7. Age Spotlight
Updated 18 November 2021
Applies to England
Introduction
This Spotlight is part of a series within the COVID-19: mental health and wellbeing surveillance report. The report is about population mental health and wellbeing in England during the COVID-19 pandemic. It includes up-to-date information to inform policy, planning and commissioning in health and social care. It is designed to assist stakeholders at national and local level, in both government and non-government sectors.
This spotlight is composed of 2 main categories of information:
-
weekly data drawn from the UCL COVID-19 Social Study up to week 30 of 2020
-
analysis from a range of ongoing academic research projects made publicly available by week 30 of 2020 or added by special request
The 2 categories of information have separate purposes.
Weekly data serves as an early warning system for potentially large changes and differences between groups. It should not be used to draw conclusions about smaller changes or differences between groups from week to week. This is because the data has not been analysed to control for any confounding factors or potential biases.
The analysis from academic research offers a good picture of change over time and differences between groups. Although less up to date, this intelligence is the basis for more nuanced interpretation and also feeds into the Important findings chapter.
The latest available version of the data presented in this spotlight can be found in the Wider Impacts of COVID-19 on Health (WICH) tool.
The Spotlight series describes variation and inequality in the population. Spotlights have also been published for gender, ethnicity and pre-existing mental health conditions.
This Spotlight presents intelligence on potential inequalities by age. Evidence of different mental health and wellbeing experiences are presented for people aged 18 and over. A separate chapter of the report describes the experiences of children and young people.
It is important to note that:
-
scales on graphs are not the same
-
surveys may not be representative (see Caveats)
-
the basis for the intelligence included is presented in the Methodology document
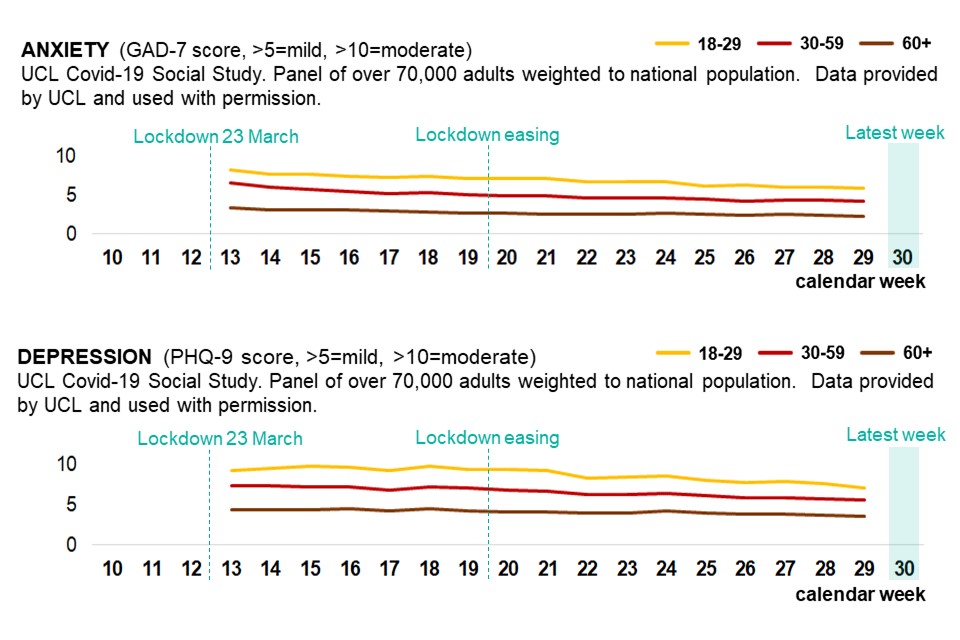
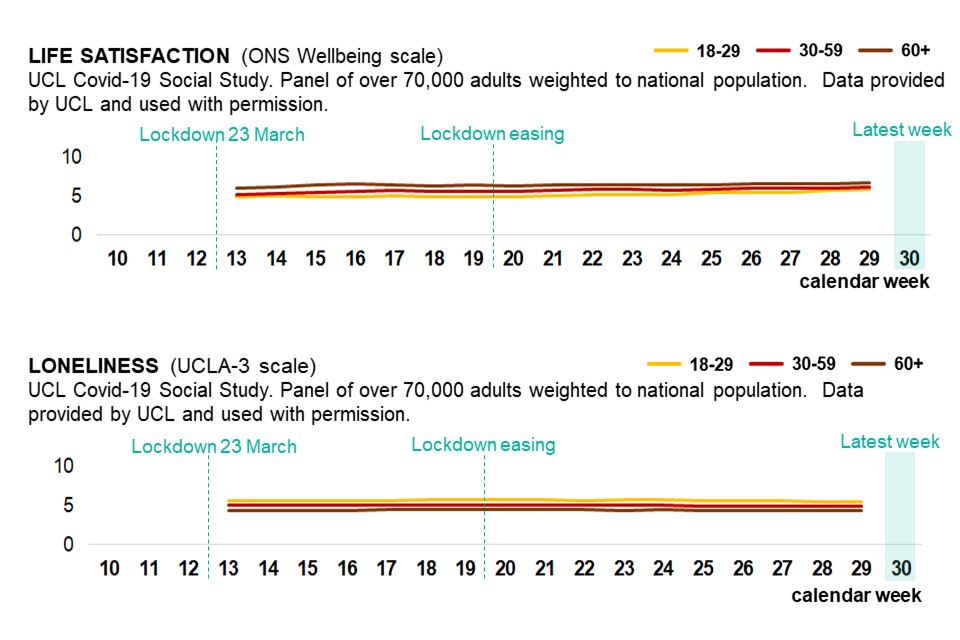
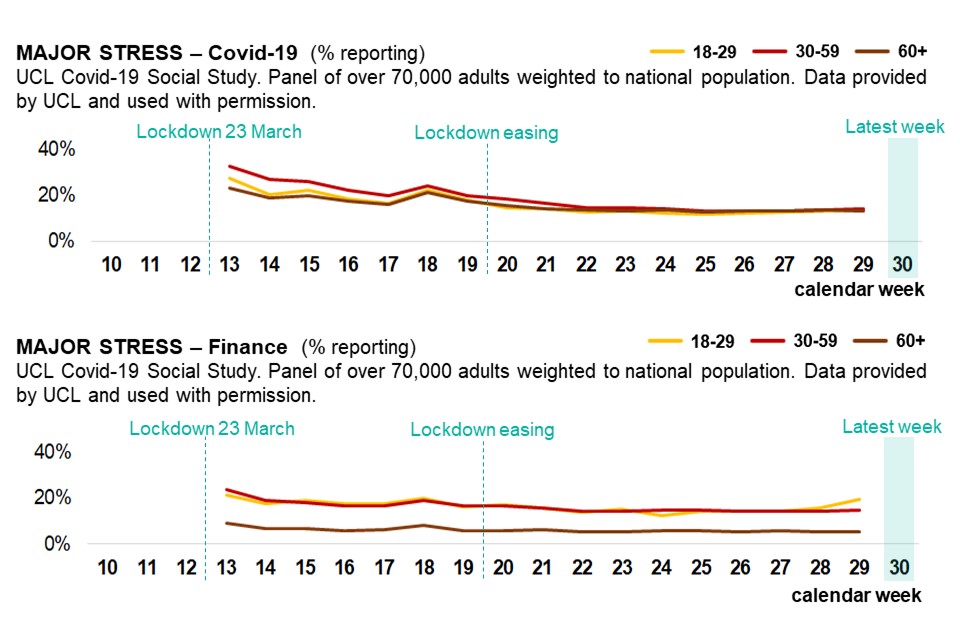
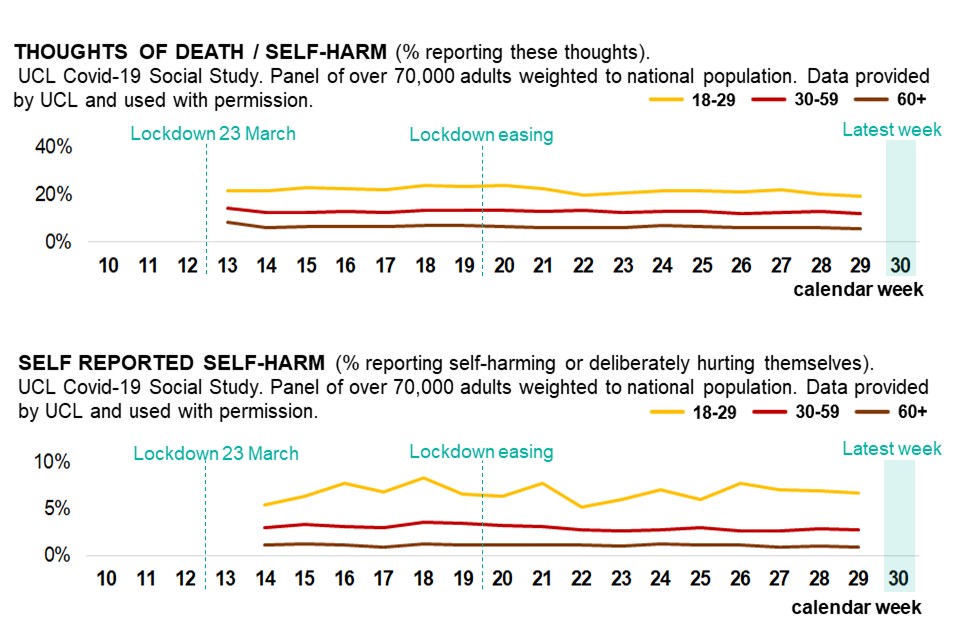
Graphs tracking age inequality in the population
Younger adults tend to report worse mental health and wellbeing during the pandemic. These differences may have narrowed over the weeks since lockdown.
Up-to-date data is available on the WICH tool.
Young adults are reporting worse mental health and wellbeing
One of the most consistent findings so far, across multiple research projects, is that young adults are reporting worse mental health and wellbeing than middle and older aged adults.
The first indications that the mental health and wellbeing effect of the pandemic may be particularly adverse for younger adults were from 2 cohort studies established in April 2020. They found mean self-reported scores for depression, anxiety, stress and trauma to be higher than pre-pandemic population norms, and that younger respondents were more likely to report worse symptoms. This was supported by initial descriptive statistics from a third cohort study established in late March 2020.
Since then, further studies have supported these findings and added detail:
-
two studies, using April 2020 data from pre-existing longitudinal cohort studies, found young adults had higher risks of general psychiatric disorders and loneliness, and that probable depression, anxiety and low wellbeing decreased with age
-
that the prevalence of anxiety in young adults after easing COVID-19 restrictions has remained high – almost double the pre-pandemic levels
-
that young adults, already at higher risk of experiencing loneliness before the pandemic, were now at even higher risk and that being a university student may also be a risk factor
-
that younger adults were more likely than older adults to report increasing rather than decreasing loneliness between late March and early May 2020
Comparison with pre-COVID-19 trends
It is important to view recent evidence in the context of background changes in mental health and wellbeing by age. For instance, the 2014 Adult Psychiatric Morbidity Survey (APMS) found that people aged 16 to 64 (17% to 18%) were around twice as likely to report symptoms of common mental disorders (CMD) as those aged 65 and over (10% 65 to 74, 8% 75 and over).
Between the 2007 and 2014 APMS surveys, increases in CMD were evident among late midlife men and women (aged 55 to 64), and approached significance in young women (aged 16 to 24). The gap in rates of CMD symptoms between young men and women increased. In 1993, 16 to 24 year old women (19.2%) were twice as likely as 16 to 24 year old men (8.4%) to have symptoms of CMD. By 2014 this had increased to almost 3 times (26% in women and 9.1% in men).
Differences by age and gender in the population’s mental health were present before the pandemic.
Is COVID-19 leading to greater differences in mental health by age, or reflecting pre-existing inequalities?
There is now evidence that between March and June 2020 young adults experienced worsening mental health and wellbeing compared to older age groups. This increase is likely to be as a result of COVID-19 and the national response. Multiple studies, using data from the same cohort of people surveyed before and during the pandemic, help to provide this evidence. These studies found that:
-
while there was an overall decline in mental well-being after the onset of the COVID-19 pandemic, this decline was larger for younger adults than older adults
-
the increase of average population GHQ-12 scores (used to measure mental distress) between 2018 to 2019 and April 2020 was 0.5 points higher than expected, after accounting for prior upward trends between 2013 and 2019. Increases were greatest in 18 to 24 year olds (2.7) and 25 to 34 year olds (1.6)
-
the percentage of participants classified as experiencing CMD overall increased from 23.3% in 2017 to 2019 to 36.8% in April 2020, but the rise was 8.6 percentage points greater among those aged 18 to 34 compared to those aged 50 to 64
-
although psychological distress substantially increased one month into the COVID-19 lockdown for all (prevalence rising from 19% in 2017 to 2019 to 30% in April 2020), the increase was most pronounced in people aged under 45
-
younger people have reported higher overall levels of loneliness, and that there has been an increase in the proportion of young people feeling lonely
Experience of older adults
One pre-existing cohort study (with a convenience sample) that focuses on older adults (aged 50+) found slight increases in average self-reported depression and anxiety symptoms and that these were associated with loneliness and decreases in physical activity. However, overall levels are lower than those reported by younger adults and have been consistently low for the last 5 years.
This is broadly supported by data from the Understanding Society cohort. Data from the April 2020 wave suggests that, among people aged 55 and over there was no evidence of a change in mental health and wellbeing due to COVID-19. However, one study, when considering data from April and May 2020 identified that between 20% and 25% of older respondents presented as new potential cases of CMD in April (which is higher than anticipated), although this returned to expected levels in May (10%), compared to 40% to 50% of younger respondents in April, and 20% in May.
In summary
For adults there appears to be an underlying relationship between age and the impact of COVID-19 on mental health and wellbeing. Younger adults are reporting both worse symptoms and a larger deterioration in mental health. On average, older age groups appear to have been less affected so far.
