National quarterly report of tuberculosis in England: Quarter 3, 2022 provisional data
Updated 30 January 2025
Applies to England
This report presents quarterly data on tuberculosis (TB) case notifications in England. Notifications include patients with culture confirmed TB or if a patient has started treatment for TB based on the clinical presentation. It is mandatory to notify cases of TB in the UK within 3 working days of making or suspecting a diagnosis of TB. You can find more details about notification of TB online.
Detailed results for data up to the end of 2021 will be published in the annual report ‘Tuberculosis in England: 2021 report’ in 2022. The most recent annual report with data up to the end of 2020 is available on the Tuberculosis in England webpage.
This report aims to provide timely and up-to-date figures of important epidemiological indicators to inform ongoing TB control efforts in England.
Please note: data for 2022 is provisional and subject to validation and should be interpreted with caution. The data used for this report was extracted on 4 October 2022.
Overall numbers and geographical distribution
In the third quarter of 2022 (Q3 2022, 1 July to 30 September), 1,084 people were notified with TB in England. This is slightly lower than quarter 3 in the previous year (Q3 2021: 1,154). The number of notifications per quarter for England are shown in Figure 1 and by UKHSA centres in Figure 2a and 2b. Exact numbers per quarter by UKHSA centre and in total are shown in Table 1.
Figure 1. Number of TB notifications in England, Q1 2020 to Q3 2022
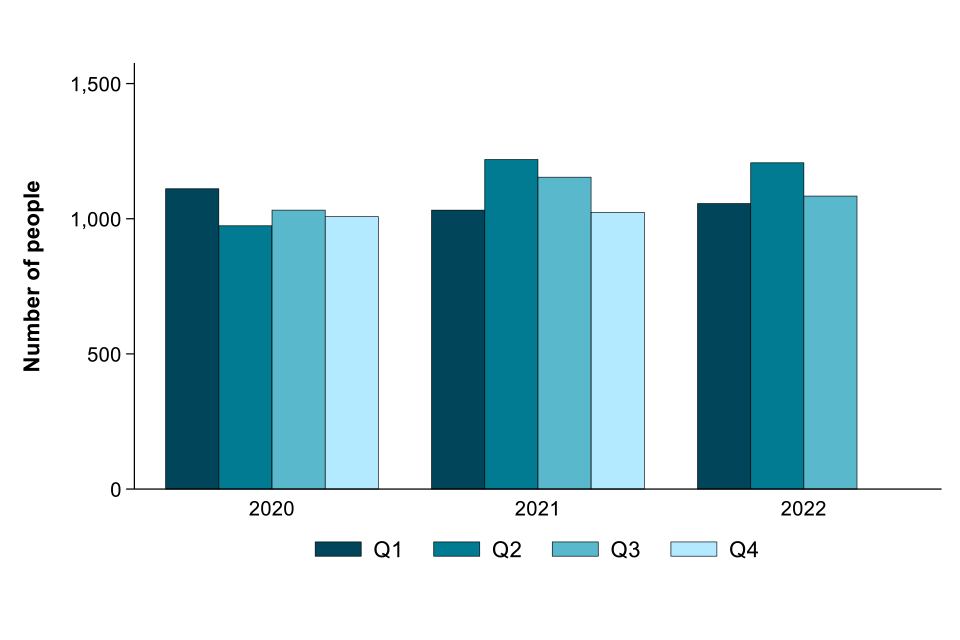
Please note: due to the seasonality of TB notifications the most recent quarter is being compared to the same quarter in the previous year rather than to the previous quarter.
In Q3 2022, the number of people notified with TB:
- increased in the South West (+20.0%) compared to Q3 2021
- remained similar in the East of England, North East, North West, South East and Yorkshire and the Humber compared to Q3 2021
- decreased in the East Midlands (-10.1%), London (-8.1%) and the West Midlands (-31.1%) compared to Q3 2021
Figure 2a. Number of TB notifications in London, England, Q1 2020 to Q3 2022
(Note: the axes on the London figure are different to that of other regions due to the higher number of TB notifications in London.)
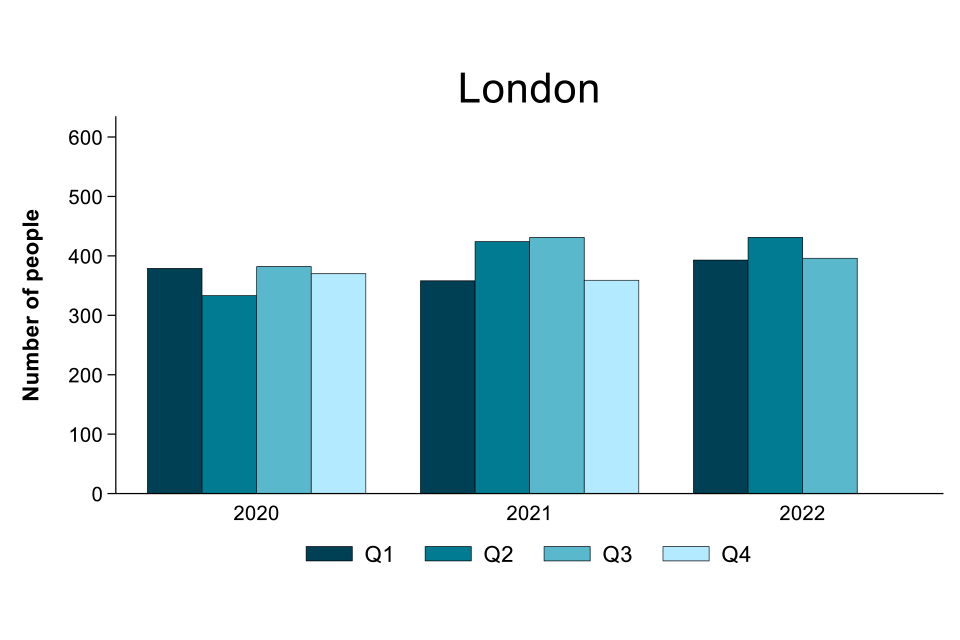
Figure 2b. Number of TB notifications by UKHSA centre, England, Q1 2020 to Q3 2022
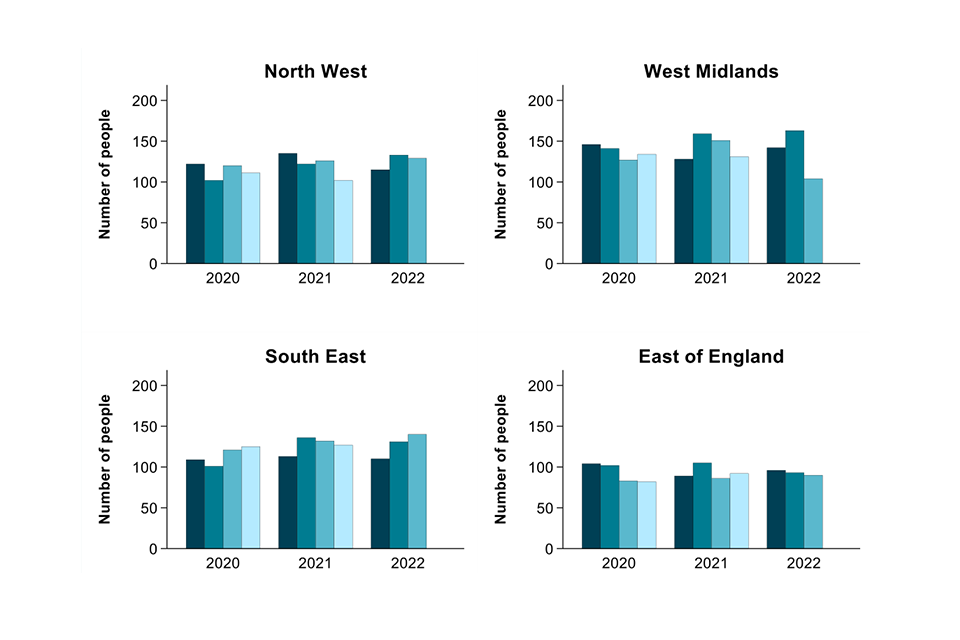
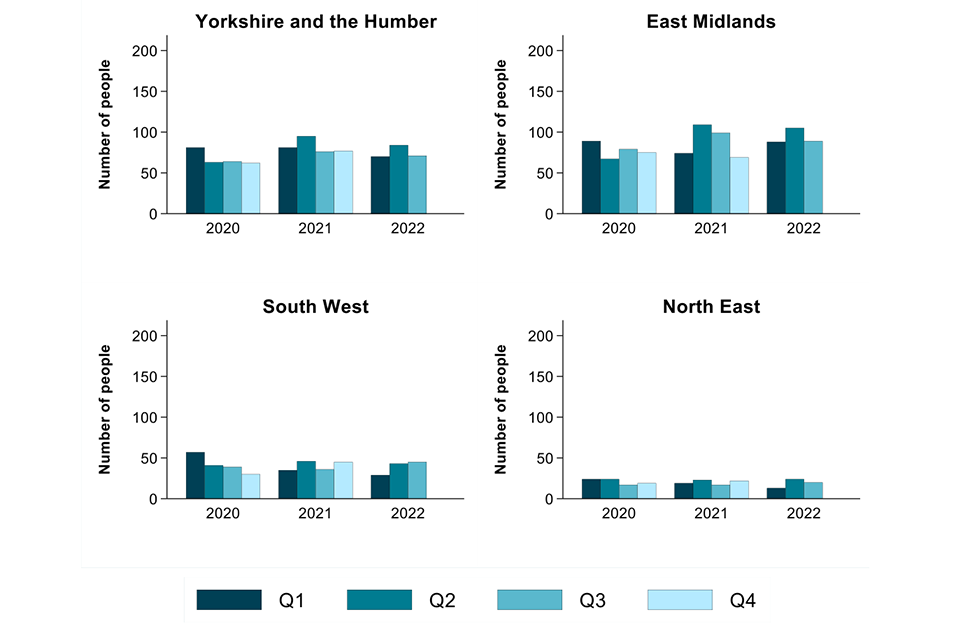
Table 1. Number of TB notifications by UKHSA centre, England, Q1 2020 to Q3 2022
| UKHSA centre | 2020 Q1 | 2020 Q2 | 2020 Q3 | 2020 Q4 | 2020 Total | 2021 Q1 | 2021 Q2 | 2021 Q3 | 2021 Q4 | 2021 Total | 2022 Q1 | 2022 Q2 | 2022 Q3 | 2022 Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| London | 379 | 333 | 382 | 370 | 1464 | 358 | 424 | 431 | 359 | 1,572 | 393 | 431 | 396 (-35) | 1220 |
| South East | 109 | 101 | 121 | 125 | 456 | 113 | 136 | 132 | 127 | 508 | 110 | 131 | 140 (+8) | 381 |
| North West | 122 | 102 | 120 | 111 | 455 | 135 | 122 | 126 | 102 | 485 | 115 | 133 | 129 (+3) | 377 |
| West Midlands | 146 | 141 | 127 | 134 | 548 | 128 | 159 | 151 | 131 | 569 | 142 | 163 | 104 (-47) | 409 |
| East of England | 104 | 102 | 83 | 82 | 371 | 89 | 105 | 86 | 92 | 372 | 96 | 93 | 90 (+4) | 279 |
| East Midlands | 89 | 67 | 79 | 75 | 310 | 74 | 109 | 99 | 69 | 351 | 88 | 105 | 89 (-10) | 282 |
| Yorkshire and the Humber | 81 | 63 | 64 | 62 | 270 | 81 | 95 | 76 | 77 | 329 | 70 | 84 | 71 (-5) | 225 |
| South West | 57 | 41 | 39 | 30 | 167 | 35 | 46 | 36 | 45 | 162 | 29 | 43 | 45 (+9) | 117 |
| North East | 24 | 24 | 17 | 19 | 84 | 19 | 23 | 17 | 22 | 81 | 13 | 24 | 20 (+3) | 57 |
| Total | 1,111 | 974 | 1,032 | 1,008 | 4,125 | 1,032 | 1,219 | 1,154 | 1,024 | 4,429 | 1,056 | 1,207 | 1,084 (-70) | 3,347 |
Table ordered by decreasing total number of people with TB in Q3 2022.
Figures in brackets in Table 3 show the change in number of people notified with TB in each UKHSA centre in Q2 2022 compared to Q2 2021.
Demographic and clinical characteristics
The number of TB notifications by where a person is born (where known) is shown in Figure 3, subdivided by whether the disease is pulmonary or extra-pulmonary (site of disease).
Figure 3. Number of TB notifications by place of birth and site of disease, England, Q3 2020 to Q3 2022
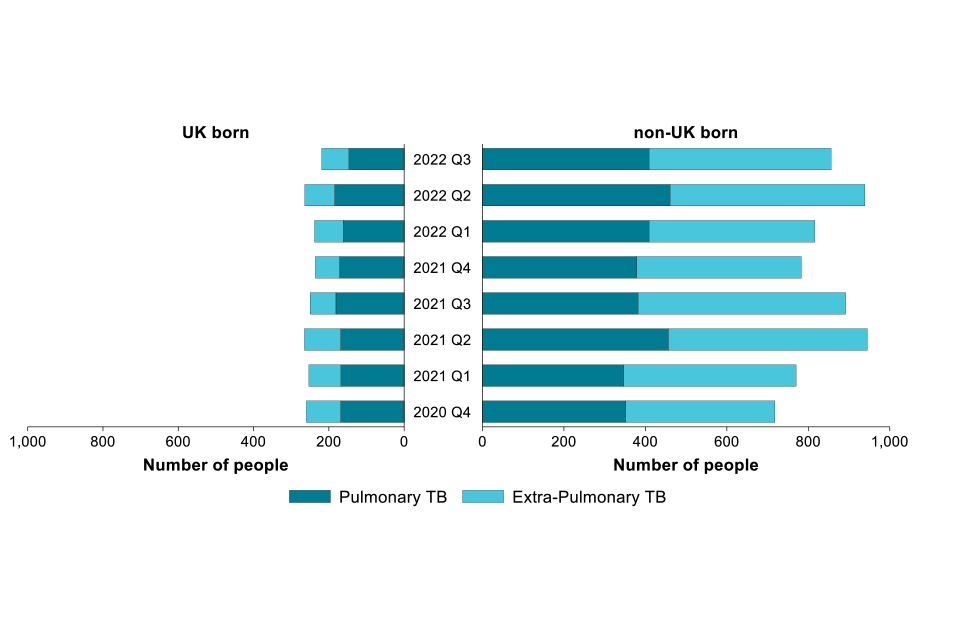
In Q3 2022 (n=856) there was a decrease (-4.0%) in the number of people notified with TB who were born outside the UK compared with Q3 2021 (n=892). The number born in the UK also decreased in the same time period (Q3 2022: n=219, Q3 2021: 250, -12.4%).
In Q3 2022, the number of people with pulmonary TB accounted for 51.8% (561 of 1,084) of all people with TB, having increased from 49.5% in Q3 2021 (571 of 1,154). For those born outside the UK, this proportion was 47.8% (409 of 856) in Q3 2022, whilst the proportion was much higher among people born in the UK (67.1%, 147 of 219).
Note that the numbers do not correspond to the total number of notifications due to missing data. Missing data may reflect the difficulties obtaining data (for example, patient died or language barriers). Place of birth was not known for 9 notifications in Q3 2022. There were 12 notifications in Q3 2021 where place of birth was unknown.
Culture confirmation
Microbiological culture of TB from patients with suspected disease confirms diagnosis and provides valuable information on antimicrobial susceptibility of TB and possible transmission events between persons notified with TB. The difficulty of obtaining cultures from some patients, especially children, is acknowledged. However, the TB Action Plan 2021 to 2026 Priority 3 workplan (Action 3.3) aims to increase culture confirmation rates by 5% per year with a specific target within the workplan (3.3.2a) to reach the European standard of 80% culture confirmation for pulmonary disease.
In 2021, preliminary data shows the number of culture confirmed cases is 60.8% (2,691 of 4,429). For pulmonary cases, the proportion culture confirmed is 74.1% (1,689 of 2,279). In Q3 2022 50.8% (551 of 1,084) of notifications are culture confirmed, of which 60.3% (332 of 551) are pulmonary. This number will increase as laboratory results are confirmed. Figure 4 shows the proportion of culture confirmed notifications received by the number of culture-confirmed notifications by disease site (pulmonary or extra-pulmonary) by quarter or year.
Figure 4. Proportion of culture confirmation among TB notifications by site of disease*, England, Q4 2020 to Q3 2022
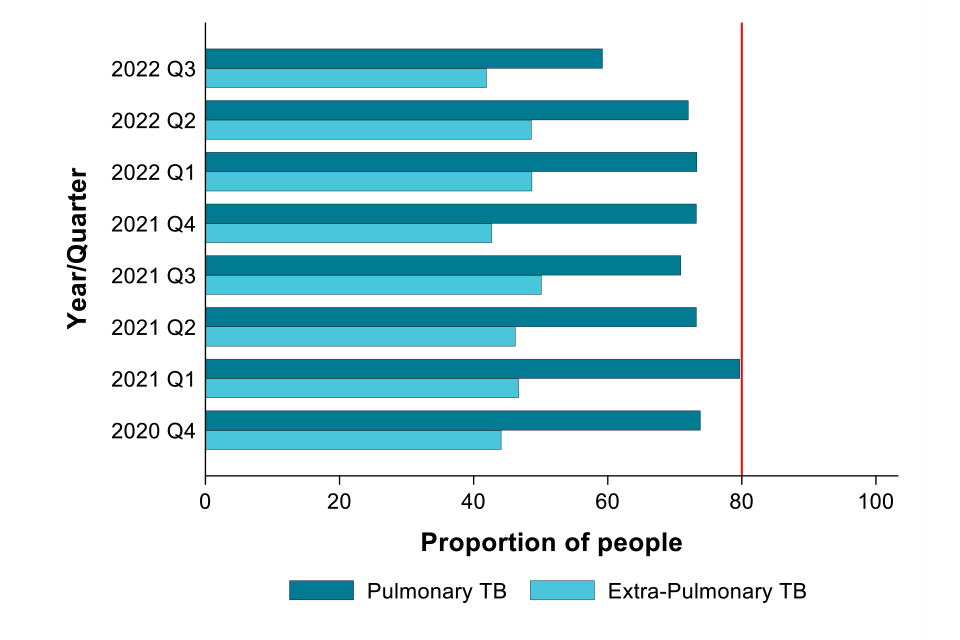
*The denominators for pulmonary and extra-pulmonary add up to more than the total number of notifications as some individuals have both pulmonary and extra-pulmonary disease.
Please note, in the following comparisons, we are comparing against figures for Q2 2022. This is due to some results for cultures from Q3 2022 not being released yet, so final results for that quarter are not yet fully available.
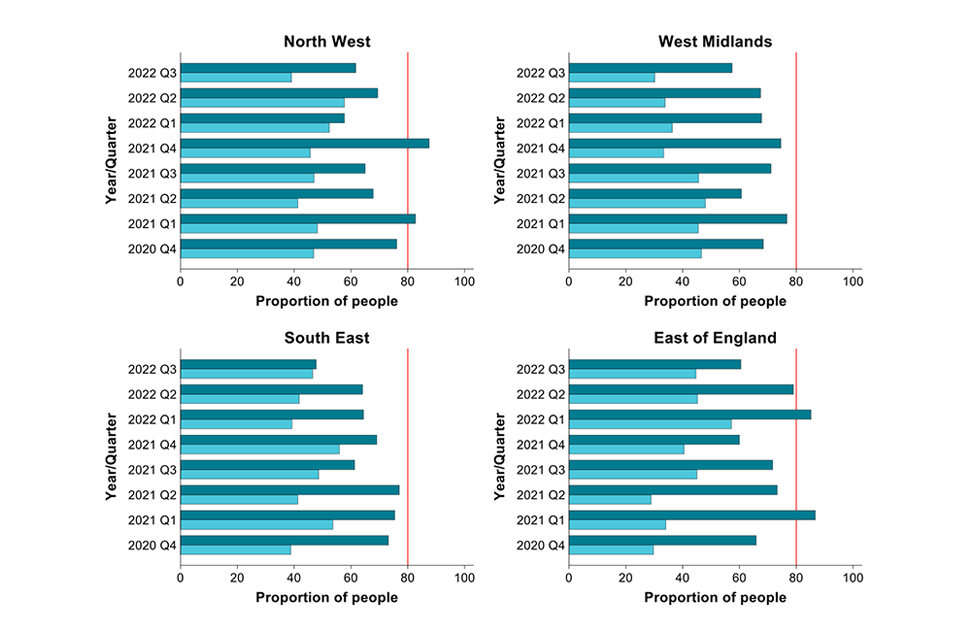
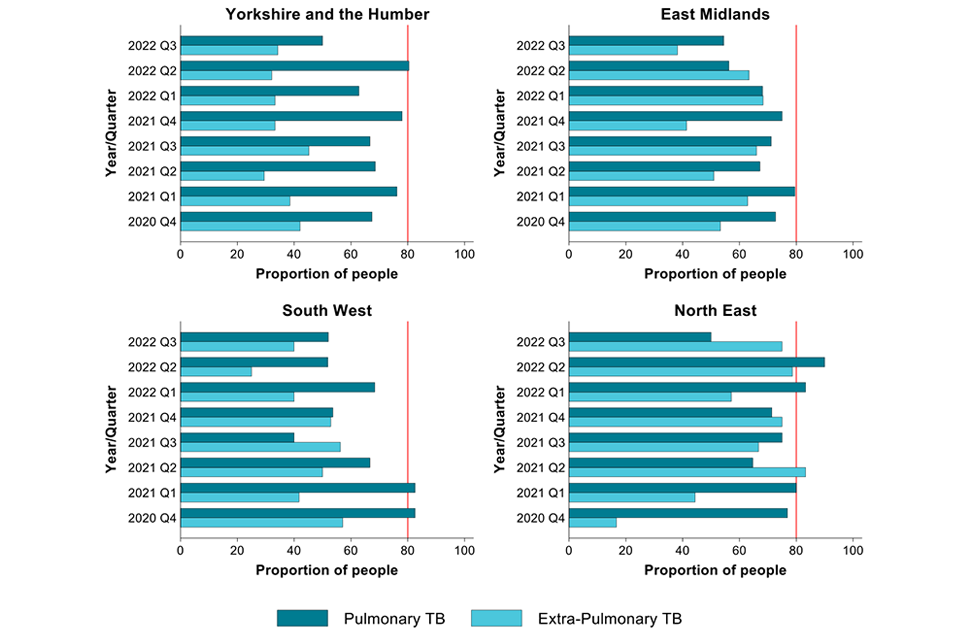
As shown in Figures 5a and 5b, in Q2 2022, the largest changes in the proportion of people with culture confirmation for:
- pulmonary TB were seen in the North East, being higher than in Q2 2021
- pulmonary TB were seen in the South West, being much lower than in Q2 2021
- extra-pulmonary TB were seen in the North West and East of England, being higher than in Q2 2021
- extra-pulmonary TB were seen in the South West, being lower than in Q2 2021
Figure 5a. Proportion of culture confirmation among TB notifications in London by site of disease, Q4 2020 to Q3 2022
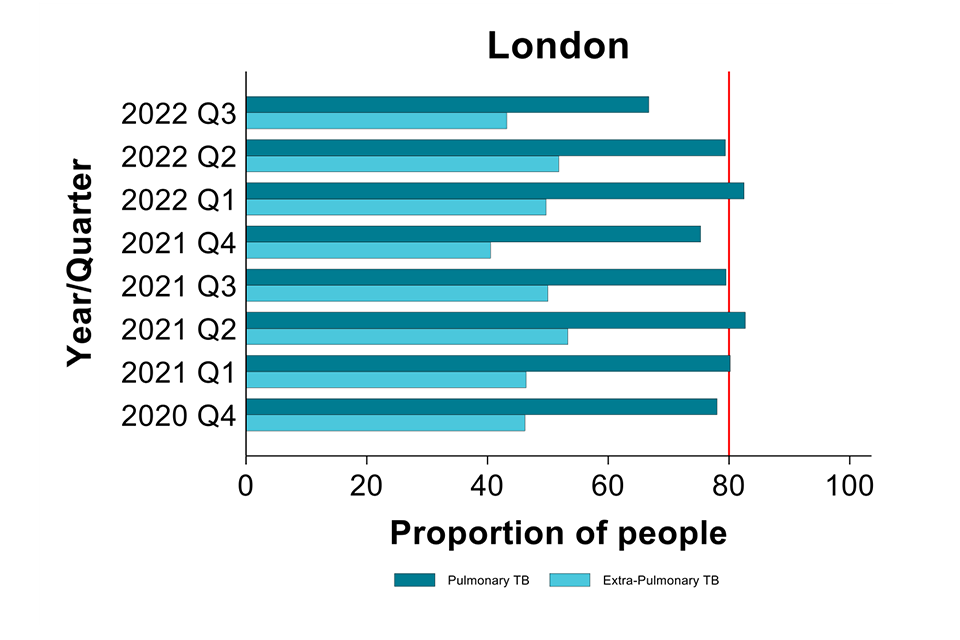
Figure 5b. Proportion of culture confirmation among TB notifications by site of disease and UKHSA centre, Q4 2020 to Q3 2022
Multi-drug resistant or rifampicin resistant (MDR/RR) TB
Resistance to antimicrobial therapy is a major concern for treatment of TB, requiring extended therapy of between 12 to 24 months. All notifications with a positive culture are tested for antimicrobial susceptibility using whole genome sequencing. If a notification does not have a positive culture, no resistance results are available.
This report uses the World Health Organization (WHO) guidance of multidrug or rifampicin resistance (MDR/RR). Multidrug resistance is classified as resistance to isoniazid and rifampicin. Figure 6 shows the number of notifications that are MDR/RR resistant.
Figure 6. Number* of TB notifications with MDR/RR-TB, England, Q4 2020 to Q3 2022
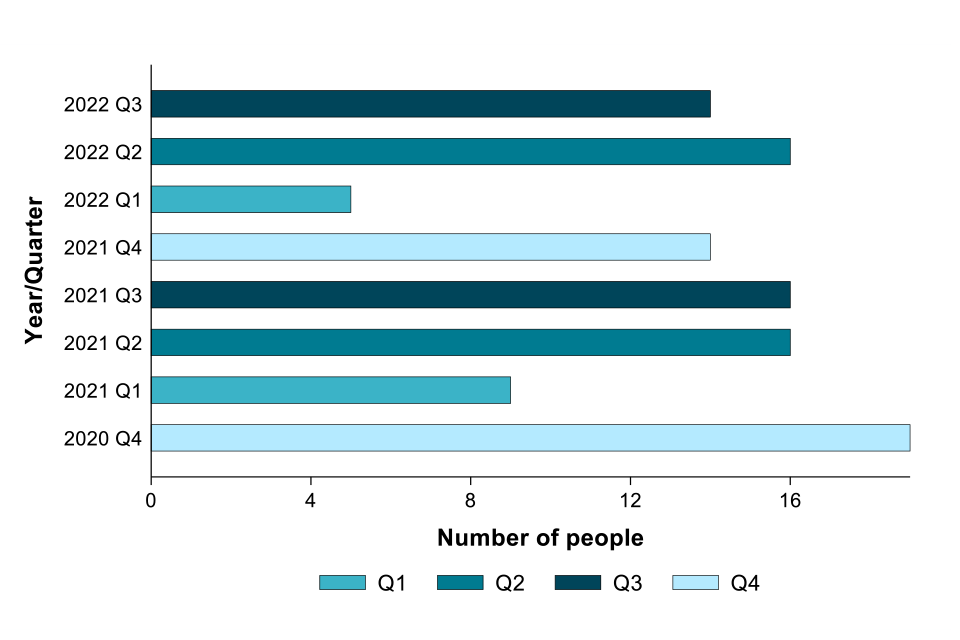
*Note: this figure displays numbers rather than proportions due to low number of MDR/RR-TB notifications.
There were 14 people notified in Q3 2022 with confirmed MDR/RR-TB. There were 16 notifications with confirmed MDR/RR-TB in Q3 2021.
Note: 55 people were notified with MDR/RR-TB between Q1 and Q4 2021, compared to 58 from Q1 to Q4 2020. Numbers may increase as results for cultures in the most recent quarter may not yet be available.
Treatment delays
Treatment delay is the time between the reported symptom onset date and treatment start date. It reflects either delays in patients seeking healthcare or delays in diagnosis after presentation, or both. Treatment delays are reported only for pulmonary TB (Figure 7) due to the risk that extended treatment delays may increase transmission within communities. The graph stops at 80%, not 100%, to reflect the Action Plan target of 80% of people starting treatment within 4 months.
Figure 7. Proportion* of pulmonary TB notifications starting treatment within 4 months (symptom onset to treatment start), England, Q4 2020 to Q3 2022
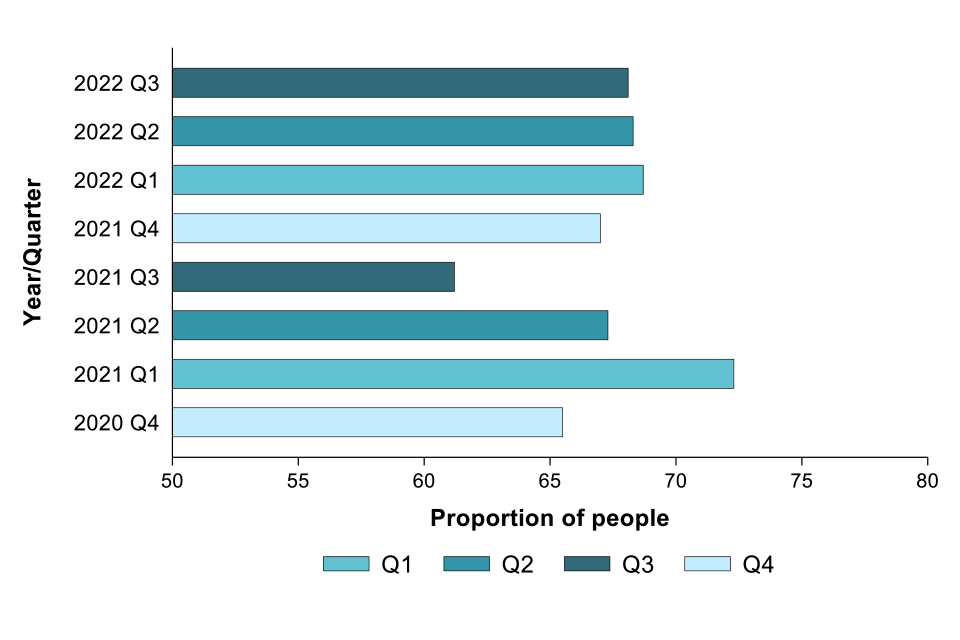
*Note: the x-axis is not scaled to start at zero to improve data visualisation.
In Q3 2022, 68.1% of people with pulmonary TB started treatment within 4 months of symptom onset, compared to 61.2% in Q3 2021. This proportion will likely increase as some people in the most recent quarter are yet to begin treatment.
Figures 8a and 8b show the proportion of people starting treatment within 4 months by UKHSA centre (note: the axis is 100% in these figures, with 80% target indicated). Analysis excludes those with post-mortem diagnosis.
Figure 8a. Proportion of pulmonary TB notifications in London starting treatment within 4 months (symptom onset to treatment start), Q4 2020 to Q3 2022
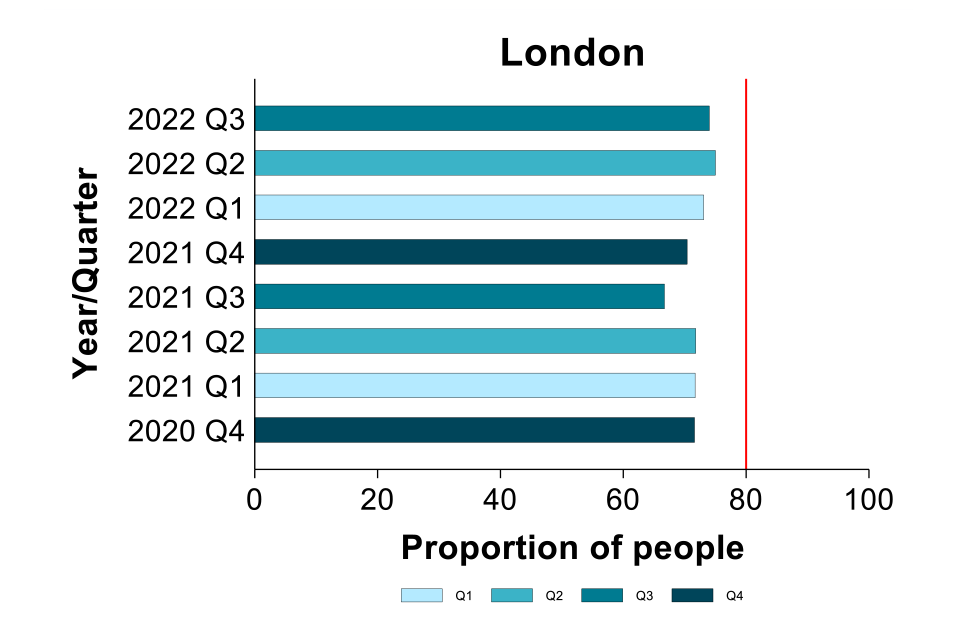
Figure 8b. Proportion of pulmonary TB notifications starting treatment within 4 months (symptom onset to treatment start) by UKHSA centre, Q4 2020 to Q3 2022
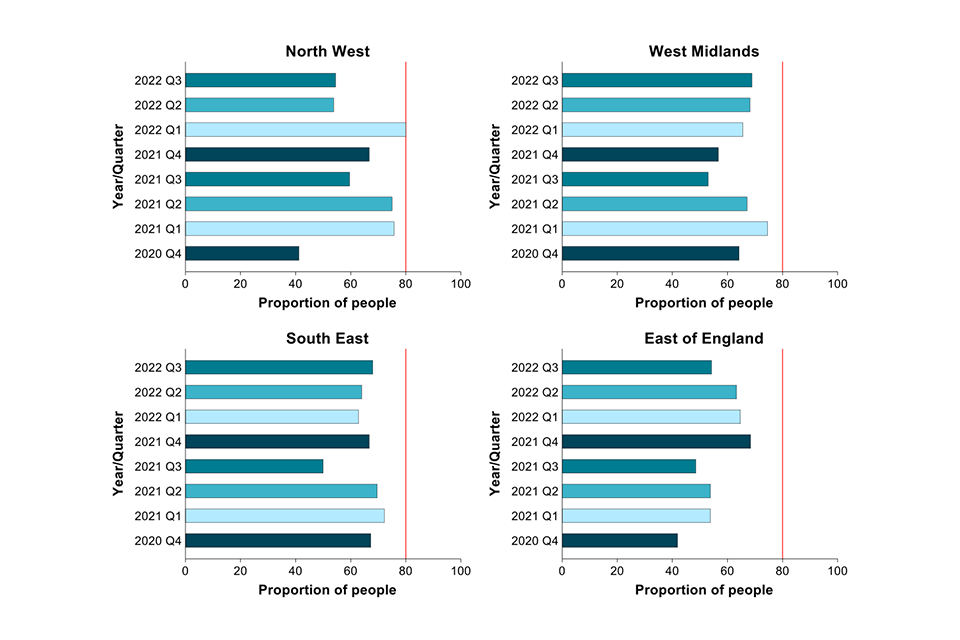
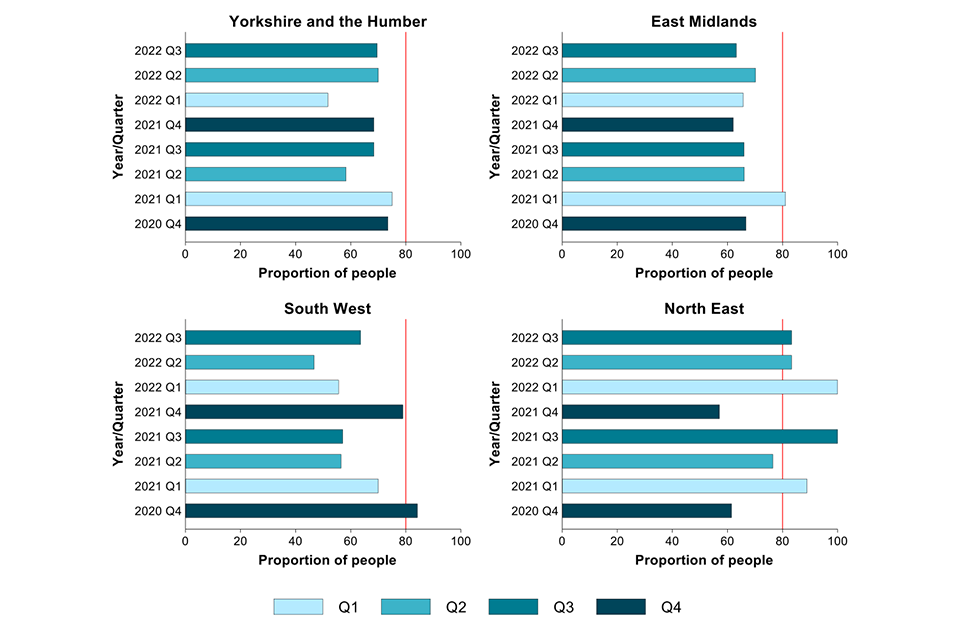
In Q3 2022, the proportion of people with TB who started treatment within 4 months of symptom onset in:
- the East of England, London, the South East, the South West and the West Midlands was higher than in Q3 2021
- the North East and the North West were lower than in Q3 2021
- the other regions were broadly similar
Treatment outcomes
Treatment outcomes are reported for persons notified up to Q3 2021 with drug sensitive TB, the majority of whom should have completed treatment within 12 months of treatment start. Data is not presented for those notified after Q3 2021 as many are not expected to have completed treatment. The data excludes people in the drug resistant cohort and those with central nervous system (CNS), spinal, miliary or cryptic disseminated TB as treatment time for these groups usually exceeds 12 months.
Where treatment outcome is reported as not known or transferred to a different country, data is included in the not evaluated group. Figure 9a shows outcomes for notifications where treatment is complete, not evaluated or other (proportion shown in bars). The category ‘other’ comprises those who died, were lost to follow-up, are still on treatment (treatment period may be extended beyond 12 months in some cases) or where the treatment was stopped, the proportion of each of these is shown in Figure 9b.
The proportion of people with drug sensitive TB (with an expected treatment duration of less than 12 months) who completed treatment at 12 months was 69.9% for people notified in Q3 2021.
Please note: the latest 3 quarters tend to show a high proportion of people with treatment outcomes recorded as ‘not evaluated’ despite having started at least 12 months previously. This reflects a delay in reporting the final outcome. The proportion not evaluated is expected to decrease with time.
Figures 9a (top) and 9b (bottom). Outcomes at 12 months for people with drug sensitive TB with expected treatment duration <12 months*, ** England, Q4 2019 to Q3 2021
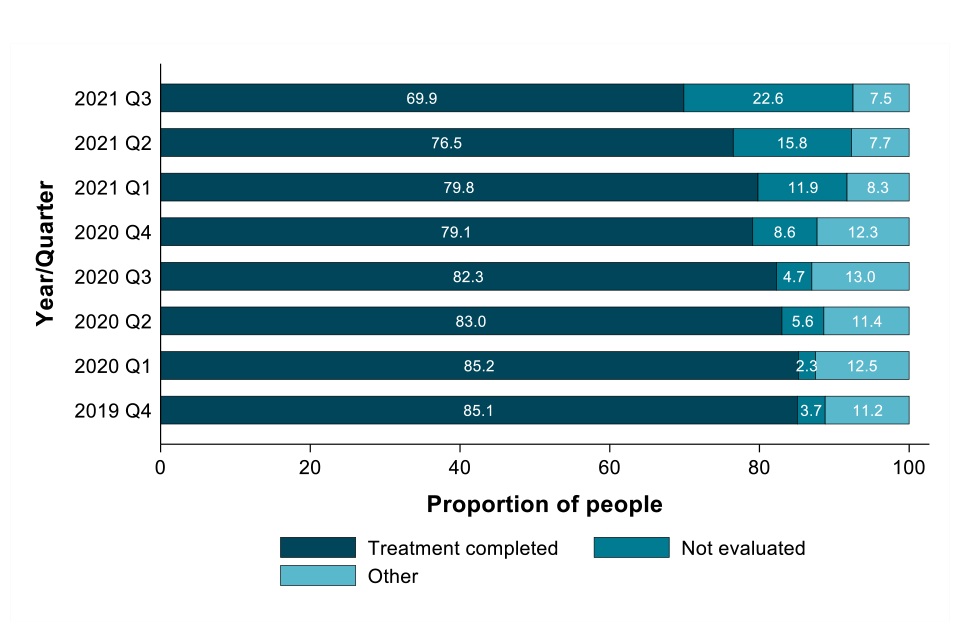
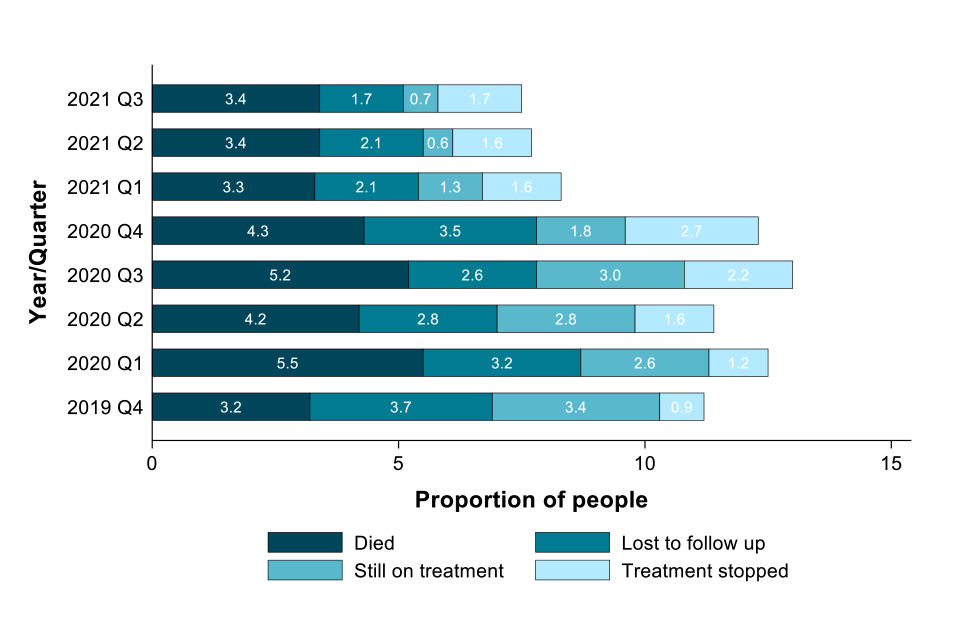
*Excludes people in the drug resistant cohort and those with CNS, spinal, miliary or cryptic disseminated TB.
**Not evaluated includes unknown and transferred out.
Social risk factors
Social risk factors (SRFs) reported as categorical yes or no variables with current or past history recorded as yes. Information on these social risk factors is collected though the routine surveillance system via interviews by the clinical team. Social risk factors that are recorded are current or history of prison, drug and alcohol use and homelessness. Data reported is for persons over 15 years and older due to low numbers in young children.
Figure 10a. Proportion of TB notifications (≥15 years) with at least one social risk factor (SRF)*, England, Q4 2020 to Q3 2022
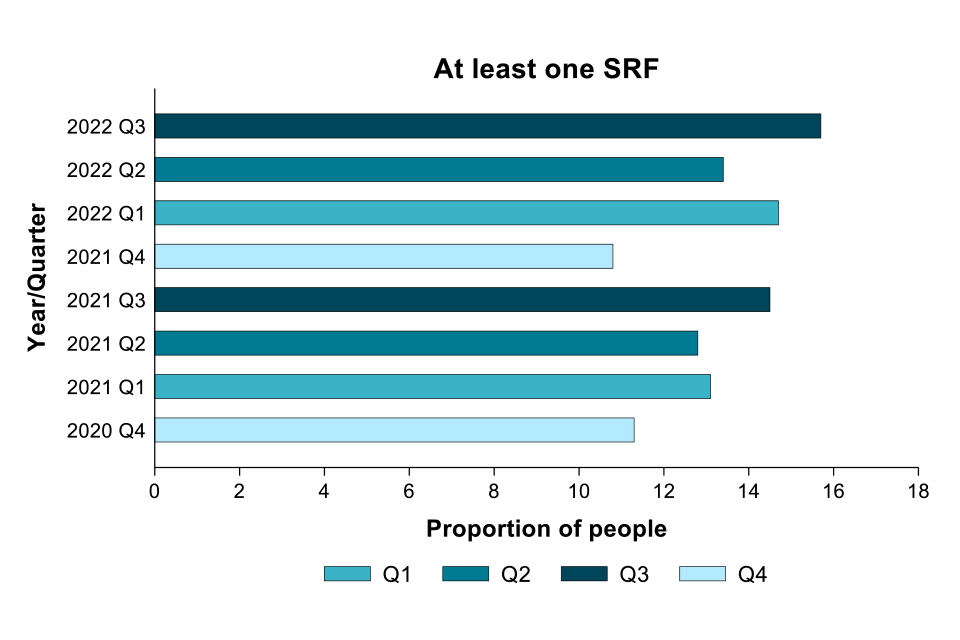
*Note: the axes on the figure for people with at least one SRF (Figure 10a) are different to that for individual SRFs (Figure 10b) due to the higher proportion of people with at least one SRF.
In Q3 2022, 15.7% of people with TB aged 15 years and older had at least one SRF. This is slightly higher than in Q3 2021 (14.5%).
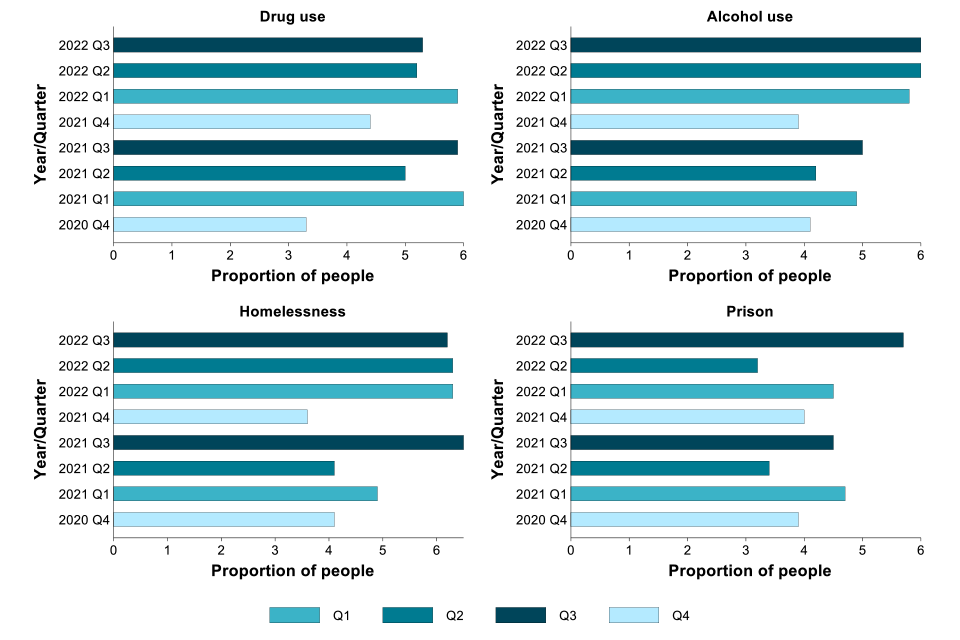
For single risk factors, shown in Figure 10, the proportion of people with TB in Q3 2022 with:
- current or a history of drug misuse was lower than in Q3 2021
- alcohol misuse was higher than in Q3 2021
- current or a history of homelessness was lower than in Q3 2021
- imprisonment was higher than in Q3 2021
Figure 10b. Proportion of TB notifications (≥15 years) by social risk factor, England, Q4 2020 to Q3 2022