Quarterly epidemiological commentary: mandatory Gram-negative bacteraemia, MRSA, MSSA and C. difficile infections (data up to July to September 2022)
Updated 9 October 2025
Applies to England
UK Health Security Agency and this report
Since the UK Health Security Agency (UKHSA) was created in April 2021, it has been responsible for protecting every member of every community from the effect of infectious diseases, chemical, biological, radiological, and nuclear incidents and other health threats. We provide intellectual, scientific, and operational leadership at national and local level, as well as on the global stage, to make the nation’s health secure.
The agency replaces Public Health England (PHE) and is an executive agency of the Department of Health and Social Care (DHSC). The transition to UKHSA included the integration of both staff and systems. Accordingly, the systems and processes responsible for the publication of the previous quarterly epidemiological commentaries were incorporated into UKHSA. The same methods of data capture, analysis and dissemination have been employed in the production of this report.
Data included in this quarterly epidemiological commentary
This report contains quarterly, national-level epidemiological commentaries for meticillin-resistant Staphylococcus aureus (MRSA), meticillin-susceptible Staphylococcus aureus (MSSA), Escherichia coli (E. coli), Klebsiella spp. and Pseudomonas aeruginosa (P. aeruginosa) bacteraemia and Clostridioides difficile infection (CDI). These include analyses on counts and incidence rates of all reported, hospital-onset (previously referred to as trust-apportioned) and community-onset (previously referred to as non-trust-apportioned) cases of MRSA, MSSA, E. coli, Klebsiella spp. and P. aeruginosa bacteraemia and CDI. All data tables associated with this report are included in an OpenDocument spreadsheet.
Revisions to data included are covered by a data-specific revisions and correction policy.
Citation to UK Health Security Agency (UKHSA), healthcare associated infections (HCAI) and antimicrobial resistance (AMR) division is required, if these data are used for publication elsewhere, using the content below.
Citation: UK Health Security Agency. Quarterly epidemiology commentary: mandatory MRSA, MSSA and Gram-negative bacteraemia and C. difficile infection in England (up to July to September 2022) London: UK Health Security Agency, January 2023.
Data for this report were extracted from UKHSA’s HCAI data capture system (DCS) on 8 November 2022.
COVID-19 and these data
The coronavirus (COVID-19) pandemic appears to have altered the pattern of bloodstream infections (BSIs) and CDIs previously being observed. In general, counts of all reported BSI and CDI cases covered in this report during the financial year April 2020 to March 2021 were lower than would be expected, while counts of hospital-onset Klebsiella spp. and P. aeruginosa BSI cases increased rapidly, exceeding previous counts of cases observed in this setting. Most of the declines in bacteraemia and CDI cases initially observed during the COVID-19 pandemic occurred within community-onset cases.
Analysis of voluntary laboratory surveillance data from financial year 2020 to 2021 to financial year 2021 to 2022, also showed a reduction (albeit to different extents) in cases of the majority of other bloodstream infections not covered by the mandatory surveillance during this period. As the voluntary laboratory surveillance shows similar trends to the mandatory surveillance scheme, these changes do not appear to be a specific ascertainment problem in the mandatory programme.
During the second wave (September 2020 to April 2021) and third wave (May 2021 to March 2022), covering quarters October to December 2020 to January to March 2022, the overall number of infections increased after the initial declines seen during the first wave (January to June 2020) for all organisms, except for E. coli and MRSA bacteraemias which are still at a lower rate than pre-pandemic levels. Incidence rates of hospital-onset CDI and MSSA, Klebsiella spp. and P. aeruginosa bacteraemias were increased compared with the pre-pandemic period.
It has been concluded that the increases seen in hospital-onset Klebsiella spp. and P. aeruginosa BSI cases during the first and second waves of the COVID-19 pandemic corresponded with increases in these BSI as co or secondary infections in persons with COVID-19 and ICU-associated BSI cases (1). It was also observed that the increases seen in hospital-onset Klebsiella spp. and P. aeruginosa BSI cases corresponded with increases in patients with respiratory-related conditions and ICU stays.
In response to the pandemic, elective procedures in hospitals were initially cancelled or delayed, although some activity resumed between COVID-19 waves. As a result, the number of occupied overnight beds (the denominator used for hospital-onset infection rates) was much lower than would otherwise be expected during these periods. This was particularly so for financial year April 2020 to March 2021, with some increase in financial year April 2021 to March 2022, albeit remaining lower than in financial year April 2019 to March 2020. Therefore, increased incidence rates of hospital-onset infection have been reported, despite a decrease in the counts of infections, in some instances. The relatively slower increase in incidence rates than counts of infections is due to a steady return to the typical number of overnight bed-days in July to September 2022, compared with the unusually low levels in July to September 2020. It is worth noting that overnight bed-days were 24.9% higher in July to September 2022 when compared with the same quarter in 2020. For these reasons, data from the beginning of the pandemic should be interpreted with caution.
Epidemiological analyses of Gram-negative bacteraemia
E. coli bacteraemia
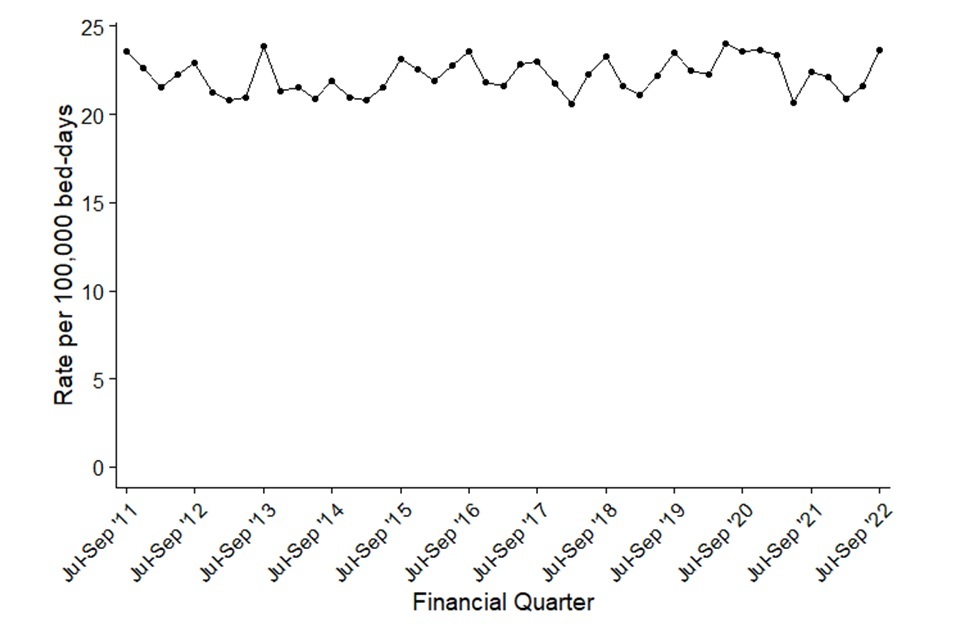
The incidence rate of all reported E. coli bacteraemia increased each financial year between the initiation of the mandatory surveillance of E. coli bacteraemia in July 2011 and the start of the COVID-19 pandemic (January to March 2020, Figure 1a). This increase was primarily caused by community-onset cases (see Table S1 in the accompanying data tables). The number and incidence rates of all reported and community-onset cases declined after the start of the pandemic but remain higher than observed at the start of E. coli surveillance (Figure 1a). In contrast, the incidence rate of hospital-onset cases remained relatively stable during the same period, except for a sharp reduction (20.7 cases per 100,000 bed days) observed in April to June 2021 (Figure 1b). This is followed by a steady return to pre-pandemic rates, however remaining lower than the start of E. coli surveillance.
Comparing quarters July to September 2011 and July to September 2022, the count and the incidence rate of all reported cases of E. coli bacteraemia increased by 26.6% from 8,275 cases to 10,473 and by 19.2% from 61.8 to 73.7 cases per 100,000 population, respectively. Similarly, over the same period, the count of community-onset cases increased by 33.7% from 6,279 to 8,397, while the incidence rate increased by 25.9% from 46.9 to 59.1 cases per 100,000 population. Concurrently, the count of hospital-onset cases increased by 4.0% from 1,996 to 2,076 cases. The incidence rate of hospital-onset cases remained broadly the same with a slight increase of 0.4% from 23.6 per 100,000 bed-days to 23.7 per 100,000 bed-days.
When comparing the most recent quarter (July to September 2022) with the same period in the previous year (July to September 2021) there was a 3.5% increase in both the count and incidence rate of all reported cases from 10,120 to 10,473 and 71.2 to 73.7 per 100,000 population, respectively (Figure 1a). Over the same time period, community-onset E. coli bacteraemia cases increased by 1.3% from 8,287 to 8,397, with the community-onset incidence rate increasing by the same percentage (1.3% from 58.3 to 59.1 per 100,000 population, Table S1 in the accompanying data tables). In July to September 2022, hospital-onset E. coli bacteraemia cases increased by 13.3% from 1,833 to 2,076 compared with July to September 2021 (Figure 1b). which corresponded to an incidence rate increase of 5.8% from 22.4 to 23.7 per 100,000 bed-days.
When comparing the most recent quarter (July to September 2022) with the equivalent pre-pandemic period in 2019, there is a 11.5% decrease in total cases from 11,828 to 10,473, with a corresponding decrease of 11.6% in the incidence rate from 83.4 to 73.7 cases per 100,000 population (Figure 1a). Community-onset cases decreased by 14.3% from 9,801 to 8,397. Similarly, the incidence rate of community-onset cases also declined by 14.5% from 69.1 to 59.1 cases per 100,000 population. Finally, the total numbers of hospital-onset cases increased by 2.4% compared with the same period from 2,027 to 2,076, while little difference was seen in the hospital-onset incidence rate which increased by 0.7% from 23.5 to 23.7 cases per 100,000 bed-days (Figure 1b). These highlight the slow increase in reports of E. coli bacteraemia cases since the start of the COVID-19 pandemic, with all reported rates for July to September returning to those last seen in 2015.
There appears to be a seasonality to the incidence of all-reported E. coli bacteraemia cases, with the highest rates observed between July to September of each year, although care is required in interpreting data for financial years April 2020 to March 2021 and April 2021 to March 2022 due to the reduction in cases and hospital activity during the pandemic.
Figure 1a. Quarterly rates of all reported E. coli bacteraemia: July to September 2011, to July to September 2022
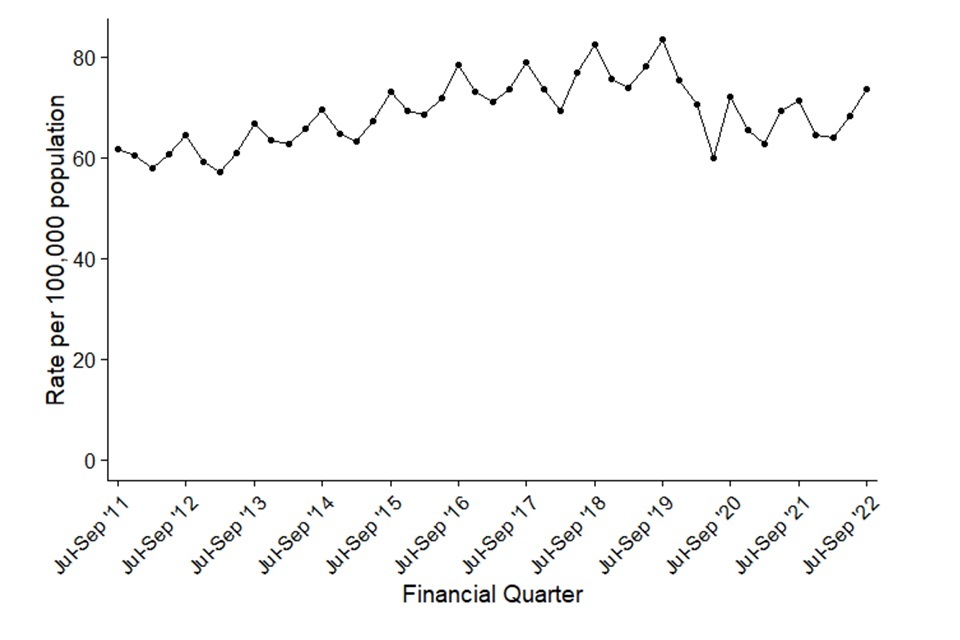
Figure 1b. Quarterly rates of hospital-onset E. coli bacteraemia: July to September 2011, to July to September 2022
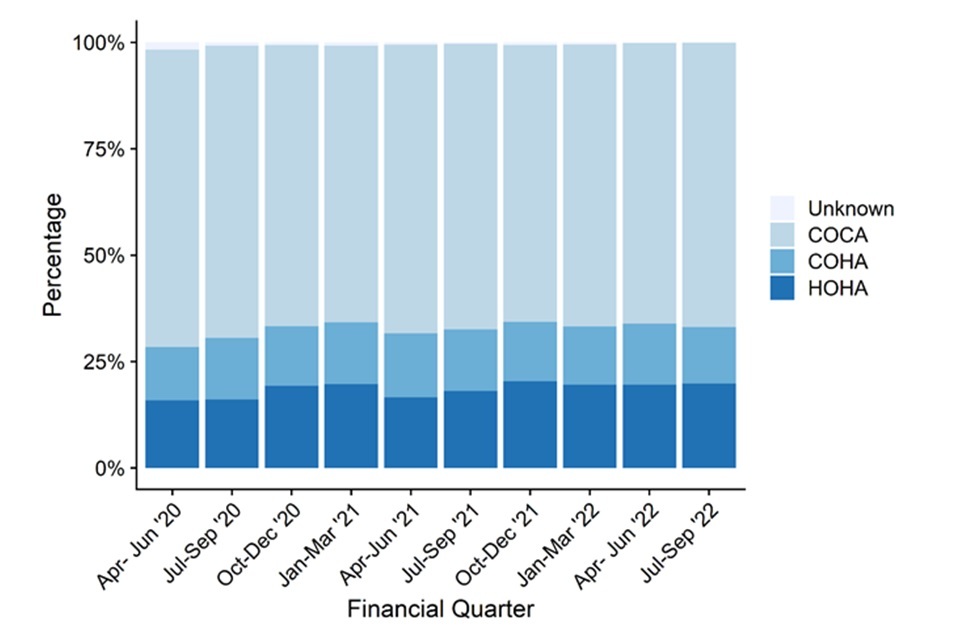
Since April 2020, community-onset E. coli bacteraemia cases have been further categorised based on a patient’s previous discharge (or not) from the same reporting acute trust within 28 days.
Cases with no previous discharge within 28 days prior to the current episode start date were recorded as community-onset, community-associated (COCA) cases. These accounted for the majority of reported community-onset E. coli bacteraemia between April to June 2020 and July to September 2022. While there have been some fluctuations, the proportion of COCA cases has remained similar at around two-thirds of all cases since.
Although the distribution of cases by these categories remained broadly stable, when comparing the number of community-onset healthcare-associated (COHA) cases from the current quarter (July to September 2022) with the same quarter in 2021, COHA cases decreased from 14.4% to 13.3%. COCA cases also decreased from 67.2% to 66.8% of cases. Hospital-onset healthcare associated (HOHA) cases on the other hand, increased from 18.1% to 19.8%.
Figure 1c. Percentage of E. coli bacteraemia cases by prior trust exposure: April to June 2020 to July to September 2022
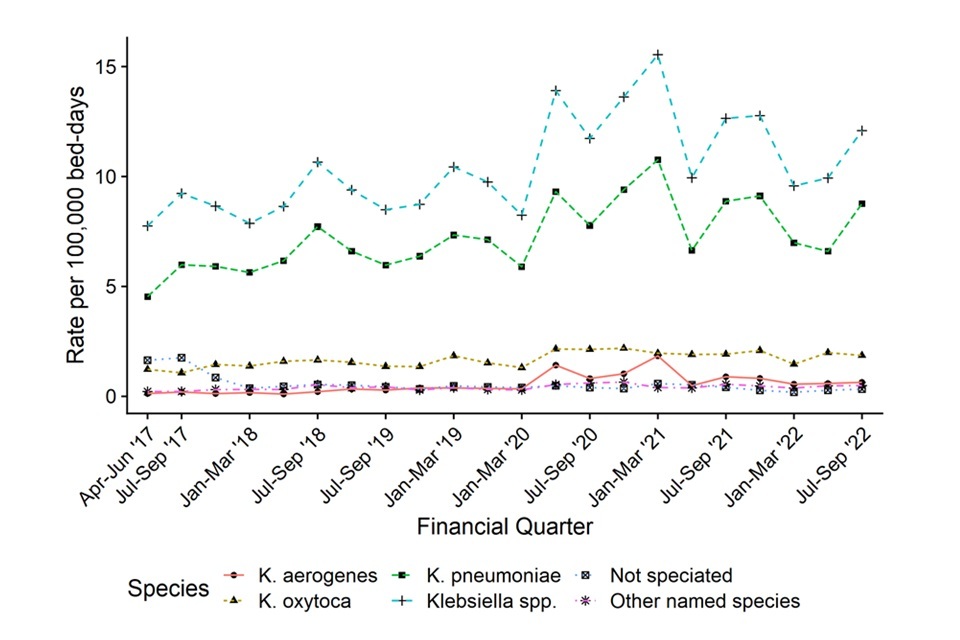
Klebsiella spp. bacteraemia
Between April to June 2017 and July to September 2022, there was a 35.1% increase in the count of all reported Klebsiella spp. bacteraemia cases from 2,348 to 3,173 and a 31.8% increase in the incidence rate from 16.9 to 22.3 cases per 100,000 population (Figure 2a). This marks the highest counts and rates seen since the inception of the Klebsiella spp. surveillance.
The count of community-onset cases increased by 25.9% from 1,678 to 2,113 cases, between the April to June 2017 and July to September 2022, with the incidence rate increasing by 22.8% from 12.1 to 14.9 cases per 100,000 population. Over the same period, the count of hospital-onset cases increased by 58.2% from 670 to 1,060 cases and the incidence rate increased by 55.9% from 7.8 to 12.1 cases per 100,000 bed-days (Figure 2b and Table S2 in the accompanying data tables). Counts and rates of hospital-onset Klebsiella spp. had an observed peak between the July to September 2020 and January to March 2021 quarters which were during the COVID-19 pandemic. Both counts and rates of hospital-onset cases increased to levels which were the highest observed since the inception of mandatory Klebsiella spp. surveillance. The incidence rate of hospital-onset cases peaked at 15.5 cases per 100,000 bed-days in January to March 2021. The specific causes of this increase are still being investigated, but we do know these trends coincided with increased incidence of COVID-19 (1).
In the most recent quarter, the number of hospital-onset Klebsiella spp. bacteraemia cases increased by 2.3.% from 1,036 to 1,060 with a corresponding decrease in the incidence rate of 4.4% from 12.6 to 12.1 per 100,000 population, when compared with the same quarter in the previous financial year (July to September 2021). Compared with the same period in 2019, a more typical year prior to the pandemic, the counts and the incidence rate of hospital-onset cases increased by 17.8% and 15.8%, respectively. The number of all reported cases and incident rate in the current quarter increased by 6.2% from 2,989 to 3,173 cases and from 21.1 to 22.3 per 100,000 population, respectively (Figure 2a and Table S2 in the accompanying data tables). The number of community-onset Klebsiella spp. cases increased by 1.1% (absolute change 2,089 to 2,113) and the infection rate increased from 14.7 to 14.9 per 100,000 population (Table S2 in the accompanying data tables).
During the July to September 2022 quarter, 72.5% (2,302 of 3,173) of all reported Klebsiella spp. bacteraemia cases were caused by Klebsiella pneumoniae, similar to the same quarter in the previous year (70.0%, July to September 2021). In July to September 2022, 16.1% of cases were identified as Klebsiella oxytoca (511 out of 3,173), a decrease from the 18.0% reported in July to September 2021.
The incidence rate of the majority of Klebsiella species increased at roughly the same pace (Figure 2a and Table S2 in the accompanying data tables). The exception to this was the incidence rate of K. oxytoca, which increased within hospital-onset cases around the start of the pandemic and subsequently stabilised at between 1.9 to 2.1 per 100,000 bed days.
There is evidence of seasonality in the trend of all reported Klebsiella spp. bacteraemia cases, with the highest incidence rates normally observed in July to September of each year (Figure 2a). However, it is important to evaluate April 2020 to March 2022 with caution due to changes related to the COVID-19 pandemic.
Figure 2a. Quarterly rates of all reported Klebsiella spp. bacteraemia by species: April to June 2017, to July to September 2022
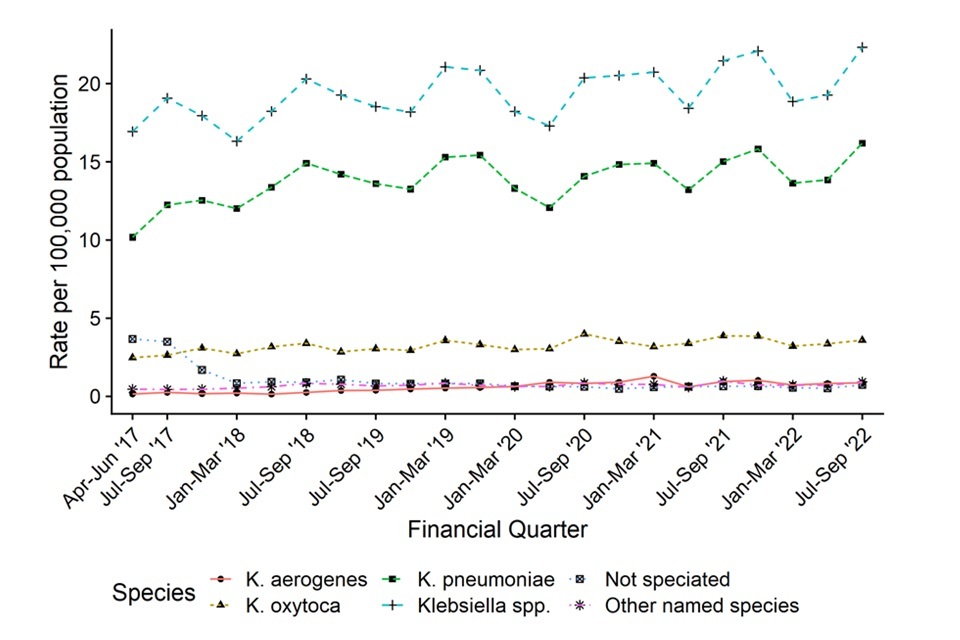
Figure 2b. Quarterly rates of hospital-onset Klebsiella spp. bacteraemia: April to June 2017, to July to September 2022
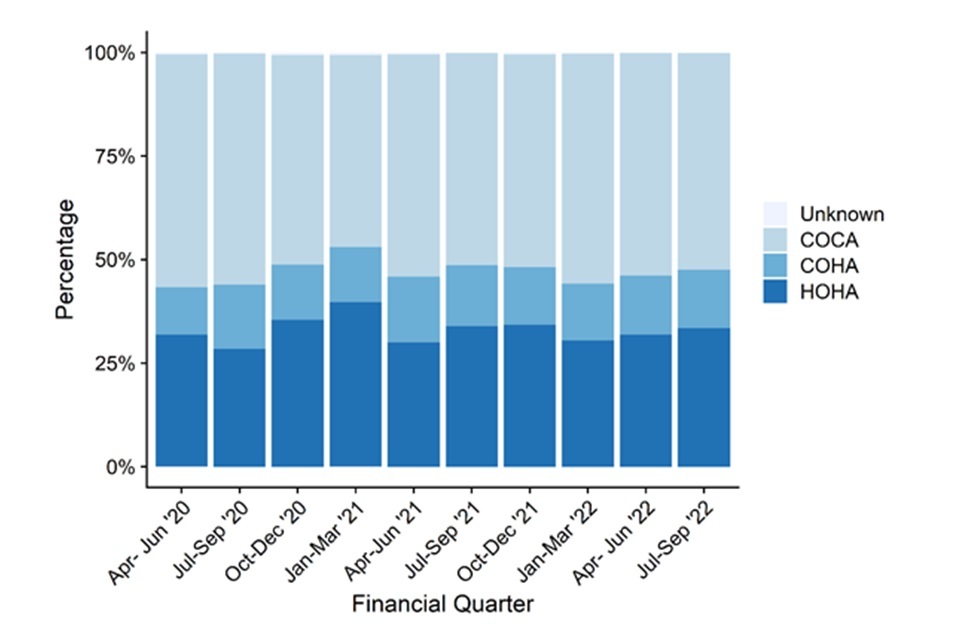
Like E. coli bacteraemia, between April to June 2020 and July to September 2022, COCA cases made up the largest percentage of all Klebsiella spp. bacteraemia, accounting for around half of all cases (Figure 2c).
Since the start of surveillance, the proportion of HOHA cases peaked at 39.7% in January to March 2021 alongside a decline in COCA cases to 46.4%. Coincidently, the increase in HOHA cases coincided with the third lockdown (January 2021), where an increase in Klebsiella spp. BSIs cases were observed in the hospital setting (1).
Comparing July to September 2022 with the same quarter in 2021, HOHA cases stayed broadly the same at 34.0% and 33.4% of all cases, as did COHA cases from 14.7% to 14.1%. While the percentage of COCA cases increase slightly from 51.1% to 52.3% of all Klebsiella spp. bacteraemia cases. (Figure 2c and Table S2a in the accompanying data tables).
Figure 2c. Percentage of Klebsiella spp. bacteraemia cases by prior trust exposure: April to June 2020, to April to June 2022
Figure 2c. Percentage of Klebsiella spp. bacteraemia cases by prior trust exposure: April to June 2020, to April to June 2022
Pseudomonas aeruginosa bacteraemia
Between April to June 2017 and July to September 2022, there was a 17.8% increase in the count, and a 14.9% increase in the incidence rate, of all reported P. aeruginosa bacteraemia cases from 1,015 to 1,196 and from 7.3 to 8.4 cases per 100,000 population, respectively (Figure 3a). The count and the incidence rate of community-onset cases also increased by 16.4% from 639 to 744 cases and by 13.6% from 4.6 to 5.2 cases per 100,000 population, respectively. Over the same period, the count and the incidence rate of hospital-onset cases increased by 20.2% from 376 to 452 cases and by 18.5% from 4.3 to 5.2 cases per 100,000 bed-days, respectively (Figure 3b and Table S3 in the accompanying data tables).
Similarly, to Klebsiella spp. cases, increases in counts and rates of hospital-onset P. aeruginosa were observed during the second wave of the COVID-19 pandemic. The counts and rates of hospital-onset P. aeruginosa increased between the quarters July to September 2020 and January to March 2021, to levels not seen previously since the start of the mandatory surveillance of P. aeruginosa bacteraemia. The incidence rate of hospital-onset cases peaked at 7.0 cases per 100,000 bed-days in the January to March 2021 period. The reasons for this increase have been investigated and it was observed that this increase coincided with a rise in the percentage of hospital-onset bacteraemia cases who were also positive for COVID-19 (1).
Comparing July to September 2022 with the same period in the previous year (July to September 2021), the total reported counts decreased from 1,270 to 1,196, and a 5.8% decrease in both counts and incidence rate from 8.9 to 8.4 cases per 100,000 population was seen. A 9.1% decline was observed in the hospital-onset counts,497 to 452, with a corresponding decrease of 15.0% in the hospital-onset incidence rate, from 6.1 to 5.2 cases per 100,000 bed-days, respectively. Community-onset cases displayed a 3.8% decrease in both counts and rates from 773 in July to September 2021 to 744 in July to September 2022 and 5.4 to 5.2 per 100,000 population, respectively.
Compared with the same period in 2019 (July to September 2019), which was pre-pandemic and a more typical year, there was a equivocal difference in the count of all reported cases from 1,197 to 1,196, whilst the incidence rate remained 8.4 per 100,000 population for both periods (Figure 3a and Table S3 in the accompanying data tables). During the same period, counts of community-onset P. aeruginosa cases saw a similar decrease of 6.4% from 795 to 744, with a corresponding decline in the community-onset incidence rate of 6.6% from 5.6 to 5.2 per 100,000 population (Table S3 in the accompanying data tables). Conversely, a rise in counts and rates of hospital-onset P. aeruginosa cases of 12.4% from 402 to 452 in counts and 10.6% increase from 4.7 to 5.2 per 100,000 bed-days was observed (Figure 3b and Table S3 in the accompanying data tables). However, it is worth noting that the bed-days data for the current quarter is 1.7% higher than it was in July to September 2019.
There is evidence of seasonality in the incidence of all-reported P. aeruginosa bacteraemia cases, with the highest rates normally observed in the July to September quarter of each financial year ((Figure 3a)
Figure 3a. Quarterly rates of all reported P. aeruginosa bacteraemia: April to June 2017, to July to September 2022

Figure 3b. Quarterly rates of hospital-onset P. aeruginosa bacteraemia: April to June 2017, to July to September 2022

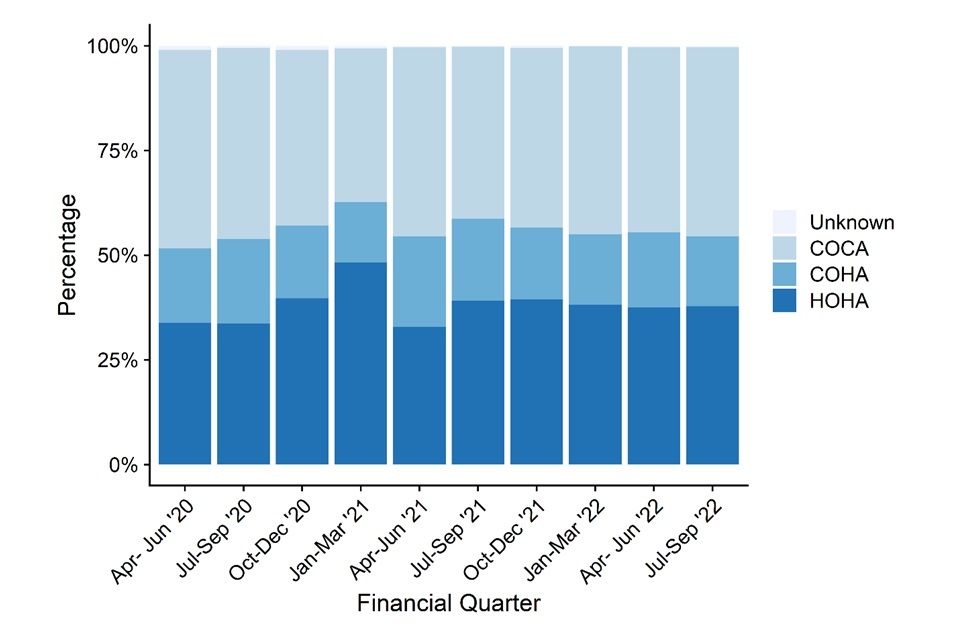
Similarly, to E. coli and Klebsiella spp., COCA cases (around 50%) tend to dominate P. aeruginosa bacteraemia cases between the April to June 2020 and January to March 2022 quarters. However, in the January to March 2021 quarter, HOHA cases (48.2%) surpassed COCA cases (36.8%) for the first time since April 2020 coinciding with the peak of the second wave of the COVID-19 pandemic.
Comparing July to September 2022 with the same quarter in 2021, HOHA and COHA cases decreased from 39.1% to 37.8% and 19.6% to 16.7% of all P. aeruginosa bacteraemia cases, respectively. The percentage of COCA cases increased from 41.0% to 45.2%. (Figure 3c and Table S3a in the accompanying data tables).
Figure 3c. Percentage of P. aeruginosa bacteraemia cases by prior trust exposure: April to June 2020, to July to September 2022
Epidemiological analyses of Staphylococcus aureus bacteraemia
MRSA bacteraemia
There has been a considerable decrease in the incidence rate of all reported MRSA bacteraemia cases since the enhanced mandatory surveillance began in April 2007 (Figure 4a and Table S4 in the accompanying data tables). The incidence rate of all reported cases fell by 86.9% from 10.2 cases per 100,000 population in the April to June 2007 quarter to 1.3 cases per 100,000 in the April to June 2014 quarter. The rate has fluctuated between 1.0 and 1.8 since then and is currently at 1.4 cases per 100,000 population in the most recent quarter (July to September 2022).
A similar trend was observed with the incidence rate of hospital-onset cases (Figure 4b and Table S4 in the accompanying data tables). There was a steep decrease of 85.4%, from 4.9 cases per 100,000 bed-days in the April to June 2008 period to 0.8 case per 100,000 bed-days in the April to June 2014 period. Subsequently, between April to June 2014 and July to September 2022, the rate has increased to 0.9 cases per 100,000 bed-days. Since April to June 2014, there have been fluctuations in both the number of hospital-onset infections and the hospital-onset incidence rate, ranging between 48 and 107 and 0.6 and 1.4 cases per 100,000 population, respectively.
Similarly to Klebsiella spp. and P. aeruginosa, there was a peak in the incidence rate of hospital-onset MRSA bacteraemia, at 1.4 cases per 100,000 bed-days during January to March 2021 (Figure 4b and Table S4 in the accompanying data tables). This was the highest rate seen for hospital-onset MRSA bacteraemia since April to June 2011. The reasons for this increase are still being investigated, although it has been observed that this increase coincided with a rise in the percentage of hospital-onset bacteraemia cases who were also positive for COVID-19(1).
There were no changes in the total case count and incidence rate, 200 total cases and 1.4 cases per 100,000 population, respectively (Figure 4a and Table S4 in the accompanying data tables) when comparing the same period in 2019 (July to September 2019), which was pre-pandemic, with the current quarter being analysed. Community-onset MRSA bacteraemia counts and rates decreased by approximately 9.7% from 134 to 121 and 0.95 to 0.85 cases per 100,000 population respectively (Table S4 in the accompanying data tables). On the contrary, the count of hospital-onset MRSA bacteraemia cases increased by 19.7% from 66 to 79, with a 17.7% increase in incidence rate from 0.77 to 0.90 per 100,000 bed-days (Figure 4b and Table S4 in the accompanying data tables).
Figure 4a. Quarterly rates of all reported MRSA bacteraemia: April to June 2007, to July to September 2022

Figure 4b. Quarterly rates of hospital-onset MRSA bacteraemia: April to June 2008, to July to September 2022

MSSA bacteraemia
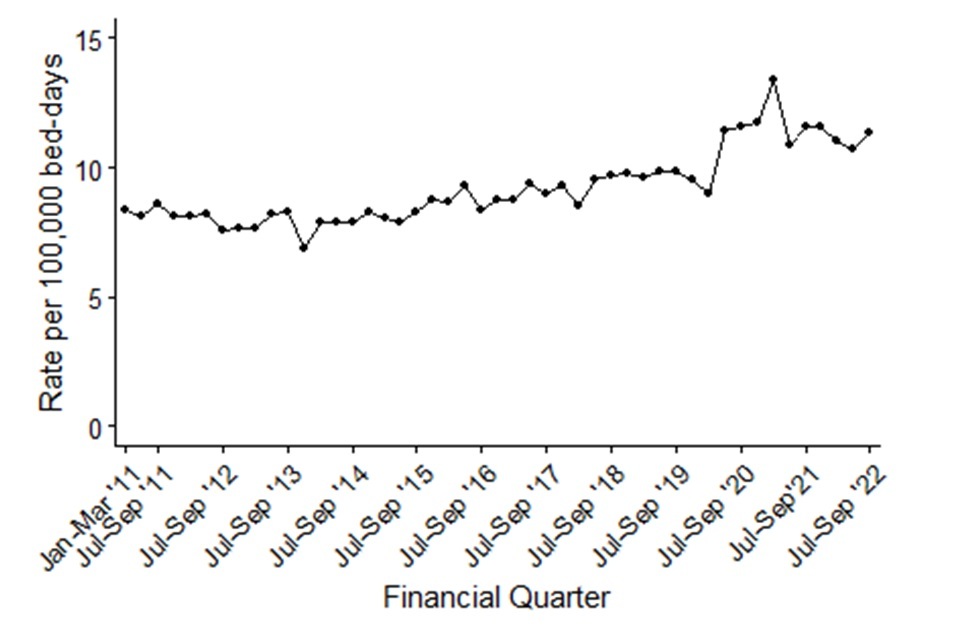
Since the mandatory reporting of MSSA bacteraemia began in January 2011, there has been a general trend of increasing count and incidence rate of cases. The count of all reported cases of MSSA bacteraemia increased by 49.3% from 2,199 to 3,283 between January to March 2011 and July to September 2022. This was accompanied by a 37.5% increase in incidence rate from 16.8 to 23.1 per 100,000 population (Figure 5a and Table S5 in the accompanying data tables). These increases have been primarily driven by increases in community-onset cases.
Between the January to March 2011 and July to September 2022 quarters, the count and the incidence rate of community-onset cases increased by 56.5% and 44.2% respectively from 1,464 to 2,291 cases and from 11.2 to 16.1 cases per 100,000 population (Table S5 in the accompanying data tables). Over the same period, the count of hospital-onset cases increased by 35.0% from 735 to 992 cases, while the hospital-onset incidence rate increased by 35.7% from 8.3 to 11.3 cases per 100,000 bed-days (Figure 5a, Figure 5b and Table S5a in the accompanying data tables).
Since the beginning of the COVID-19 pandemic (April to June 2020) to the current quarter, reported MSSA cases dropped to 2,754 and the rate fell to 19.6 cases per 100,000 population. However, this count and rate is still higher than at the beginning of the MSSA surveillance (January 2011). This drop in cases and rates preceded a steady increase in quarterly counts followed by another drop in all counts and rates towards the end of wave two of the COVID-19 pandemic (April to June 2021). Subsequently, all reported cases and rates have been on a steadily increasing trend. Between April to June 2021 and the most recent quarter, a 9.5% increase in all counts of MSSA bacteraemia has been observed (2,998 to 3,283). This coincides with an 8.3% increase in incidence rate from 21.3 to 23.1 per 100,000 population.
Since the July to September 2020 quarter, there has been an increase in the incidence rate of hospital-onset MSSA bacteraemia cases. The increase in hospital-onset rate is, in part, a result of reduced hospital activity, resulting in reduced occupied overnight bed-days (Table S5 in the accompanying data tables), the denominator used for the hospital-onset rates. The increasing rate culminated in a peak during the January to March 2021 quarter, when it was 13.4 cases per 100,000 bed-days and 998 cases reported. This was the highest MSSA hospital-onset rate and count that has been observed since the inception of MSSA surveillance. This pattern is comparable to that observed in both Klebsiella spp. and P. aeruginosa.
In comparison with July to September 2019, which was during a pre-pandemic year which was more typical, there has been a 3.7% increase in the counts of all reported cases from 3,166 to 3,283 and a 3.5% increase in the rate from 22.3 to 23.1 cases per 100,000 population in the current quarter (July to September 2022). Over this same period, hospital-onset MSSA bacteraemia cases have increased by 17.0% from 848 to 992, which corresponds to a 15.0% increase in the incidence rate from 9.8 to 11.3 per 100,000 bed-days. Community-onset MSSA bacteraemia cases displayed the least change with a slight decrease in both counts and incidence rate of 1.2% from 2,318 to 2,291, and 1.4% from 16.3 to 16.1 per 100,000 population, respectively over the same period.
Figure 5a. Quarterly rates of all reported MSSA bacteraemia: January to March 2011, to July to September 2022
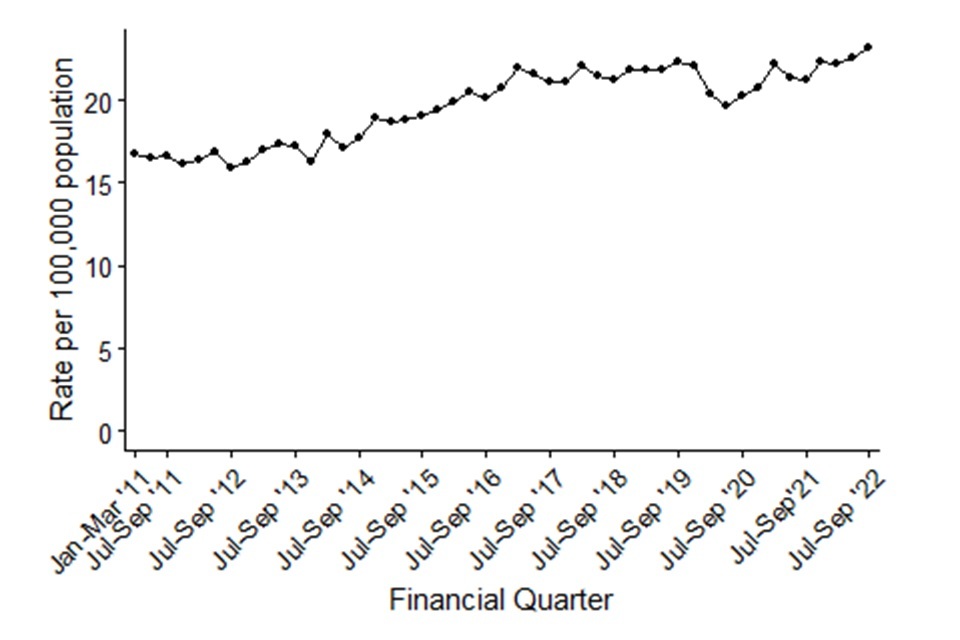
Figure 5b. Quarterly rates of hospital-onset MSSA bacteraemia: January to March 2011, to July to September 2022
Epidemiological analyses of Clostridioides difficile infection
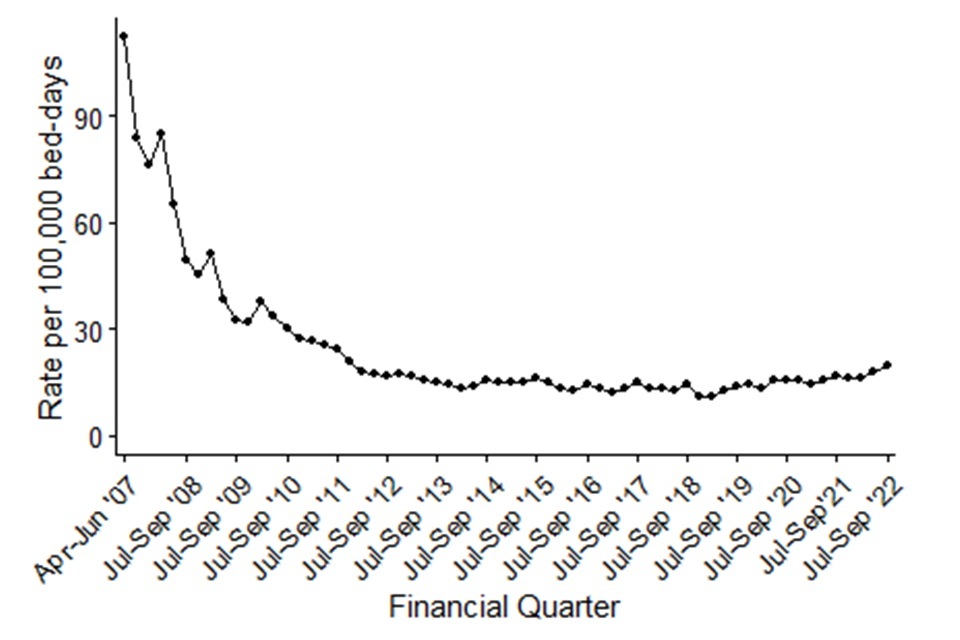
Since the initiation of C. difficile infection (CDI) surveillance in April 2007, there has been an overall decrease in the count and incidence rate of both all-reported and hospital-onset cases (Figure 6a, Figure 6b and Table S6 in the accompanying data tables).
The greatest decrease in CDI cases and incidence rate occurred between the April to June 2007 and January to March 2012 quarters. There was a 78.0% decrease in all reported cases of CDI, from 16,864 to 3,711 cases, and an associated 78.8% reduction in incidence rate, from 131.6 cases to 27.9 cases per 100,000 population, remaining stable thereafter. Subsequently, between January to March 2012 and July to September 2022, the count of all-reported cases increased by 19.9%, from 3,711 to 4,449 cases. However, the incidence rate reduced by 12.2% from 27.9 to 31.3 cases per 100,000 population. This is, in part, due to an absolute population count increase of 6.9%.
There were similar, but greater, reductions among hospital-onset CDI cases with an 84.5% reduction in count of cases between April to June 2007 and January to March 2012 from, 10,436 to 1,613 cases, and an 83.9% reduction in the incidence rate, from 112.1 to 18.1 per 100,000 bed-days. This was followed by a further 7.6% increase in the count of cases, from 1,613 to 1,736 cases and an increase of 9.5% in the incidence rate from 18.1 to 19.8 cases per 100,000 bed-days between January to March 2012 and July to September 2022.
When comparing the most recent quarter with July to September 2019, which was a more typical period prior to the first wave of the COVID-19 pandemic, there has been a 22.3% increase in the count of all reported cases from 3,639 to 4,449. This corresponds with an 22.0% increase in the incidence rate, from 25.6 to 31.3 cases per 100,000 population (Figure 6a and Table S6 in the accompanying data tables). Community-onset CDI cases increased by 11.7%, from 2,428 to 2,713, while the rate increased by 11.5%, from 17.1 to 19.1 per 100,000 population (Table S6 in the accompanying data tables). Hospital-onset CDI cases increased by 43.4%, from 1,211 to 1,736, which corresponds to an incidence rate increase of 41.0%, from 14.0 to 19.8 cases per 100,000 bed-days (Figure 6b and Table S6 in the accompanying data tables). The reasons for these observed increases are still being investigated.
Figure 6a. Quarterly rates of all reported C. difficile: April to June 2007, to July to September 2022
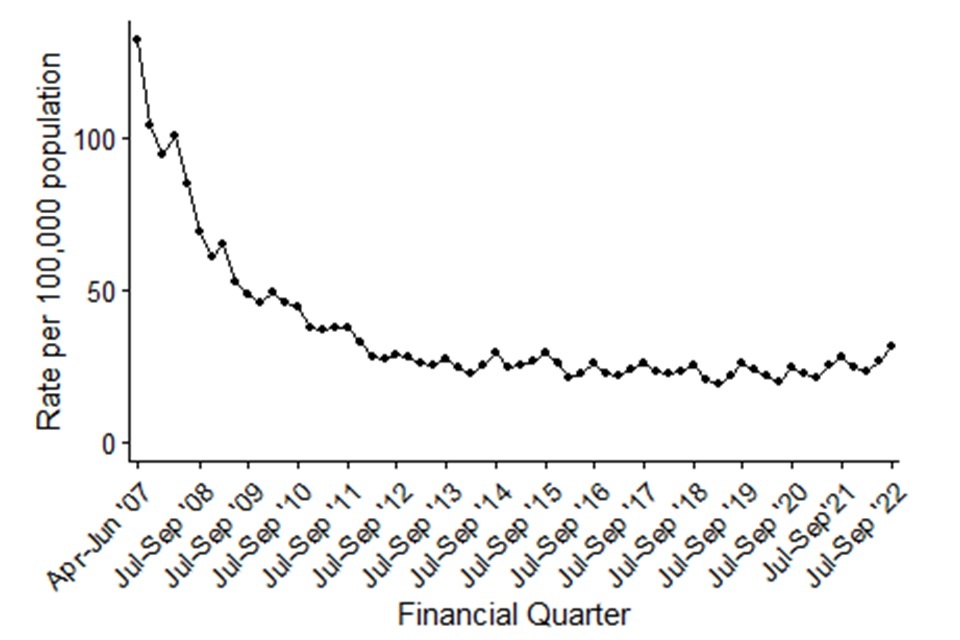
Figure 6b. Quarterly rates of hospital-onset C. difficile: April to June 2007, to July to September 2022
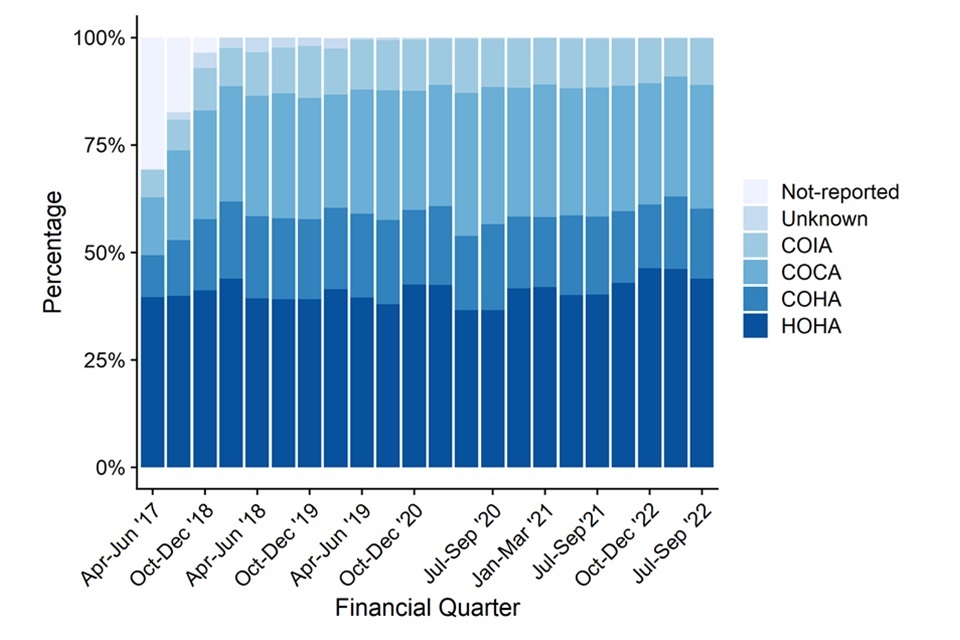
Between April to June 2017 and July to September 2022, the largest percentage of cases were HOHA, at approximately 40% of all cases but this has increased 43.9%. Over the same period, the percentage of COCA cases increased from 13.4% to 28.8% (although primarily in the early quarters) and COHA cases have increased from 9.7% to 16.3% of all CDI. Community Onset Indeterminate Association (COIA) cases increased from 6.3% to 10.8% of all CDI. Much of the increase observed is likely due to improved data quality as shown by the sharp decline of cases with missing or not reported data (Figure 6c and Table S7 in the accompanying data tables).
Figure 6c. Percentage of CDI cases by prior trust exposure April to June 2017, to July to September 2022
Appendix
Bed-day data
For bacteraemia and CDI, the average bed-day activity reported by acute trusts via KH03 returns is used to derive the bed-day denominator for acute trust incidence rate rates (assigned and apportioned). As of quarter 1 2011 to 2012, bed-day data has been available on a quarterly basis and has been used as such for quarter 2 2011 to 2012, to quarter 2 2022 to 2023.
However, UKHSA has reviewed its policy for processing KH03 data. Data irregularities identified have been flagged with colleagues at NHS England (data owners of the KH03 data set). Until we receive confirmation that any identified change in the occupied overnight bed-days for an acute trust is anomalous, UKHSA now uses the data as published in the KH03 data set. This affects all reports published since 1 December 2015 and incidence rate rates published prior that time will differ slightly as a result.
For the KH03 data used to calculate rates included in this report to be consistent over the full-time period, previously amended KH03 data for trust United Lincolnshire Hospitals (RWD) for financial year 2014 to 2015, has been altered to reflect that published in the KH03 data set. Please note that this could lead to slight differences in hospital-onset assigned rates when compared with publications prior to 1 December 2015.
KH03 data can be found on the NHS England website.
Missing data for acute trusts in the KH03 returns will continue to be processed as before, where the KH03 return for the same quarter from the previous year will be used as a proxy. The following acute trusts were thus affected:
-
Moorfields Eye Hospital NHS Foundation Trust (RP6) 2007 to 2008, and 2008 to 2009 KH03 figures: replaced with 2006 to 2007 KH03 figure
-
Rotherham NHS Foundation Trust (RFR): 2009 to 2010 and from April to June 2010, to April to June 2011 KH03 figures: replaced with 2008 to 2009 KH03 figure
-
Sheffield Teaching Hospitals NHS Foundation Trust (RHQ) from April to June 2010, to April to June 2011 KH03 figures: replaced with 2009 to 2010 KH03 data
-
The Princess Alexandra Hospital NHS Trust (RQW) April to June 2014, and October to December 2014 KH03 figures: replaced with April to June 2013, to October to December 2013 KH03 figures, respectively
- Ipswich Hospital NHS Trust (RGQ) January to March 2016 KH03 figure: replaced with January to March 2015 figures
-
West Suffolk NHS Foundation Trust (RGR) April to June 2016, to October to December 2016 and April to June 2017 KH03 figures: replaced with April to June 2015, to October to December 2015 KH03 figures
- Gloucestershire Hospitals NHS Foundation Trust (RTE) October to December 2016, to January to March 2017 KH03 figures: replaced with October to December 2015, to January to March 2016 KH03 figures
The KH03 data used for this report were published on 24 November 2022. This may include revisions of previously published KH03 data used in earlier reports.
Population data
National incidence rates are calculated using 2007 to 2020 mid-year resident population estimates which are based on the 2011 census for England (2021 and 2022 estimates are based on 2020 mid-year estimates).
Definitions
Bacteraemia hospital-onset (trust-apportioned) cases
This includes patients who meet all three of the criteria:
- in-patients, day-patients, emergency assessment patients or not known
- have had their specimen taken at an acute trust or not known
- specimen was taken on or after day 3 of the admission (admission date is considered day ‘one’)
Cases that do not meet these criteria are categorised as community-onset (not-trust apportioned).
CDI hospital-onset (trust-apportioned) cases
Include patients who meet all three of the criteria:
- in-patients, day-patients, emergency assessment patients or not known
- have had their specimen taken at an acute trust or not known
- specimen was taken on or after day 4 of the admission (admission date is considered day ‘one’)
Cases that do not meet these criteria are categorised as community-onset (not-trust apportioned).
Historically, reports published before September 2017 have used the term ‘trust- apportioned’ to describe cases meeting the above conditions for apportionment and ‘not trust-apportioned’ for those that do not. Moving forward, these terminologies have been updated to ‘hospital-onset’ and ‘community-onset’ respectively. Please note that this is simply a change in terminology and does not constitute a change in the methodology for apportionment.
Prior trust exposure
From April 2017, reporting trusts were asked to provide information on whether patients with CDI had been admitted to the reporting trust within the 3 months prior to the onset of the current case. This allows a greater granulation of the healthcare association of cases. This was extended to all other data collections in 2019.
Cases are split into one of 6 groups for CDI and 5 groups for the bacteraemias:
CDI prior trust exposure categories
- Hospital-onset healthcare-associated: date of onset is greater than 2 days after admission (where day of admission is day 1).
- Community-onset healthcare-associated: is not categorised HOHA and the patient was most recently discharged from the same reporting trust in the 28 days prior to the specimen date (where day 1 is the date of discharge).
- Community-onset indeterminate association: is not categorised HOHA and the patient was most recently discharged from the same reporting trust between 29 and 84 days prior to the specimen date (where day 1 is the date of discharge).
- Community-onset community-associated: is not categorised HOHA and the patient has not been discharged from the same reporting organisation in the 84 days prior to the specimen date (where day 1 is the date of discharge).
- Unknown: the reporting trust answered ‘Don’t know’ to the question regarding previous discharge in the 3 months prior to CDI case.
- No Information: the reporting trust did not provide any answer for questions on prior admission.
Bacteraemia prior trust exposure categories
In addition, in April 2020, the HCAI DCS has included questions relating to prior trust exposure to the same acute trust reporting Gram-negative bacteraemia cases. These additional mandatory items were developed to assist the UK governments ambition to reduce healthcare-associated Gram-negative BSI and CDI from a 2019 baseline to threshold levels. This supports the intention to reduce Gram-negative BSI by 25% by March 2022, and by 50% by March 2024.
Cases since April 2020 have also been categorised as:
- Hospital-onset healthcare-associated: date of onset is greater than 2 days after admission (where day of admission is day 1).
- Community-onset healthcare-associated: is not categorised HOHA and the patient was most recently discharged from the same reporting trust in the 28 days prior to the specimen date (where day 1 is the specimen date).
- Community-onset community-associated: is not categorised HOHA and the patient has not been discharged from the same reporting organisation in the 28 days prior to the specimen date (where day 1 is the specimen date).
- Unknown: the reporting trust answered ‘Don’t know’ to the question regarding previous discharge in the month prior to the current episode.
- No Information: the reporting trust did not provide any answer for questions on prior admission.
Total reported cases
This is the total count of infections for each organism as of the date of extraction. Please note that for C. difficile, this count excludes those from patients less than 2 years old.
Episode duration
The length of an infection episode is defined as 14 days (28 days for CDI) from the earliest case’s specimen date (day ‘one’).
Incidence rate calculations
MRSA, MSSA and E. coli, Klebsiella spp., P. aeruginosa bacteraemia, and CDI population incidence rate (episodes per 100,000)
This incidence rate is calculated using the number of episodes and the mid-year population for England:

That is: the number of episodes is multiplied by 100,000, then multiplied by the number of days in the year, then divided by the mid-year population for the same year for England, then divided by the number of days in the quarter.
MRSA, MSSA and E. coli, Klebsiella spp., P. aeruginosa and CDI hospital-onset incidence
This incidence rate is calculated using the number of episodes and the KH03 average bed-day activity (see bed-day data above) and is calculated as follows:

That is: the number of episodes is multiplied by 100,000, then divided by the average number of beds occupied overnight in a quarter, then divided by the number of days in the same quarter.
Graphs and percentage change calculation
Please note that percentage changes in rate have been calculated using raw rates figures while those presented in the tables and commentary have been rounded to one decimal place. Similarly, graphs included in this report were plotted using raw rates figures. The raw rates figures are included in the Quarterly Epidemiological Commentary’s accompanying data.
Quarters
In publications prior to March 2016, all references to quarterly data are based on calendar year definitions and not financial year definitions, that is:
- Quarter 1: January to March
- Quarter 2: April to June
- Quarter 3: July to September
- Quarter 4: October to December
However, for all subsequent publications, including this one, all references to quarterly data are based on financial year definitions and not calendar year definitions, that is:
- Quarter 1 2014 to 2015: April to June 2014
- Quarter 2 2014 to 2015: July to September 2014
- Quarter 3 2014 to 2015: October to December 2014
- Quarter 4 2014 to 2015: January to March 2015
References
- Sloot R, Nsonwu O, Chudasama D, Rooney G, Pearson C, Choi H, Mason E, Springer A, Gerver S, Brown C, Hope R. 2022, ‘Rising rates of hospital-onset Klebsiella spp. and Pseudomonas aeruginosa bacteraemia in NHS acute trusts in England: a review of national surveillance data, August 2020 to February 2021.’ Journal of Hospital Infection, 119, 175-181
Further information
This publication forms part of the range of National Statistics outputs routinely published by UKHSA which include monthly and annual reports on the mandatory surveillance of MRSA, MSSA and E. coli, Klebsiella spp. and P. aeruginosa bacteraemia and CDI.
Annual report output
Further epidemiological analyses by financial year can be found in UKHSA’s annual epidemiological commentary.
Monthly report outputs
The following reports are produced by UKHSA monthly.
MRSA bacteraemia – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated MRSA bacteraemia by organisation.
MSSA bacteraemia – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated MSSA bacteraemia by organisation.
E. coli bacteraemia – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated E. coli bacteraemia by organisation.
Klebsiella spp. bacteraemia – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated Klebsiella spp. bacteraemia by organisation.
P. aeruginosa bacteraemia – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated P. aeruginosa bacteraemia by organisation.
CDI – counts of all reported, hospital-onset cases, community-onset cases, healthcare associated and community associated CDI by organisation.
Enquiries and feedback
For any enquiries or feedback on this report, or to request copies of this report in PDF format, please contact mandatory.surveillance@ukhsa.gov.uk
