Patient safety visits
Secretary of State Jeremy Hunt writes about why patient safety is a priority, and the different approaches taken by different hospitals.

Last week I visited 5 NHS trusts to hear about their plans on patient safety. They told me what they were doing and I told them what I was doing - and the conversations were frank and productive.
I’ve learnt that you can only have a few central priorities in this job if you really want to change things. The question is what to pick - and meeting patient safety campaigners like Julie Bailey, Melissa Mead, Martin Bromiley and James Titcombe made my mind up for me. Their quiet dignity in reliving their own tragedies time after time to try and get the NHS to change how it works is truly humbling. And I started all my presentations by talking about their campaigns and what we in the NHS need to learn from them.
That is not to say there is not great work already happening - much of which I saw on my visits.
Coincidentally when I was in the middle of them the independent American think tank the Commonwealth Fund said of the 11 countries analysed, the UK has the safest healthcare system in the world - a great tribute to the extraordinary lengths NHS staff go to in order to provide excellent care, often in very challenging circumstances. In spite of this, the Hogan, Darzi and Black analysis says that 3.6% of hospital deaths in England have a 50% or more chance of being avoidable - that’s potentially around 150 avoidable deaths every single week.
What does this say about standards of safety in global healthcare?
I visited 3 hospitals in Dorset, then 2 more in Southampton and Portsmouth. Whilst their approaches were different, the priority placed on improving the safety of care was the same.
At the Royal Bournemouth Hospital, the focus was on staff engagement – which we know from Michael West’s research for the King’s Fund is a compelling predictor of organisational performance in the NHS. Royal Bournemouth now has among the highest levels of staff engagement in the country, and it’s having real effects. Their work on emergency laparotomy has more than halved mortality rates.
At Poole Hospital, the focus was on developing as a learning organisation with a huge amount of emphasis on improving mortality reviews and other investigations into adverse incidents. They have reduced deaths from acute kidney injuries by 26% simply by changing the way they record information about care.
At Dorset County Hospital, practical programmes to improve performance on sepsis and gram-negative infections and maternity safety are having a significant impact, following our work nationwide to drive progress in these areas.
At Southampton General, I learnt about their internal medical examiners’ group (IMEG), which reviews all in-hospital deaths to ensure the circumstances of each case are understood, led by the Associate Medical Director Neil Pearce. In Portsmouth, it was incredibly encouraging to see progress towards meeting the 7-day standards as well as the enthusiasm of staff who want to learn from setbacks rather than just move on from them.
The most reassuring thing is that when you talk about patient safety to staff across the country, it feels like preaching to the converted – what a contrast to the organisational and leadership cultures uncovered by Robert Francis at Mid Staffs only a few years ago.
Understandably, I got a number of questions about resources. The NHS is treating more people than it ever has before, and trusts are grappling with significant financial pressures. Some people assume that the goals of sound financial management and providing good quality care are mutually contradictory - but in fact the opposite is the case, with ‘good’ or ‘outstanding’-rated CQC trusts likely to be in surplus and ‘requires improvement/inadequate’-rated ones likely to be in deficit.
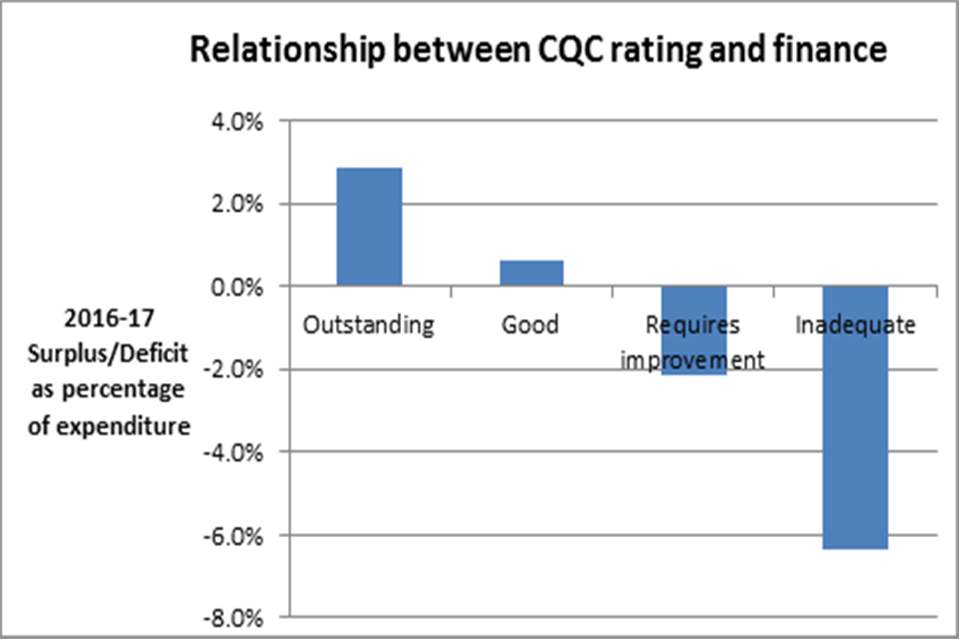
A graph showing the relationship between CQC rating and finance
Looking after patients and looking after pounds go hand in hand - I suspect because good financial management releases more resource for patient care, which in turn reduces the more than 10% of hospital expenditure which goes on avoidable medical mistakes or infections that people catch in hospitals.
There also remains a huge level of variation in clinical processes. According to the brilliant GIRFT programme led by Professor Tim Briggs, there is a 20-fold variation in post-operative infection rates among trusts for orthopaedic surgery – and given each infection not only causes untold human misery but costs £100,000 to put right, the NHS could save millions simply by reducing unwarranted variation.
At every hospital I visited, the issue of staffing numbers came up. I agree with staff that we need more doctors and nurses, which is why we are training tens of thousands of nurses and are rapidly increasing the number of places for doctors. But culture, leadership and transparency are more effective than any ministerial fiat in getting safe staffing numbers.
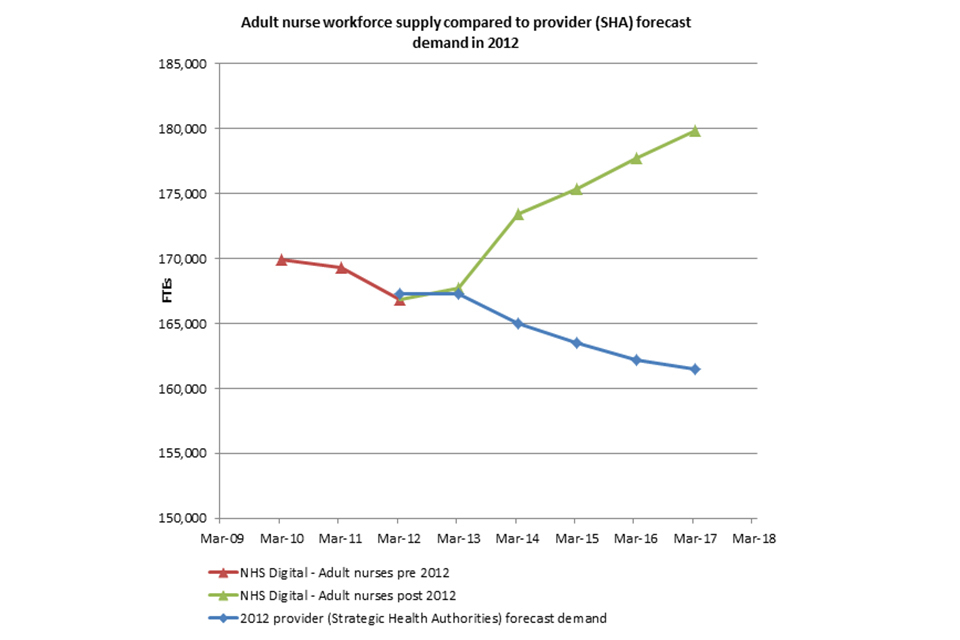
A graph showing adult nurse workforce supply compared to SHA provider forecast demand in 2012
As this graph demonstrates, in 2012, many trusts had cut adult nursing numbers by several thousand - and were planning thousands more cuts to follow. Following the Francis report we then asked them to publish nurse numbers every month on every ward - after which instead of cutting numbers they went up by around 13,000.
That is surely the reason why NHS in-patient satisfaction rates are currently at their highest ever level, despite ever-growing demands for care.
There is clearly a lot more to do on patient safety, but it was encouraging to feel that for NHS staff this is pushing at an open door.