National intelligence network on drug health harms briefing: July 2018
Updated 13 January 2020
This briefing is based on a meeting of the national intelligence network (NIN) on the health harms associated with drug use. The NIN is made up of representatives from drug treatment services, local authority public health and commissioning teams and national professional and membership bodies. Network meetings are chaired by Dr Michael Kelleher, consultant addictions specialist and clinical lead for Lambeth Addictions at the South London and Maudsley NHS Foundation Trust.
1. Evaluation of needle and syringe programmes (NSP)
Professor Peter Vickerman (University of Bristol)
Needle and syringe programmes (NSP) and opiate substitution treatment (OST) are the primary hepatitis C virus (HCV) prevention interventions for people who inject drugs (PWID) in the UK. A number of European studies, outlined in a recent Cochrane review, shows that NSPs are associated with a 50% to 60% reduction in the risk of PWID acquiring hepatitis C.
A recent study set in Bristol, Walsall and Dundee has shown that current levels of OST and high coverage needle and syringe provision is preventing an increase in hepatitis C transmission in the UK. Research suggests that NSP also saves money in terms of health benefits compared to where there is no NSP.
The study suggests that scaling-up OST and high coverage needle and syringe provision would reduce the amount of hepatitis C treatment needed through directly decreasing infection and re-infection. This could help achieve the World Health Organization (WHO) strategy to eliminate HCV as a public health threat.
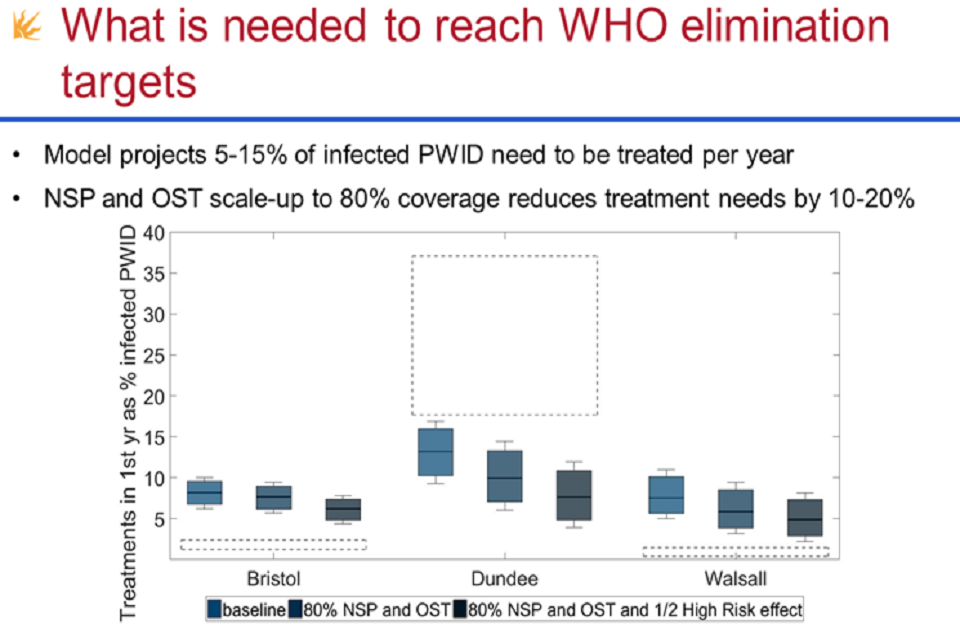
Graph showing how many infected people who inject drugs would need to be treated each year to meet World Health Organization targets to eliminate hepatitis C
Data from the unlinked anonymous monitoring (UAM) survey of people who inject drugs suggests there are distinct groups of people who inject drugs who use different drugs in different ways and use either low dead-space syringes (LDSS) or high dead-space syringes (HDSS). LDSS have a design to limit the dead space that exists between the syringe hub and needle. This space can retain blood and other waste. Users of HDSS who predominantly inject into their groin (they need longer needles to inject into some areas) tend to be older and inject crack.
HDSS could increase the risk of becoming HCV-infected, as can groin injecting, and interventions are needed to target these behaviours. New evidence shows that wider use of low dead space detachable syringes would save money and prevent new infections.
2. Implementing research findings on the acceptability of low dead space syringes for people who inject drugs
Dr Joanna Kesten (National Institute for Health Research (NIHR), Collaboration for Leadership in Applied Health Research and Care (CLAHRC) and NIHR Health Protection Research Unit (HPRU) in Evaluation of Interventions, University of Bristol)
Sharing injecting equipment is a major risk factor for passing infections between people who inject drugs. The level of risk of transmission of infection is affected by the amount of virus in the syringe, which is partly determined by the quantity of blood.
Studies which simulated common injection practices have shown that low dead space syringes (LDSS) retained up to 1,000 times less blood than high dead space syringes and transferred significantly less blood after rinsing the equipment.
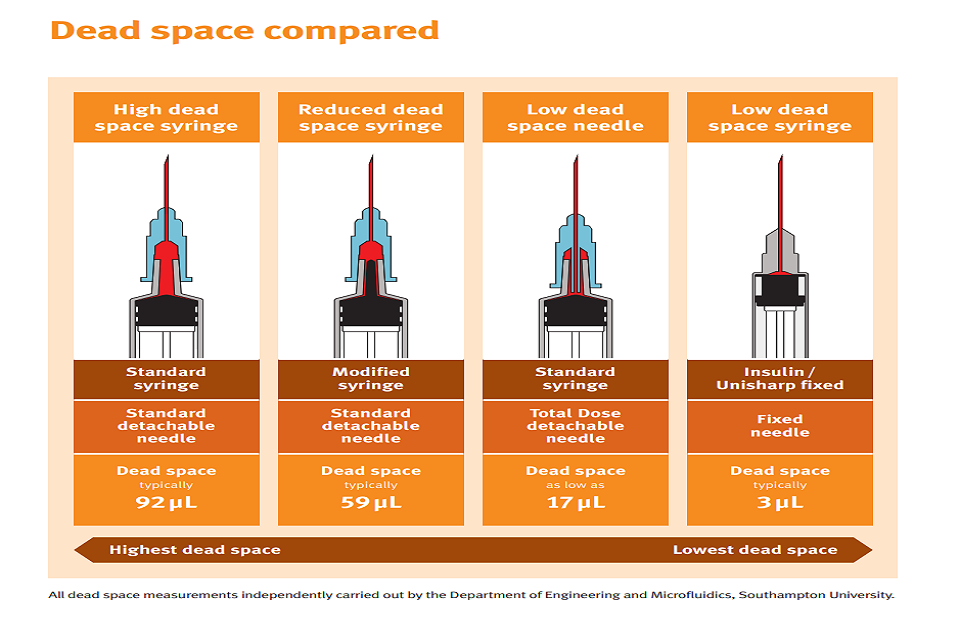
The graphic shows different types of syringes with different amount of dead space, from highest to lowest dead space
Developing detachable LDSS could increase the proportion of LDSS syringes in circulation.
A recent study explored the views of people who inject drugs, professionals and the volunteers who work with them, on the acceptability of detachable LDSS. Staff and PWID saw benefits to using LDSS, including less wasted drug and a lower risk of passing on infections, but they felt that changing equipment which is an established part of an injecting routine would be a challenge. The study recommended gradual implementation of low dead space equipment, offered alongside existing equipment and supported by training and education.
Implementation work is being carried out to encourage PWID to use appropriate injecting equipment, including detachable LDSS and other practices to reduce harm. This work involves creating harm reduction infographics for PWID and needle and syringe programme staff and accompanying training materials for staff.
NICE guidance on provision of needle and syringe programmes recommends that local areas commission services which offer and encourage the use of low dead space needles and syringes.
3. Smoking and substance misuse
Qasim Chowdary (PHE alcohol,drugs, tobacco and justice division)
Adult smoking rates have been steadily falling and the UK has the second lowest smoking rates in Europe. But some populations have been left behind and smoking prevalence among people who misuse alcohol and drugs remains high. According to the National Drug Treatment Monitoring System (NDTMS), people in treatment for opiate use had the highest reported rates of smoking when starting treatment (59%) and 2014 research found that 88% of all clients in substance misuse treatment were current smokers.
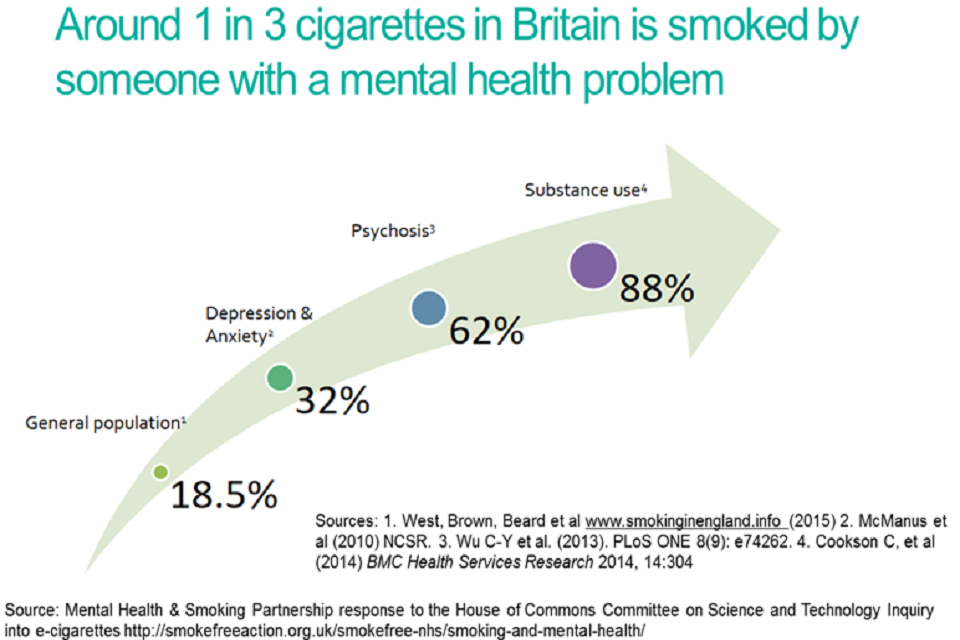
Graphic shows different smoking rates of different groups of people who have mental health or substance misuse problems
There can be a misperception that people in alcohol and drug treatment are not worried about their smoking and are unwilling or unable to address it. A Cochrane review in 2016 shows that interventions to address smoking along with alcohol and drug misuse are effective for stopping smoking and can also support changes in alcohol and drug use.
Smoking cessation interventions are effective, and they can lead to reduced risk of heart disease, stroke, cancer and premature death. Developing effective treatment programmes and effective care pathways can improve local smoking cessation outcomes for people in alcohol and drug treatment
4. Nasal naloxone
Steve Taylor (PHE alcohol, drugs, tobacco and justice division)
Naloxone is the emergency antidote for overdoses caused by heroin and other opiates and opioids (such as methadone, morphine and fentanyl).
The main life-threatening effect of heroin and other opiates is to slow down and stop breathing. Naloxone blocks this effect and reverses the breathing difficulties.
Naloxone is a prescription-only medicine and can’t be sold over the counter. However it can be supplied without prescription by drug services, following a change in legislation in 2015. In the UK, there are currently only intramuscular and intravenous injectable preparations, but intranasal naloxone is likely to be available in the near future.
Improvised intranasal devices have been used for some time in the US. Their experience shows that intranasal administration of naloxone appears to be more acceptable to non-medics, such as social workers or friends and family who may need to administer naloxone. However, there have been concerns about the effectiveness of these improvised, relatively high volume-low concentration products, so there have been efforts to develop specific intranasal preparations at lower volume and higher concentration.
In Europe, Mundipharma’s product (1.8mg naloxone in a single-dose container, 2 containers per pack, called Nyxoid) received marketing authorisation in November 2017 and there will be a phased programme of market introduction. The cost is still to be determined and it may be higher than existing injectable formulations.
It is currently uncertain when and how intranasal naloxone will be allowed to be provided by drug services without prescription.
A recent Local Government Association survey found there is naloxone provision, especially from drug services, but also that more can be done to promote its availability and provision, even before nasal naloxone becomes available.
5. Novel buprenorphine preparations
Dr Michael Kelleher (South London and Maudsley NHS Foundation Trust)
The 2017 drug treatment clinical guidelines refer to different forms of buprenorphine (an opioid used in opioid substitution treatment) being in development.
These include rapid-dispersal forms of buprenorphine such as quick-dissolving film or tablets, which may be of clinical benefit by enabling simpler supervised consumption.
Ultra-long-acting forms of buprenorphine are available as subcutaneous depot injections, transdermal patches, and subdermal implants. This means that daily dosing is no longer required and can be given less frequently such as weekly or monthly.
Depot buprenorphine may mean more consistent doses received by patients. There are advantages for homeless people who might find it challenging to attend services or safely carry and store their prescription. The most significant potential benefit could be in freeing keyworker (and client) time up from the workload and pressure of dealing with prescribing and dispensing and consumption. Time freed up could be spent more creatively and productively on psychological support, and other recovery-orientated interventions. Other potential benefits are a reduced risk of diverting medication and reduced risk to children because the medication does not need to be kept at home.
However, there is also a risk that less time needs to be spent with each client, resulting in a stripped-down ‘script-only’ service.
The opinions of service users on ultra-long-acting depot and implant medications were collected at focus groups.
Service users had positive perceptions about these medications and thought that the benefits would be:
- more freedom from pharmacy and drug service
- to liberate users from habit-forming medication-taking behaviours
- to give users greater privacy and dignity in treatment
The service users also have some concerns and anxieties about:
- the surgical implant procedure
- irreversibility if a medical problem occurred
- irreversibility if the individual changed their mind
There were some negative perceptions related to:
- a reduction in personal power and control
- the state of being ‘semi-permanently’ in treatment
- being unaccustomed to steady and continuous maintenance on medication
Current information suggests that one or more of these products could be authorised and made available sometime in 2019.
6. Public Health England update
Pete Burkinshaw, Steve Taylor and Eamonn O’Moore (PHE Alcohol, Drugs, Tobacco and Justice Division) and Stephanie Migchelsen (PHE National Infection Service) updated the network on recent PHE activity related to drug-related health harms
Fentanyls
In response to concerns about deaths from heroin adulterated with fentanyls (potent synthetic opioids) in 2016 to 2017, PHE has an extensive programme of work to prevent future deaths, including supporting an increase in the provision of naloxone, the heroin overdose antidote. Two resources for local authorities are now available: guidance on preparing to respond to future threats from potent opioids, and modelling of recommended levels of local authority naloxone provision.
Hepatitis C tests
PHE is working with voluntary sector service providers to improve reporting of dried blood spot test results for hepatitis C. PHE is also working with NHS England and others to promote good practice among Operational Delivery Networks (ODNs) across the country.
Hepatitis B vaccination shortage
The shortage of hepatitis B vaccinations is improving but continues as a ‘national enhanced incident’. A likely backlog in ordering by sexual health clinics and drugs services might lead to an increase in ordering in the weeks ahead, meaning stock is likely to remain low for the next couple of months.
Needle exchange monitoring system
PHE’s needle exchange monitoring system (NEXMS) has stopped operating, as of 3 April 2018. Data submissions to NEXMS had been falling for some time and the system did not meet national requirements sufficiently to make it worthwhile promoting or expanding its use. PHE is still committed to supporting the recording of information from needle and syringe programmes (NSP) and other harm reduction interventions and there may be a national initiative to collect more complete NSP data in the future, including for reporting to the World Health Organization.
National prison treatment statistics
Statistics for substance misuse treatment in secure settings published for 2016 to 2017 showed a slight overall fall in the number of adults in contact with treatment services in these settings. There was an increase in people with problematic crack use, which is in line with treatment numbers in the community and with prevalence estimates. Although there was an increase in people treated for new psychoactive substances, it was perhaps not as large as might have been expected given the widespread issues with synthetic cannabinoids in prisons. Continuity of care between treatment services in prisons and the community, defined as engaging with community treatment within 21 days of release, was only 30% and continues to be an area of concern.
Why Invest?
PHE published the updated why invest? slide set and accompanying materials to help commissioners, providers and healthcare professionals with making the case for investing in drug and alcohol treatment and interventions.
PHE e-cigarette review
An update of the PHE e-cigarettes evidence review has been published and concludes that vaping poses only a small fraction of the risk of smoking, and switching completely from smoking to vaping results in substantial health benefits.
Xanax
Reports of Xanax (a potent, short-acting benzodiazepine) use among young people have continued across the country. Anecdotal evidence suggests the drug is taken not just recreationally but also as self-medication. PHE is continuing to call for intelligence through PHE Centres via their local authority contacts, while the RIDR (Report Illicit Drug Reactions) system has received recent reports of Xanax overdose.
7. Members’ update
The drugs information network DrugWatch has issued a briefing on ‘lean’ (also known as ‘purple drank’). Use of lean in the UK has been more prominent in recent months and specifically linked to young people, with concerns raised by drug service practitioners from around the country.
