COVID-19: infection prevention and control dental appendix
Updated 14 April 2022
1. About this guidance
This document is an appendix to the Infection prevention and control for seasonal respiratory infections in health and care settings (including SARS-CoV-2) for winter 2021 to 2022 issued jointly by the Department of Health and Social Care (DHSC), Public Health Wales (PHW), Public Health Agency (PHA) Northern Ireland, NHS National Services Scotland, UK Health Security Agency (UKHSA) and NHS England as official guidance.
This appendix has been updated in line with the revision of the IPC guidance for health and care settings. It has been revised to take account of advice from bodies such as UKHSA, the National Institute for Health and Care Excellence (NICE) and the World Health Organisation (WHO). The content of this document has been agreed by the four UK Chief Dental Officers.
The IPC principles in this document apply to all dental settings, including those in the independent and private sector, including:
- general dental services
- community dental services
- public dental services
- armed forces dental services
- prison dental services
- dental teaching hospitals
- specialist dental services provided from primary care settings
Hospital dental services (secondary care) should liaise with their trust or organisation to determine whether this appendix or the IPC guidance for health and care settings is most appropriate for their services.
When implementing this guidance practitioners must consider the specific conditions of their individual place of work and comply with all applicable legislation.
2. Summary
This section summarises the guidance. Refer to the relevant section for further detail. The two pathways are summarised in Figure 1. All patients should be screened for potential COVID-19 infection, ideally prior to attendance at the setting, using the COVID-19 screening questions. An example of COVID-19 screening questions can be found in Appendix 1.
Based on screening the patient should be assigned to either a respiratory or non-respiratory pathway.
For patients on the non-respiratory pathway standard infection control precautions (SICPs) apply. Testing for patients on the non-respiratory pathway should be in line with country specific requirements.
For patients on the respiratory pathway transmission-based precautions (TBPs) apply in addition to SICPs.
For patients on the respiratory pathway undergoing aerosol generating procedures (AGPs), post AGP downtime applies.
Figure 1: Diagram summarising the 2 pathways for patients attending dental settings
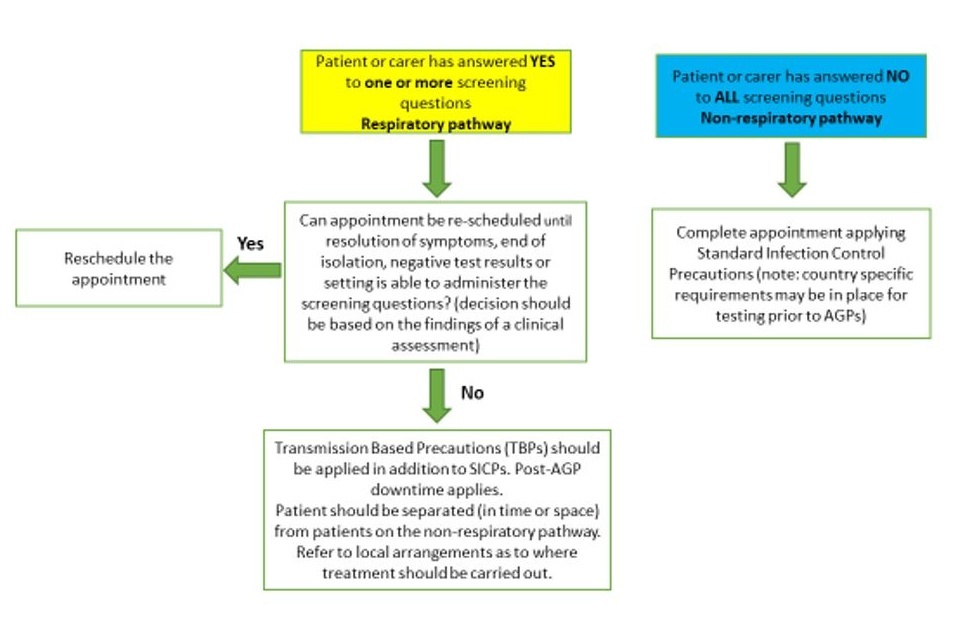
2.1 Diagram summarising pathways: plain text description
Left top of chart begins with statement: ‘Patient or carer has answered yes to one or more screening questions?’
Move to: ‘Can appointment be re-scheduled until resolution of symptoms, end of isolation, negative test results or setting is able to administer the screening questions?’
Answer no: ‘Transmission-based precautions (TBPs) should be applied in addition to SICPs. Post-AGP downtime applies.’
Answer yes: ‘Reschedule the appointment’
Right top of the chart begins with statement: ‘Patient or carer has answered no to all screening questions’
Move to: ‘Complete appointment applying standard infection control precautions’
3. Main messages
The main changes from the previous version of this guidance include:
- removal of the 3 distinct COVID-19 care pathways (high, medium and low)
- use of a screening tool to place patients on either a non-respiratory or a respiratory pathway
- for the non-respiratory pathway, guidance that physical distancing should be at least 1 metre in all areas where possible, for example when not providing direct clinical care. This should be increased to 2 metres whenever feasible
What has not changed:
- organisations and employers have a responsibility to assess, manage and monitor risk based on the measures prioritised in the hierarchy of controls
- all patients should be screened for COVID-19
- universal masking/face coverings to remain as an IPC measure for staff and patients within dental settings across the winter period
- patients with suspected or confirmed respiratory infection should have non-urgent treatment deferred if it is considered clinically appropriate
- patients with symptoms of respiratory infection, or who have a confirmed respiratory infection, and whose treatment cannot be deferred, should be segregated or isolated, for example separated by space or time, from other patients
- continuation of 2 metres physical distancing for patients with suspected or confirmed respiratory infection (respiratory pathway)
4. Scope and purpose
The COVID-19 pandemic remains a threat (see COVID-19 alert levels) and as such there continues to be a need to be cautious in order to prevent and control transmission of the virus. New variants of SARS-CoV-2 remain a risk as do other respiratory infections, specifically influenza and RSV which are likely to present over winter 2021 to 2022.
Please note that this guidance is of a general nature and employers should consider the specific conditions of each individual place of work and comply with all applicable legislation and regulations, including the Health and Safety at Work etc. Act 1974. This guidance does not supersede existing legislation or regulations across the UK.
While this document seeks to ensure a consistent and resilient UK wide approach, some differences in operational details and organisational responsibilities may apply in the different UK nations.
5. Governance and responsibilities
Employers and organisations are responsible for ensuring safe systems of work, including managing the risk associated with infectious agents through the completion of risk assessments. Further details on the organisational and employer responsibilities in relation to infection prevention and control can be found in the main IPC guidance.
This national guidance outlines the recommended principles to support local decision making within individual organisations, practices, and settings. This guidance sets the minimum levels of IPC that settings should follow.
The pathways described assume that the dental setting has completed a risk assessment in line with the ‘hierarchy of controls’ and that the setting has implemented effective controls, based on the risk assessment, to reduce the spread of respiratory pathogens.
6. Hierarchy of controls
Limiting transmission of infection in health and care setting requires a range of IPC measures. Included is the ‘hierarchy of controls’ which, if applied in order, are used to identify the appropriate controls. Safe systems of work outlined in the hierarchy of controls, including elimination, substitution, engineering, administrative controls and personal protective equipment (PPE), are an integral part of IPC measures. Organisations and employers, for example dental practice owners, have a responsibility to ensure risk assessments are undertaken in the context of managing infectious agents. Key areas and measures for assessment are outlined in the main IPC guidance.
7. Ventilation requirements
All enclosed workplaces must be ventilated by natural or artificial means as set out in the Workplace (Health, Safety and Welfare) Regulation. UK building regulations recommend whole building ventilation to be 10 l/s/person, and current healthcare guidance for new buildings and major refurbishments specifies that a treatment room should have at least 10 air changes per hour (ACH).
Ventilation is important to reduce the risk of aerosol contamination from potential airborne and droplet pathogens in dental settings. Clearance of infectious particles after an aerosol generating procedure (AGP) is dependent on the ventilation and air change within the room. Specialist advice should be sought on how best to achieve the recommended air changes.
Further information on ventilation for dentistry is available.
It is recognised that transitional arrangements may need to be in place to support dental practices where air changes are unknown or below this recommended level.
8. Occupational health and vaccination
Prompt recognition of cases of respiratory infection among health and care staff is essential to limit transmission. Staff testing negative for SARS-CoV-2 by polymerase chain reaction (PCR) who remain symptomatic of another respiratory infection should consider the risk to service users (particularly those who are immunosuppressed or at high risk of complications from respiratory infections) before returning to work. Once medically fit to return to work, if staff are in doubt about any risk they may pose to service users or colleagues, this should be discussed with their line manager in the first instance. Bank, agency and locum staff should follow the same deployment advice as permanent staff.
Staff should be vaccinated against respiratory infections, for example influenza and COVID-19, in line with country specific requirements.
Staff who are fully vaccinated against COVID-19 and are a close contact of a case of COVID-19 may be allowed to return to work without the need to self-isolate. There are country-specific variations on the requirements for PCR and lateral flow device (LFD) antigen testing and these policies are under continual review and subject to change.
Refer to country specific policy for:
- England – COVID-19 management of exposed healthcare workers and patients in hospitals and accompanying letter issued by NHS England
- Scotland - Coronavirus (COVID-19) – exemption of fully vaccinated social care staff from isolation: information for providers
- Wales - COVID-19 contacts: guidance for health and social care staff
- Northern Ireland - management of self-isolation of close contacts of COVID-19 cases who are fully vaccinated - additional safeguards for health and social care staff
Regardless of whether staff have had and recovered from, or have received vaccination for a specific respiratory pathogen they should continue to follow the IPC precautions, including PPE as outlined in this document.
Staff asymptomatic testing (PCR or LFD) for SARS-CoV-2 must be implemented in accordance with current national and local policy:
- England - Asymptomatic staff testing for COVID-19 for primary care staff
- Scotland - COVID-19 healthcare worker testing
- Wales - COVID-19 testing health and social care staff
- Northern Ireland - COVID-19 health and social care workers
A risk assessment is required for health and care staff who may be at high risk of complications from respiratory infections such as influenza and severe illness from COVID-19, for example, pregnant and Black, Asian and Minority Ethnic (BAME) staff.
Guidance on carrying out risk assessments is available.
As part of an employer’s duty of care, they have a role to play in ensuring that staff understand and are adequately trained in safe systems of working, including donning and doffing of PPE. A fit testing programme should be in place for those who may need to wear respiratory protection.
9. Use of masks
9.1 Universal masking by staff, patients and visitors
Universal masking (with face coverings or surgical masks (Type II or IIR)) to prevent the transmission of SARS-CoV-2 and other respiratory infectious agents in dental settings should continue to be applied for all staff, patients and visitors.
For patients on the non-respiratory pathway face coverings are acceptable. Surgical facemasks should continue to be worn during the winter period 2021 to 2022 by staff in all areas within dental settings, except in staff areas when eating and drinking.
Patients with confirmed or suspected respiratory infection should be provided with a surgical facemask (Type II or Type IIR). The patient requirement to wear a surgical facemask must never compromise their clinical care.
Organisations in NHS Scotland should refer to Coronavirus (COVID-19): Guidance on the extended use of facemasks and face coverings in hospitals, primary care and wider community care settings.
9.2 Surgical masks (Type IIR)
Surgical masks can be either Type II or Type IIR. When worn as PPE to protect against splash or spray, a fluid-resistant surgical mask (FRSM) (Type IIR) should be worn.
Surgical masks must:
- be well fitted covering both nose and mouth
- not be allowed to dangle around the neck after or between each use
- not be touched once put on
- be changed when they become moist or damaged
- be disposed of as single use
- be worn once and then discarded as healthcare (clinical) waste. Hand hygiene must always be performed after disposal
Further information about hand hygiene, respiratory and cough etiquette, safe management of the care environment, waste and safe management of linen can be found in the main IPC guidance.
10. Screening for COVID-19
Screening is a way of identifying apparently healthy people who may have an increased risk of a particular condition. In this guidance, screening is used to identify patients before or at entry to the care area who may have COVID-19 but who do not have any symptoms.
Patients attending for an appointment/admission who have been screened (and have answered ‘no’ to all screening questions), and have no clinical signs or symptoms of respiratory infection and have been tested (with a negative result) as per country or local testing strategies only require the application of standard infection control precautions (SICPs) at the point of care.
The application of SICPs during care delivery is determined by an assessment of risk to and from individuals and includes the task, level of interaction and/or the anticipated level of exposure to blood and/or other body fluids. TBPs, as outlined in this guidance, are not routinely required. However, the application of IPC measures must be assessed, and risks mitigated as outlined under the hierarchy of controls.
Screening for early recognition of COVID-19 should be undertaken for all patients. Wherever possible this should be done prior to attendance at the dental setting to ensure rapid implementation of recommended control measures.
Screening of patients in advance of them attending at the dental setting will minimise the risk to staff and other patients and minimise the inconvenience to the patient (country-specific requirements for screening may vary and should be followed). Patients should be encouraged to inform the dental setting as soon as any symptoms occur and not to wait until the day of the appointment.
Signage should be displayed prior to and on entry to the dental setting instructing patients with respiratory symptoms or suspected or confirmed respiratory infection to inform reception staff immediately on their arrival. Screening should be undertaken by staff who are trained and competent. See Appendix 1 for an example of COVID-19 screening questions.
Screening for COVID-19 should also be applied to individuals accompanying the patient. Anyone accompanying the patient should be advised not to attend if they have symptoms of respiratory infection. Accompanying persons who are symptomatic should not be permitted to enter the dental setting. Exceptions should only be made for specific circumstances and following a risk assessment.
11. Use of rapid COVID-19 testing
Pre-appointment testing is not a requirement of the respiratory or non-respiratory pathway. Dental settings may choose to use LFD testing to provide pre-appointment testing as part of their risk mitigation, providing it is agreed by the country that they are working in that this is an appropriate use for these tests. As testing arrangements are a devolved responsibility, settings should ensure that any testing is carried out in line with country specific requirements. Lack of a negative test must not be used to refuse patient care.
12. Physical distancing
In health and care settings physical distancing is the recommended distance that should be maintained between staff, patients and visitors unless mitigations are in place such as the use of PPE. WHO continues to advise that a physical distance of at least 1 metre should be maintained between and among patients, staff, and all other persons in healthcare settings. This distance should be increased wherever feasible, especially in indoor settings. Physical distancing should remain at 2 metres where infectious respiratory patients are cared for.
Patients who have been screened to the non-respiratory pathway are able to sit in waiting rooms together provided a physical distance of at least 1 metre can be maintained.
13. Standard infection control precautions (SICPs)
All health and social care providers should be familiar with SICPs and TBPs.
SICPs are the basic IPC measures necessary to reduce the risk of transmission of infectious agents from both recognised and unrecognised sources of infection. Sources of potential infection include blood and other body fluids secretions or excretions (excluding sweat), non-intact skin or mucous membranes, and any equipment or items in the care environment that could have become contaminated. SICPs are to be used by all staff, in all care settings, at all times, for all patients.
SICPs should be used in treatment of patients in all healthcare settings. For patients on the respiratory pathway TBPs should applied in addition to SICPs.
National (country specific) policy for SICPs is available for Wales, Northern Ireland, and Scotland. NHS England is developing a national IPC Manual for England as set out in the UK 5-year Tackling Antimicrobial Resistance National Action Plan (2019 to 2024).
13.1 Personal protective equipment (as part of SICPs)
Before undertaking any procedure, staff should assess any likely exposure and ensure PPE is worn in line with guidance and the risks associated with the procedure or task being undertaken. Disposable gloves and aprons should be worn when contact with blood or body fluids is anticipated.
A summary of the PPE required for staff as part of SICPs is shown in Table 1.
Table 1. SICPs PPE for staff in dental settings
| Patient pathway | Non-respiratory pathway |
|---|---|
| Waiting room, reception Non-clinical areas |
Hand hygiene FRSM Type II or Type IIR |
| Dental surgery and clinical areas when providing direct clinical care Non-AGP and AGP treatment |
Hand hygiene Single use disposable gloves* Single use disposable plastic apron** FRSM Type IIR Eye protection*** |
*Vinyl gloves are not recommended for direct patient care; they may be used for equipment and environmental cleaning.
**Required when carrying out close contact patient care and AGPs. A single use fluid repellent gown should be used if an apron will not provide adequate protection against splashing or spraying.
***Goggles or visor. Regular corrective spectacles are not considered as eye protection.
All PPE should be:
- compliant with the relevant BS/EN standards (technical standards as adopted in the UK post-EU exit)
- located close to the point of use
- stored to prevent contamination in a clean/dry area until required for use (expiry dates must be adhered to)
- single use only, unless specified by the manufacturer
- disposed of after use into the correct waste stream for example healthcare waste
Hand hygiene should be performed after removal of PPE. See guidance on donning (putting on) and doffing (removing) PPE.
Any reusable PPE must have a decontamination process in place that follows manufacturer’s instructions, and responsibility assigned.
Disposable gloves should:
- be worn when exposure to blood and other body fluids, non-intact skin or mucous membranes is anticipated or likely
- be changed immediately after each patient and after completing a procedure or task even on the same patient
- be put on immediately before performing an invasive procedure and removed on completion
- not be decontaminated with alcohol-based hand rub (ABHR) or soap between use
- be changed when they become moist or damaged
Inappropriate use of gloves, that is not changing them as recommended above, risks the gloves contributing to the transfer of organisms and cross-infection.
Gloves are not required when undertaking administrative tasks for example using the telephone, using a computer or tablet, writing in the patient notes.
Gloves are not an alternative to hand hygiene.
Disposable plastic aprons (or gowns if an apron does not provide sufficient protection) should be worn to protect staff uniform or clothes from contamination when providing direct patient care (if there is a risk of extensive splashing or spraying) and during environmental and equipment decontamination.
Aprons should be:
- worn to protect uniform or clothes when contamination is anticipated or likely
- changed between patients or after completing a procedure or task
- fluid-resistant gowns should be worn when a disposable plastic apron provides inadequate cover of staff uniform or clothes for the procedure or task being performed and when there is a risk of extensive splashing of blood or other body fluids
- disposable aprons and gowns should be changed between patients and immediately after completion of a task
- disposed of and replaced if damaged
Aprons are not required when undertaking administrative tasks, (for example using the telephone, using a computer or tablet).
Eye or face protection (including full-face visors) should:
- be worn if blood and/or body fluid contamination to the eyes or face is anticipated or likely and always during aerosol generating procedures
- not be impeded by accessories such as piercings or false eyelashes
- not be touched when being worn
- if reusable, must have a decontamination schedule in place in line with the manufacturers’ instructions
Regular corrective spectacles are not considered as eye protection.
14. Respiratory pathway
14.1 Deferral of treatment
Following screening, if a patient is identified as having a suspected or confirmed COVID-19 infection (answers yes to one or more of the screening questions), a clinical assessment should take place to determine whether it is appropriate to defer treatment. Treatment should not be deferred unless there has been a clinical assessment. This assessment can be undertaken remotely, if necessary.
If treatment is deferred antibiotic stewardship is advocated to ensure antibiotics are only prescribed when appropriate. UK guidelines on antimicrobial stewardship can be found at dental AMR toolkit.
14.2 Patient placement
In all healthcare settings, including dental settings, patients with symptoms of respiratory infection or a suspected or confirmed respiratory infection should be segregated from other patients as promptly as possible. If a separate room is not available, the patient should be asked to return home or return to their car and asked to phone the dental setting so arrangements for their care can be discussed.
Dental services should identify in advance areas, routes and consultation rooms for these individuals who have been assessed as requiring treatment. Ideally, these individuals should be seen at the end of the day or session to reduce any post AGP downtime (where an AGP is performed) impacting on the remaining patient consultation list. Where space allows, a dedicated consultation or treatment room should be identified for placement of individuals with respiratory symptoms.
Physical distancing of at least 2 metres is required for patients on the respiratory pathway.
15. Transmission-based precautions (TBPs) (for use in the Respiratory Pathway)
This section describes specific actions that should be taken when applying TBPs in the care of a person known or suspected to have a respiratory infection (the respiratory pathway).TBPs are applied when SICPs alone are insufficient to prevent cross transmission of an infectious agent.
The risk of spread of infection may be minimised by ensuring that:
- there are separate waiting and reception areas or use of physical barriers
- patients wear surgical facemasks whilst in the dental setting
- in settings where multiple chairs are in use in the same room, there is physical spacing of at least 2 metres
- when AGPs are undertaken, a method of physical segregation that provides at least a 2 metre barrier in the horizontal and vertical planes is provided
- each clinical area has adequate ventilation
- patients on the respiratory pathway are seen at a different time from other patients, with disinfection of shared areas taking place between patients
- the procedure is deferred or re-scheduled, providing this is not detrimental to their condition and has been assessed as clinically appropriate
- patients are advised to arrive on time (not early) and wait in their car or outdoors if possible, until contacted to advise to enter the building for their appointment
- patient care is transferred to a designated site for example an urgent care centre. This option will be dependent on local arrangements
- any accompanying persons are not present during AGPs unless they are considered essential following a risk assessment, for example a carer, parent or guardian
15.1 PPE requirements (as part of TBPs for care provided on the respiratory pathway)
While providing care to patients with suspected or confirmed respiratory infection, PPE as described in Table 2 should be applied.
Table 2: PPE required by staff when caring for patients with suspected or confirmed respiratory infection
| PPE required | Respiratory pathway PPE |
|---|---|
| Waiting room/reception Non-clinical areas |
Hand hygiene FRSM Type II or Type IIR |
| Non-AGP treatment | Single use disposable gloves* Single use apron (or single use fluid repellent gown if risk of extensive spraying or splashing)** FRSM Type IIR for direct patient care Eye protection - single use or reusable*** |
| AGP treatment | Single use disposable gloves* Single use apron (or single use fluid repellent gown if risk of extensive spraying or splashing)** FFP3 or respirator /hood Eye protection - single use or reusable*** |
*Vinyl gloves are not recommended for direct patient care; they may be used for equipment and environmental cleaning.
**Required when carrying out close contact patient care and AGPs. A single use fluid repellent gown should be used if an apron will not provide adequate protection against splashing or spraying.
***Goggles or visor. Regular corrective spectacles are not considered as eye protection.
Airborne precautions should be applied in multiple chair rooms where AGPs are carried out on patients on the respiratory pathway. Where possible patients with a known or suspected respiratory infection should be managed in a closed surgery with adequate ventilation.
Refer to guidance on donning (putting on) and doffing (removing) PPE.
15.2 Respiratory protective equipment (RPE)
Respirators can be single use or single session use (disposable or reusable). Reusable respirators can be used if they comply with HSE recommendations and should be decontaminated and maintained according to the manufacturer’s instructions.
In some countries of the UK reusable respirators are not recommended. Dental settings should check the relevant country-specific advice on the use of reusable respirators.
All tight fitting RPE, for example FFP3 (filtering face piece or hood) respirators must:
- be fluid-resistant
- be fit tested on all healthcare staff who may be required to wear a respirator to ensure an adequate seal and fit according to the manufacturer’s guidance. Where fit testing fails, suitable alternative equipment must be provided
- be fit checked (according to the manufacturer’s guidance) every time a respirator is donned to ensure an adequate seal has been achieved
- be compatible with other facial protection used, for example protective eyewear, so that this does not interfere with the seal of the respiratory protection. Regular corrective spectacles are not considered adequate eye protection
- be disposed of and replaced if breathing becomes difficult, the respirator is damaged or distorted, the respirator becomes obviously contaminated by respiratory secretions or other body fluids, or if a proper face fit cannot be maintained
- not be allowed to dangle around the neck of the wearer or hang from one ear after or between each use
- not be touched once put on
Remove RPE and eye protection in a safe area (for example outside the clinical area). If RPE is removed in a clinical area following an AGP, appropriate post AGP downtime must have elapsed before the RPE is removed. All other PPE should be removed in the patient care area. Perform hand hygiene after removing and disposing of RPE.
All staff who are required to wear an FFP3 respirator must be fit tested for the relevant model to ensure an adequate seal or fit according to the manufacturer’s guidance.
Further information regarding fitting and fit checking of respirators can be found on the Health and Safety Executive website.
Respirators with exhalation valves are not fluid-resistant unless they are also ‘shrouded’. Valved non-shrouded respirators should be worn with a full-face shield (a Type IIR mask is not acceptable) if blood or body fluid splashing is anticipated.
Respirators and powered hoods with exhalation valves should not be worn by a healthcare worker when sterility directly over the surgical field is required, for example in theatres or surgical settings or when undertaking a sterile procedure as the exhaled breath is unfiltered. Dental care such as surgical extractions and implant placement are not considered sterile procedures in this context. It is unlikely that this will apply to situations where an FFP3 is worn while carrying out surgical procedures in primary care settings as they are not usually considered sterile procedures. See CAS alert for more information.
Further information on RPE can be found in section 6.5.6 of the main IPC guidance.
16. Aerosol generating procedures
An AGP is a medical procedure that can result in the release of airborne particles (aerosols) from the respiratory tract. When treating someone who is suspected or known to be suffering from an infectious agent transmitted wholly or partly by the airborne or droplet route an AGP can transmit the infectious agent. AGPs should only be carried out on when essential and only staff who are needed to undertake the procedure should be present.
TBPs are required when undertaking AGPs for patients on the respiratory pathway. Only essential staff who are needed to undertake the procedure should be present. Dental procedures that use high velocity air and water streams are considered a high risk of creating aerosols and include:
- ultrasonic scaler (including piezo)
- high speed air rotor (or electric rotor that is greater than 60,000 rpm)
- piezo surgical handpiece
- air polishers
Research has demonstrated that use of the 3-in-1 syringe with either air-only or water-only resulted in lower levels of contamination, with water-only causing the least contamination. There is currently no consensus to include the use of a 3-in-1 as an AGP. Non-surgical dental extractions are not considered AGPs.
The defined list of AGPs is currently under review, this is expected to be finalised by end November 2021 at which point this appendix will be updated.
16.1 Post AGP downtime (respiratory pathway)
A multidisciplinary working group (the Scottish Dental Clinical Effectiveness Programme, SDCEP) has proposed a pragmatic algorithm with mitigation factors for post AGP downtime that has been accepted by the 4 UK Chief Dental Officers. The SDCEP rapid review of AGPs is available.
See Figure 2 for post AGP downtime algorithm.
The working group advises that:
- where there is ventilation but the number of ACH are unknown, or there are 1 to 5 ACH, a baseline post AGP downtime of 30 minutes is recommended with mitigation such as high-volume suction/rubber dam
- where there are 6 to 9 ACH, a baseline post AGP downtime of 20 minutes is recommended
- where there are 10 or more ACH, a baseline post AGP downtime of 15 minutes is recommended
- where dentists use other mitigating measures such as screening, high volume suction/rubber dam and cleaning/disinfection of the environment between patients, post-AGP down time is not considered necessary for successive appointments between members of the same household
- patients on the respiratory pathway should be separated by space or time from other patients for example with end of session appointments
- AGPs should not be conducted in a room that has no natural ventilation (that is a window) or mechanical ventilation (see section 7 for further detail on ventilation requirements)
- all equipment, including ventilation, suction and air cleaners, is maintained according to manufacturer’s instructions and is operating effectively
- a minimum post AGP downtime of 10 minutes should apply to allow larger droplets to settle before environmental cleaning
- post AGP downtime can commence at the end of aerosol production (as soon as the use of the piece of equipment generating the aerosol has ceased)
Post-AGP downtime is not required for AGPs on patients or individuals with no known or suspected respiratory infection (those on the non- respiratory pathway).
Figure 2: Algorithm for post AGP downtime
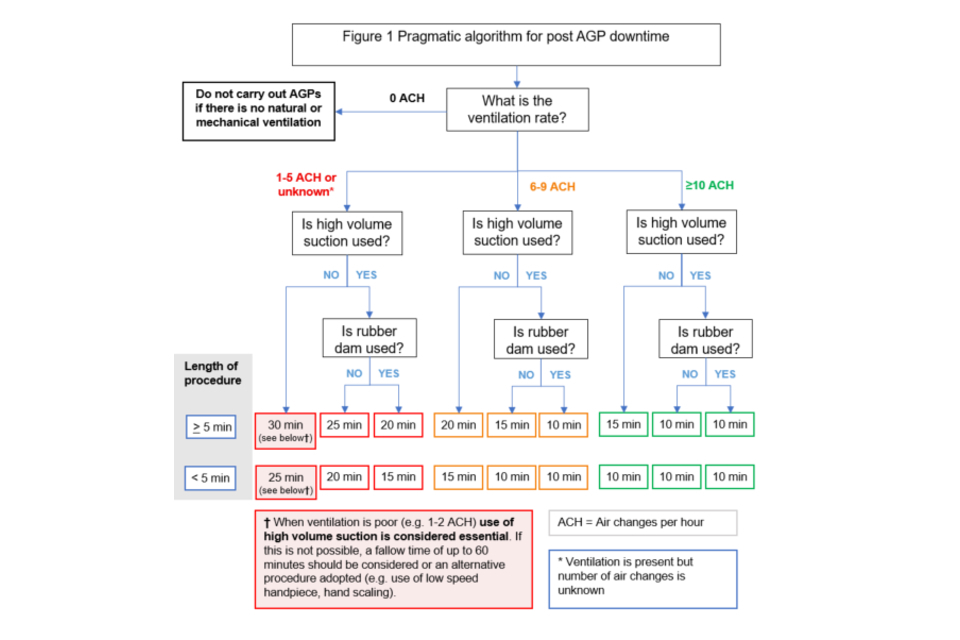
16.2 Algorithm for post AGP downtime: plain text description
Top of chart begins with question: ‘What is the ventilation rate?’
1) If ‘0 ACH’, do not carry out AGPs if there is no natural or mechanical ventilation
2) If ‘1 to 5 ACH or unknown’, then question: ‘Is high volume suction used?’
2a) If ‘Yes’, then question: ‘Is rubber dam used?’
-
If ‘Yes’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 20 minutes
- If ‘less than 5 minutes’ then post AGP down time = 15 minutes
-
If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 25 minutes
- If ‘less than 5 minutes’ then post AGP down time = 20 minutes
2b) If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 30 minutes
- If ‘less than 5 minutes’ then post AGP down time = 25 minutes
3) If ‘6 to 9 ACH’, then question: ‘Is high volume suction used?’
3a) If ‘Yes’, then question: ‘Is rubber dam used?’
-
If ‘Yes’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 10 minutes
- If ‘less than 5 minutes’ then post AGP down time = 10 minutes
-
If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 15 minutes
- If ‘less than 5 minutes’ then post AGP down time = 10 minutes
3b) If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 20 minutes
- If less than 5 minutes’ then post AGP down time = 15 minutes
4) If ‘10 or greater ACH’, then question: ‘Is high volume suction used?’
4a) If ‘Yes’, then question: ‘Is rubber dam used?’
-
If ‘Yes’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 10 minutes
- If ‘less than 5 minutes’ then post AGP down time = 10 minutes
-
If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 10 minutes
- If ‘less than 5 minutes’ then post AGP down time = 10 minutes
4b) If ‘No’, then question: ‘What is the length of procedure?’
- If ‘5 minutes or greater’ then post AGP down time = 15 minutes
- If ‘less than 5 minutes’ then post AGP down time = 10 minutes
17. Safe management of the care environment and equipment
Frequently touched sites and points in waiting rooms and surgeries, for example dental chairs, should be cleaned between patients and:
- equipment used for cleaning, for example cloths, should preferably be disposable; however, reusable items such as mops/buckets should be stored clean and dry between use
- medical devices and equipment should be managed as per manufacturer’s instructions. Decontamination of equipment and the environment following dental treatment should follow country specific guidance for England, Scotland, Wales or Northern Ireland
Reusable (communal) equipment (for example dental chairs, cabinetry, dental lights, x-ray equipment) should be decontaminated:
- between each patient
- after blood and body fluid contamination
- at regular intervals as part of equipment cleaning
Decontamination of equipment must be performed following manufacturer’s advice. Cleaning of care equipment as per manufacturer’s guidance and instruction and recommended product ‘contact time’ must be followed for all cleaning or disinfectant solutions and products.
Other reusable dental equipment (for example handpieces, scalers, probe) should be decontaminated in accordance with manufacturer’s advice and in line with decontamination guidance.
An increased frequency of decontamination and cleaning should be incorporated into the environmental decontamination schedules for areas where there may be higher environmental contamination rates for example:
- toilets
- frequently touched surfaces such as door and toilet handles
- staff room equipment, for example kettles
Decontamination of the care environment must be performed using a detergent and a disinfectant that has proven efficacy against bacteria and viruses, including RSV, influenza and SARS-CoV-2.
18. Additional advice for environmental mitigation measures
18.1 Air cleaning devices
Recirculating air cleaning devices based on HEPA filter systems or UV-C are likely to be effective, but each device needs to be validated by the manufacturer and maintained.
It is difficult to make general recommendations for devices that remove viable microbes from air, either by filtration or microbicidal action. This is because there is variability in the rate they pass air through the device, the removal or inactivation will vary according to filtration or microbicidal efficacy, and over time filters will become progressively blocked. Microbicidal treatment such as UV can become obscured by a build-up of dust and the spectrum of UV emission, critical for microbicidal efficacy, can change over time.
Addition of recirculating air cleaning devices could enhance the effective air change rate. Devices should be correctly sized and the impacts on the room air flow considered. The effectiveness of air cleaning devices will depend on the flow rate of the device, the efficiency of air cleaning and the size of the room.
18.2 Fans
Fans should be cleaned regularly to remove visible soiling and should not be used on the respiratory pathway. Fans should be directed to move air towards windows and mechanical extract points. Fans should not be directed towards doors, driving air into other rooms. Planned preventative maintenance, and cleaning of fans and their blades should continue.
18.3 Air conditioning units
Fixed air conditioning units (for example, wall or ceiling mounted recirculating air coolers -split units) and portable air conditioning, which do not recirculate to other rooms, can be used. Where there is poor air circulation within a room, it may be beneficial to mix air to dilute aerosols. These types of air conditioning will cool staff wearing water repellent PPE.
Portable air conditioning should not be directed towards doors as this will drive air into other rooms, nor should any pipework or cables impede fire doors. Care should be taken when emptying the reservoir of portable air conditioning due to the risk of legionella or other microorganisms being present in the condensate water. See separate HTM 04-01 guidance for England, Wales, Northern Ireland and Scotland on this. Daily emptying of the reservoir should be recorded. Planned maintenance should be carried out on the device following manufacturer’s guidance and should be recorded. Do not use portable air conditioning that incorporates humidifiers.
18.4 Fumigation and fogging
The use of fumigation and fogging devices with disinfection chemicals are not advised for routine cleaning and or disinfection against COVID-19 and should only be considered in healthcare settings when multi-drug resistant organisms cannot be eradicated. Any use must always be under specialist IPC advice.
