Alcohol and drug treatment in secure settings 2018 to 2019: report
Published 30 January 2020
1. Main findings
1.1 Adult treatment numbers and substance use
There were 53,193 adults in alcohol and drug treatment in prisons and secure settings between 1 April 2018 and 31 March 2019.
Around 65% (34,590) of these people also started treatment in the year. Of the people starting treatment, 50% said they had a problem with opiate use.
Of the adults starting treatment with opiate problems, 75% also had a problem with crack cocaine.
1.2 Adults leaving treatment
A total of 30,882 people left treatment in secure settings in 2018 to 2019.
Just over a quarter (27%) of those were discharged after completing their treatment free of dependence.
1.3 Young people’s treatment
There were 1,276 young people receiving treatment for drug and alcohol problems in secure settings in 2018 to 2019.
Cannabis was the most common problem substance for young people in secure settings (94%).
Of the 926 young people who left treatment in secure settings in 2018 to 2019, 29% completed their treatment successfully.
2. Adults in treatment: overview
2.1 Definitions
The National Drug Treatment Monitoring System (NDTMS) statistics report presents information on adults (aged 18 and over) who were receiving help in prisons and secure settings in England for problems with drugs and alcohol in the period 2018 to 2019.
Many people experience difficulties with and receive treatment for both substances. While they often share many similarities, they also have clear differences, so this report divides people in treatment into the 4 substance groups:
- opiate - people who are dependent on or have problems with opiates, mainly heroin
- non-opiate - people who have problems with non-opiate drugs only, such as cannabis, crack and ecstasy
- non-opiate and alcohol - people who have problems with both non-opiate drugs and alcohol
- alcohol only - people who have problems with alcohol but do not have problems with any other substances
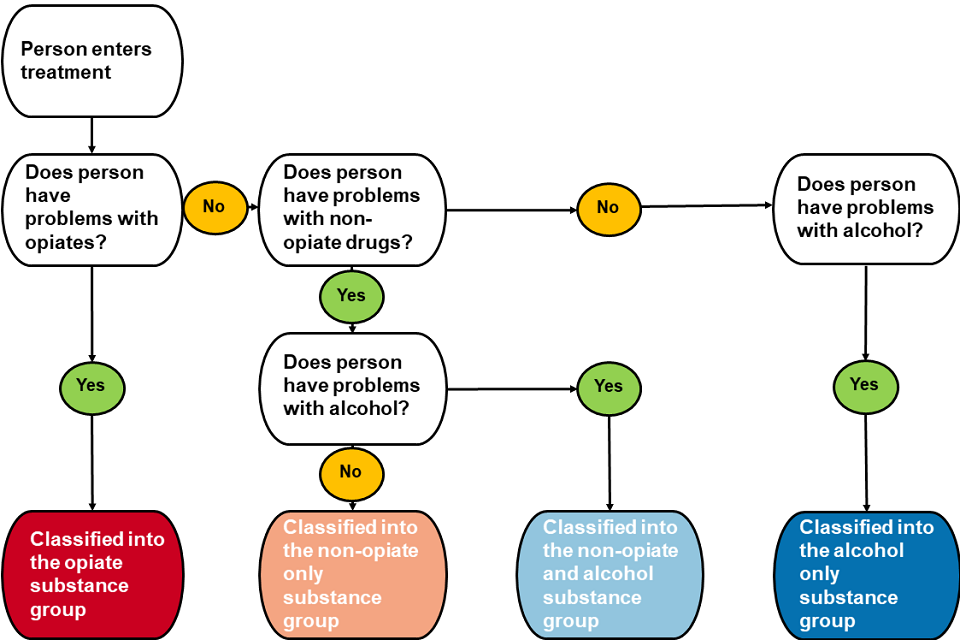
Flow diagram showing how people are classified into one of the 4 different susbstance groups when they are assessed by alcohol and drug treatment services.
2.2 Numbers in treatment
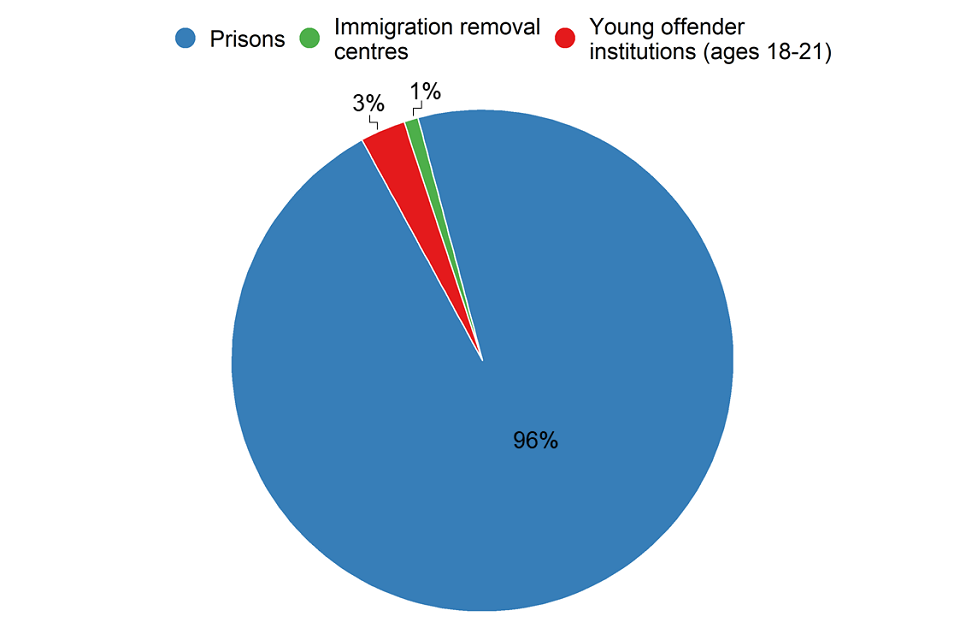
Pie chart showing the numbers of people in alcohol and drug treatment in different secure settings. The vast majority are in prison, with only small percentages in young offender institutions and immigration removal centres.
There were 53,193 adults receiving treatment for drug and alcohol problems in secure settings between April 2018 and March 2019. Most adults received structured treatment in prison (96%), either in a local, training, high security or open prison.
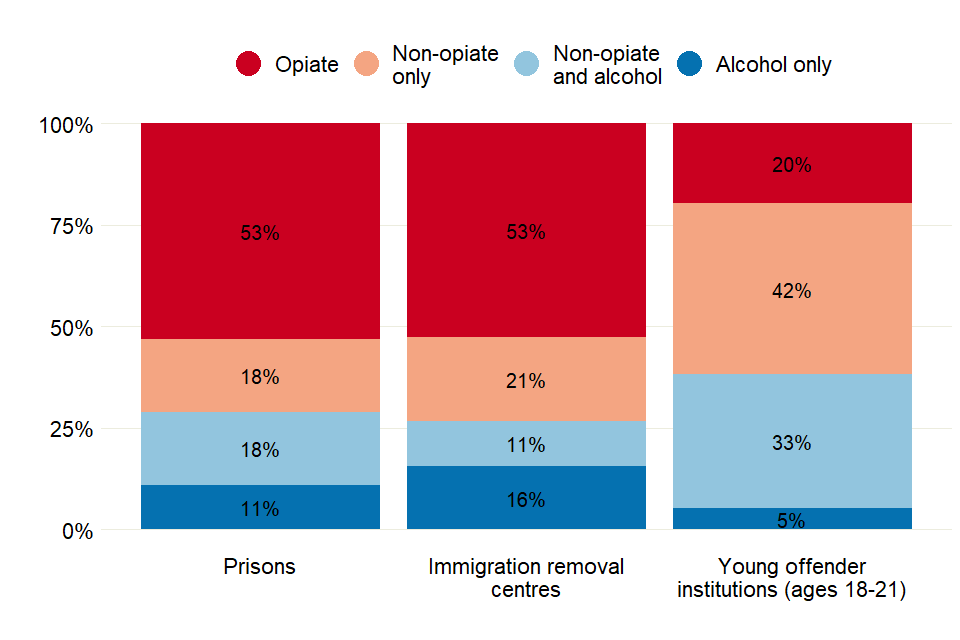
Bar chart showing the proportions of people in treatment for the 4 substance groups in prisons, young offender institutions and immigration removal centres.
A higher proportion of people were treated for alcohol only (16%) in immigration removal centres than in other areas of the secure estate. People in young offender institutions were mainly treated for non-opiate drug use (75%).
2.3 Sex
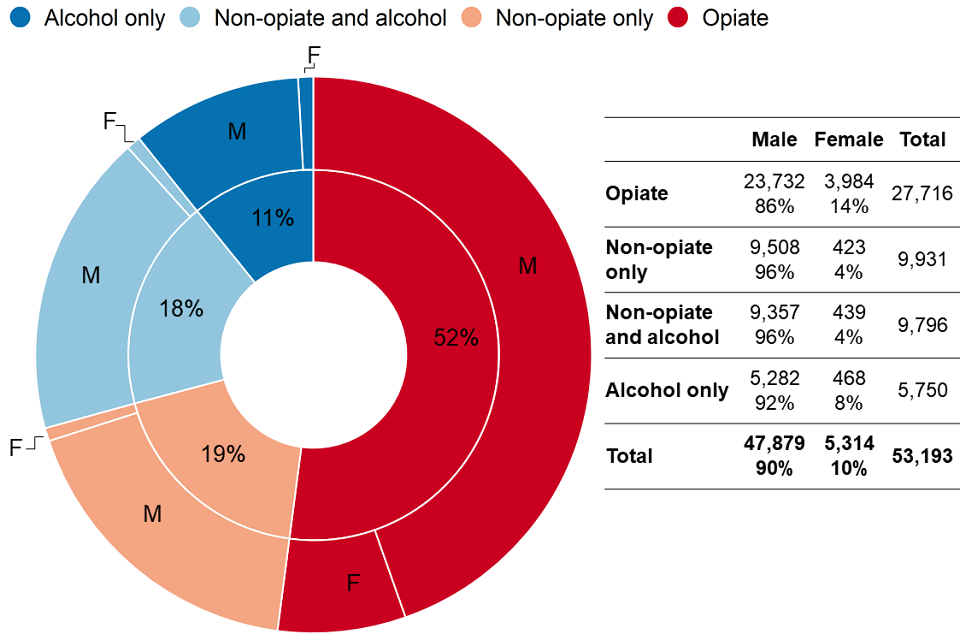
Pie chart showing a breakdown of adults in treatment for the 4 different substance groups. Over half are in treatment for opiates.
Ninety percent of the people in treatment in adult secure settings were men and 10% were women. This is double the proportion of women in the total prison population (which was 5% at the end of March 2019, as reported by Her Majesty’s Prison and Probation Service (HMPPS))
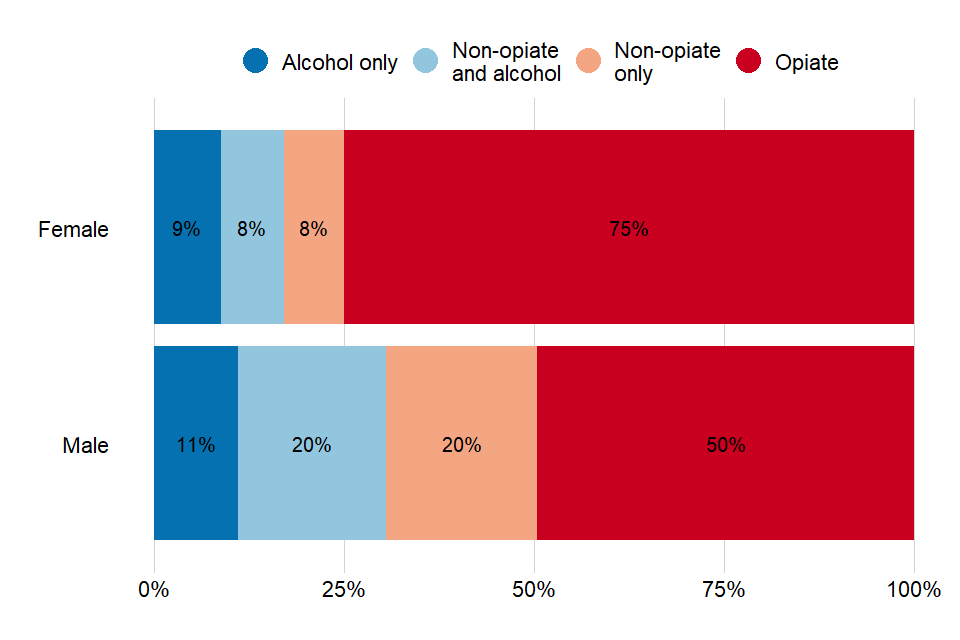
Bar chart showing the proportion of the 4 different substance groups for men and women.
The substance groups showed large differences by sex. Three-quarters of women (75%) in treatment had problems with opiate use compared with half (50%) of men.
Two percent of women in treatment reported that they were pregnant at the start of treatment.
2.4 Age
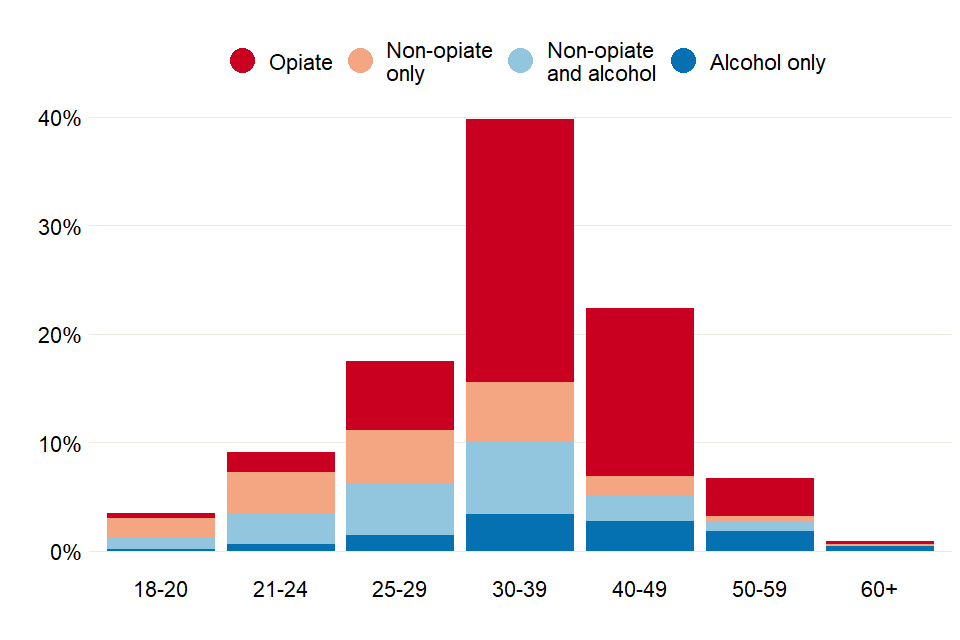
Bar chart showing the proportions of prisoners in treatment for the 4 different substance groups, across a range of age bands. The 30-30 age band has the most people in treatment.
The median age of people in treatment for alcohol alone was 38 years. It was 37 years for those in treatment for opiate use (the corresponding figures for community treatment were 46 years and 41 years).
People in the non-opiate and alcohol and non-opiate only groups had median ages of 30 years and 28 years respectively (the median ages were 34 years and 30 years in community treatment).
Adults in alcohol and drug treatment in prisons tended to be younger than those in community-based treatment. Although, like community treatment, adults being treated for only alcohol problems or for opiates tended to be older than those treated for other substances.
2.5 Substance use
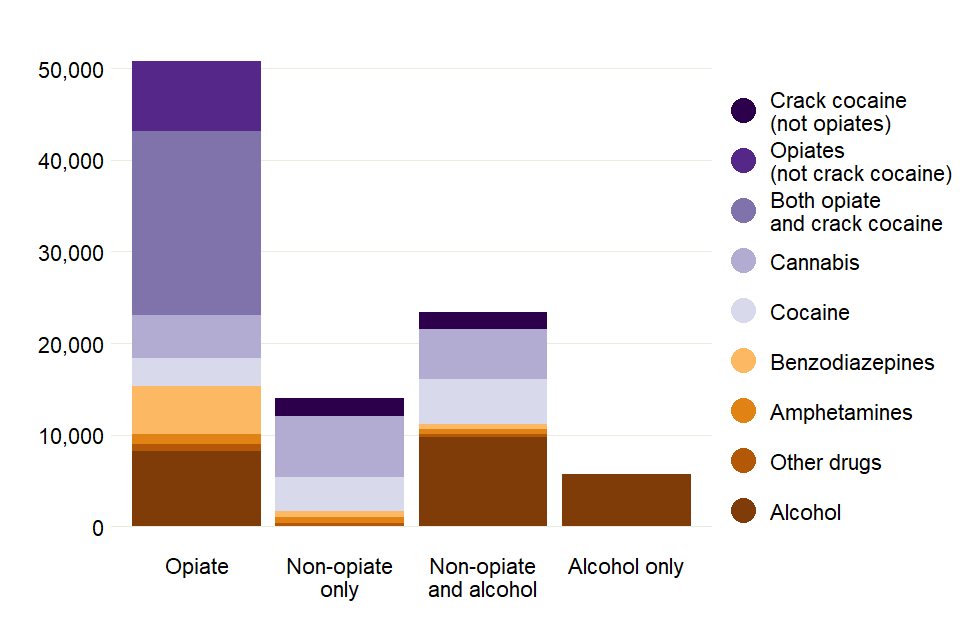
Bar chart showing numbers of people in treatment for the 4 substance groups and all substances they reported having a problem with.
Up to 3 substances can be recorded at the start of treatment, so a person may be counted more than once within the substance group in which they are reported in the chart above.
Of the people in treatment:
- 59% said they had a problem with opiate or crack use
- 48% said they had a problem with alcohol (11% of which were alcohol alone)
- 32% said they had a problem with cannabis
- 22% said they had a problem with powder cocaine
Of the people with opiate problems:
- 73% said they had a problem with crack cocaine
- 29% said they had a problem with alcohol
- 19% said they had a problem with benzodiazepines
New psychoactive substances (NPS) were a problem for 11% of people. This is the proportion of everyone in treatment in secure settings and is not a reflection of overall NPS use in prisons.
3. Adults starting treatment: pathways, age, substances
3.1 Pathways into treatment
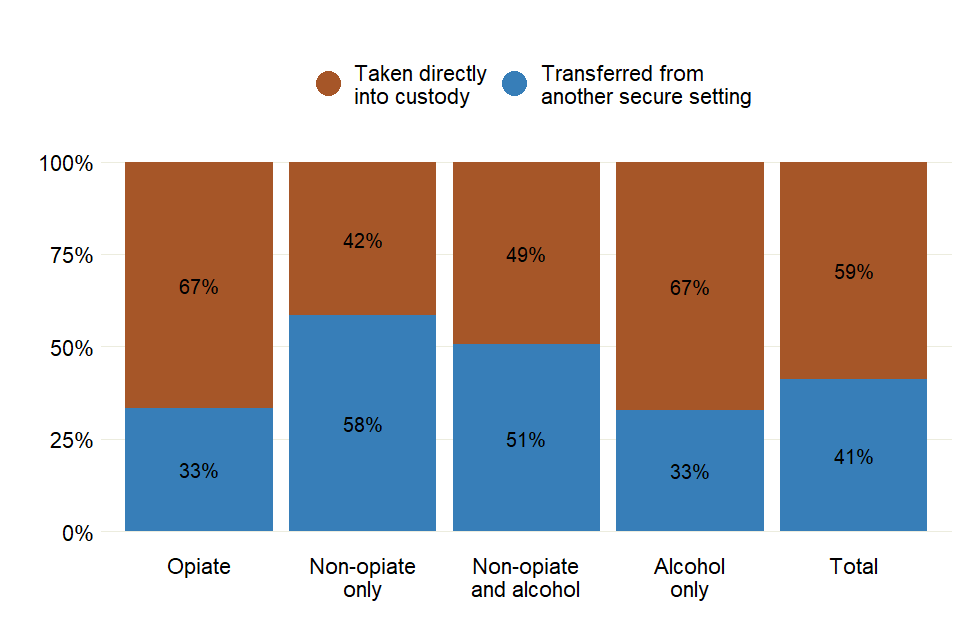
Bar chart showing the different ways people came into prison, either directly into custody or transferred from another prison, for the 4 substance groups.
Over half (59%) of the people starting treatment in an adult secure setting between 2018 and 2019 were taken directly into custody or detention from the community. Most of these adults (61%) started treatment immediately on arrival into custody. However, only 15% of adults transferred from another secure setting started treatment immediately on arrival.
Ninety percent of people starting treatment after beginning a new stay in custody, started the treatment within 3 weeks of arrival. However, 41% of people transferring from another secure setting took more than 3 weeks to start treatment.
3.2 Age and substances used
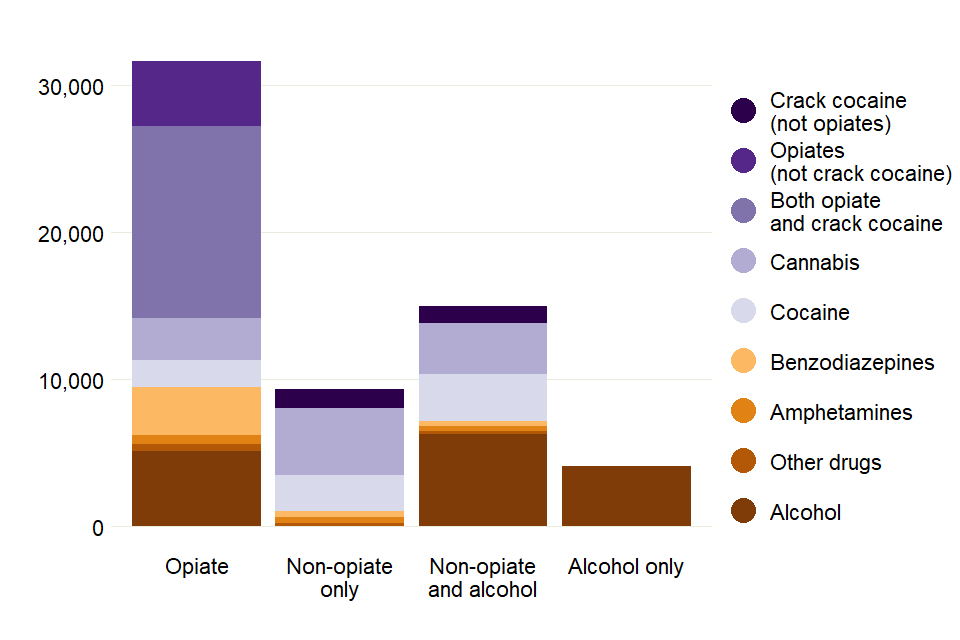
Bar chart with all the substances reported across the 4 substance groups, for people who started treatment in 2018 to 2019.
In 2018 to 2019, 34,590 people started treatment for drug and alcohol problems in a secure setting. This is where a person started a new treatment episode, which might also include returning to treatment.
Of the people starting treatment:
- 50% said they had a problem with opiate use
- 45% said they had a problem with alcohol
- 31% said they had a problem with cannabis
- 22% said they had a problem with cocaine
Of the people with opiate problems:
- 75% said they had a problem with crack cocaine
- 29% said they had a problem with alcohol
- 19% said they had a problem with benzodiazepines
Of the people with alcohol problems 26% said they only had a problem with alcohol.
Six in 10 (61%) non-opiate users reported having problems with cannabis (67% for non-opiate only users and 54% for non-opiate and alcohol users). Just over a third (37%) of the non-opiate-only group reported problems with cocaine powder at the start of treatment, compared to over half (51%) of the non-opiate and alcohol group.
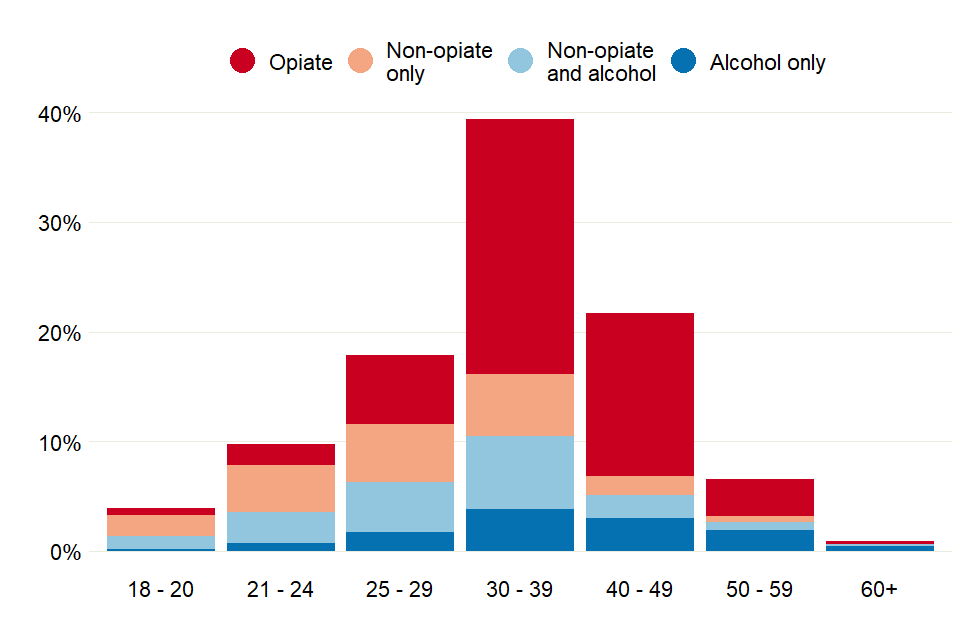
Bar chart showing the proportion of prisoners who started treatment in 2018 to 2019, across the 4 substance groups for a range of age groups
Younger adults (aged 18 to 20) were most likely to start treatment reporting problems with cannabis (76%), alcohol (37%), cocaine (28%) or opiates (14%).
Most people who started treatment (61%) were between the ages of 30 and 49 and said they had problems with opiates (62%). People who started treatment saying they had problems with only non-opiates were generally younger, with 84% aged under 40. Those that started treatment saying they had problems with only alcohol tended to be older, with 53% of people aged 60 or over.
4. Mental health
Over a third (35%) of people starting treatment in 2018 to 2019 were identified as having a mental health need. The highest proportion was seen in opiate users (39%), compared to 28% of non-opiate only users.
The mental health needs recorded in NDTMS should reflect the needs identified by prison healthcare staff or identified in the community before the person was in the secure setting.
5. Injecting drugs
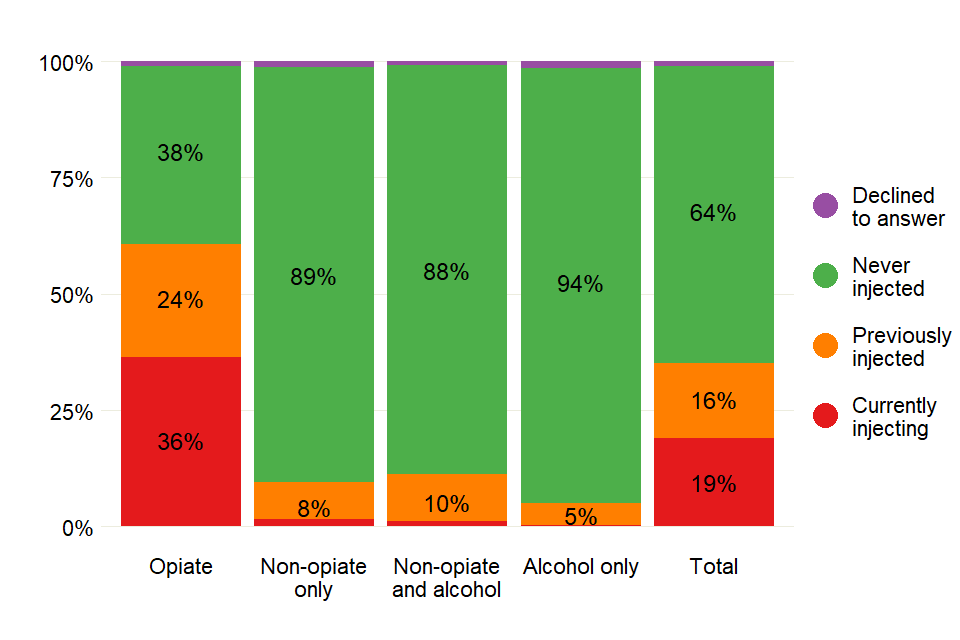
Bar chart showing the injecting status (whether they are injecting or not, or have in the past) of prisoners across the 4 substance groups.
Most people starting treatment in 2018 to 2019 had never injected (64%). Opiate users were most likely to be currently injecting (36%) compared to less than 2% for all other groups.
6. Parental status and safeguarding children
6.1 Parental status
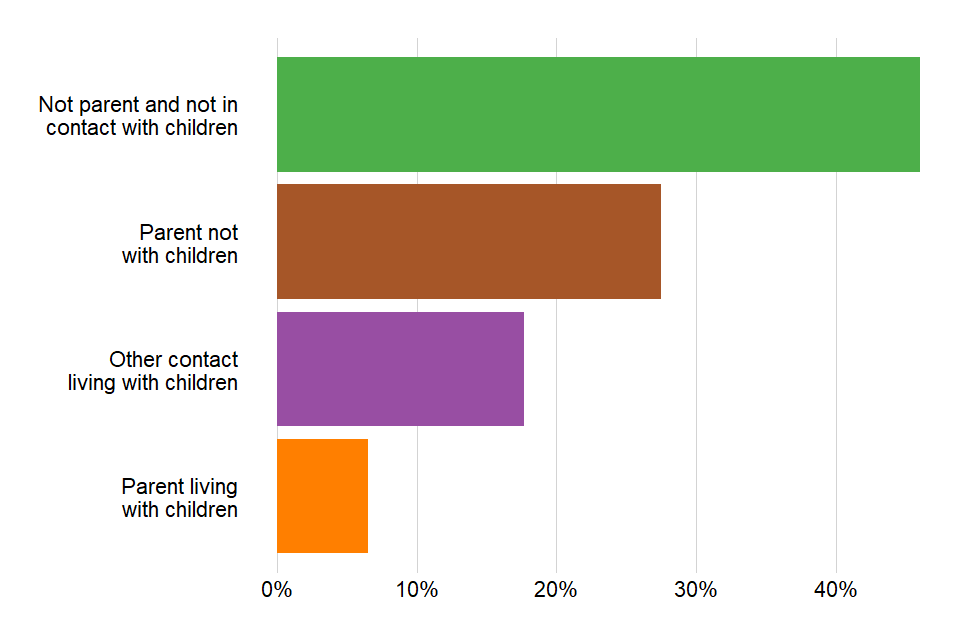
Bar chart showing the proportions of different parental statuses (parents or not, living with kids or not) for prisoners starting treatment in 2018 to 2019.
A quarter (25%) of people starting treatment in 2018 to 2019 were living with children, either their own or someone else’s, before coming into the secure setting. This is very similar to the proportion starting treatment in the community in the same period (21%).
There were a further 14,643 (28%) people who said they were parents but did not currently live with their children. Again, this was similar to those in treatment in the community (31%).
6.2 Safeguarding and early help
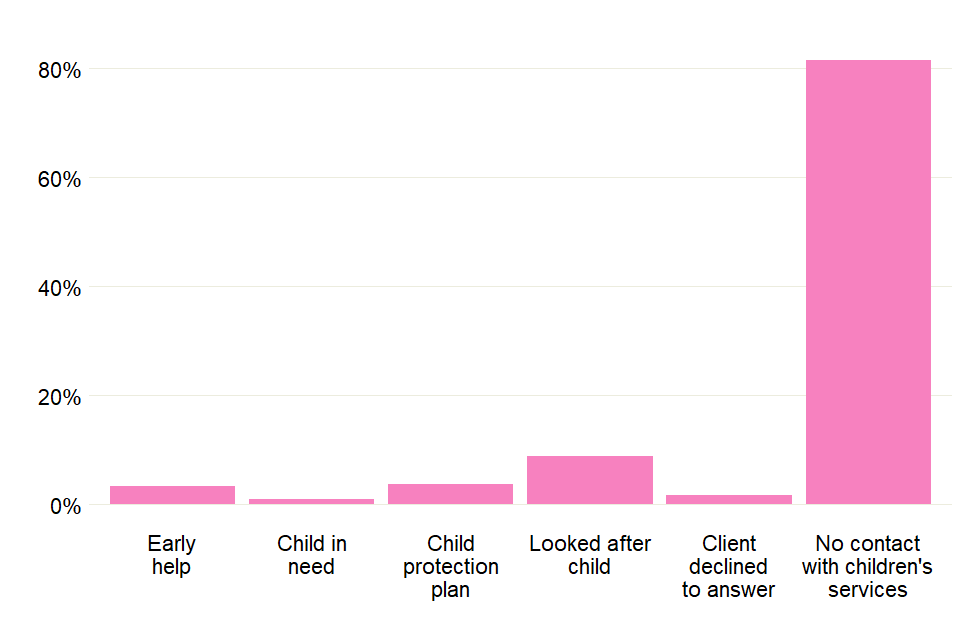
Bar chart showing the proportions of the children of prisoners starting treatment who were in contact with social care or were receiving different types of support.
Eighty-one percent of the children of people starting treatment had no contact with children’s services. Nine percent of people starting treatment had a looked-after child, though this figure rose to 12% in the opiate group.
7. Smoking
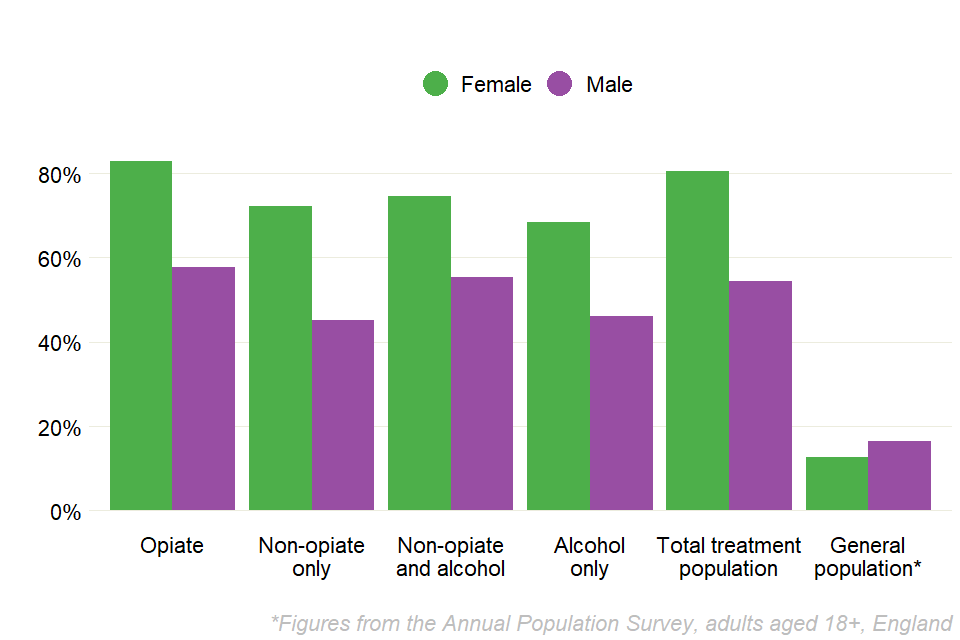
Bar chart showing the proportions of prisoners who were smoking at the start of treatment, by the 4 substance groups and sex.
Just over 7,500 people said they had smoked tobacco in the 28 days before entering prison and starting treatment. This is based on information collected at the start of treatment as part of Public Health England’s treatment outcomes profile (TOP).
Across all substance groups, women consistently reported smoking at higher levels than men. In all cases, the level of smoking was substantially higher than the smoking rate of the general population, which the latest Office for National Statistics report says is 16.4% for men and 12.6% for women.
8. Treatment types
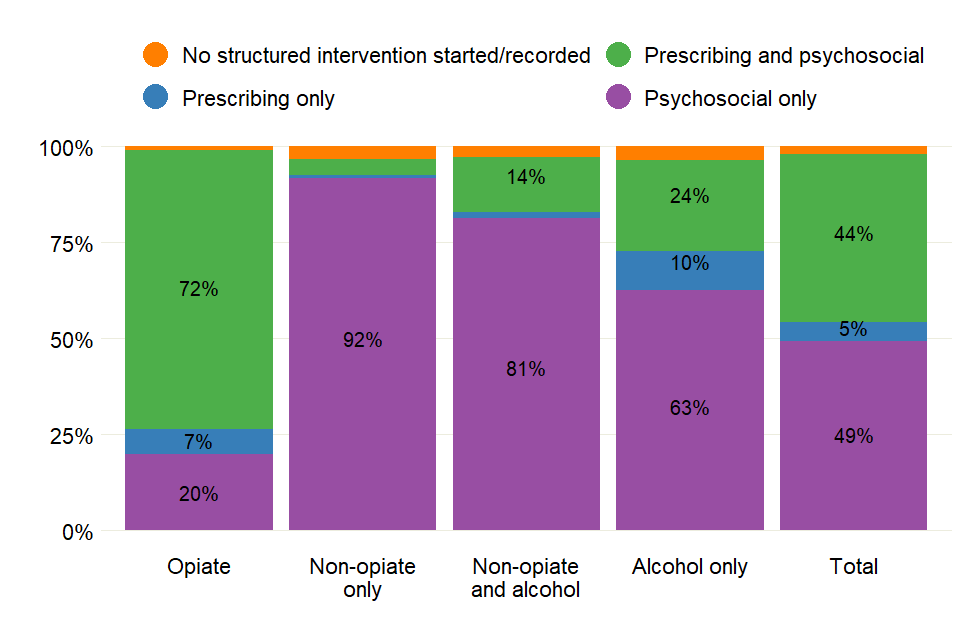
Bar chart showing the proportion of prisoners receiving different types of treatment, across the 4 substance groups.
Almost all adults in treatment in secure settings (93%) in 2018 to 2019 received psychosocial interventions. Five percent received prescribing interventions only, and 2% either did not start an intervention or an intervention was not recorded.
Almost half (49%) of adults in treatment received a prescribing intervention. There were 79% of the opiate group receiving these, 34% of the alcohol-only group and just 5% of the non-opiate group.
Prescribing interventions are generally provided alongside a psychosocial component to help support a person’s recovery, as recommended by the UK drug treatment clinical guidelines.
9. Treatment outcomes
9.1 Treatment exits and successful completion
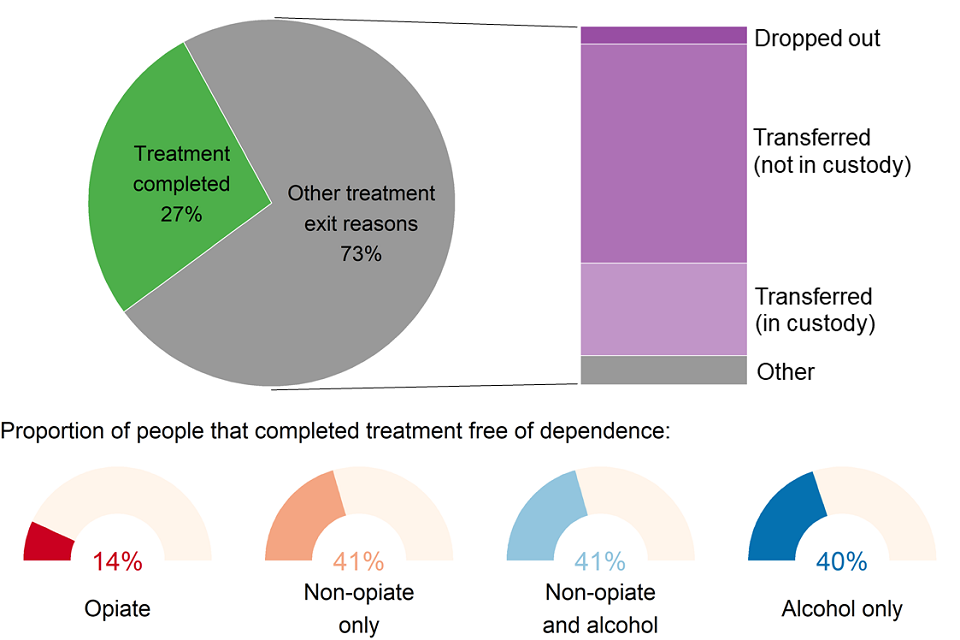
Chart showing the different reasons that prisoners left treatment.
A total of 30,882 people left treatment in secure settings in 2018 to 2019. Just over a quarter (27%) of those were discharged after completing their treatment free of dependence. Adults in treatment for opiate problems had the lowest rate of successful completion (14%) compared to the other substance groups where the rate was 40% or higher.
Nearly two-thirds (64%) of adults leaving treatment were transferred for further treatment either in the community (45%) or in another secure setting (19%).
Continuity of care between treatment services in prisons and the community is monitored by the Public Health Outcomes Framework (PHOF) indicator C20. The proportion of adults successfully starting community treatment within 3 weeks of release was 34% in 2018 to 2019.
The remaining 9% of adults left treatment without completing it, mainly having dropped out of treatment (3%) or discharged due to being released from court (4%).
9.2 Deaths in treatment
There were 54 people who died while they were in treatment in 2018 to 2019, which was 0.2% of all people in treatment. This was more than the previous year when 43 people died. People with opiate problems accounted for most of these deaths (61%), similar to the proportion in adult community treatment (65%).
Of those who died in treatment, 91% were male and 9% were female. The median age of adults who died was 38, with the median age ranging from 32 for the non-opiate-only group, to 43 for the non-opiate and alcohol group and the alcohol-only group.
The UK clinical guidelines for drug misuse and dependence highlight the importance of take-home naloxone for previously heroin-dependent prisoners when they leave prison. Of all the people who were treated for opiate problems, 17% were provided with take-home naloxone when they were released in 2018 to 2019, compared to 12% in the previous year.
10. Young people in treatment: overview
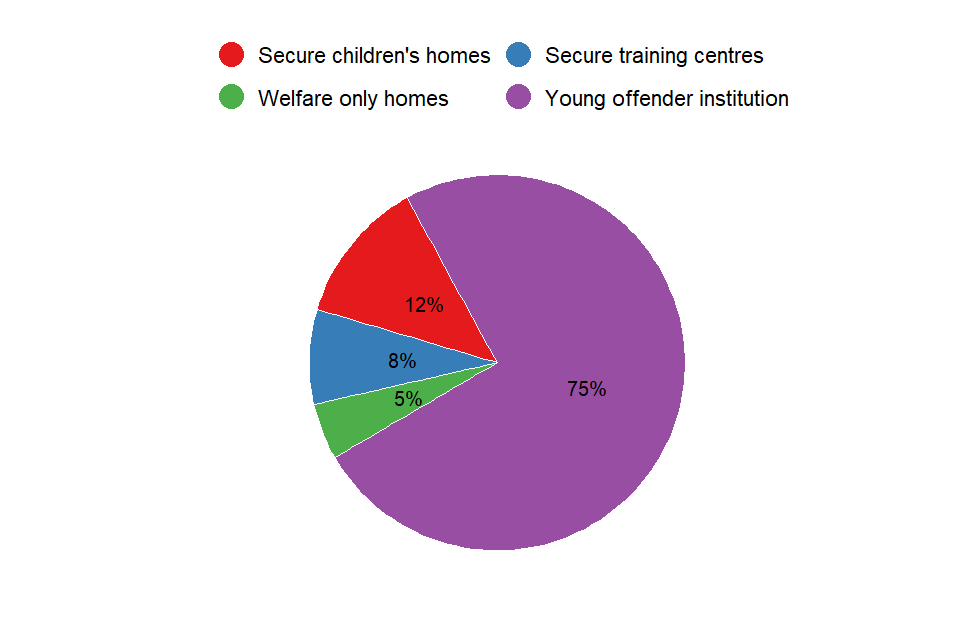
Pie chart showing the proportions of young people in treatment in different secure settings. Three quarters are in young offender institutions.
There were 1,276 young people receiving treatment for drug and alcohol problems in secure settings in 2018 to 2019. Most (75%) of these were in young offender institutions, with a further 12% in secure children’s homes, 8% in secure training centres and 5% in welfare-only homes.
10.1 Young people: age and sex
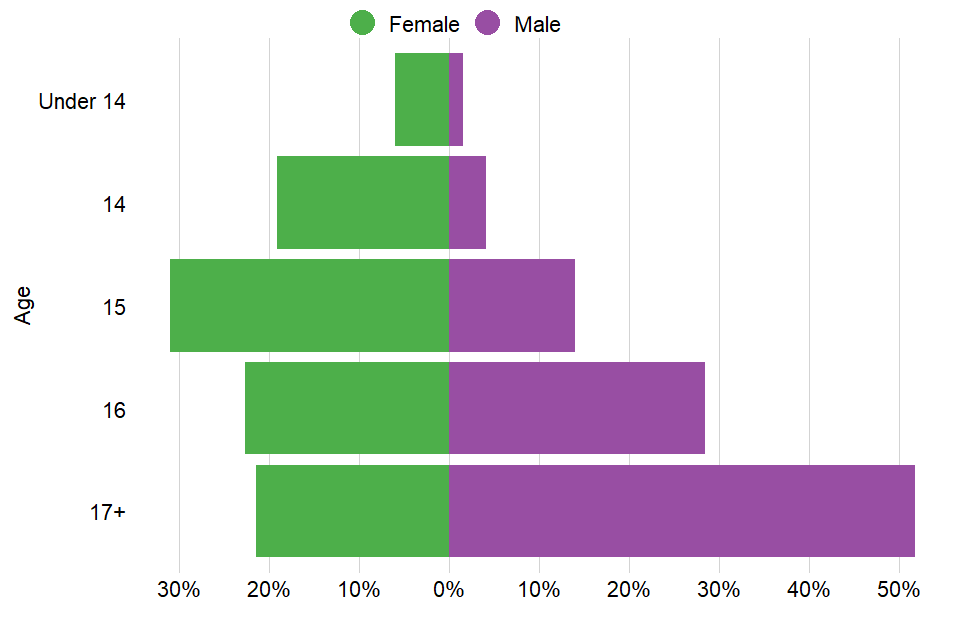
Chart showing the proportions of young people in treatment by age and sex.
Most (93%) of the young people in treatment in secure settings were male. HMPPS statistics show that 97% of the total youth custody population was male in March 2019 (excluding welfare-only places but including settings in Wales).
There were 84 girls in treatment. Boys tended to be older, with a median age of 17, compared to girls who had a median age of 15.
10.2 Young people: substance use
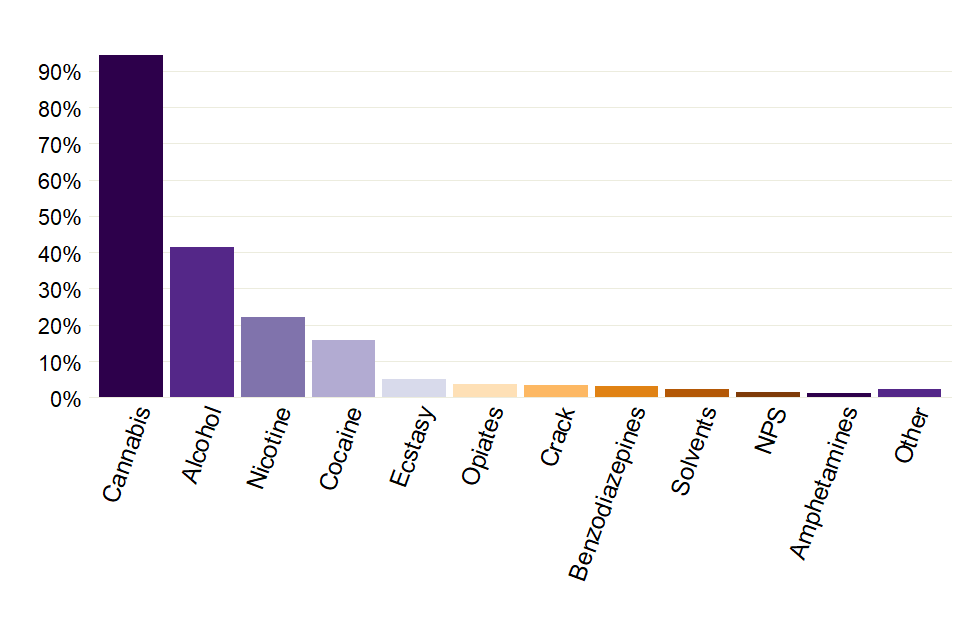
Bar chart showing the proportions of the different problem substances reported by young people in treatment.
Of the young people starting treatment in secure settings in 2018 to 2019:
- 94% said they had a problem with cannabis.
- 42% said they had a problem with alcohol
- 22% said they had a problem with nicotine
- 16% said they had a problem with cocaine powder
- 5% said they had a problem with ecstasy
- 4% said they had a problem with opiates
- 3% said they had a problem with crack cocaine
Young people in treatment for problems with opiates, cocaine powder or crack were older (median age of 17) than those reporting other substances (the median age for cannabis, alcohol and nicotine was 16).
10.3 Vulnerabilities of young people starting treatment

Bar chart showing the proportions of young people in treatment who had different vulnerabilities.
Young people often enter specialist substance misuse services with a range of problems or ‘vulnerabilities’ which are related to, or in addition to, their substance use. These include using multiple substances (poly-substance use) and being a parent or pregnant.
The most common vulnerability by far was poly-substance use (61%). Six percent reported high-risk alcohol use and 5% said they used opiates or crack. Three percent of young people reported being a parent or pregnant.
Nearly half (49%) reported only one vulnerability, while 12% reported 2 vulnerabilities, and only 1% said they had 3 or more vulnerabilities.
10.4 Young people: treatment type
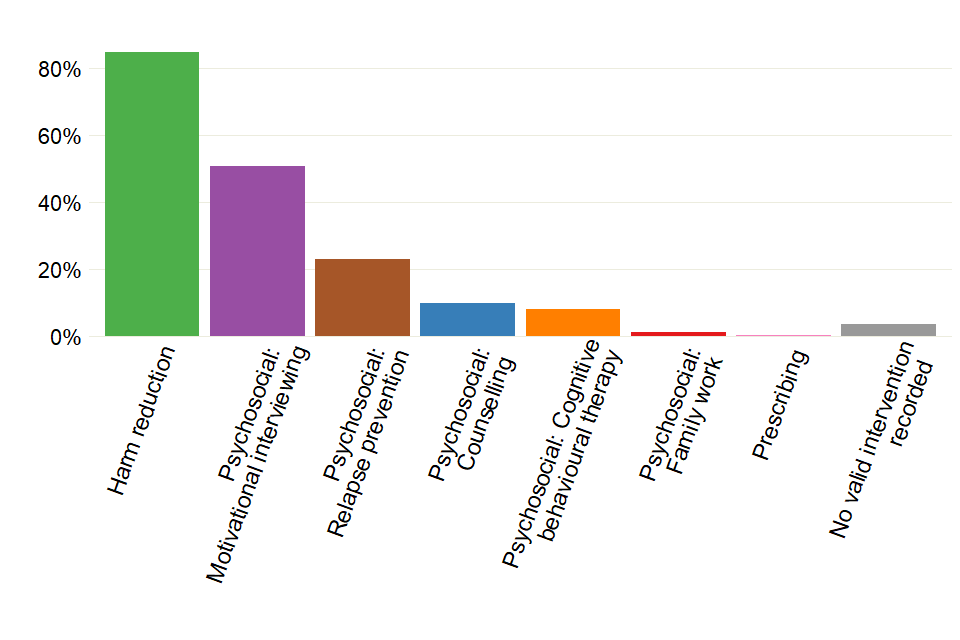
Bar chart showing the proportions of different treatment interventions received by young people in secure settings.
Most young people in treatment (85%) received a harm-reduction intervention. These include support to manage risky behaviour associated with substance misuse, such as overdose or accidental injury.
Just over half (51%) received motivational interviewing and just under a quarter (23%) received relapse prevention. The proportion receiving cognitive behavioural therapy was 8%, and only 1% of young people received a pharmacological intervention (this involves medication prescribed by a clinician).
10.5 Young people: treatment exits
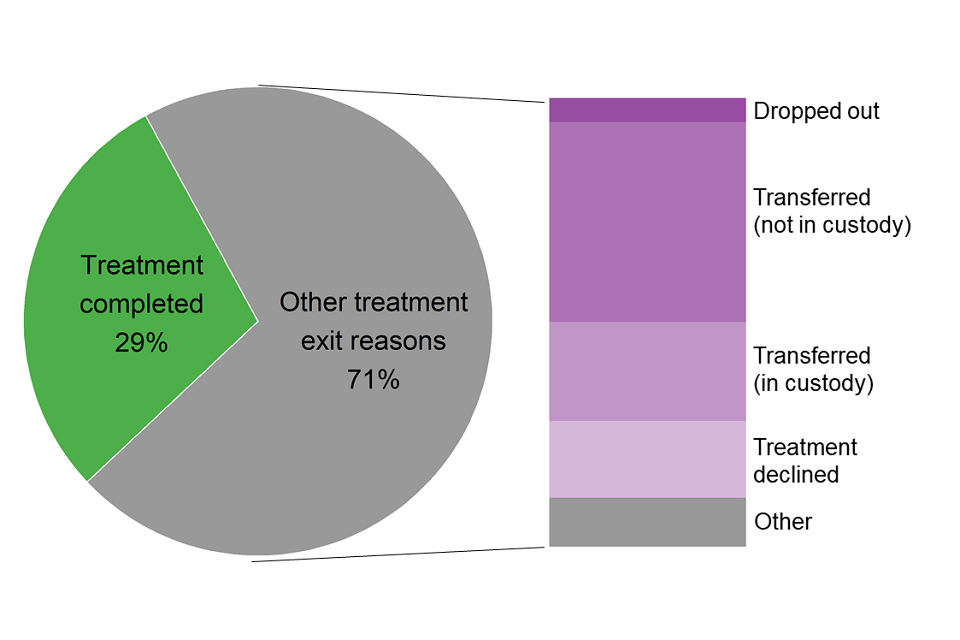
Chart showing proportions and different reasons for young people leaving treatment
There were 926 young people who left treatment in secure settings in 2018 to 2019. Of these, 29% completed their treatment successfully. Nearly a third (32%) were released from custody and referred for further treatment in the community, and 16% were transferred to another secure setting with the intention that their treatment would continue. Twelve percent of young people declined treatment and 8% left treatment due to being released from court.
11. Trends over time
Due to data compliance issues in the last 2 years, trends are displayed as proportions and not numerical volume in the adult sections, except the deaths in treatment section.
11.1 Trends: adults in treatment
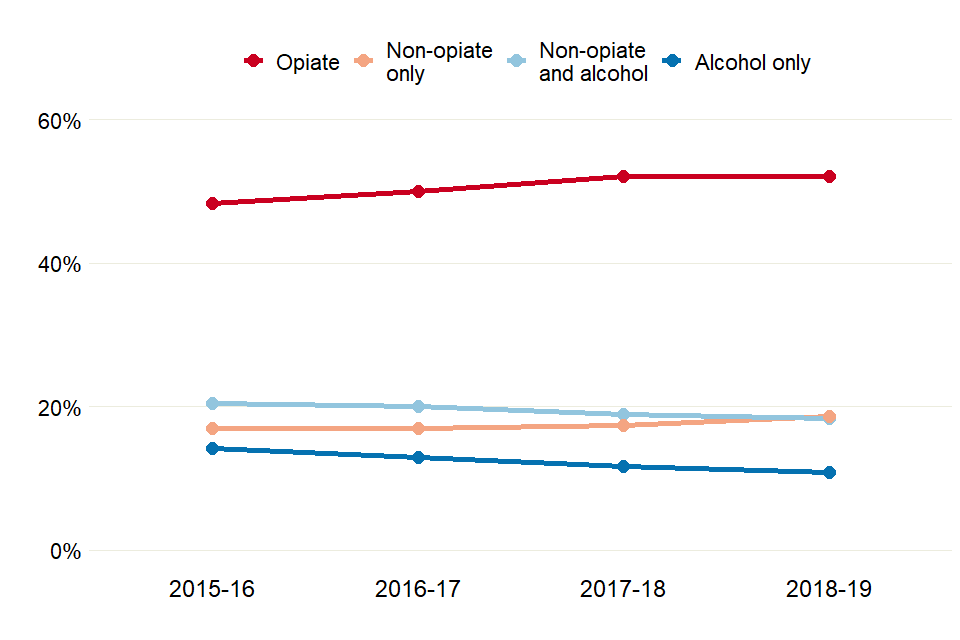
Line chart showing how the proportions of prisoners in treatment for each of the 4 substance groups have changed over 4 years.
There was a 4% fall in adults in treatment in 2018 to 2019 compared with the previous year, continuing a year-on-year decrease that is now 12% lower than the first year these statistics were reported (2015 to 2016). Most of this decrease was in the non-opiate and alcohol group (6%) and alcohol-only (11%) group.
The HMPPS offender equalities annual report shows that the overall prison population was 1% lower in March 2019 than in March 2018.
11.2 Trends: adults starting treatment

Line chart showing how the proportions of prisoners in starting treatment that year have changed over 4 years, for each of the 4 substance groups.
The number of adults starting treatment in secure settings in 2018 to 2019 was 3% lower than the previous year and 14% lower than the first year of reporting. The decrease was largest in the alcohol-only group and the opiate group (8% and 5% decreases respectively), though there was an increase in the non-opiate group (7%).
11.3 Trends: substance use by adults starting treatment
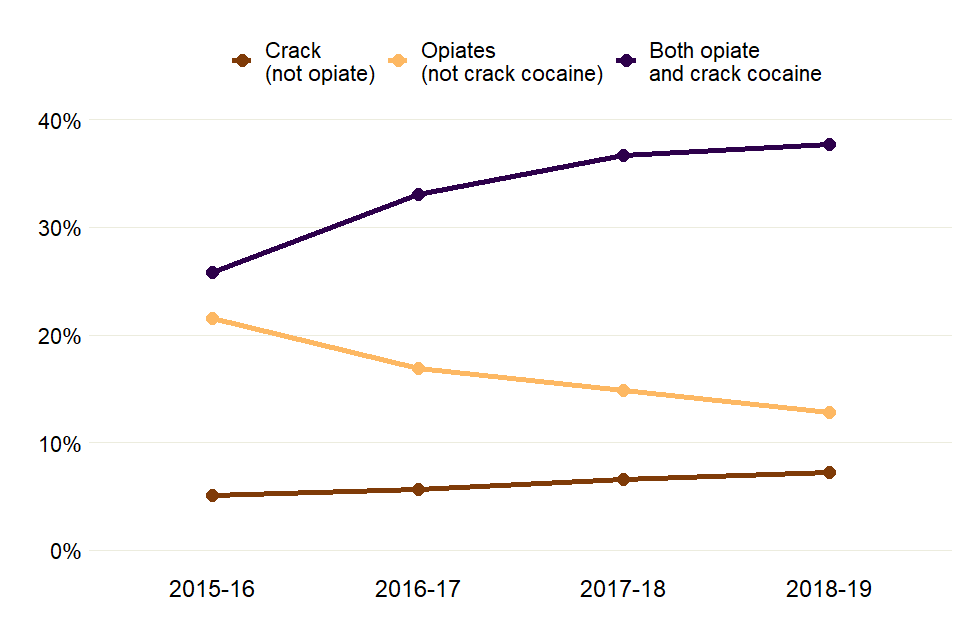
Line chart showing how the proportions of adults starting treatment with opiate or crack problems have changed over 4 years.
Thirty eight percent of people starting treatment in 2018 to 2019 reported problems with crack and opiate use. This has increased from 26% in 2015 to 2016. However, the proportion of people starting treatment for opiate problems without crack use has fallen year-on-year (from 22% in 2015 to 2016, to 13% in 2018 to 2019).
The proportion of people starting treatment for crack problems without opiates has gone up each year these statistics have been published (from 5% in 2015 to 2016 to 7% in 2018 to 2019).

Line chart showing how the proportions of adults starting treatment for drug problems that are not opiates or crack have changed over 4 years.
The proportion of people starting treatment for problems with alcohol has fallen year-on-year (a 22% decrease from 2015 to 2016).
Benzodiazepines and amphetamines have also seen large decreases since these statistics were first reported (decreases of 32% and 54% respectively).
The number of people reporting problems with other drugs has risen steadily since 2016 to 2017, from 1.6% to 2.4% this year. Half of these (50%) were from people who reported problems with pregabalin use.
The proportion of people in treatment for NPS has continued to rise. Eleven percent of adults in treatment said they had a problem with this in 2018 to 2019 compared to 6% in 2015 to 2016.
11.4 Trends: adults leaving treatment
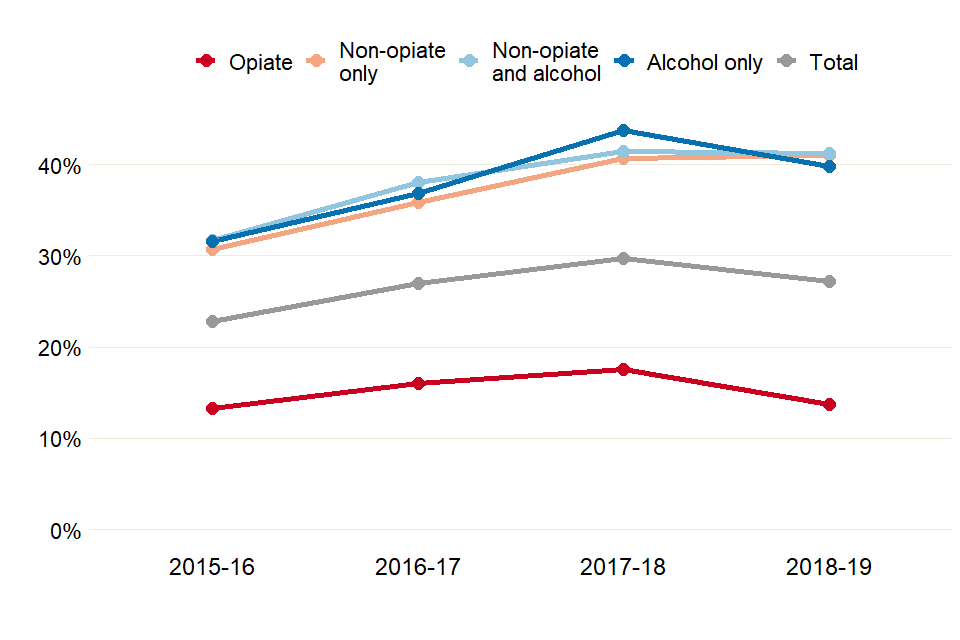
Line chart showing changes to the proportions of adults completing treatment for the 4 substance groups, over 4 years.
The proportion of adults leaving treatment after successfully completing their treatment free of dependence decreased to 27% in 2018 to 2019 from 30% the previous year.
Continuity of care between treatment services in prisons and the community is monitored by the PHOF indicator C20. The proportion of adults successfully starting community treatment within 3 weeks of release increased to 34% in 2018 to 2019 (from 32% in 2017 to 2018).
The number of people starting community-based treatment after release from prison increased for all regions except for London and the South West. The biggest increase was in the East Midlands, where 9% more people engaged with local treatment services than the previous year.
11.5 Trends: deaths in treatment
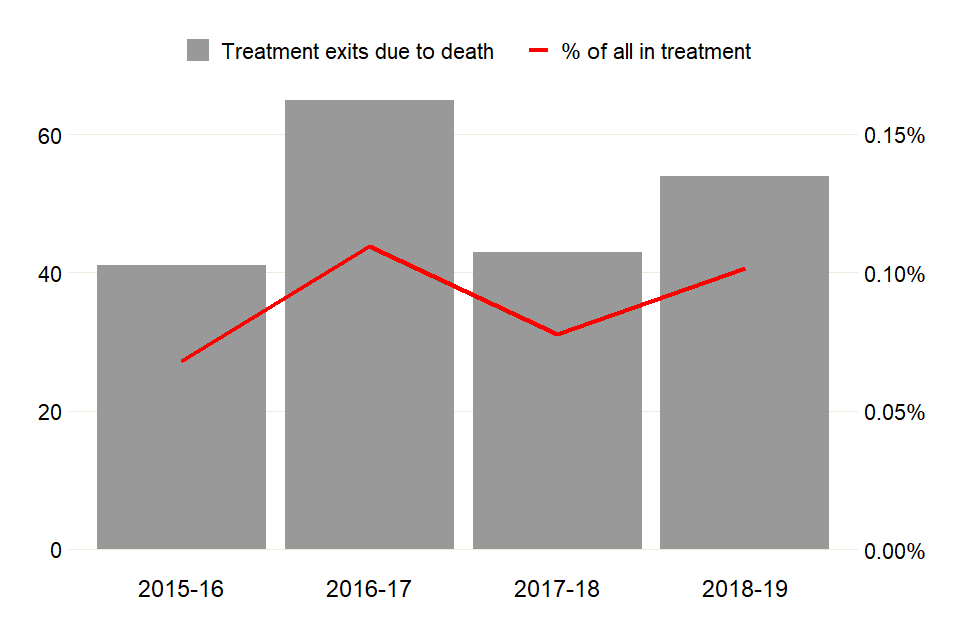
Bar and line chart showing how the numbers of people who died while in treatment has changed over 4 years.
The number of adults who died in 2018 to 2019 while they were in contact with treatment services increased 26% from the previous year (from 43 to 54), with increases in all substance groups.
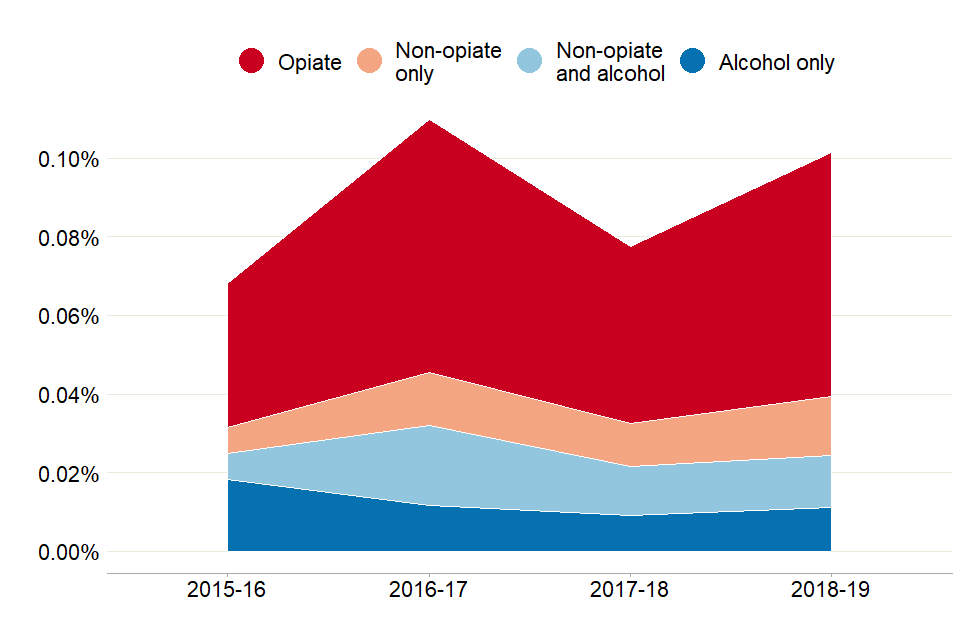
Chart showing how the numbers of people who died while in treatment has changed over 4 years, by substance group
People with opiate problems continue to be the most at risk, with 61% of deaths in this group. The other substance groups did not make up more than 15% of the total deaths in 2018 to 2019.
11.6 Trends: young people in treatment

Line chart showing the decrease in numbers of young people in treatment over 4 years.
The number of young people in treatment in secure settings in 2018 to 2019 fell by 6% compared to the previous year. This is similar to the 8% decrease in the youth custody population (which includes 18 year olds) for England and Wales between 2017 to 2018 and 2018 to 2019 reported by HMPPS.
11.7 Trends: substance use by young people starting treatment
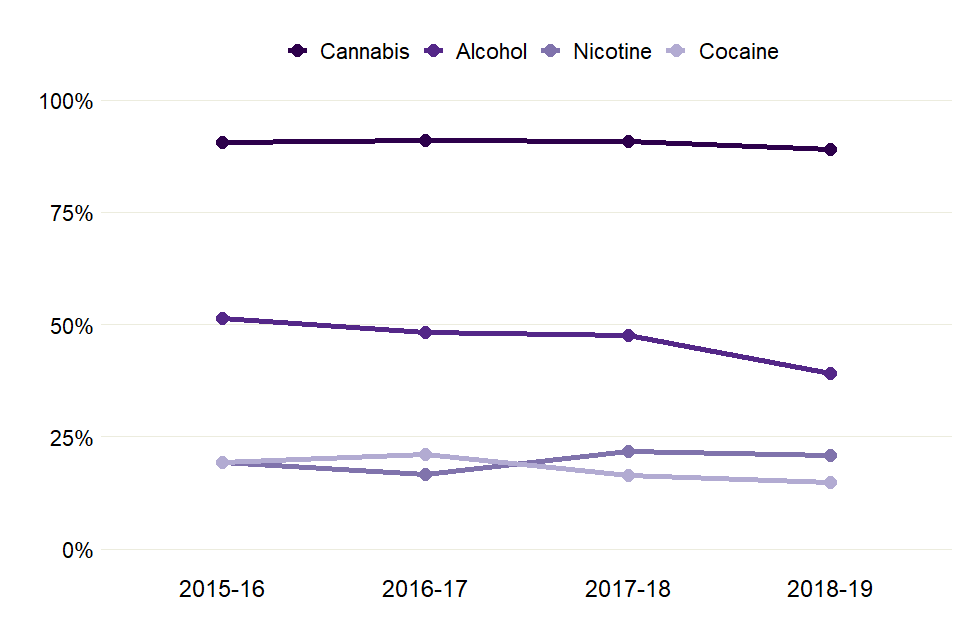
Line chart showing changes in proportions of the most problematic substances that young people were treated for, over 4 years.
Cannabis has always been the most common problem substance for young people in secure settings since these statistics were first published (94% had a cannabis problem in 2018 to 2019). The proportion has remained at similar levels across the 4 years these statistics have been reported.
The proportion of young people reporting problems with nicotine (22%) and cocaine (16%) has also remained similar to previous years.
Fewer young people in treatment said they had problems with alcohol use in 2018 to 2019 (42%) than in 2015 to 2016 (51%).
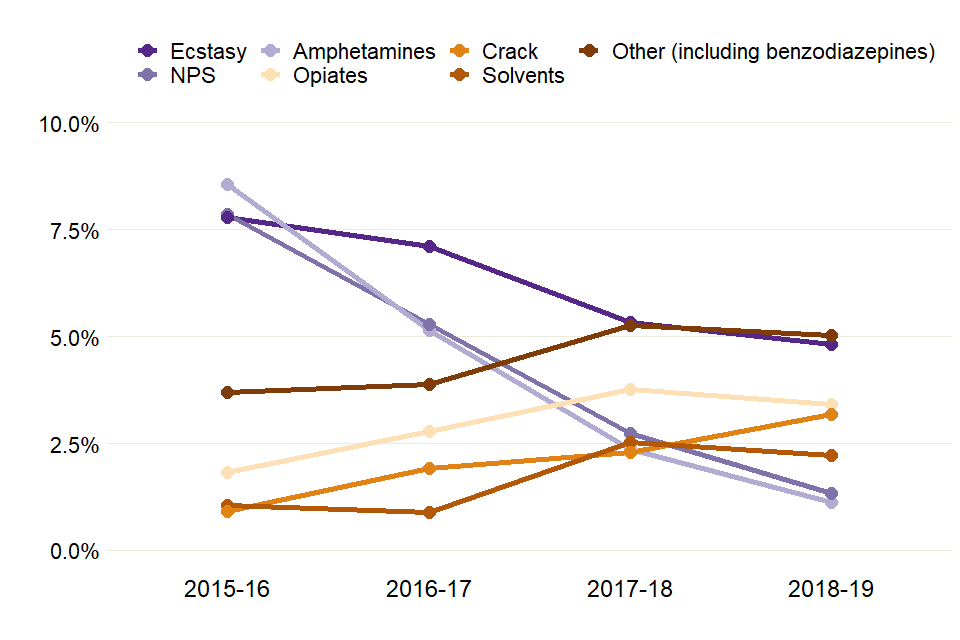
Line chart showing changes in proportions of young people being treated for other substances over 4 years
The proportion of young people reporting problems with opiates (4%) and ecstasy (5%) has remained similar to previous years, while the proportion saying they have problems with crack use has increased to 3% from 1% in 2015 to 2016. The proportion of young people reporting problems with NPS use has fallen to 1% from 8% in 2015 to 2016.
11.8 Trends: young people’s treatment exits
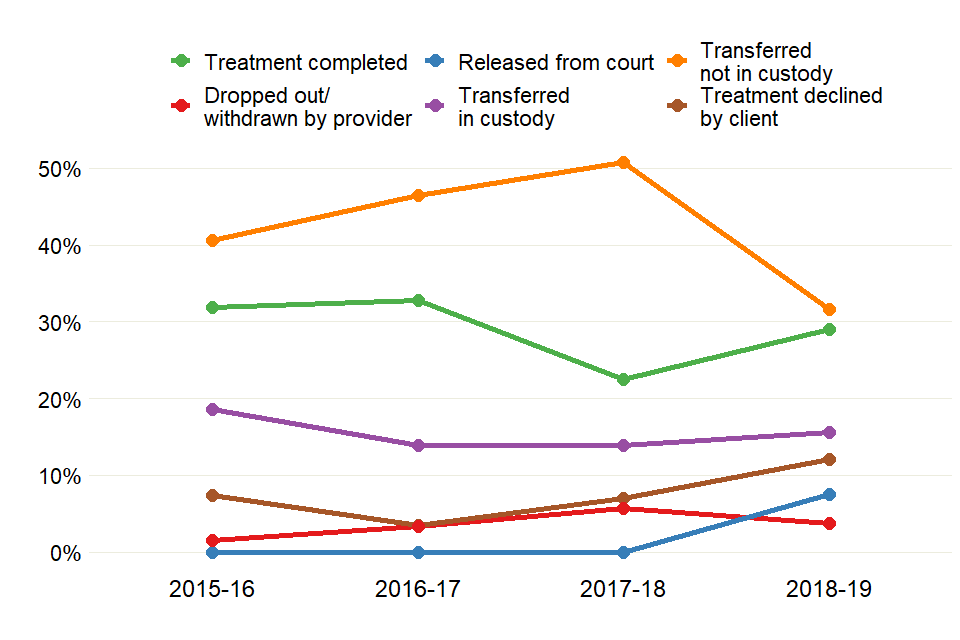
Line chart showing changes in proportions of young people leaving treatment for different reasons, over 4 years.
More young people completed substance misuse treatment in secure settings in 2018 to 2019 than in the previous year, increasing from 23% to 29%. However, this is still lower than the proportion completing in 2016 to 2017 (33%).
There was a fall in young people transferred to treatment services in the community on their release, from 51% (462) in 2017 to 2018 to 32% (293) in 2018 to 2019. There was also a fall in the number of young people dropping out of treatment across these 2 years, from 6% to 4%.
These decreases may be explained in part by the NDTMS data set introducing a new discharge reason from April 2018, to include the young people who were released from court and discharged before a transfer to community services could be arranged.
12. Background and policy context
12.1 Background
This report presents statistics on the availability and effectiveness of alcohol and drug treatment in prisons and secure settings in England, and the profile of people accessing this treatment.
The statistics in this publication come from analysis of the NDTMS which collects data from services providing structured substance misuse interventions to adults and young people in about 140 prisons and secure settings across England, including adult settings (prisons and immigration removal centres) and the children and young people’s secure estate.
The data collected includes information on the demographics and personal circumstances of people receiving treatment, as well as details of the interventions delivered and their outcomes.
You can find more details on the methodology used in the report in the NDTMS annual statistics quality and methodology information paper.
12.2 Policy context
Alcohol and drug treatment services in prisons and secure settings for adults and young people are commissioned by NHS England.
NHS England commissions specialist treatment services in secure settings which are equivalent to community-based treatment and informed by evidence-based clinical guidance.
Treatment includes interventions to reduce harm and to help people recover from alcohol and drug dependence. NHS England’s latest service specification describes how substance misuse services in prisons and secure settings should be provided.
The Royal College of Paediatrics and Child Health has published healthcare standards for children and young people in secure settings
Continuity of care for offenders leaving prison who still need treatment is a priority for NHS England, HMPPS Public Health England, the Department of Health and Social Care and the Ministry of Justice as set out in their National Partnership Agreement. There is also a partnership agreement for children and young people which includes continuity of care as one of the shared objectives.
The Public Health Outcomes Framework supports this priority by monitoring the engagement rates of adults who leave prison and continue their substance misuse treatment in the community.
Under the Children Act 1989, local authorities can place children in secure children’s homes and welfare-only homes. In these circumstances, children and young people are held there because of concerns about their welfare, rather than because they have offended.
