree to which their needs were met.
- Those with access to fewer resources experienced difficulty meeting their health-related needs and some also struggled to afford essential day-to-day living costs, such as heating and food. This included fewer financial resources, a lack awareness and take-up of available support, social support networks and digital access and/ or skills. Additional constraints to meeting needs included having less visible health conditions (mainly mental health conditions), unmanageable debt and more limited approaches to money management.
- Participants who were able to meet most or all of their needs had access to greater resources, including financial resources and social networks. These participants were better informed about forms of support or entitlements available to them. Typically, they lived with a partner or their parents who were in well-paid jobs.
- Wherever participants could afford to, they used health and disability benefits alongside other sources of income to pay for health-related costs such as mental health counselling or equipment and aids.
- Having access to a wide range of resources did not always mean all needs were met, such as the need for social interaction, and this was found across the spectrum of health conditions and disabilities and financial circumstances.
- The degree to which needs were met was not always stable. Changes in the availability of free support were influenced by life stage transitions (e.g. turning 18) which affected eligibility and by changes in the landscape of available charity and voluntary sector (CVS) support.
6.1. Access to resources that influence how health-related needs were met
Access to a range of resources influenced the extent to which participants’ health-related needs were met and this drove usage of health and disability benefits[footnote 14] . These resources included monetary support, social support networks, awareness and uptake of free provision, personal preferences for support, digital capacity and the influence of health conditions on participants’ ability to manage money. The extent of all of these resources interacted to influence the degree to which additional health-related needs were met. Participants who had limited access to one or more resource experienced difficulties meeting their needs, while those with access to a wider range of resources had less difficulty meeting their needs. Figure 6.1 below illustrates the resources that influenced the extent to which health-related were met.
Figure 6.1 Resources influencing extent to which health-related needs were met
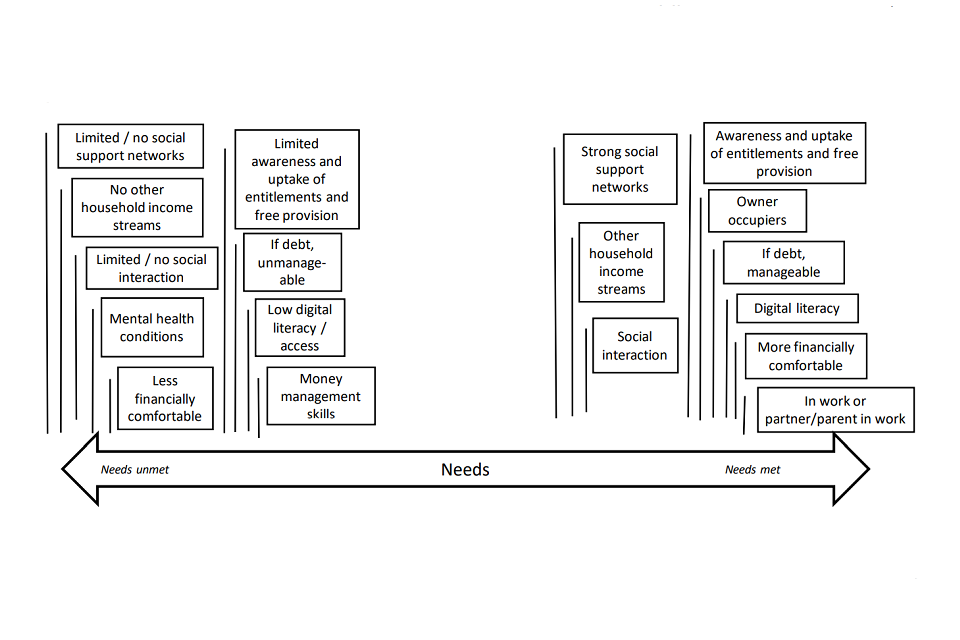
Text version of Figure 6.1, in order of needs unmet to needs met:
- Limited/no social support networks
- No other household income streams
- Limited/no social interaction
- Mental health conditions
- Less financially comfortable
- Limited awareness and uptake of entitlements and free provision
- If debt, unmanageable
- Low digital literacy/access
- Money management skills
- Strong social support networks
- Other household income streams
- Social interaction
- Awareness and uptake of entitlements and free provision
- Owner occupiers
- If debt, manageable
- Digital literacy
- More financially comfortable
- In work or parent/partner in work
Participants who had difficulties meeting their health-related needs had some or a combination of the following characteristics: fewer resources, both financial and in terms of informal support networks. This was often combined with unmanageable debt; low awareness or take up of free entitlements and provision; fluctuating and less visible health conditions (mainly mental health conditions); health conditions that affected their ability to work and manage money; tenure in the private rental sector and limited internet access due to affordability or impairments which limited access to information, support and resources. The case illustration below highlights how limited resources influenced the extent to which needs are met.
This case illustration demonstrates how limited financial circumstances, social isolation and limited awareness of services led to this participant experiencing difficulties meeting their needs
The participant had kidney failure, arthritis in his back, legs and arms, depression and bulimia which caused chronic stomach pains. He lived alone in a flat rented from a Housing Association, using Housing Benefit. He was in the ESA Support Group and received PIP. He made monthly repayments for utility bill arrears and had a £5,000 bank loan which he could not afford to repay. His debt repayments meant he could not afford essential day-to-day living needs and used a foodbank. He found it difficult to wash independently due to his arthritis and needed a walk-in shower but could not afford one and seemed unaware that he may be eligible for support through the local authority. He also needed support with cooking and cleaning and received help from a cousin. His cousin would like to claim Carer’s Allowance but neither of them knew how to make an application. He had no other support networks close by.
Male, 50+
Participants who were able to meet most or all of their additional health-related needs had access to a wider range of resources. These were financial resources, support from social networks and awareness and uptake of free entitlements and provision. In addition, some participants had found work that accommodated their health condition. This group was typically made up of younger claimants living with their parents and those living with a partner, who worked in a well-paid job. They were financially ‘cushioned’ by their parents or partners or had long work histories themselves which provided an income or well-paid pension. The case illustration below highlights how access to a wide range of resources leads to a variety of health-related needs being met.
This case illustration demonstrates how strong social support networks enabled a participant to meet all of their health-related needs.
The participant has recently moved in with her mother and sister, she had previously lived alone in a council-rented flat but had begun to feel isolated and found paying the rent and bills difficult so decided to move in with her mother. She has a range of health conditions and disabilities including Asperger syndrome, anxiety, ADHD, joint stiffness and IBS. She works 28 hours a week and receives PIP. Before moving to live with her mother she was concerned about how her income would cover essential day-to-day living costs. She also struggled with maintaining her personal hygiene and found it difficult to leave the house as she did not like going out alone. Moving in with her mother has helped her to meet all of her health-related needs.
Female, 18-29
6.1.1 Types of resources influencing the extent to which health-related needs were met
As described above participants’ ability to meet their health-related needs, were influenced by the number and level of resources that they had access to. Below we take each resource in turn and discuss how access to it influenced the extent to which needs were met.
Financial resources
Participants’ benefit spending behaviours, particularly in relation to their health, were influenced by their overall financial circumstances, other commitments, such as children and money management skills, including their ability to manage debt.
Those who could afford to meet almost all of their health-related needs had more financial resources as a result of having additional income streams in their household (their own, or from a parent or partner). These households usually included someone (for example a partner or parent), who was working in a relatively well-paid role. Where these participants had debt, it was manageable. These participants did not report competing spending priorities and were able to self-fund certain treatments rather than needing to rely solely on free provision. Examples included: private mental health counselling, paying for equipment and aids (such as wheelchairs or mobility scooters); paying for therapies and treatments not available on the NHS (such as osteopathy); or buying special food or drink.
They could also afford activities that supported their independence or wellbeing, such as exercise classes. Although these participants could cover health-related costs at present, concerns were raised about how they would afford them in the future, either as their health deteriorated and their needs increased, or when other household members who financially supported them were no longer there.
This case illustration demonstrates how despite in some cases having severe health conditions, participants with multiple household income streams and high levels of formal support from the care system often had fewer unmet needs.
Due to developmental complications in the womb, the participant had multiple health conditions including quadriplegia, epilepsy and incontinence. He could not communicate verbally and used a wheelchair. He lived with his parents who owned their house, were both in work and paid for all the household bills. He was in receipt of DLA, ESA and the Independent Living Fund in Scotland (ILF). He required 24-hour care, which was covered via a mixture of the Independent Living Fund, local authority funded care and was being topped up by his parents’ income. DLA and ESA were pooled with other income streams to cover the cost of the microwave meals he ate each day at a day-centre, as well as social and health-related activities, such as music therapy he received.
Male, 30-49
On the other end of the spectrum was a group of participants with limited financial resources who reported prioritising their essential day-to-day living costs over other health-related costs. Participants with limited financial resources included claimants in working households with low paid jobs, participants in out-of-work households whose only income stream came from benefits and those with unmanageable debt. Having other financial commitments, such as children, also led these participants to limit or stop spending on their health. Those with children who had restricted financial resources usually described putting their own needs, including their health-related needs, after those of their children. This included single parent families and participants who had children with additional health needs.
Decisions about what to spend limited financial resources on were unique to each individual’s particular health and personal circumstances, with participants weighing up and prioritising spending on different needs. As a result, some additional needs were not met, such as transport costs (for healthcare appointments), additional therapies, equipment and aids and in-home adaptations. In these circumstances participants either went without or saved up to afford these costs occasionally or rationing their usage.
Within this group were participants who were often unable to meet essential day-to-day living needs, such as heating their house or buying food. To help them cope with the shortfall in their finances, they borrowed from family and friends or relied on them to cover certain expenses (such as groceries) and/ or used support services such as foodbanks.
Level of informal support
Another important resource which determined the extent to which needs were met was the level of informal social support participants had access. Informal networks provided a range of free help and support, including: daily personal care; support around the house; help with childcare; lifts or company when going out and financial support either through lending or regularly paying for groceries, petrol, clothes and other costs. In comparison, participants who had small social support networks, or whose family or friends could only provide limited support, sometimes incurred additional costs to meet their needs. For example, participants who could not get lifts to medical appointments paid for taxis instead or paid neighbours to take them. In some cases, those with limited informal networks were paying to access formal support through assisted living arrangements. A significant informal support network was able to mitigate to some degree the negative impact of limitations to resources, such as the effect of a low income. This is illustrated in the case below.
This case illustration demonstrates the balancing role that informal social support can play in meeting some but not all needs.
The participant was single parent who lived in private rental accommodation with her two young children. She experienced anxiety and depression and struggled to leave the house and do basic tasks like cooking, cleaning, eating and taking medication. She received ESA and DLA alongside housing and child benefits as her only income streams. Despite budgeting, she found she did not have enough money to cover all of her costs. She felt that she was not receiving adequate formal support for her mental health condition and was not satisfied with her medication. However, she received a high level of informal support from her parents who lived nearby, her friend and her ex-partner. Her dad drove her to appointments, while her mum bought the family groceries or toiletries once a week. Her ex-partner supported with childcare, taking her son to the nursery and helping around the house. Her best friend visited every day to help her clean, cook and take her medication. Without this support she would have been less able to meet her needs.
Female, 30-49
While this informal support was crucial, it was not always sustainable. The level of care needed for severe and multiple health conditions could put a strain on close relationships, as parents, partners and friends struggled to adapt. In some cases, individuals providing support to participants felt that the care they provided was covering gaps in local social care or social services, sometimes at the cost of their own health.
Availability and awareness of free support and provision
Availability of different forms of support locally and participants’ awareness of such support also influenced how they used their health and disability benefits and the degree to which their needs were met. It appeared from participants’ accounts that support varied considerably between local authorities and different NHS Trusts, which is consistent with other research.[footnote 15] However, if participants were not accessing services and showed no awareness of them, it was not always possible to ascertain whether this was simply due to lack of awareness as opposed to a lack of availability.
Where the availability of formal local authority provided social care support[footnote 16] was limited due to eligibility criteria, those who could afford to do so paid for top-up hours for additional support, as described in chapter 5. Those with restricted financial resources went without this support. Services that were unavailable or that had limited availability on the NHS were also paid for by those with the financial means. For mental health support, long waiting times for NHS services meant that those who could afford to, paid for private support. Additional therapies, such as hydrotherapy or physiotherapy, also fell into this category.
Lack of awareness of free support also drove spending behaviour, leading to participants paying for health-related costs themselves or going without, despite being entitled to free support. For example, some participants seemed unaware that local authorities could fund equipment such as crutches and walkers or in-home adaptations and had instead paid for them themselves.
Beyond a lack of awareness, there was sometimes a reluctance to make requests to local authorities for adaptations such as a stairlift or a walk-in shower, due to a perception that they would not be eligible or due to a feeling of stigma. In other cases, participants were aware that support existed but were unaware of the eligibility criteria or who to contact to access support.
I’d like to get a [free] bus pass to try and get me out more and out and about, but I don’t know how to go about that if I’m entitled to one or not. (Female, 50+)
Preferences for support
Participants’ preferences for the type of support they received also affected how needs were met. As explained in chapter 5, rather than seeking free local authority social care support, some participants chose to pay friends, family and neighbours for personal care, support with housework or transport to medical appointments. Participants felt this offered them more flexibility over the care they received, for example being able to choose what time to go to bed.
It suits me so much better to have all these other friends that I can pay the same than the council carers, because as I say, if I need them to take me away to an appointment, I pay them to do that, whereas if it was council carers, I wouldn’t have that facility. (Male, 50+)
There were also examples of participants choosing to spend extra money on equipment, such as electric wheelchairs or mobility scooters, rather than relying on free equipment from the NHS or local authorities. This gave them greater choice to pick the equipment that best suited them, such as a scooter that could handle uneven surfaces. Those with greater financial resources were able to make outright purchases from their savings, whereas those with restricted financial resources saved and sought out second-hand items to reduce costs.
Digital capability and access
Inability to access online resources played a role in the extent to which health-related needs were met. Lack of digital access could be the result of low digital capability or due to affordability. Socially isolated participants, who found it difficult to get out utilised the internet to meet some of their needs such as online food shopping or banking. For those who were socially isolated but did not have internet access, they had other costs they had to prioritise such as taxis to go to the shops. It is likely that a lack of digital access resulted in lower awareness of entitlements and free provision from other sources. In some cases, it also led to greater social isolation or led to participants having to rely more on their informal support networks. One participant who could not afford the internet and who found it difficult to leave the home, reflected on what he felt he was missing:
There would be groups on there and people that you can talk to without actually sitting face-to-face to and organisations you can get in touch with and stuff. (Male, 30-49)
Types of health conditions
A pattern also emerged in terms of the nature of health conditions and the way participants used their income and the extent to which needs were met. Participants with mental health conditions tended to report a wide variety of basic needs, health and care needs and social needs that were unmet. In comparison, those with profound learning disabilities and severe physical disabilities were typically in the group that identified having fewer unmet needs. While the latter group experienced a high level of need across a range of areas, these were usually being met through a combination of local authority support and informal support networks, usually parents who provided a high level of care.
A reason for this difference could be that mental health conditions were often less visible and participants with these conditions found it difficult to communicate their needs during benefit or local authority assessments, which impacted the level of support they had access to. Participants who experienced fluctuating conditions which varied day-to-day also experienced these difficulties in communicating their needs and accessing adequate levels of support. In these cases, participants often relied on informal support networks, where available, which was felt to be more flexible than formal support.
Health conditions also affected the degree to which participants were able to effectively manage their money (see 3.3.3). Some health conditions caused participants to experience particular anxiety in relation to money, difficulties understanding budgeting or too fatigued to manage their money effectively. This in turn could lead to issues of unmanageable debt.
6.2. Changes in support or need
As discussed above, participants varied in the extent to which they were accessing a wide range of other support, whether from the local authority, CVS organisations or their informal support networks. This was sometimes because support was not available, they were unaware of it and/or they had limited social networks they could draw on. Some of this support acted directly in funding certain health-related costs or enabled a reduction in costs. However, the level of support that was available could also change over time, as could participants’ health needs. This meant that the degree to which needs were met was not stable, particularly for those with fluctuating conditions.
As discussed in chapter 5, CVS organisations provided support to those with health conditions and disabilities. This included not just financial support in the form of direct grants (for therapies or to tackle fuel poverty), but also a range of support groups and activities and specialist one-to-one personal support such as for leaving the house or accessing other services. Conversely, the withdrawal of support from CVS organisations as a result of funding cuts limited the support available, leading to participants having difficulty meeting their needs. For instance, someone with a mental health condition became socially isolated when he could no longer be accompanied out by a charity support worker as the charity had had its funding reduced.
Transitions in life stage, such as when children turned 18 or left education, could also lead to changes in the social care support they received. One parent of a participant who had recently reached 18 reflected on the impact of the withdrawal of their daughter’s carer.
It was hard because all the stuff that had been being done for her just stopped. So, between us we just had to do it and try and teach her independence at the same time. (Female, 18-29)
At these stages parents reported having to take on more care as participants’ eligibility for social care support changed.
7. Participants’ suggestions for improvements
This chapter outlines the factors that participants’ felt would improve their quality of life. It also sets out the improvements they would like to see to services, support and provision that would address unmet needs identified through the research.
Key findings
- Participants believed better access to health services, particularly mental health services, would improve their quality of life and wellbeing.
- Support to combat social isolation and loneliness through peer support, was identified as a key need amongst participants, regardless of financial circumstances.
- Suggested improvements to DWP services included: greater awareness-raising and signposting to benefit entitlements, enhanced customer service from Jobcentre Plus (JCP) increasing certain benefit amounts and giving claimants more control over when and how payments were made.
7.1 Improving quality of life / wellbeing
Participants across the spectrum of financial circumstances suggested a range of ways that their quality of life and wellbeing could be improved. While having a higher income was seen as an important enabler of an improved lifestyle, improvements to services and support from local authorities, health services and employers were equally important for some.
7.1.1 Health services and support
As explained in chapter 6, a recurring theme across interviews was a lack of mental health provision, such as access to psychiatric services, counselling and talking therapies, due to long waiting lists or a lack of free provision. There was frustration from participants that, rather than access to these services, they were offered prescribed medication which often resulted in side effects that impacted negatively on their day-to-day life. Furthermore, where mental health support was in place, issues were reported with the continuity and reliability of care.
Similarly, other participants noted that more frequent access to therapeutic services and treatments that are not available on the NHS would help alleviate their symptoms. It was also felt that there could be more signposting from NHS settings and charities to entitlements and services for people with health conditions and disabilities e.g. benefits and respite care.
7.1.2 Greater social interaction or peer support
As explained in chapter 6, social isolation was an unmet need reported by participants across a range of health conditions and disabilities, including learning disabilities, visual impairments and mental health conditions. Participants, including proxy participants, suggested that support groups, places to meet similar people and socialise and buddying / befriending schemes could be ways to help combat their isolation and loneliness.
Everything she goes to now it’s all older person orientated. She needs I think now somebody in her own age group. (Female, 30-49, proxy interview)
7.1.3 Specialist or one-to-one support
Participants with health conditions and disabilities such as autism or dementia felt that their quality of life would be improved if they had access to one-to-one personal assistant support. These participants wanted help with administrative tasks in the home, such as opening and responding to post, as well as support to leave the house.
I need a PA; I need somebody to work with me on a one-to-one basis; someone who understands autism, who can help me do things I need. (Male, 18-29)
Others expressed the need for practical support with health-related needs such as securing adaptations or equipment and social work support.
7.1.4 Work, learning and being active
Both those actively seeking work and those whose health condition was stopping them from working, felt that their wellbeing would be improved by some form of work, paid or voluntary.
He’s happier when he’s doing these courses and going out, but when he’s at home he’s not, I can tell, so he needs a job. I would prefer him to work than getting Universal Credit. (Male, 18-29, proxy interview)
As described in chapter 2, one of the key barriers to work experienced by participants, were the negative attitudes they faced from prospective employers. Participants actively seeking work wanted the government to give employers greater financial incentives to employ and/or train disabled people.
For similar reasons participants wanted to be able to participate in sports, music and workshops. Others wanted to increase their skills and independence by developing IT literacy and learning to cook.
In relation to this, there were participants who reported that improvements to the accessibility of public transport e.g. more wheelchair space or additional transport options for disabled people in rural areas, would provide them with more independence and the ability to leave the home alone.
7.1.5 Respite
It was suggested that respite either in the form of a support worker or the option of going into respite care would relieve emotional / psychological burden on family members.
We can’t really go on a decent holiday because we can’t afford it, but those are luxuries anyway. (Female, 50+)
7.1.6 Housing
There were a range of housing needs that participants felt would improve their quality of life. Younger participants who lived with their parents, felt they would benefit from living independently, but could not afford to live alone. Others, who lived in private rented accommodation, had landlords who had not accepted their request to introduce adaptations and wanted the opportunity to move into social housing, so these needs could be met. There were also participants in private rented accommodation who wanted to move closer to family and friends but due to high debts (that were largely as a result of a mental health condition causing compulsive spending) they were concerned they would not be able to find a landlord willing to offer them a property.
7.2 Suggested improvements to DWP services
Participants’ suggestions for improving DWP’s services for recipients of health and disability benefits encompassed three main areas:
- Awareness raising and support;
- Services provided by Jobcentre Plus (JCP) and
- Benefit payments.
7.2.1 Awareness raising and support
Greater awareness-raising and signposting to benefit entitlements were suggested, including information for parents about benefits for disabled children. More information, signposting and practical support around financial and health-related needs were also mentioned, for instance in relation to money management, seeking adaptations or equipment, or social work support. Participants with barriers to using the internet, due for example to affordability, visual impairments or concerns about online security, wanted more offline information provision.
7.2.2 Services provided by JCP
Among ESA and UC recipients who had experienced contact with JCP as part of their claim, there was a view that JCP staff could improve their customer service through more respectful and compassionate treatment of those with health conditions and disabilities. For those with mental health conditions specifically, suggestions included offering private waiting and appointment spaces in JCP offices to limit anxiety; equipping work coaches with a better awareness of mental health issues and pacing job search activities slowly to build up confidence.
As some health conditions and disabilities could pose barriers to remembering and reaching appointments, participants with memory loss and anxiety wanted appointment reminders and to be able to contact their JCP office directly if they were running late.
A further suggestion was better information sharing between medical professionals and JCP, to avoid claimants having to repeat details of their health, which could be distressing. Finally, encouraging employers to offer training and employment opportunities to people with health conditions and disabilities.
7.2.3 Benefit payments
Participants with very limited financial resources in particular said that an increase in benefit payments would improve their overall wellbeing. Recipients of PIP felt that eligibility for the benefit should enable passporting to other benefits, including free prescriptions, eye tests and housing benefit. Where participants had moved from one benefit to another e.g. DLA to PIP, they felt payment amounts should be maintained and not reduced. Relatedly, parents felt that 18 rather than 16 was a more appropriate age for young claimants to switch from DLA to PIP, as they would be more capable of managing their finances independently at this age.
The research also explored participants’ views on receiving multiple health and disability benefits as a single payment. The preferences expressed were largely underpinned by individual budgeting style and did not necessarily correspond with existing payment arrangements. For example, some participants in receipt of UC who received a single monthly payment wanted to return to separate payments.
Single monthly payments were preferred by those who thought this would align better with Direct Debits as benefits that were paid periodically on different dates of the month (e.g. every four weeks) could result in missed Direct Debits. Receiving income from benefits as a single sum was also anticipated to make budgeting more straightforward. On the other hand, separate payments, including more frequent payments of a single benefit, were preferred by those who used staggered payments as a budgeting tool and relied on them to avoid running out of money at the end of the month. For some, e.g. participants with mental health conditions or conditions such as autism, maintaining the current routine was the overriding factor.
Reflecting these diverse payment preferences and budgeting approaches, participants suggested more choice and flexibility around payments, including when, how frequently and in what way benefits were paid would make finances easier to manage.
8. Conclusions
This report presents the findings from in-depth qualitative research into how health and disability benefits are used by participants to meet a variety of needs arising from their health condition(s) and/or disabilities. This chapter summarises the main findings and addresses some of the wider implications of the research.
8.1 Uses of health and disability benefits
Spending of health and disability benefits was highly influenced by the wider context of resources available to participants, including their financial circumstances, availability and awareness of free formal support and the strength of their informal social networks. Although different health and disability benefits are designed to serve particular purposes[footnote 17] the research found that in reality the way these benefits were used was influenced by wider circumstances.
Whilst the precise use of health and disability benefits was obscured when they were pooled with other household income, when looking at household income as a whole, the most significant expenditure was on essential day-to-day living costs, including utility bills, groceries, mortgage/rent payments and car expenses. However, health and disability benefits, alongside other income streams, were used to meet almost all areas of additional health-related needs.
This research also shows that health and disability benefits are an important part of a much wider landscape of services and support. Other services such as health and social care services, informal support networks, Community and Voluntary Sector organisations and other household income streams were also heavily relied on to help meet needs. Passported benefits, such as free NHS prescriptions and support provided by local authorities, such as free bus travel, were also important elements of support that allowed participants to save money and use their income in other ways to meet their health needs. The Motability Scheme also enabled some participants to access reliable, quality cars that might otherwise have been unaffordable, although not all eligible participants chose to take up the scheme.
8.2 Additional health-related needs
This research aimed to identify the uses of health and disability benefits, therefore it first sought to establish the areas of additional need arising from claimants’ conditions. The findings point to personal needs such as dietary requirements, clothing or footwear; home-focused needs such structural adaptations and help with housework and needs outside of the home, with using transport, attending healthcare appointments or running errands. Participants often experienced additional needs across a range of these areas and for some, the level of their need varied and depended on their health condition or disability and the severity of condition. Many of these needs resulted in additional costs: either costs that were specifically related to their health condition or disability, such as paying for medical goods or equipment, or in heightened essential day-to-day living costs, such as for utilities or transport, confirming previous research findings.[footnote 18] The research highlighted how some health conditions and disabilities led to additional needs or difficulties in budgeting and managing finances. In addition to these areas of need, the findings also reveal that participants had needs around social participation, primarily because of difficulties leaving the home.
8.3 Factors driving how health and disability benefits are used
Participants’ access to a number of different resources, from social support, to use of free provision and financial resources affected how health and disability benefits (alongside wider income) were used and the degree to which participants could meet their health-related needs.
Participants with more resources used health and disability benefits alongside wider income, such as from a partner or parent, to meet essential day-to-day living costs and additional needs that supported health, independence and wellbeing. For this group, benefits could be used to plug gaps in free provision, for example, by paying for private counselling for mental health. In circumstances, where participants or their partner or parents were in work, health and disability benefits also provided a financial cushion which allowed participants, their partner or their parent(s) flexibility at work to take time off as sick days or to provide care as necessary.
Among those with more limited financial resources, i.e. where health and disability benefits were the main or only source of income, they offered a regular income which provided reassurance that some essential day-to-day living costs would be met. In these cases, participants could not afford to pay for all additional health-related costs and participants felt that some health specific needs were not met. Also, these participants sometimes relied on other support from family and friends or CVS organisations to meet essential day-to-day living costs.
The stability and visibility of health condition(s) also influenced the degree to which participants were able to access the support that they needed. Those with fluctuating or less visible conditions and in particular, those with mental health conditions, found it harder to access support and often presented with a greater number of unmet needs.
These factors interacted in complex ways and in some cases one factor was able to mitigate the negative impact of others. For instance, strong informal support networks could to some extent help to lessen the impact of limited financial resources. Other needs, such as the need for social interaction, could not be met with money alone, meaning that isolation and loneliness were experienced across the financial spectrum. Moreover, the extent to which needs were met could change, the most important factors that influenced this were: fluctuating or deteriorating health, changes to personal and financial circumstances such as benefits re-assessments or changes to employment and reductions in informal support or local voluntary services.
8.4 Participants’ suggestions for improvements
Reflecting the wide range of services and support participants drew on, they suggested a range of ways that their quality of life and wellbeing could be improved. This included improvements to health services, in particular better access to mental health services; improved access to social and/ or peer support; for those who wanted to work, improved government incentives to employ disabled people or those with health conditions and better access to social housing.
Participants also felt that services provided by Jobcentre Plus (JCP) could be made more flexible and appropriate to those with health conditions, for instance, by having private appointment spaces at JCP offices for those with mental health issues and by providing better training to staff. Participants also made suggestions about the benefits systems overall. These included upholding payment amounts when individuals were switched from DLA to PIP, providing more flexibility around payment dates and increasing the overall level of benefit payments to help participants meet health needs and improve overall wellbeing.
References
Corden, A., Sainsbury, R., Irvine A., and Clarke, S. (2010) The Impact of Disability Living Allowance and Attendance Allowance: Findings from exploratory qualitative research, DWP Research Report 649
Hill, K. and Davis, A., (2018) Making ends meet below the minimum income standard: families experiences over time. Loughborough: Loughborough University, Centre for Research in Social Policy
John E., Thomas, G. and Touchet, A. (2019). The Disability Price Tag 2019. Scope Policy Report
Ritchie, J., Lewis, J., Nichols, C.M. and Ormston, R. (2014). Qualitative Research in Practice. Sage: London. (2nd Edition)
The King’s Fund 2018. Briefing: Key Challenges Facing the Adult Social Care Sector in England.
Appendix A.1 Sample breakdown
To ensure the achieved sample included participants with conditions that varied in severity levels a definition of severity was built into the sample design. The definition used DLA/ PIP rates and ESA/UC groups as a proxy to place participants into three severity categories - higher, medium or low. Categories were defined in the following ways:
Higher severity level
- ESA Support Group / UC No Work Related Requirements Group
- Or PIP/DLA daily living/care and mobility at higher / enhanced rates
- Or a combination of both
Medium severity level
- PIP/DLA daily living/care or mobility at a higher / enhanced rate
- Or ESA WRAG/UC Work Preparation Group / enhanced rate of PIP/DLA
Lower severity level
- ESA Work Related Activity Group/UC Work Preparation Group only
- Or in combination with lower or middle rates of PIP/DLA.
Table A1 Sample breakdown by benefit type and
| PIP/DLA only | Number |
|---|---|
| High | 9 |
| Medium | 12 |
| Low | 14 |
| Total | 35 |
| ESA/UC only | Number |
|---|---|
| High | 12 |
| Low | 10 |
| Total | 22 |
| Combination | Number |
|---|---|
| High | 42 |
| Medium | 11 |
| Low | 10 |
| Total | 63 |
| Subtotal | 120 |
A range of secondary criteria were established with quotas set against each to ensure the achieved sample achieved range and diversity in terms of demographic characteristics. Table A2 provides a breakdown of the demographic characteristics of the achieved sample.
Table A2 Sample breakdown by demographic characteristics
| Work status | Number |
|---|---|
| Part-time | 8 |
| Full-time | 3 |
| Permitted work | 0 |
| Not in work | 109 |
| Age | Number |
|---|---|
| 18-29 | 16 |
| 30-49 | 41 |
| 50+ | 63 |
| Type of health condition | Number |
|---|---|
| Physical | 45 |
| Mental health condition | 24 |
| Both | 51 |
| Dependents | Number |
|---|---|
| Yes | 22 |
| No | 98 |
| Gender | Number |
|---|---|
| Female | 61 |
| Male | 59 |
| Housing tenure | Number |
|---|---|
| Social housing | 57 |
| Private rented | 11 |
| Lives with family | 24 |
| Owner occupied | 20 |
| Live in care home | 8 |
| In receipt of social care support | Number |
|---|---|
| Yes | 19 |
| No | 101 |
| Eligible for Motability | Number |
|---|---|
| Yes | 46 |
| No | 74 |
| Claiming Universal Credit | Number |
|---|---|
| Yes | 10 |
| No | 110 |
| Type of ESA | Number |
|---|---|
| Income Related | 52 |
| Contribution Based | 6 |
| Both | 17 |
| N/A | 45 |
Appendix A.2 Types of health conditions and disabilities
Table 1.1 Types of health conditions and disabilities
Physical health conditions and disabilities
- Inflammatory conditions/skin conditions (e.g., psoriasis, angioedema, Crohn’s)
- Movement and coordination conditions (e.g., Cerebral Palsy)
- Neurological conditions (e.g., epilepsy, brain damage, Alzheimer’s)
- Cardiovascular conditions (e.g., Hypertrophic Cardiomyopathy, hypertension)
- Organ diseases (e.g., kidney disease, liver cirrhosis, endometriosis, COPD)
- Immune system conditions (e.g., Multiple Sclerosis, HIV, allergies)
- Musculoskeletal conditions (e.g., arthritis, spinal disc problems, scoliosis)
- Cancer (e.g., lymphoma, prostate cancer, lung cancer)
- Amputations (e.g., leg amputation)
- Metabolic disorders (e.g., diabetes, thyroid problems)
Mental health conditions and disabilities
- Anxiety
- Depression
- Bipolar disorder, unipolar
- Borderline Personality Disorder
- Post-Traumatic Stress Disorder
- Obsessive Compulsive Disorder
- Eating disorder (Anorexia, Bulimia)
- Psychosis
- Schizophrenia
Neurodevelopmental and behavioural conditions
- Attention Deficit Hyperactivity Disorder
- Autistic Spectrum Disorder
- Dyspraxia
- Down’s Syndrome
- Foetal alcohol syndrome
- Microcephaly
- Agenesis of the corpus callosum
- Learning difficulties
- Tourette’s Syndrome
Sensory impairments
- Visual impairments
- Hearing impairments
Appendix A.3 Topic Guide
Contextual information
Section aims: To ease the participant into the discussion and to get an understanding of their household and wider circumstances.
Explain that it would be good to know a bit about them before we begin the discussion
What is a typical week like for them
- What are their regular day-to-day living activities – e.g. social activities, work, volunteering, caring responsibilities
- Who do they see – who do they see most often – family, friends, neighbours, health professionals, support services
- What do they enjoy most
- What if anything particularly worries or frustrates them
- What they would like to do more of / less of and barriers to this
Living situation (where necessary, remind them that nothing said will affect their claim(s) or any dealings with DWP)
- Who lives in the household, their age / age groups
- How long have they lived at their current address
- Tenure (owners, social, private renting)
- Any changes to their living situation in recent years
Work and education
- Education / skills background
- If currently doing some paid or voluntary work
- What they do
- Hours
- How long they’ve been doing this
- How feel about their job
- Whether they experience any challenges
- Overview of recent employment history
- If not currently in any paid employment
- How they feel about work – currently looking / future option
- Have they worked in the past / how long ago / what did they do
- What led them to leave work
- Are they doing any unpaid work e.g. voluntary work, work experience
- Do they have any contact with or receive support from their Jobcentre – if so, how often and what form does this support take
Health condition and/or disability (explain to participants that we are interested in hearing about their health condition and / or disability in their own words – reassure them that we are not here to assess their condition)
- How their health is at the moment
- Nature of each specific condition or disability (where appropriate, list health conditions to come back to in section 4, verbalise for those with sight impairments)
- Description of health conditions and disabilities, including characteristics or symptoms
- Onset, and length of time experienced
- State of each condition / disability e.g. chronic, fluctuating, terminal
- What a typical day looks like
- What a good and bad day looks like
- Any change over time
- Treatment / therapies they are receiving
- NHS / other
- Frequency
Finances
Section aim: to develop a picture of participants’ financial situation.
Where appropriate, use a weekly / monthly calendar to help participant recall about income and expenditure and list the benefits they receive
Income and savings
Health and disability benefit income streams
- Current health / disability benefits received
- Components and rates
- Whether they are aware of the DLA / PIP components and do they know which rates they receive
- Whether they are aware of ESA / UC groups
- How long have they been receiving these
- If combination of benefits, benefits received for which specific health conditions / disabilities
- Whether they have made a claim for any other health / disability benefits that they are still waiting to hear about
- Ask PIP/DLA recipients only if they have previously made a claim for ESA / UC
- Ask ESA/UC recipients only if they have previously made a claim for PIP / DLA
Other income streams e.g. types of income, rough value and frequency
- Other benefits – e.g. Housing Benefit, Carer’s Allowance, tax credits
- Earnings
- Pensions (there shouldn’t be anyone there who receives a state pension, but they may be receiving an occupational or private pension early)
- Child maintenance
- Rental or investment income
- Money from other people – parents, adult children
- Other
Income from others in the household
Overall income
- A general sense of their overall household income amount
- Identify most significant income streams(s), as an individual and/or household - the stream(s) most relied on and why
Changes in individual and / or household income
- Overall stability of household income and extent to which it fluctuates
- Any recent changes, reasons and perceived impact
- Any future expected changes – reasons and perceived impact
Savings, rough value
Expenditure and debt
Main types of expenditure
- Rent / mortgage
- Utility bills
- Grocery and other household shopping
- Health related expenses e.g. care
- Transport costs (taxis, vehicle)
- Childcare
- Debt
- Other
Key debts types (credit cards, loans)
- Size of debts
- Reasons for debt
- Accumulative debt from living on low income
- Specific life events (e.g. divorces)
- Health related issues
Most significant outgoings, probe around how significant health and disability related expenditure is
Budgeting and financial management
How household finances are managed
- Do they pool all their income together or do they allocate different income streams to different uses
- Their use of different benefits
- If receiving ESA & PIP – are both used for different purposes/seen as different
- If receiving ESA/UC only or DLA/PIP only - whether they think about / treat them differently to other income
- If receiving Carer’s Allowance – used for a different purpose than other benefits
- Who takes responsibility for managing finances in their household
- How household finances are managed, extent to which they ‘budget’ or monitor money
For people who receive multiple ‘pots’ of health & disability money e.g. ESA, PIP/DLA, LA funding, social care
- What do they think about this
- Views about having different income streams vs being paid everything in one payment
Help, advice and/or support received to manage money – source and type of support (e.g. Citizens Advice, Money Advice Service, accountant)
Meeting needs: Use of health and disability benefits and other support
Section aim: to bring together the previous discussion on health/disability and finances to understand: (a) how their health affects them; (b) what additional needs arise from this; (c) how these needs are met, including gaps in meeting these.
Understanding needs: impact of health condition or disability
How health conditions / disabilities affect them generally day-to-day (including interaction between conditions), and related needs
- The home
- Needing help around the home (e.g. cleaning, shopping, gardening, DIY, personal admin)
- Equipment (mobility, household fittings / aids, furniture)
- Fuel – heating and power
- Housing – e.g. additional room for a carer
- Technology
- Their person
- Food and drink requirements
- Clothing, footwear and appearance
- Personal care and assistance
- Technology (e.g. need to use a washing machine more often)
- Health goods / services
- Medication
- Therapeutic services
- Relationships and social interaction
- Getting out of the house
- Taking part in social activities
- Communication / technology (e.g. for the sight and hearing impaired, internet)
- Interpreter
- Transport (e.g. blue badge, dial a ride, additional journeys)
Where participant is working/actively looking for work, how health conditions / disabilities affect their day-to-day employment situation and related needs
- Looking for work
- Transport / getting to work
- Adjustments at work
- What has been helpful in enabling them to stay into work
- What would be helpful in helping them to enhance their ability to work (e.g. more hours, progress in work)
Understanding how needs are met
For EACH general need, explore how needs met and reasons
- Whether they can meet this need – identifying any gaps
- How they use their health and disability benefits
- Other benefits
- Other passport benefits/concessions
- Other income sources
- Other support
- Informal help received from other people
- Partner / other household / family members (whether Carer’s Allowance is paid)
- Friends, neighbours, volunteers (whether Carer’s Allowance is paid)
- Formal care arrangements
- Support received from Adult Social Care (LA, respite care, short breaks)
- Care from the NHS (e.g. GP, hospital staff, therapists)
- Local and community support groups
- Support they self-fund
- Services
- Meals on wheels; prepared foods
- Private vehicle (ask blue badge/Motability)
- Taxis/community transport (ask blue badge)
- Support groups/helplines
- Informal help received from other people
Where participant is working/ actively looking for work, how needs are met and reasons
- Whether they can meet this need – identifying any gaps
- How they use their health and disability benefits
- Ask about the Access to Work scheme – whether applied/received support
- Other benefits
- Other passport benefits/concessions
- Other income sources
- Support they are receiving from their JCP – including any they have declined
- Other support (same as general needs)
- Whether finances are a barrier to looking for / progressing in work
For participants eligible for the Motability Scheme (on higher rate mobility component DLA and enhanced PIP mobility component), whether they access the scheme
- If not, why not (e.g. awareness, meeting needs in other ways)
- If yes, why (i.e. what use it for and why decided to use it – e.g. perceived benefit)
Summing up
Overall spending priorities and reasons
- Health and disability
- Other spending priorities – whether compete with health and disability priorities
The overall use of health and disability benefits
- What they enable them to do/ what they would not be able to do without them
- Extent to which health and disability benefits are used for non-health purposes – including context in which they would use these for other purposes
- Whether availability of local support or provision affects decisions and spending behaviour, what provision
- Extent to which income from these benefits covers all health-related needs – if not
- Which needs not met
- How decisions to prioritise specific needs made
- What can’t they do with the type, level and form in which they receive the benefit
Extent to which health and disability needs met
- If met fully, why
- If not met fully, why
- Impact it has on them
- Decisions around which needs are met and why
Views on quality of life
Whether they can live the way they would like to
- What practical support would make their life better
How they would describe their wellbeing (how happy or comfortable they feel with their life in general)
Concluding thoughts
Key suggestions for how the government could improve its services for people receiving health and disability benefits
What changes would most help to make their life easier:
- Benefit system
- Wider support system
-
Note that DWP health and disability benefits are not intended to necessarily meet all extra costs of long-term ill health or disability, which vary considerably for different claimants depending on their personal and household circumstances. Further information is available on GOV.UK. ↩
-
Ritchie, J., Lewis, J., Nichols, C.M. and Ormston, R. (2014). Qualitative Research in Practice. Sage: London. (2nd Edition). ↩
-
See how essential day-to-day living costs has been defined in the glossary of terms ↩
-
See how additional health-related costs has been defined in the glossary of terms ↩
-
Budgeting loans are available to those on ESA to cover larger expenses or participants had received advance payments for their UC. Repayments on both types are removed directly from benefit payments. Get an advance on your first payment Budgeting Loans ↩
-
This echoes findings of previous research, see: Corden, A., Sainsbury, R., Irvine A., and Clarke, S. (2010) The Impact of Disability Living Allowance and Attendance Allowance: Findings from exploratory qualitative research, DWP Research Report 649. ↩
-
This approach has been found in a number of other studies of those living on low incomes or benefits. See, for example: Corden et al (2010) and Hill, K. and Davis, A., (2018) Making ends meet below the minimum income standard: families experiences over time. Loughborough: Loughborough University, Centre for Research in Social Policy ↩
-
A range of techniques were used including: diaries/calendars or notebooks with key payment dates marked; online banking or banking apps; weekly/fortnight budgets; as well as direct debits and standing orders. Some participants also used separate bank accounts to manage different income streams or different forms of expenditure. ↩
-
The listing of additional needs reflects no particular order as the extent and frequency of each area of need varied from individual to individual. ↩
-
Examples include grants from community interest companies and charities or council funded care combined with privately funded care. ↩
-
The English National Concessionary Travel and the London Freedom Pass schemes provide individuals with certain health conditions or disabilities with free access to public transport. ↩
-
Taxicard is a scheme that subsidises the cost of taxis for individuals who have restricted mobility or are severely sight impaired. ↩
-
There is no second assessment to join the Motability Scheme, being in receipt of enhanced PIP or higher rate DLA passport those claimants onto the Scheme. ↩
-
Note that DWP health and disability benefits are not intended to necessarily meet all extra costs of long-term ill health or disability, which vary considerably for different claimants depending on their personal and household circumstances. ↩
-
The King’s Fund 2018. Briefing: Key Challenges Facing the Adult Social Care Sector in England. ↩
-
Differences in social care provision relate both to the thresholds of needs at which care is provided and to the level of care (e.g. number of visits) provided see: Age UK (no date). Social care eligibility thresholds briefing [online]. Available at AgeUK. ↩
-
Income replacement in the case of Employment and Support Allowance/ Universal Credit and to help with the extra costs of long-term ill health or disability for Disability Living Allowance/ Personal Independence Payment ↩
-
John E., Thomas, G. and Touchet, A. (2019). The Disability Price Tag 2019. Scope Policy Report. ↩
